Management Solid Pseudopapillary Neoplasm of the Pancreas
Dr. Mahrukh Rehman*
Department of Surgical Gastroenterology and Liver Transplantation, United Kingdom
- *Corresponding Author:
- Dr. Mahrukh RehmanDepartment of Surgical Gastroenterology and Liver Transplantation, United Kingdom; Tel: 07806747279 ; E-mail: kmahrukh3710@gmail.com
Received Date: September 30, 2020; Accepted date: August 21, 202; Published date: August 31, 2021
Citation: Mahrukh Rehman (2021) Management Solid Pseudopapillary Neoplasm of the Pancreas Gen Surg Rep 5:1
Abstract
Solid pseudopapillary neoplasm (SPN) of the pancreas is a rare tumor with low malignant potential. SPN accounts for approximately 1% to 2% of all pancreatic neoplasms. Most of the patients are young women. It is generally located in the body and tail of the pancreas. Most of the cases are asymptomatic and are usually diagnosed during incidental examinations. Neoplasms have a low malignant potential and the reported incidence of malignant transformation is approximately 15%. Metastasis or local invasion are the most important criteria for malignant transformation. Radical resection of the tumor provides long-term survival. There is no clear recommendation in the literature regarding the resection of the primary neoplasm and the management of its metastasis, if any. The aim of this study is to evaluate the diagnostic approach and treatment options of pancreatic SPN disease.
Background
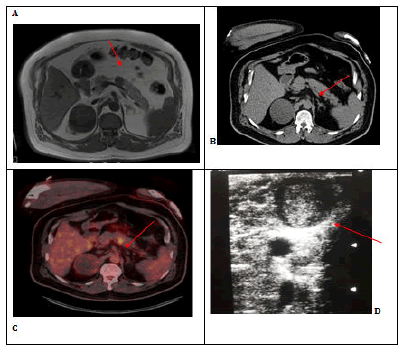
56-year-old male patient presented with complaints of abdominal pain and nausea. On examination, there was mild tenderness in the epigastric region. Laboratory tests revealed increased urea and creatine. MRI, a well-circumscribed nodular lesion enhancing late period and thought to show mild diffusion restriction, located just to the left of the midline at the level of the pancreatic corpus and reached a diameter of approximately 20 mm, PET CT was planned for the patient. On PET CT (Figure 1B, C), a nodular hypodense lesion, approximately 2 cm in size, showing increased FDG activity (SUVmax: 11.01) at the level of the pancreatic corpus was detected. Surgical decision was made for the lesion in the pancreas. Tumor markers of the patient were, Ca 19.9: 24.7 U / mL (N: 0-35 U / ml), CEA: 7.09 ng / ml (N: 0-7 ng / ml).
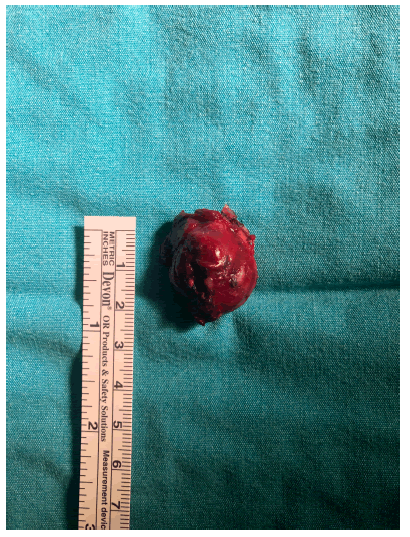
On exploration, the lesion in the pancreatic body was palpated and confirmed by peroperative USG (Figure 1D). It was excised with the enucleation technique (Figure 2). Pathology result was reported as 2.2x2.7x2 cm solid pseudopapillary neoplasia (Figure 3). The patient was discharged on the 4th postoperative day without any complications.
Figure 1: A:Dynamic MR: T1W hypointense, T2W heterogeneous-slightly hyperintense nodular lesion. B: CT imaging C: PETCT,increased FDG activity (SUVmax: 11.01). D: well-circumscribed 35x28 mm lesion was detected on peroperative USG. Research Article iMedPub Journals www.imedpub.com General Surgery Reports Vol.5 No.1:6289 2021 ©
Dıscussıon
Solid pseudopapillary neoplasm (SPN) of the pancreas was first reported by Frantz in 1959. Since the first definition of SPN in the literature, according to its varying components, "papillary cystic neoplasm", "solid and papillary epithelial neoplasm", "papillary and solid neoplasm", "papillary and cystic tumor", "solid and cystic papillary epithelial neoplasm" and Frantz Various names have been used such as tumor. The world health organization recently named this tumor as solid pseudopapillary tumor of the pancreas in 1996 [1, 2].
Solid pseudopapillary neoplasms comprise approximately 1% to 2% of all pancreatic neoplasms and 6% of exocrine pancreatic tumors [3]. 90% of the patients are young women in the 2nd and 3rd decades [4].The origin of solid pseudopapillary tumors is uncertain. SPN can originate from multidirectional primordial cells, ductal cells, acinar cells, endocrine cells or extrapancreatic cells [5].
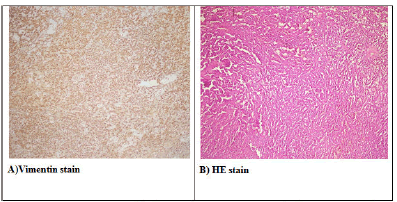
Microscopically, the tumor consists of solid areas, pseudopapillary structures and cystic cavities. Mitosis is rarely seen in tumor cells. Tumor markers; ß-catenin, cyclin D1 and D3 are vimentin, antitrypsin, NSE and progesterone receptors. These immunohistochemical markers do not correlate with malignancy potential. In our patient; The ß-catenin, vimentin, antitrypsin, and progesterone receptors were found to be positive and the KI 67 index was less than 1%.
The differential diagnosis includes mucinous cystic neoplasm, nonfunctional islet cell tumor, microcystic adenoma, pancreatic adenocarcinoma, pancreaticoblastoma, cystic degeneration of solid tumor and calcified hemorrhagic pseudocyst [5]. Neoplasms have a low malignant potential and the reported incidence of malignant transformation is around 15% [6].The most accepted criteria for malignant transformation are metastasis or local invasion. Tumor diameter over 5 cm is also significant for malignant potential. In our patient, the tumor was 2 cm in diameter and there was no local invasion or metastasis.
Radical resection of malignant SPN provides long-term survival. Post-surgery recurrence rate is very low and it has been reported as 3-7% [7]. Local invasion, metastasis and recurrence are not contraindications for surgery.
Contrast-enhanced CT scanning is the most commonly used imaging method in the diagnosis of these neoplasms. They are seen as large-sized solid masses with a typical appearance on CT, which can be clearly distinguished from the adjacent pancreas, with peripheral solid, central necrosis and areas of cystic degeneration in varying degrees due to intra-tumor bleeding [8, 9]. In magnetic resonance imaging (MRI), the hemorrhagic component of the lesions can be visualized much beter. The lesion is larger than 5 cm, the cyst wall is thicker than 3 mm, the detection of intramural nodules, solid-cystic bleeding and necrosis areas are the findings that increase the malignancy potential [10]. In our patient, the size of the lesion was 2x2 cm in size, and there were no findings that increased the potential for other malignancies.
The reported SUV max values of primary SPN ranged from 2.6 to 16.2.Nakagohri et al. reported that four of 5 SPN tumors with intense FDG uptake had signs of malignant potential, such as microscopic or venous tumor invasion [11, 12]. In our patient, PET CT was reported as a nodular hypodense lesion with a size of 2 cm showing increased FDG activity (SUV max: 11.01).
In a study by Castro et al. a definite diagnosis of SPN was reached with percutaneous FNAB in two out of three patients. In the study of Bardales et al. this rate is one sixth [13]. Therefore, fine needle aspiration cytology may be helpful in making the diagnosis, but is not usually necessary. 5-year survival is reported to be between 95-98% .
Complete surgical excision is curative in more than 95% of patients with SPN limited to the pancreas. In locally advanced cases, resection of the involved organs with a 1 cm intact surgical margin is sufficient. Some studies suggest more limited surgery in the form of enucleation rather than radical surgery in small lesions. For larger lesions, the type of surgical resection depends on their location. Lesions on the head of the pancreas are treated with a pancreatoduodenectomy (Whipple procedure), while those on the trunk and tail are best treated with a distal pancreatectomy.
The incidence of lymph node metastasis is extremely rare. In the study by Mao et al in which 292 SPNs were reviewed, 43 of the cases (15%) were reported as malignant, and lymph nodes were involved in only five of them (2%) [14].A formal lymph node dissection was not planned in our patient.
In our patient, enucleation technique was used to avoid complications of radical surgery and to prevent long-term hospitalization. In a series of 3 cases we previously operated, patients who underwent laparoscopic distal pancreatectomy, distal subtotal pancreatectomy and whipple procedure, had a hospital stay of 8, 9, 19 days, respectively. This patient was discharged on the 4th day without any complications.
Conclusion
PPPD (pylorus preserving pancreatoduodenectomy), whipple procedure and distal pancreatectomy in the tail are the most commonly used surgical methods in lesions compatible with SPN in the preoperative evaluation of the pancreas. In lesions compatible with small sized SPN in the pancreatic body in selected patients in experienced centers; corpus resection or enucleation can be performed with low complications and high surgical success rates. In this way, the number of days of hospitalization and treatment costs can be reduced.
References
- Castro SMM, Singhal D, Aronson DC (2007) Management of Solid-pseudopapillary Neoplasms of the Pancreas: a Comparison with Standard Pancreatic Neoplasms. World J Surg. 31: 1129–1134.
- Coleman KM, Doherty MC and Bigler SA (2003) Solid pseudopapillary tumor of the pancreas. Radiographics. 23:1644–48.
- Martin RC, Klimstra DS, Brennan MF, et al. (2002) Solid-pseudopapillary tumor of the pancreas: a surgical enigma? Ann Surg Oncol. 9: 35–40.
- Mao C, Guvendi M, Domenico DR (1995) Papillary cystic and solid tumors of the pancreas: a pancreatic embryonic tumor? Studies of three cases and cumulative review of the world’s literature Surgery 118:821–828.
- Huang HL, Shih SC, Chang WH, et al. (2005) Solid-pseudopapillary tumor of the pancreas: clinical experience and literature review World J Gastroenterol 11: 1403–1409.
- Tipton SG, Smyrk TC, Sarr MG, et al. (2006) Malignant potential of solid pseudopapillary neoplasm of the pancreas. Br J Surg 93: 733–737.
- Adams AL, Siegal GP, Jhala NC (2008) Solid pseudopapil¬lary tumor of the pancreas: a review of salient clini¬cal and pathologic features Adv Anat Pathol 15: 39-45.
- Poustchi-Amin M, Leonidas JC, Valderrama E, et al. (1995) Papillary-cystic neoplasm of the pancreas Pediatr Radiol 25: 509–511.
- Anil G, Zhang J, Al Hamar NE, Nga ME et al. (2017) Solid pseudopapillary neoplasm of the pancreas: CT ima¬ging features and radiologic-pathologic correlation Diagn Interv Radiol 23: 94-9.
- Cantisani V, Mortele KJ, Levy A, et al. (2003) MR imaging features of solid pseudopapillary tumor of the pancreas in adult and pediatric patients AJR Am J Roentgenol 181:395– 401.
- Kim YI, Kim SK, Paeng JC, Lee HY et al. (2014) Comparison of 18F-FDG PET/CT findings between pancreatic solidpseudopapillary tumor and pancreatic ductal adenocarcinoma. Eur JRadiol 83 (1) 231-235.
- Bardales RH, Centeno B, Mallery JS, et al. (2004) Endoscopic ultrasound-guided fine-needle aspiration cytology diagnosis of solid-pseudopapillary tumor of the pancreas: a rare neoplasm of elusive origin but characteristic cytomorphologic features Am J Clin Pathol 121:654–662.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences