Editorial Announcement
Nirupama Moran1*, Diptesh Bandyopadhyay1
Junior consultant, Central hospital Kalla, Eastern coal fields ,Department of Otorhinolaryngology, West Bengal, India
- *Corresponding Author:
- Dr. Nirupama MoranCentral hospital Kalla, Eastern coal fields ,Department of Otorhinolaryngology, West Bengal, India, Tel: 9800129396; E-mail: nirupamamoran50@gmail.com
Received Date: August 11, 2020; Accepted date: August 18, 2021; Published date: August 30, 2021
Citation: Moran N (2021) An Observational Study of Management of Traumatic Perforation of Tympanic Membrane. Gen Surg Rep Vol.5 No.1.
Abstract
Background and objectives
Traumatic perforation of tympanic membrane is a very common finding in ear trauma. This can occur in while fighting, household violence, abuse, slapping, road traffic accidents etc.Proper note of condition of tympanic membrane should be kept as this is a grievous hurt (Indian Penal Code 320).Symptoms of traumatic perforation of tympanic membranes are Pain (which usually subsides within 1-2 days) Decreased hearing (improves as tympanic membrane heals if there is no ossicular disruption) Tinnitus, Bleeding from ears etc. Generally prognosis of traumatic perforation of tympanic membrane where there is no occicular disruption is very good. Our Study was to compare the outcomes of treatment modality of traumatic perforation of tympanic membranes where (Group A) one group with wait and watch technique and another (Group B) group with where patients were given combination ear drop (ofloxacin+clotrimazole +dexamethazone + lignocaine).
Materials and Method
A prospective and observational study was undertaken from October 2017 to October 2019. It was conducted in the department of Otorhinolaryngology, Kalla Central Hospital, Eastern Coal Field, Asansol, and West Bengal India.
Result
The total numbers of cases were 50.Average patients age group were 15-52. The numbers of male patients were 27 and female 23. Follow up of cases were done on 3th day ,20th day, 40th day and 60thh day of first visit. Group a patients where we adopted wait and watch method on 20th days of follow-ups 28 %( 7/25 ) patients perforations healed completely, 60% (15/25) healed on 40th day and rest 12 %( 3/25) were not healed on 60th days follow-ups. On the other hand group B patients where we were using combination ear drop (Ofloxacin +Clotrimazole +Dexamethazone + Lignocaine)28% (7/25) completely healed on 20thdays of follow-ups, 64 %(16/25) healed on 40thday and 8% (2/25) failed to heal on 60thday.So,overall success rate on group A was 88% (22/25),whereas group B was92%(23/25). Minimal difference in outcome in 2 groups was noted.
Conclusion
Addition of ear drops does not change prognosis of traumaticear drum perforation .Antibiotic, antifungal drops can be given to prevent infection further more for patient satisfaction but this does not change natural course of disease process.
Keywords
Traumatic Perforation, Tympanic Membrane. Tinnitus
Introduction
The ear is located within the cranio-facial skeleton which is exposed to environmental trauma that can occur as blunt injuries like contusion, concussion, decompression and penetrating injuries or fractures1.The incidence of middle ear trauma is more than the inner ear, which is estimated 6.8 per 1000 person2 .Traumatic perforation of tympanic membrane is a very common finding in ear trauma. It is a delicate translucent pearly white membrane which separates the external from the middle ear and when it is traumatized it produces a rupture, tear or perforation.The TM functions is to aid in hearing by vibrations whenever struck by sound waves and transmitting those vibrations to the inner ear3 .The TM injury can predispose to middle ear infection which has grave consequences including facial nerve paralysis, formation of cholesteatoma,perilymph fistula, intracranial infections and may require an intracranial exploration4. Symptoms and signs of a ruptured tympanic membrane may include otalgia,hearing loss, tinnitus, spinning sensation, mucous like,pus-filled or bloody drainage from the ear.Adegbiji WA et al showed that the most common presenting symptom was otorrhea(81.5%), followed by otalgia(72.8%) and Tinnitus5.Patients with tympanic membrane perforations(TMP) based on history of trauma to the ear and otoscopic examinations .Definite diagnosis for occult TM rupture would require otomicroscopy or middle ear impedance studies, performed on an outpatient basis6.Otoscope fogging may also be used as an indicator for perforation, as warm humidified air is connecting from the nasopharynx into the middle ear and communicating to the EAC (External auditory canal) via the perforation, leading to condensation on the otoscope7.Most of isolated traumatic perforations of the tympanic membrane can be managed with conservative care.The ear should be kept clean and dry while the TM heals; insertion of vaseline impregnated cotton ball into the ear when bathing, avoid nose blowing, as the pressure created when blowing the nose can damage healing TM tissue and causes infection8. . Our Study was to compare the outcomes of treatment modality of traumatic perforation of tympanic membranes where (Group A) one group with wait and watch technique and another (Group B) group with where patients were given combination ear drop(Ofloxacin +Clotrimazole +Dexamethazone +Lignocaine).
Materials and Method
A prospective and observational study was undertaken from October 2017 to October 2019. It was conducted in the department of Otorhinolaryngology, Kalla Central Hospital, Eastern Coal Field, Asansol, and West Bengal India. Details of history and clinical examinations findings were recorded. Only device used in this study was Otoscope and Audiometer (Figure 1).
The patients were also subjected to pure tone audiometry (PTA). Pure- tone audiometric testing was performed at the initial and final visits after treatment.The pure-tone averages were determined for air and bone conduction at 500, 1000, 2000 and 4000 Hz. Age, sex, duration of injury, cause of injury, size of TMP and presence or absence of otorrhea was recorded at the time of each hospital visit. Patients were randomly chosen. The total numbers of cases were 50. The numbers of male patients were 27 and female 23.The patients were divided into two groups. Group A-25 patients were given no treatment (wait and watch) Group B-25 patients were given combination ear drop (Oofloxacin+Clotrimazole +Dexamethazone + Lignocaine). Patients were not aware that they were in group A or group B.Inclusion criteria’s were age group between 15-55 years irrespective sexes with good general conditions, central perforation of the pars tensa of the tympanic membrane with history of trauma less than 48 hours. Exclusion criteria’s were Pus in ear, Patients with other known co morbidity like Diabetes Mellitus,Hypertension,Immunosupression, Patients who did not report regularly and Hearing loss in pure tone audiometry( PTA) more than 35 decibel (db). Group A patients where we adopted wait and watch method so no treatment given where as Group B the patient external auditory canal (EAC) was cleaned with a cotton bud soaked in Povidone –iodine solution .But the perforation edges were neither approximated nor scaffolding material was used. Instead we used 2-3 drops of (Ofloxacin+Clotrimazole +Dexamethazone + Lignocaine) solution was applied by self ( patient) or attendants to the remnant of membrane thrice daily; the perforated ear was angled upward for at least 10 minutes to insure that the remnant membrane remained moist. In the first follow-up on day 3th of the first visit any inappropriate patient technique was corrected (neither dry nor overly wet) Thereafter follow up was scheduled on 20th day, 40th day and 60thh day of first visit. Patients were advised to reduce the number of ear drops and take oral antibiotics if there is any infection. Data were grouped and analyzed by standard statistical method.
Result and Observations
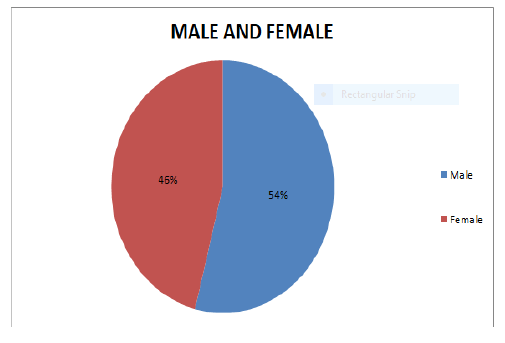
Out of 50 cases, 27(54%) cases were male and 23 cases were female (46%) (Figure 2).
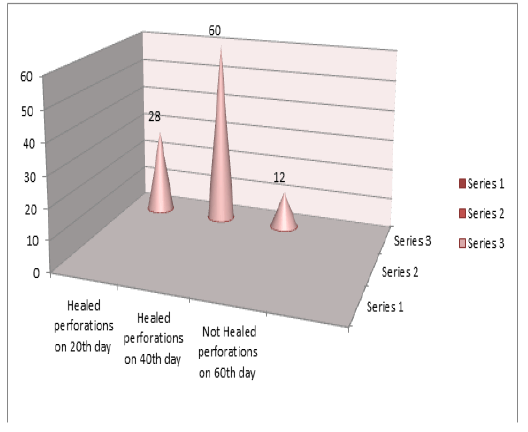
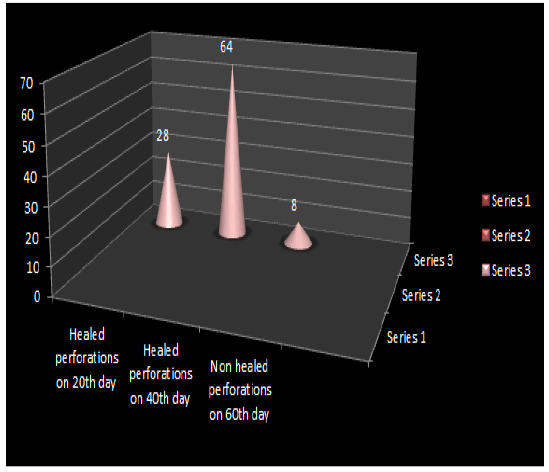
Follow up of cases were done on 3th, 20th day, 40th day and 60th day of first visit. Closure of tympanic membrane was noted down according to their follow up days(Table 1).Group A patients where we adopted wait and watch method on 20th days of follow- ups found 28 %( 7/25) patients perforations healed completely, 60% (15/25) healed on 40th day and rest 12 %( 3/25) were not healed on 60th days of follow-ups( Figure 3). On the other hand group B patients where we were using combination ear drop (Ofloxacin+Clotrimazole +Dexamethazone + Lignocaine) 28% (7/25) completely healed on 20thdays of follow-ups, 64 %(16/25) healed on 40thday and 8% (2/25) failed to heal on 60thday(Figure 4).So, overall closure (Tympanic membrane) success rate on group A was 88% (22/25), whereas group B was 92%(23/25). No treatment- related complications such as vertigo, otomycosis were observed. Only the 7 patients complained ear ache in the spontaneous healing group. Mean hearing improvement at final visits after treatment were 13±2.5 dB for the ear drop group whereas 12.8±3 Db for the spontaneous healing group. Differences in hearing improvement rates among the two groups were not statistically significant.
| GROUP | TOTAL PATIENTS | HEALED PERFORATION ON 20TH DAY | HEALED PERFORATION ON 40TH DAY | NOT HEALED PERFORATION AFTER 60TH DAY |
| GROUP A | 25 | 28 %(7/25) | 60% (15/25) | 12%( 3/25) |
| GROUP B | 25 | 28% (7/25) | 64 %(16/25) | 8% (2/25) |
Table 1: Showing comparison of closure rate in both group A and B.
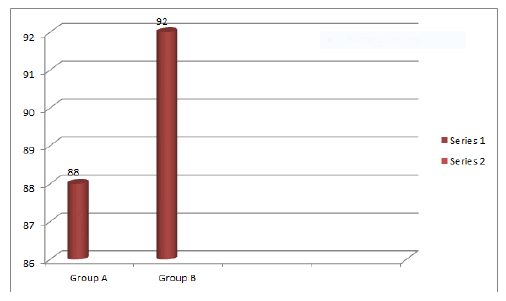
At the 60th of follow-up, successful closure of the tympanic membrane was achieved in 22 (88%) in case of group A and 23 out of 25 cases (92%) in the group B (Figure-5).
Discussion
Traumatic tympanic membrane (TTM) is an injury of the ear drum, which is frequently faced by Otorhinolaryngologists worldwide. Most of the cases of TTM heal spontaneously within 4 weeks9.Although TTM is a common entity in otology outdoor clinics, still there is debate regarding its optimal treatment. Some groups prefer spontaneous healing in cases of TTM.However, large TTMs have a lower rate of spontaneous healing and require longer healing times10.In our study we found 88% closure rate in the spontaneous healing group on the other hand 92% in the topical ear drop group in 60 days of follow -up. Lou et al reported closure rate of 80% in large perforations over a 12 month follow-up period11.Ott MC et al reported a spontaneous healing rate of 67.5%(27/40);the time to closure was more than 3 months in 7 of these 27 patients12. Others have suggested that to keep the EAC dry and avoid use of antibiotics ear drops12,13,14. Park MK et al reported that biological materials have not been widely used because of expense and inconvenience15.While Ofloxacin otic solution is safe and use for the treatment of inflammatory diseases. Recent clinical and experimental studies have suggested that gelatine sponge and ofloxacin otic solution aid in eardrum healing16,17,18,19.However, it remains unclear which treatment is more suitable for traumatic tympanic membrane perforation. In our study closure rate was bit higher in the topical ear drops(92%) group than the wait and watch group(88%) but it is not significantly high . .We assess TTM closure by Otoscope when patient visited at our clinics for follow-ups. Usually reported that disappearance or improvement of symptoms when the perforation heals. However, although the patients reported disappearance of symptoms sometimes remnant of perforations are seen by otoscope.
The limitations of our study were Size of perforation on day 1 of visit, Age and sex of patient was not taken in consideration and average healing time in both groups could not be calculated .All patients are not equally vigilant in maintaining dry ear especially during rains. This surely affects prognosis.
Conclusion
Although it had been noticed that Ofloxacin ear drops group showing marginal higher success rate than the spontaneous healing group but it was not significant. So, addition of ear drops does not change prognosis of traumatic tympanic membrane perforation. Antibiotic, antifungal drops can be given to prevent infection further more for patient satisfaction but this does not change natural course of disease process. Tricarboxylic acid cycle (TCA) cautery, surgery can be done where conservative treatment has failed.
References
- Guenzani S, Merue D, Messersmith M, Olivary D, Arena M, Spano A (2016) Inner ear decompression sickness in nine trimix recreational divers. Diving Hyperb Med 46: 111-116.
- Neuenschwander MC, Deutsch ES, Cornetta A, Willcox TO (2005) Penetrating middle ear trauma: a report of 2 cases. Ear Nose Throat J 84: 32-35.
- Lim DJ (1995) Structure and function of the tympanic membrane:a review Acta Otorhinolaryngol Belg 49(2): 101-15.
- Francis B (2002) Trauma to the middle and inner ear: Grands Round presentation, UTMB,Dept of Otolaryngology.
- Adegbiji WA, Olajide GT, Olajuyin OA, Olatoke F, Nwawolo CC (2018) Pattern of tympanic membrane perforation in a tertiary hospital in Nigeria. Niger J.Clin Pract 21(8): 1044-1049.
- Chen F, Yang XP, Lieu X,Dong DA,Zhou XR,Fan LH (2018) Retrospective Analysis of 24 cases of forensic Medical identification on traumatic tympanic membrane perforations.Fa Yi Xue Zhi 34(4): 392-395.
- Naylor JF (2014) Otoscope fogging: examination finding for perforated tympanic membrane. BMJ case Rep 30.
- Carol A, Turkington (2002) Perforated ear drum Health Article.Gale Encyclopedia of Medicine.
- Pusp MD, Robitschek J (2017) Traumatic hearing loss in the context of blast-related tympanic membrane perforation.Mil Med 182(1): 1645-1648.
- Xiuguo Li, Hui Zhang, Yuanyuan Zhang (2020) Repair of large tympanic membrane perforation using ofloxacin otic solution and gelatine sponge. Braz J of Otorhinolaryngol.
- Z.C.Lou YM, Tang J, Yang (2011) A prospective study evaluating spontaneous healing of aetiology,size and type-different groups of traumatic tympanic membrane perforation; Clin Otolaryngol 36: 450-460.
- Ott MC, Lundy LB (2001) Tympanic membrane perforation in adults. How to manage,when to refer. Postgrad Med 110: 81-4.
- Griffin WJ (1979) A prospective study of traumatic tympanic membrane perforations in a clinical practice. Laryngoscope 89: 261-282.
- Grant JR, Arganbright J, Friedland DR (2008) Outcomes for conservative management of traumatic conductive hearing loss. Otol Neurotol 29: 344-349.
- Park MK, Kim KH, Lee JD, Lee BD (2001) Repair of large traumatic tympanic perforation with a steri-strips patch. Oto-laryngol Head Neck Surg 145: 581-5.
- Lou Z-C, He J-G (2011) A randomised controlled trial comparing spontaneous healing, gelfoam patch and edge-approximation plus gelfoam patch in traumatic tympanic membrane perforation with inverted or everted edges. Clin Otolaryngol 36: 221-6.
- Lou ZC, Tang YM, Chen HY, Xiao J (2015) The perforation margin phenotypes and clinical outcome of traumatic tympanic membrane perforation with a gelfoam patch: our experience from a retrospective study of seventy-four patients. Clin Otolaryngol 40: 389-92.
- Lou ZC,Lou ZH,Liu YC,Chang J.Healing human moderate and large traumatic tympanic membrane perforations using basic fibroblast growth,0.3% Ofloxacin eardrops and gelfoam patching.Otol Neurotol.2016;37:735-41.
- Lou Z, Lou Z,Tang Y,Xiao J.The effect of Ofloxacin otic drops on the regeneration of human traumatic tympanic membrane perforations. Clin Otolaryngol. 2016; 41:564-70.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences