Multidisciplinary Approach in a Patient with Seat-belt Trauma to the Breast: Case Reports
1Breast Unit, Verona Integrated Hospital Company P.le A. Stefani, Verona, Italy
2Radiology Division, Integrated Hospital Verona P.le A. Stefani, Verona, Italy
3Plastic Division, European Institute of Oncology via Ripamonti 435 20141, Milano, Italy
- *Corresponding Author:
- Alessandra Invento
Plastic Division, European Institute of Oncology,
Ripamonti 435 20141, Milano, Italy
E-mail: alessandra.invento@ieo.it
Received date: November 07, 2018; Accepyed date: December 20, 2018; Published date: December 30, 2018
Citation: Pellini F, Accordini B, Puntel G, et al. (2018) Multidisciplinary approach in a patient with seat-belt trauma to the breast: case reports. Gen Surg Rep. Vol.2 No.2:7.
Abstract
Keywords
Fainting; Mortality; Injuries; Syndrome
Introduction
The use of three-point lap-diagonal seat-belt restraint has resulted in a significant reduction in car accident-related mortality [1], but it has increased the incidence of bone, soft-tissue and internal organ injuries, known as “seat belt syndrome” [2].
Breast traumas are rarely described in literature even if the clinical characteristics and the evolution fisio pathologic as are complex and should be described specific guidelines. The severity of breast injuries following road traffic collisions can range from a small bruising in the breast to an avulsed breast. The injuries usually result from compression of the breast tissue between the bony thorax and the seat belt as the torso decelerates suddenly and shearing stresses incurred by the soft tissues due to rotation of the trunk.
Case Presentation
A 50-year-old overweight woman presented independently with fainting symptoms to the emergency department after a motor vehicle crash. She was the driver and her car was rear-ended by another vehicle with a subsequent frontal collision. At the moment of the accident she was wearing seat-belts and the airbag didn’t open.
When she came at the emergency department, the patient had a systolic blood pressure of 103 mm Hg, a heart rate of 108 beats per minute, normal respiration rates, and no neurological deficit. During clinical examination emerged an extensive bruising in medial quadrants of the right breast along the line of contact with the diagonal portion of the seat belt.
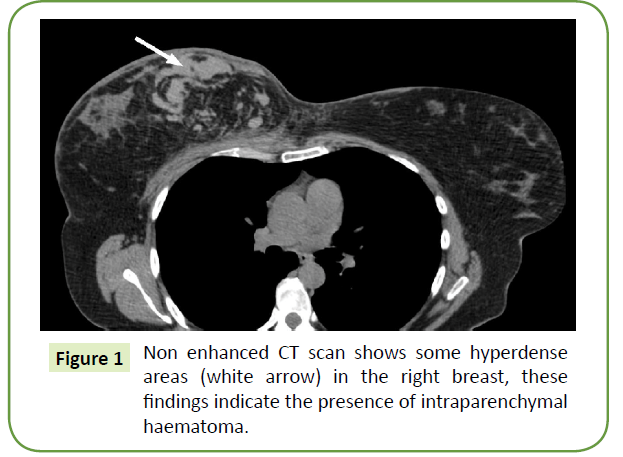
Initial chest radiography, abdominal ultrasonography and cervical spine radiography were normal and showed no bone fracture. Chest CT scan showed a large right breast hematoma (Figure 1). Subsequent hemoglobin measurements confirmed haemodynamic stability. The patient was admitted and monitored.
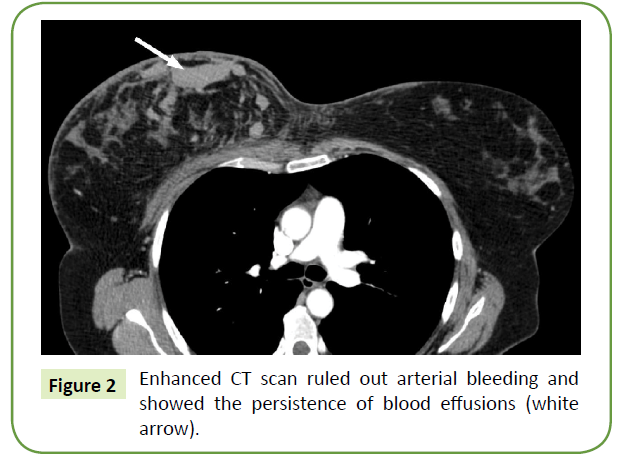
During the hospitalization the patient has been subjected to several blood tests to monitor haemodynamic stability, and to CT scan and breast ultrasound, which did not show any increase in the size of hematoma in the right breast (Figure 2). Contrast CT ruled out arterial extravasation. In the view of the above, a supportive bandage was applied to the breast and the patient got discharged with pain killers and antibiotic therapy at home. The patient was examined a week after with breast ultrasonography and blood test.
At the follow-up six months later, physical examination showed symmetrical breasts and the resolution of the bruising in medial quadrats of the right breast. At the mammography a band like area of increased density that was compatible with the hematoma was identified. The ultrasound check of this area showed a sharp decrease in the size of blood collections previously described, resulting in a 3.3 centimeters area with hyper echoic material in it compatible with clots.
An annual follow-up, inclusive of mammography and breast US, has been recommended for her.
Results
In acute setting the patient was assessed to advanced trauma life support (ATLS) protocols. After ruling out with clinical and radiological data a life-threatening bleeding, our approach with a stable patient aimed to exclude without doubt any active bleeding and to ensure the treatment more suitable for the patient. Comparison between specialists allowed choosing if an endovascular or surgical intervention was needed or not: the stability of the clinical situation and the absence of active arterial extravasation of contrast material depicted by CT favored a conservative management.
Discussion
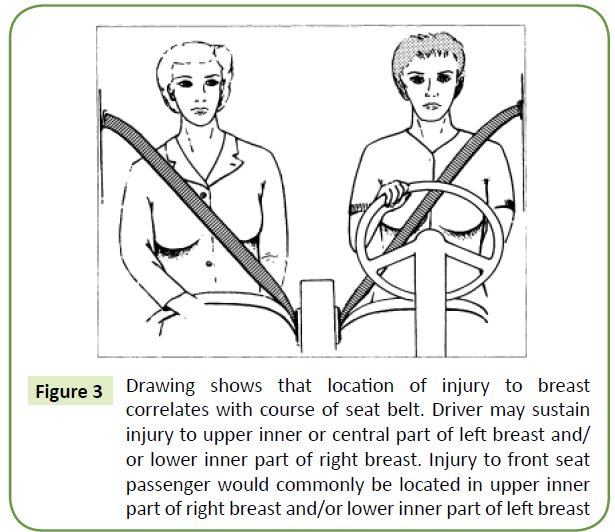
The rapid deceleration of the body against the sash of the seat belt results in compression and shearing of tissues. The soft tissues of the anterior chest are crushed between the seat belt and the bony thorax. This results in a range of injuries from bruising to avulsion of breast tissue [3,4]. The site of injury to the breast correlated with the location of the seat belt, as shown diagrammatically in Figure 3 [5].
Figure 3: Drawing shows that location of injury to breast correlates with course of seat belt. Driver may sustain injury to upper inner or central part of left breast and/ or lower inner part of right breast. Injury to front seat passenger would commonly be located in upper inner part of right breast and/or lower inner part of left breast
The arterial supply to the breast comes from several sources; the internal mammary artery with perforator vessels through the chest wall leads to the medial breast and the lateral thoracic branch of the axillary artery leads to the lateral breast. Shear injuries might cause the perforating vessels rupture. The severity of the previously reported injuries ranges from small hematomas to breast avulsions that require emergency mastectomy to stop bleeding [6].
In 2014 Song and Teo published a systemic review about seatbelt injuries to the female breast, proposing a new four-tier classification for diagnosis and management based on timing to presentation and symptoms (Table 1). They aimed to overcome the limits of the previous classification published by Majesky in 2007, in which a significant number of patients were not easily categorized as late presentation, pregnant women or patients with breast prostheses [7].
Table 1. Teo and Song classficiation: a new diagnosis and management classification for seat-belt injury to the female breast.
| Teo and Song classification | |||
|---|---|---|---|
| Class | Presentation | Definitive investigations | Proposed management |
| 1a | Immediate presentation with bruising and pain of the breast with or without minor wounds. New breast asymmetry for patients with implants in situ. | - CXR in all patients to rule out rib fractures. | - Dress or close wounds. |
| - USS for patients with implants or capsule rupture. | - Capsulotomies and/or implant exchange where indicated. | ||
| - Warn patients of the risk of fat necrosis and possible need for future reconstruction. | |||
| 1b | Immediate presentation with expanding breast. | - CT scan | - Possible causes include arterial extravasation, milk duct injury (in pregnancy) and pneumothorax. |
| - Contrast angiogram to evaluate extravasation. | -Resuscitate patient and angiographic embolization of culprit vessel in arterial extravasation. | ||
| -Aspiration of milk collection in pregnant patients and consider placement of a drain. Consider medical treatment to suppress lactation. | |||
| - Warn patients of the risk of fat necrosis and possible need for future reconstruction. | |||
| 2a | Late presentation with tender breasts, mild bruising or palpable lump. | - Triple assessment (clinical examination, imaging and fine-needle aspiration or core biopsy) | - Oncological treatment if indicated. |
| - Pain management with lump excision may not be effective. | |||
| 2b | Late presentation with structural distortion (breast cleft or capsule contracture). | - Triple assessment | - Oncological treatment if indicated. |
| - MRI to assess implant status | - Reconstruct affected breast and consider contralateral reduction. | ||
| - Capsulectomy and/or implant exchange if indicated. | |||
In this specific case the MRI has not been used, MRI is used to second level method of in the study of the pathological mammary [8-10]. In our case, trauma is verified during the night hours and we must saw the thoracic situation of the patient with thoracic CT.
Clinical late presentations following seat belt injury may include tender breasts, mild bruising and palpable lump in the line of seat-belt trauma or breast distortion due to fat necrosis or cleft deformity. Fat necrosis is defined as a palpable, discrete, and persistent subcutaneous firmness that measures at least 1 cm during physical examination [11] and it is a consequence of breast trauma in 21-70% of cases [12]. Although it is considered a benign condition, it can mimic breast cancer clinically or radiologically, and in other cases it can obscure malignant lesions [13]. There are insufficient data to predict if, how or when necrosis or a cleft deformity fats would develop. Factors that may be implicated include accident severity, motor vehicle safety rating, breast size and airbag employment [7], therefore Song and Teo recommend informing all patients about the potential risk of developing fat necrosis or a cleft deformity in the affected breast.
Moreover, in view of the variety of clinical and radiological findings of presentation, a follow-up of blunt traumatic lesions of the breast supported in literature [1,14] suggests that all patients undergo a physical breast examination and baseline mammography at 3-6 months post-injury, with annual mammography’s thereafter. The manifestations of breast trauma (especially fat necrosis) are often suspicious of carcinoma on clinical and imaging grounds, with areas of calcification commonly seen in both. This highlights the importance of triple assessment with clinical examination, imaging and histological investigation in patients who present with a post-traumatic breast mass, despite the clear history of trauma [7].
Conclusion
This case shows how a multidisciplinary approach may improve the possibility of a correct management, as well as breast cancer, also in uncommon circumstances like seat-belt trauma to the female breast.
References
- Gavriilidou O, Papazoglou LG, Kouki M, Strantzia E Giannouli M, et al. (2015) Axial pattern skin flaps in cats: 8 cases (2000-2015). J Hellenic Vet Med Soc.
- Grigoropoulou VA, Prassinos NN, Papazoglou LG, Galatos AD, Pourlis AF (2013) Scrotal flap for closure of perineal skin defects in dogs. Vet Surg 42: 186-191.
- Field EJ, Kelly G, Pleuvry D, Demetriou J, Baines SJ (2015) Indications, outcome and complications with axial pattern skin flaps in dogs and cats: 73 cases. J Small Anim Pract 56: 698-706.
- Kokkinos P, Kouki M, Montzolis G, Savvas I, Delligiani A, et al. (2017) Lateral caudal axial pattern flap for coverage of a dorsal pelvic and perineal skin defect in a cat. Aust Vet Pract 47: 15-18.
- Mentzikof L. Kambouri P, Kariki A, Papazoglou LG (2017) Mesh skin grafting in the dog and cat. Indications, pathophysiology, surgical technique and complications. Hellenic J Comp Anim Med 6: 51-67.
- Tsioli V, Papazoglou LG, Papaioannou N (2009) A review of the use of skin stretchers for closing skin defects and its application to small animal cases. Aust Vet Pract 39: 112-119.
- Tsioli V, Papazoglou LG, Papaioannou N, Psalla D, Savvas I, et al. (2015) Comparison of three skin-stretching devices for closing skin defects on the limbs of dogs. J Vet Sci 16: 99-106.
- Papazoglou LG (2016) Elucidation of a therapeutic paradigm shift found on Kuhn’s structure of scientific revolutions: The story of canine external ear canal surgery. Int J Hist Phil Med 6: 1-4.
- Riggs J, Jennings JL, Friend EJ, Halfacree Z, Nelissen P, et al. (2015) Outcome of full-thickness skin grafts used to close skin defects involving the distal aspects of the limbs in cats and dogs: 52 cases (2005-2012). J Am Vet Med Assoc 247: 1042-1047.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences