ISSN : 2348-9502
American Journal of Ethnomedicine
Ayurvedic Influences and Novel Combination of Phytotherapy and Zootherapy by a Folk Medicinal Practitioner of Domar Upazila in Nilphamari District, Bangladesh
Samsun Nahar1, Be-nazir Farzana2, Rownak Jahan2, Taufiq Rahman3, Md Shahadat Hossan4, Christophe Wiart5 and Mohammed Rahmatullah1*
1Department of Pharmacy, University of Development Alternative, Lalmatia, Dhaka-1207, Bangladesh
2Department of Biotechnology and Genetic Engineering, University of Development Alternative, Lalmatia, Dhaka-1207, Bangladesh
3Department of Pharmacology, Tennis Court Road, CB2 1PD, Cambridge, UK
4School of Pharmacy, University of Nottingham, UK
5School of Pharmacy, University of Nottingham Malaysia Campus, Semenyih, Malaysia
- *Corresponding Author:
- Rahmatullah M
Faculty of Life Sciences
University of Development Alternative
Lalmatia, Dhaka-1207, Bangladesh
Tel: +88-01715032621
Fax: +88-02-8157339
E-mail: rahamatm@hotmail.com
Received Date: November 02, 2017; Accepted Date: November 22, 2017; Published Date: November 30, 2017
Citation: Nahar S, Farzana B, Jahan R, Rahman T, Md Hossan S, et al. (2017) Ayurvedic Influences and Novel Combination of Phytotherapy and Zootherapy by a Folk Medicinal Practitioner of Domar Upazila in Nilphamari District, Bangladesh. Am J Ethnomed Vol.4 No.2:17
Abstract
Background: Bangladesh is possibly unique in that many different traditional medicinal systems are present like Ayurveda, Unani, homeopathy, and folk medicine. The objective of the present study was to document the novel therapeutic practices of a folk medicinal practitioner (FMP) in Nilphamari district, who used a combination of phytotherapy and zootherapy practices, and whose formulations further included his own modifications of standard Ayurvedic formulations.
Methods and findings: Interviews of the FMP regarding his ethnomedicinal practices were carried out with the help of a semi-structured questionnaire and the guided field-walk method from August 2016 till February 2017. The FMP used a total of 44 plants distributed into 29 families in his formulations. The total number of formulations used was 25 for treatment of a diverse group of ailments like respiratory tract disorders, eye disorders, filariasis, diabetes, weakening of immune system, erectile dysfunction, hypertension, tuberculosis, heart disorders, puerperal fever, and jaundice. The FMP also used parts from seven animals (fish, insect, bird – all are classified as animal) alone or in conjunction with plants in his treatment. Conclusions: The FMP used a number of plants in his treatment, the ethnomedicinal uses of which plants being hitherto not reported from Bangladesh. The combination of phytotherapy and zootherapy is unique as well as modifications of Ayurvedic formulations, and if scientifically validated, may prove useful for treatment of a number of diseases. Overall, the FMP’s treatment methods merit further scientific attention especially towards development of an effective method to treat diabetes, hypertension, and filariasis.
Keywords
Phytotherapy; Zootherapy; Folk medicine; Ayurveda; Nilphamari; Bangladesh
Introduction
It is very possible that human beings have been afflicted with diseases of some sort or other since their very advent. It has been suggested from genetic evidence that many tropical diseases of human beings may have originated during Paleolithic times or before, that is even as early as 2.5 million years ago when our early human ancestors were still isolated in Africa [1]. Whether human beings knew how to treat themselves after occurrence of diseases during Paleolithic times is not known with certainty; however, the great apes and other animals have been reported to self-medicate following diseases [2], which makes it a possibility that human beings also treated themselves during diseases. It has been reported that human beings became aware or were already aware of the medicinal properties of plants somewhat around 5,000 years ago [3]. Since then, plants have been and still are excellent sources for the discovery of many modern allopathic drugs, and many modern drugs have been discovered through close observations of indigenous or traditional medicinal practices [4].
The need for new drugs has become really acute in present times. There has been an emergence of new infectious diseases like AIDS, Ebola, Hanta, Zica, MERS to name only a few, and which details have been reviewed by the World Health Organization (WHO) [5]. In addition, there has been emergence of antibioticresistant bacteria and drug-resistant vectors [6,7]. Plants can form the first line of resource in discovering novel and efficacious drugs against these threats of new diseases as well as drugresistant diseases.
Bangladesh can be regarded as a hot spot for traditional medicinal systems. Some of the oldest and established traditional medicinal practices present in the country with their own training institutions and registered practitioners include Ayurveda, Unani and homeopathy [8]. The various tribes have their tribal medicinal practitioners, who use mostly medicinal plants but may also include rituals, amulets and zootherapy in their practices [9-12]. There are religious healers, whose practice method deals with amulets and incantations [13]. There are folk medicinal practitioners (FMPs), who can possess quite detailed and accurate knowledge on the healing properties of plants [14-17]. The other interesting part about FMPs in Bangladesh is that although Bangladesh is a small country, the FMPs differ remarkably in the selection of plant(s) to treat any given disease even within adjoining villages [18].
As such, documentation of the practices of FMPs of Bangladesh can be a rich source of knowledge on the medicinal properties of plants and their therapeutic uses. Since a relatively fewer number of FMPs combine phytotherapy with zootherapy and/or other inanimate ingredients, their use of various items for treatment of diseases can provide an extra dimension to traditional medicinal knowledge. The objective of the present study was to document the practices of a FMP at Paschim Boragari village, Domar Upazila (sub-district) in Nilphamari district, Bangladesh who was selected because of his novel combinations of phytotherapy and zootherapy in his folk medicinal practice, use of previously unreported medicinal plants, and use of Ayurvedic formulations with his own innovative modifications.
Materials and Methods
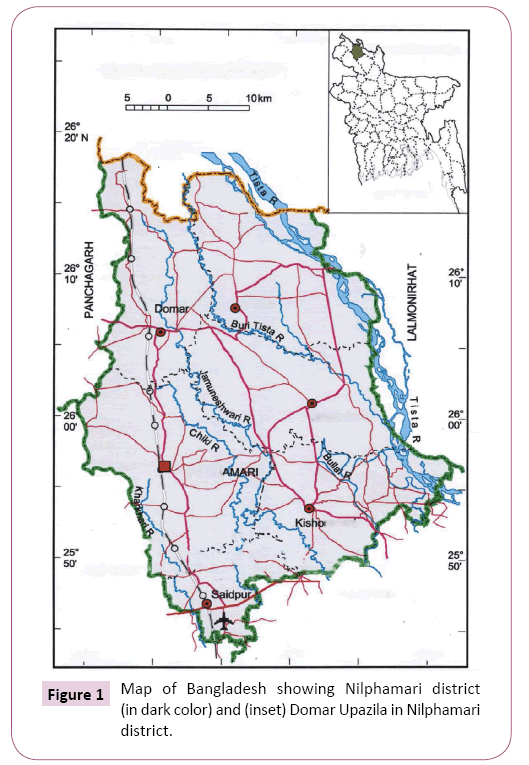
Nilphamari district is in northern Bangladesh. The area of the district is 1580.85 sq km, and is located in between 25°44' and 26°19' north latitudes and in between 88°44' and 89°12' east longitudes (Figure 1). It is bounded by West Bengal state of India on the north, Rangpur district on the south, Lalmonirhat district on the east, Panchagarh and Dinajpur districts on the west. Domar Upazila has an area of 250.84 sq km and is one of the six Upazilas of the district. There are 47 villages in Domar Upazila with a combined population of 215699.
The FMP (initials RI, male, age 50 years) resided in Paschim Boragari village in Domar Upazila. A number of visits were made to the FMP by the authors (but most frequently SN) between August 2016 and February 2017 to interview the FMP, collect plant specimens and gather accurate information on the animal parts used in his formulations. Prior Informed Consent was obtained from the FMP to disseminate any information obtained. At the same time, the villagers were randomly queried as to whether they have at least once visited the FMP for treatment, and regarding the success of the FMP’s formulations in treatment of diseases.
Actual interviews of the FMP were conducted with the help of a semi-structured questionnaire and the guided field-walk method of Martin [19] and Maundu [20]. The FMP was further queried with the help of the semi-structured questionnaire as to plants, animals, and formulations used, disease(s) treated, source and mode of collection and preservation of plants, season of collecting, preparation of formulations, mode of administration, and any precautions which needed to be followed during medication period together with any other details which the FMP wanted to provide. In the guided field-walk method, the FMP took the interviewers on guided field-walks through areas from where he collected his medicinal plants, pointed out the plants, and mentioned their use(s). The semi-structured questionnaire and the guided field-walks were augmented with informal conversations between the authors and the FMP, in which conversations the FMP discoursed freely on any topic of his choice and which informal conversations really increased the extent of rapport between the authors and the FMP and provided more information on the medicinal use of plants and animals.
The plants used by the FMP were found to be available within the village area within a radius of about five miles. However, some plants or plant parts (Table 1) as well as two products, namely Mahalaxmi Vilas and Mrityunjaya Rasa were bought from a shop at Saidpur in Nilphamari district, which sold Ayurvedic and Unani medicines, herbs (dried) and spices. Some of these dried herbs and spices were imported from India. Both Mahalaxmi Vilas and Mrityunjaya Rasa, according to the FMP were manufactured by Ayurvedic companies of Bangladesh; the FMP, however, did not divulge the names of the Companies although he gave the names of the ingredients of both preparations. The FMP mentioned that previously he used to get these two medicines from India. Likewise, with the exception of tiger fat, which supposedly was extremely rare and supposed to be smuggled in from outside Bangladesh (possibly India) by travelling vendor(s), the rest of the animal items were common and could be procured locally. The FMP himself was not able to guarantee that the fat really came from a tiger. Most plants could be easily identified through their local names. However, all plants were verified as to their identities by the plant taxonomist at the Medicinal Plant Collection Wing of the University of Development Alternative with help from Bangladesh National Herbarium (where necessary). Plant or plant part specimens were deposited at the Medicinal Plant Collection Wing of the University of Development Alternative [12]. The various animals (including also fish, insects, and shells) were identified on the basis of their local names (Bengali) and validated through discussion with a trained zoologist of the University of Development Alternative.
Table 1: Medicinal plants and formulations of the FMP from Nilphamari district, Bangladesh.
| Serial Number | Scientific Name (Accession Number) | Family Name | Local Name(Bengali) | Parts used(Origin) | Ailments and mode of medicinal use |
|---|---|---|---|---|---|
| 1 | AdhatodavasicaNees(MPCW-UODA 547/2017) | Acanthaceae | Bashok | Leaf(Found in the wild; also cultivated in homesteads.) | Accumulation of mucus in chest. Leaves are boiled in water with table salt and the water is taken orally in small sips after it has become lukewarm.Coughs. Decoction of leaves of Adhatodavasica and Solanumsurattense is orally taken. See Picrorhizakurroa. |
| 2 | Acoruscalamus L.(MPCW-UODA 548/2017) | Acoraceae | Boj | Rhizome(Herbal/spice shop; also available in the wild. Dried or fresh rhizomes were used depending on availability.) | Loss of eyesight, night blindness, eyes assuming a totally white color. Paste is prepared in goat milk of rhizomes of Acoruscalamus, roots of Saussurealappa, fruits of Terminaliabellirica, Terminaliachebula, Piper peepuloides, Piper nigrum, bark of Xeromphisspinosa and ‘shankhanavi’ (Zoological name: Turbinellapyrum, English – conch or sea shell, dried section of a conch containing shell and meat, which has been dried to hard stone like substance; used in Ayuvedic medicine and also used as gemstone). A little amount of water is added to the paste and the mixture stirred with a pigeon feather and applied inside the eyes with the soft part of the feather.Hypertension. Mahalaxmi Vilas (a decoction of aerial parts and fruits of Tribulusterrestris, whole plants of Withaniasomnifera, fruits of Piper nigrum, fruits of Piper peepuloides, leaves of Laurusnobilis, dried rhizome of Zingiberofficinale, fruits and seeds of Amomumsubulatum, aril of Myristicafragrans, and tuber of Acoruscalamus) is taken orally.See Ipomoea mauritiana. |
| 3 | Calotropisprocera (Aiton) W.T. Aiton(MPCW-UODA 550/2017) | Apocynaceae | ShetAkondo | Root(Found in the wild.) | Filariasis. Paste of roots (where root paste is made in a ‘kanji’ – iron mortar and pestle) is topically applied to swollen areas. Kanji is the local name for a mortar and pestle made from stone. |
| 4 | Alocasiaindica (Roxb.) Schott.(MPCW-UODA 553/2017) | Araceae | Mankochu | Tuber(Cultivated for consumption of stems and tubers as vegetable.) | Night blindness. Dried tubers are cooked and taken orally. |
| 5 | Saussurealappa (Decne.)(MPCW-UODA 554/2017) | Asteraceae | Kur | Root(Found in the wild.) | See Acoruscalamus. |
| 6 | Brassica juncea (L.) Czern.(MPCW-UODA 558/2017) | Brassicaceae | Shorisha | Seed oil, seed(Cultivated for its seed oil, which is used in cooking.) | Accumulation of mucus in chest accompanied with labored breathing. Seed oil is massaged on the chest. When massaged on a regular basis, the oil has both preventive and therapeutic effects.See Schimawallichii. |
| 7 | Carica papaya L.(MPCW-UODA 559/2017) | Caricaceae | Pepe | Fruit(Cultivated for its edible fruits.) | See Picrorhizakurroa. |
| 8 | Terminaliabellirica (Gaertn.) Roxb.(MPCW-UODA 560/2017) | Combretaceae | Bohera | Fruit(Cultivated for its fruits, which are considered medicinal.) | See Picrorhizakurroa.See Acoruscalamus. |
| 9 | Terminaliachebula Retz.(MPCW-UODA 561/2017) | Combretaceae | Haritoki | Fruit(Cultivated for its fruits, which are considered medicinal.) | See Picrorhizakurroa.See Acoruscalamus. |
| 10 | Ipomoea mauritianaJacq.(MPCW-UODA 562/2017) | Convolvulaceae | Bhuikumra | Tuber(Found in the wild.) | Diabetes. Dried and powdered tubers are taken orally every morning.To boost immunity, to keep body warm during cold weather. Tubers from at least 12 years old plants of Ipomoea mauritiana are mixed with flowers of Gardenia jasminoides, made into a paste and taken orally.Erectile dysfunction. Tuber of Ipomoea mauritiana is mixed with “Mahalaxmi Vilas’ (a claimed Ayurvedic decoction of aerial parts and fruits of Tribulusterrestris, whole plants of Withaniasomnifera, fruits of Piper nigrum, fruits of Piper peepuloides, leaves of Laurusnobilis, dried rhizome of Zingiberofficinale, fruits and seeds of Amomumsubulatum, aril of Myristicafragrans, and tuber of Acoruscalamus), seed husks of Plantagoovata, and ghee (clarified butter) and taken orally. [Mahalaxmi Vilas was obtained from a herbal/spice shop in Saidpur, Nilphamari district, which shop also sold other Ayurvedic and Unani preparations] |
| 11 | Cassia fistula L.(MPCW-UODA 562/2017) | Fabaceae | Shona pata | Leaf(Found in the wild.) | See Swertiachirayita. |
| 12 | Glycyrrhizaglabra L.(MPCW-UODA 563/2017) | Fabaceae | Josthimodhu | Root(Herbal/spice shop; roots are imported from India and bought in the dried form.) | Tuberculosis (where blood comes out with vomit). Roots are orally chewed. Alternately, paste prepared from roots of Glycyrrhizaglabra and wood of Pterocarpussantalinus in goat milk is orally taken. Accumulation of mucus in chest. Roots are chewed and taken orally.See Rubiatinctorum. |
| 13 | PterocarpussantalinusL.f.(MPCW-UODA 564/2017) | Fabaceae | Roktochandan | Wood(Herbal/spice shop; dried wood or bark is imported from India.) | Respiratory difficulties, asthma, coughs, pneumonia. Oil obtained from wood is rubbed on the chest till cure.See Glycyrrhizaglabra. |
| 14 | Swertiachirayita(Roxb. ex Fleming) H. Karst.(MPCW-UODA 566/2017) | Gentianaceae | Chirata | Aerial part(Cultivated for its aerial parts, which are common home remedies.) | Diabetes. 2 parts of leaves of Cassia fistula, 2 parts of aerial parts of Swertiachirayita, 1 part of Azadirachtaindica leaf, and 1 part of Clerodendrumviscosum leaf are mixed and taken orally daily. Chest pain (heart problem). Decoction of Piper chaba leaf, Azadirachtaindica leaf and Swertiachirayita aerial part is orally taken.See Picrorhizakurroa. |
| 15 | Laurusnobilis L.(MPCW-UODA 567/2017) | Lauraceae | Tejpata | Leaf(Herbal/spice shop; leaves are imported from India and obtained in the dried form.) | See Ipomoea mauritiana. |
| 16 | Azadirachtaindica A. Juss.(MPCW-UODA 568/2017) | Meliaceae | Neem | Bark, leaf(Cultivated as a useful medicinal tree; also grows in the wild.) | See Picrorhizakurroa.See Swertiachirayita. |
| 17 | Tinosporacordifolia (Willd.) Miers.(MPCW-UODA 570/2017) | Menispermaceae | Guloncho | Leaf, stem(Collected from the wild.) | Puerperal fever. Leaves and stems of Tinosporacordifolia are orally taken with boiled rhizomes of Zingiberofficinale and honey.See Picrorhizakurroa. |
| 18 | Ficuscarica L.(MPCW-UODA 572/2017) | Moraceae | Dumur | Bark, fruit(Cultivated for its edible fruits.) | Diabetes (symptoms: acidic feeling in mouth, whitishness in eyes, whitishness in soles of feet, feeling of dizziness after eating sweets). Bark juice and fruits are taken orally once or twice daily. |
| 19 | Moringaoleifera Lam.(MPCW-UODA 573/2017) | Moringaceae | Shajina | Root bark(Cultivated for its edible leaves and fruits.) | See Schimawallichii. |
| 20 | Musa sapientum L.(MPCW-UODA 574/2017) | Musaceae | Kola | Fruit(Cultivated for its edible fruits.) | Puerperal fever. A small piece from the tip of a tail of the common house gecko (Hemidactylusfrenatus) is taken orally after inserting the piece within a ripe fruit. |
| 21 | Myristicafragrans (Houtt.)(MPCW-UODA 575/2017) | Myristicaceae | Jayatri | Aril(Herbal/spice shop; imported from India and available in the dried form.) | See Ipomoea mauritiana. |
| 22 | Boerhaviarepens L.(MPCW-UODA 577/2017) | Nyctaginaceae | Punornava | Root(Collected from the wild.) | See Rubiatinctorum.See Schimawallichii. |
| 23 | Phyllanthusemblica L.(MPCW-UODA 578/2017) | Phyllanthaceae | Amloki | Fruit(Cultivated for its edible fruits, which are also considered medicinal.) | See Picrorhizakurroa. |
| 24 | Piper betle L.(MPCW-UODA 579/2017) | Piperaceae | Pan | Leaf(Cultivated for its leaves, which are chewed with lime.) | Night blindness. 21 drops of leaf juice are applied to the eyes for 3-4 days. |
| 25 | Piper chabaBlume(MPCW-UODA 580/2017) | Piperaceae | Choi | Leaf(Cultivated; stems are used as spice in cuisines of southern districts of Bangladesh.) | See Swertiachirayita. |
| 26 | Piper longum L.(MPCW-UODA 581/2017) | Piperaceae | Pipla | Fruit(Cultivated for its fruits, which are used as spice.) | See Piper nigrum. |
| 27 | Piper nigrum L.(MPCW-UODA 582/2017) | Piperaceae | Golmorich | Fruit(Cultivated for its fruits, which are used as spice.) | Hypertension. Mrityunjaya Rasa is taken orally. The medicine was made from 10 g fine powder of each of: ShuddhaVatsanabha – purified Aconitum ferox, Maricha – Black pepper – Piper nigrum fruits, Pippali – Long pepper fruit – Piper longum, ShuddhaGandhaka – Herbal purified Sulfur, TankanaBhasma – Borax, ShuddhaHingula – Purified and processed Cinnabar (Mercury compound) – 20g or ShuddhaParada – Herbal purified Mercury – 20g. Fine powder of ingredients are triturated with juice extract and made into paste form, pills are prepared and taken orally.[Mrityunjaya Rasa was obtained from a herbal/spice shop in Saidpur, Nilphamari district, which shop also sold other Ayurvedic and Unani preparations]See Acoruscalamus.See Ipomoea mauritiana. |
| 28 | Piper peepuloidesRoxb.(MPCW-UODA 583/2017) | Piperaceae | Pipul | Fruit(Cultivated for its fruits, which are used as spice.) | See Acoruscalamus.See Ipomoea mauritiana. |
| 29 | PicrorhizakurroaRoyle ex. Benth(MPCW-UODA 586/2017) | Plantaginaceae | Kotki | Bark(Collected from the wild.) | Jaundice. Fermented combination of bark of Picrorhizakurroa and Azadirachtaindica, along with fruits of Terminaliabellirica, Terminaliachebula, Phyllanthusemblica, dried aerial parts of Swertiachirayita, and leaves of Adhatodavasica and Tinosporacordifolia is orally taken with honey. Ripe fruits of Carica papaya are also taken orally as well as cooked unripe fruits of the same plant during the medication period. |
| 30 | PlantagoovataForssk.(MPCW-UODA 587/2017) | Plantaginaceae | Isapgul | Seed husk(Herbal/spice shop; seeds soaked in water are generally taken as home remedy for relief of constipation.) | See Ipomoea mauritiana. |
| 31 | Gardenia jasminoides Ellis.(MPCW-UODA 590/2017) | Rubiaceae | Gonduraj | Flower(Grown in homesteads for its fragrant flowers.) | All diseases except gastrointestinal disorders, to boost immunity. Flowers are orally taken.See Ipomoea mauritiana. |
| 32 | Rubiatinctorum L.(MPCW-UODA 592/2017) | Rubiaceae | Monjistha | Leaf(Collected from the wild.) | Filariasis. Paste prepared in a ‘kanji’ (iron mortar and pestle) of roots of Rubiatinctorum, Glycyrrhizaglabra, Solanumnigrum, and Boerhaviarepens is applied as a poultice on swollen areas. |
| 33 | Xeromphisspinosa (Thunb.) Keay.(MPCW-UODA 594/2017) | Rubiaceae | Mon | Bark(Collected from the wild.) | See Acoruscalamus. |
| 34 | Schleicheraoleosa (Lour.) Oken(MPCW-UODA 596/2017) | Sapindaceae | Lakkha | Bark(Herbal/spice shop; imported from India in the dried form.) | Tuberculosis (where blood comes out with vomit). Bark and ‘alta’ (Bengali term for lac, which is the scarlet resinous secretion of a number of species of lac insects, of which the most commonly cultivated species is Kerrialacca) soaked water is orally administered. |
| 35 | Daturametel L.(MPCW-UODA 597/2017) | Solanaceae | Dhutra | Root (Collected from the wild.) | See Schimawallichii. |
| 36 | Solanumnigrum L. (MPCW-UODA 600/2017) | Solanaceae | Gurkamai | Root(Collected from the wild.) | See Rubiatinctorum. |
| 37 | SolanumsurattenseBurm.f.(MPCW-UODA 602/2017) | Solanaceae | Kantakari | Leaf(Collected from the wild.) | See Adhatodavasica. |
| 38 | Withaniasomnifera (L.) Dunal(MPCW-UODA 604/2017) | Solanaceae | Ashwagandha | Whole plant(Collected from the wild.) | See Ipomoea mauritiana. |
| 39 | SchimawallichiiChoisy(MPCW-UODA 607/2017) | Theaceae | Kanak | Root(Collected from the wild.) | Filariasis. Roots of Schimawallichii, Daturametel, Vitexnegundo, Boerhaviarepens, and bark of roots of Moringaoleifera are made into a paste with Brassica juncea seeds and applied as poultice on swollen areas. |
| 40 | Clerodendrumviscosum Vent.(MPCW-UODA 608/2017) | Verbenaceae | Vati | Leaf(Collected from the wild.) | See Swertiachirayita. |
| 41 | Vitexnegundo L.(MPCW-UODA 609/2017) | Verbenaceae | Nishinda | Root(Collected from the wild.) | See Schimawallichii. |
| 42 | AmomumsubulatumRoxb.(MPCW-UODA 610/2017) | Zingiberaceae | Boroelach | Fruits and seeds(Herbal/spice shop; dried fruits containing seeds are imported from India and used as spice.) | See Ipomoea mauritiana. |
| 43 | Zingiberofficinale Roscoe(MPCW-UODA 611/2017) | Zingiberaceae | Ada | Rhizome(Cultivated locally as a spice.) | See Tinosporacordifolia.See Ipomoea mauritiana. |
| 44 | Tribulusterrestris L.(MPCW-UODA 612/2017) | Zygophyllaceae | Gokkhur | Aerial parts, fruits(Herbal/spice shop; imported from India.) | See Ipomoea mauritiana. |
Results and Discussion
Medicinal plants and diseases treated by the FMP
The FMP was found to use a total of 44 plants distributed into 29 families in his formulations, which were 25 in number. These formulations were used to treat respiratory tract disorders, eye disorders, filariasis, diabetes, weakness of immune system, erectile dysfunction, hypertension, tuberculosis, heart disorder, puerperal fever and jaundice. The results are shown in Table 1. The formulations included both monoherbal and polyherbal formulations. Different formulations were used to treat the same disease; an example is the treatment of filariasis with three different formulations and the treatment of tuberculosis with two different formulations. Multiple formulations for treatment of the same disease usually implied that either the disease was quite common and possibly serious, or all the ingredients of a particular formulation were not easy to obtain at any given time. This was an important issue, for although the formulations may contain dried plant(s) or plant part(s) (dried months or even 1-2 years ago), every formulation was made fresh before dispensing it to a patient. It may be mentioned in this context that lymphatic filariasis is endemic in Nilphamari district [21]. Tuberculosis and what is more important, multidrug-resistant tuberculosis is also present in Bangladesh [22].
Animal parts and diseases treated by the FMP
The FMP used parts from 7 animals in his formulations to treat various diseases, which are shown in Table 2. Three animal parts were used by themselves while four animal parts were combined with plant parts for treatment. Body fat obtained from the graylag goose (domesticated) was rubbed on chest to prevent mucus accumulation and pneumonia; various fish species belonging to the Puntius genera were advised to be fried in clarified butter and taken orally; and body fat of the Bengal tiger was advised to be rubbed all over the body to prevent cold. Animal parts which were used with plants included milk of Black Bengal goat (for eye disorders and tuberculosis), tail of common house gecko (for puerperal fever), secreted resin of Indian lac insect (for tuberculosis), and shell of conch (for night blindness).
Table 2: Animal parts and formulations used by the FMP in Nilphamari district, Bangladesh.
| Serial Number | Scientific Name(English name) | Family Name | Local Name(Bengali) | Parts used | Ailments and mode of medicinal use |
|---|---|---|---|---|---|
| 1 | Anseranser(Graylag goose) | Anatidae | Raj hansh | Body fat | Accumulation of mucus in chest, pneumonia. The fat of the Indian domesticated goose (graylag goose, zoological name – Anseranser) is rubbed on and both sides of the chest. This can bring cough relief and prevent occurrence of pneumonia. |
| 2 | Capra aegagrushircus (Black Bengal goat) | Bovidae | Chagol | Milk | See Acoruscalamus, Glycyrrhizaglabra in the plant list (above). |
| 3 | Puntiusconchonius (Rosy barb), Puntiusphutunio (Spotted sail barb), Puntiussarana (Olive barb), Puntiussophore (Pool barb), Puntiusticto (Ticto barb) | Cyprinidae | Kanchanpunti, Phutanipunti, Sarpunti, Jatpunti, Tit punti (respectively) | Whole fish after taking off scales and clearing the insides | Night blindness (nyctalopia). Whole fish is fried in ‘ghee’ (clarified butter) and taken orally. The fish can be any Puntius species found in Bangladesh. |
| 4 | Pantheratigristigris (Bengal tiger) | Felidae | Bagh | Body fat | Cold. Body fat is rubbed all over the body to prevent catching cold. |
| 5 | Hemidactylusfrenatus (Common house gecko) | Geckkonidae | Tiktiki | Tail | See Musa sapientum in the plant list (above). |
| 6 | Kerrialacca (Indian lac insect) | Kerridae | Laksha | Secreted resin | See Schleicheraoleosa in the plant list (above). |
| 7 | Turbinellapyrum (Conch) | Turbinellidae | Shankha | Shell | See Acoruscalamus in the plant list (above). |
FMP’s treatment with animals and ayurvedic influences
Although the FMP used conch with other plants to treat eye disorders, the shell of the conch by itself (grounded to a fine powder or its ash) or in combination with plants is used as a collyrium in Ayurvedic medicines for treatment of eye disorders [23]. Paste prepared from roots of Glycyrrhiza glabra and bark of Santalum album in goat milk was used by the FMP to treat tuberculosis. In classical Ayurvedic texts in Sanskrit, which dates back to at least more than 3,000 years ago, tuberculosis has been described as ‘Rajayakshma’ and treatment has been prescribed with ‘Chhagaseva’, ‘Chhaga’ being Sanskrit for goat; in fact, patients were advised to stay with goats and consume as many products they can obtain from goats including milk and clarified butter obtained from the milk [24]. The patients were also advised to make use of goat feces and goat urine by remaining in close proximity to them, and to acquire a ‘goat’ odor.
FMP’s treatment with plants and minerals and ayurvedic influences
One possible example of Ayurvedic influence was the use of Mahalaxmi Vilas by the FMP to treat erectile dysfunction and hypertension (see Acorus calamus and Ipomoea mauritiana, Table 1). However, it should be pointed out that Ayurvedic texts mention Mahalaxmi Vilas Ras and not Mahalaxmi Vilas. Mahalaxmi Vilas Ras is a herbo-metallic preparation and contains: Abhraka Bhasma – Bhasma (calx) of Mica – 48 g; Shuddha Gandhaka – Purified and processed Sulfur – 24 g; Vanga Bhasma – Bhasma (calx) of Tin – 12 g; Shuddha Parada – Purified and processed Mercury – 6 g; Shuddha Haratala – Purified Orpiment (Arsenic trisulfide) – 6 g; Tamra Bhasma – Bhasma (calx) of Copper – 3g; Karpoora – Camphor – Cinnamomum camphora – 6 g; Jatiphala – Nutmeg (fruit) – Myristica fragrans – 12 g; Vriddhadaru – Argyrea speciosa – 12 g; Swarna Bhasma – Bhasma (calx) of Gold – 12 g. The fine powder of above ingredients is ground with the juice extract, made into paste and pills are prepared [25]. However, the FMP used Mahalaxmi Vilas and not Mahalaxmi Vilas Ras, the latter being used for a multitude of diseases by Ayurvedic practitioners but not erectile dysfunction or hypertension. Since the product was claimed by the FMP to be bought from a shop, which (according to the FMP) sold it as an Ayurvedic preparation, it is possible that the product was given a slightly modified Ayurvedic classical name (Mahalaxmi Vilas instead of the actual Mahalaxmi Vilas Ras) and passed along as the original Ayurvedic product. It is also possible that since Mahalaxmi Vilas contained different ingredients from Mahalaxmi Vilas Ras, it was given a different name. It is further to be noted that the FMP himself further modified the obtained product, Mahalaxmi Vilas from Mahalaxmi Vilas Ras with his own addition of tubers of Ipomoea mauritiana, seed husks of Plantago ovata, and clarified butter, and the product used by the FMP did not include any metallic elements present in Mahalaxmi Vilas Ras. The FMP further used his product to treat different diseases (erectile dysfunction and hypertension) other than specified by Ayurveda for Mahalaxmi Vilas Ras (skin diseases, diabetes, elephantiasis), assuming that Mahalaxmi Vilas and Mahalaxmi Vilas Ras signified the same product. Interestingly, we were not able to obtain Mahalaxmi Vilas at the Saidpur herbal shop; the owner mentioned that a new batch will come on an unspecified date.
The Mahalaxmi Vilas used by the FMP for treatment of hypertension and erectile dysfunction contained among other plants, Withania somnifera. This plant, according to Ayurveda, can lower stress [26], and so can be useful in cases of hypertension. Another plant, present in this polyherbal formulation was Tribulus terrestris, described in Charaka Samhita (a classical Ayurvedic text) as diuretic (which can help hypertensive patients through increased urine output), and other Ayurvedic texts as an aphrodisiac [27]. Zingiber officinale, another component of Mahalaxmi Vilas is also considered an Ayurvedic anti-hypertensive plant [28].
Another formulation of Ayurvedic influence (in terms of ingredients but not therapeutic use) is the use of Mrityunjaya Rasa by the FMP for treatment of hypertension (see Piper nigrum, Table 1). This is a classical Ayurvedic herbo-metallic preparation, whose ingredients include 10 g fine powder of each of Shuddha Vatsanabha – Purified Aconitum ferox, Maricha – Black pepper – Piper nigrum, Pippali – Long pepper fruit – Piper longum, Shuddha Gandhaka – Herbal purified Sulfur, Tankana Bhasma – Borax, Shuddha Hingula – Purified and processed Cinnabar (Mercury sulfide) – 20 g or Shuddha Parada – Herbal purified Mercury – 20 g. Fine powder of ingredients are triturated with juice extract and made into paste form, from which pills are prepared [29]. This shows that the FMP used Mrityunjaya Rasa, which had the same ingredients as described in classical Ayurvedic texts and did not contain any innovations or changes introduced by the FMP as he did for Mahalaxmi Vilas. It is to be mentioned that as per Ayurveda, Mrityunjaya Rasa is to be used for treatment of all types of fever; the FMP used the same product to treat hypertension. The FMP mentioned that this treatment is an innovation over the classical treatment, which he learned from his grandfather.
The use of poisonous plants like Aconitum ferox, which contains large quantities of the toxic alkaloid pseudaconitine, along with other metallic toxic elements (as in Mritunjaya Rasa) raise concerns about this Ayurvedic formulation used by the FMP. However, herbo-metallic preparations and ‘bhasmas’ (ashes or calcined elements) were considered safe in Ayurveda and are still claimed to be safe [30]. The word ‘Shuddha’ used before some ingredients in Mritunjaya Rasa (above) means purified and safe from toxicity (in general it means use of the elements as bhasmas). Bhasmas are prepared by either the Putapaka method (purification, wet grinding, and incineration) or the Kupipakwa method (purification, mixing metals with mercury and sulfur, wet grinding, and incineration); it has been claimed that these processes lead to formation of non-toxic nano-particles and so increasing the efficacies of the medicine containing bhasmas [31]. Mercury, when converted to the sulfide form, apparently becomes safe to use in medicine, as claimed through toxicity studies on a mercury-based Ayurvedic formulation, Sidh Makardhwaj [32]. Rural patients are quick to raise a furor in Bangladesh over alleged mistakes particularly by FMPs; that there have been no allegations of immediate poisoning or other mishaps following use of Mritunjaya Rasa by this FMP (or others to the best of our knowledge) suggests that any toxicity if present in the product possibly manifests itself only after long-term use or after a long time following use, in which case Mritunjaya Rasa will have been forgotten or considered as the cause.
Although not actually prescribed in Ayurvedic classical texts like Charaka, the use of Calotropis procera in the treatment of lymphatic filariasis (similar to the FMP) has been reported for the southern Indian district of Gulbarga [33]. However, the Vedas (which contains description of a number of Ayurvedic plants) mention C. procera as a plant active against parasites, which include leishmanial parasites [34]. The FMP used Adhatoda vasica to treat coughs and mucus. Similar uses have been reported in Ayurveda, where the Sanskrit name of the plant has been mentioned as ‘amalaka’ or ‘bashika’ [35].
The FMP used rhizomes of Acorus calamus along with parts from other plants (polyherbal formulation) to treat eye disorders. Interestingly, the word acorus is derived from the Greek word ‘acoron’, which in turn is derived from the Greek word ‘coreon’ meaning pupil of the eye, and has been used since ancient times for eye disorders [36]; an Ayurvedic medicine named Chandroday Varti containing rhizomes of A. calamus is used for eye disorders like early stages of cataract, pterygium (surfer’s eye), and growth over the eyes (pinguecula) [37]. Saussurea lappa, another plant used in the polyherbal formulation for eye disorder by the FMP, has also been described in Ayurveda as useful for ‘netraroga’ (diseases of the eye; the Ayurvedic name for the plant is ‘kustha’ [38]. Any traditional medicinal uses of Xeromphis spinosa, to our knowledge, has not been reported from Bangladesh, so the FMP was unique in using this plant along with other Ayurvedic plants of known uses against eye disorders. An Ayurvedic medicine – Triphala Ghrita Netratarpan containing fruits of Terminalia bellirica, Terminalia chebula and Phyllanthus emblica (to be noted is that the fruits of the first two plants were used by the FMP in his formulation for eye disorders) is used to treat Computer Vision Syndrome (CVS), an eye disorder [39].
Alocasia indica, used by the FMP for night blindness, has been reported to be used by other FMPs in Jhalokati district, Bangladesh for treatment of rhinitis [40]. Brassica juncea seed oil (used by the FMP for accumulation of mucus in chest accompanied with labored breathing) is a very well-known Ayurvedic plant, known in Sanskrit as rajika, and described in classical Ayurvedic texts like Charaka Samhita, Sushruta Samhita, Bhela Samhita, and Kasyapa Samhita for treatment of a variety of diseases including massaging on body to ward off cold-related disorders [41]. Ipomoea mauritiana, used by the FMP to treat diabetes, is reportedly used in Rangpur district, Bangladesh to treat rheumatic pain [42].
The use of Mahalaxmi Vilas (MV) by the FMP for treatment of erectile dysfunction (ED) cannot be evaluated as to whether it is an Ayurvedic formulation, for as explained earlier, Ayurveda does not have any formulation with this name. However, the use of several plants by the FMP in his Mahalaxmi Vilas (Table 1), namely Tribulus terrestris, Withania somnifera, and Myristica fragrans have been mentioned as plants used as herbal aphrodisiacs in traditional medicines to treat ED [43]. Plants present in MV like Zingiber officinale, T. terrestris, W. somnifera, and M. fragrans are also mentioned in Ayurvedic texts to improve sexual performance and virility (Vajikaran) [44]. Fruits of Piper nigrum (another ingredient of MV) are used by traditional medicinal practitioners of Khulna city, Bangladesh to treat spermatorrhea [45]. The Pankho tribe of Rangamati district, Bangladesh use leaves of Acorus calamus (tuber of the plant is used in MV) to treat asthma [46]. Leaves of A. calamus are taken for typhoid, and roots for snake bites by the Soren clan of the Santal tribe in Rajshahi district, Bangladesh [47]. The Ayurvedic use of Amomum subulatum (another ingredient of MV) is for stomach disorders [48]. Taken together, it appears that the FMP used a combination of already known Ayurvedic plants along with some local plants of his own selections to treat erectile dysfunction. Whether such a combination is helpful needs scientific evaluation but it does show the versatility of a FMP’s practice in Bangladesh.
A paste of roots of Glycyrrhiza glabra and wood of Pterocarpus santalinus in goat milk was used by the FMP to treat tuberculosis. Incidentally, this is the same preparation used in Ayurveda to treat tuberculosis, except that in this formulation in Ayurveda (Ayurveda has several formulations for treating tuberculosis) milk from other animals can be used [49]. The FMP used a combination of leaves or aerial parts of Swertia chirayita, Cassia fistula, Azadirachta indica, and Clerodendrum viscosum to treat diabetes. C. fistula (aragbadh in Ayurveda), A. indica (nimba), and S. chirata (ardhatikta) are considered Ayurvedic antidiabetic plants [50,51]. Leaves of C. viscosum are used by the Marakh sect of the Garo tribe living in Mymensingh district, Bangladesh to treat diabetes [52]. It thus appears that the FMP is in this case also using a combination of Ayurvedic and locally used (meaning used in Bangladesh) antidiabetic plants.
Azadirachta indica is considered in Ayurveda to be good for treatment of cardiovascular disorders [53]; S. chirayita has uses as an Ayurvedic plant to treat hypertension [54]; Piper chaba is used by folk medicinal practitioners of Chalna area, Khulna district, Bangladesh as a tonic [55]; thus these three plants used by the FMP to treat chest pain (heart problem) is again a combination of local and Ayurvedic influences. It is interesting to note that the Central Council for Research in Ayurveda and Siddha, New Delhi, India recommends Tinospora cordifolia and Zingiber officinale to treat chikungunya, a disease causing fever and pain [56]; the FMP used a combination of the two plants to treat puerperal fever, which also causes fever and pain. Ficus carica (used by the FMP for diabetes treatment) is recommended in all three of the established traditional medicinal systems of India, namely Ayurveda, Unani and Siddha to treat diabetes [57]. East Javanese people use several banana (Musa sapientum) cultivars to treat typhoid and yellow fever [58]; the FMP used bananas along with the tip of the tail of common house gecko to treat puerperal fever.
Picrorhiza kurroa and Azadirachta indica bark, along with fruits of Terminalia bellirica, Terminalia chebula, Phyllanthus emblica, dried aerial parts of Swertia chirayita, and leaves of Adhatoda vasica and Tinospora cordifolia were used by the FMP with honey and fruits of Carica papaya to treat jaundice. P. kurroa (known in Ayurveda as kutki) is one of the major components of Arogyavardhini Ras, an Ayurvedic preparation for treatment of liver illnesses [59]. Besides P. kurroa, Arogyavardhini Ras also contains fruits of Terminalia bellirica, Terminalia chebula, and Phyllanthus emblica and juice extract of A. indica and is taken with honey. The ingredients of Arogyavardhini Ras includes - Shuddha Parada – Herbal purified Mercury – 10 g; Shuddha Gandhaka – Herbal purified Sulphur – 10 g; Loha Bhasma – Bhasma prepared from Iron – 10 g; Abhraka Bhasma – Purified and processed Mica – 10 g; Tamra Bhasma – Bhasma prepared from Copper – 10 g; Haritaki – Chebulic Myrobalan fruit rind – Terminalia chebula – 20 g; Vibhitaki – Belliric Myrobalan fruit rind – Terminalia bellirica – 20 g; Amalaki – Indian gooseberry fruit – Emblica officinalis – 20 g; Shilajatu – Asphaltum – 30 g; Pura – Guggulu – Indian bedelium (gum resin) – Commiphora mukul – 40 g; Chitra – Eranda – Castor – Ricinus communis – 40 g; Tikta – Katuki – Picrorhiza kurroa – 220 g. Juice extract of Nimba – Neem – Azadirachta indica – Quantity Sufficient. Fine powders of the above ingredients are ground with the neem juice extract, made into paste and pills are prepared. Pills are taken with honey, fresh ginger juice, water or milk [60]. The differences in the FMP’s and original Ayurveda formulation again shows that the FMP made his own modifications to classical Ayurveda formulations, as has been shown before with other formulations like Mahalaxmi Vilas. It also appears that the FMP is trying to limit the use of metals in his modified formulations. Adhatoda vasica and Carica papaya have been reported to be used by some FMPs of Bangladesh to treat jaundice [61]. In Ayurvedic treatises like Charaka Samhita and Ashtanga Hridaya, Tinospora cordifolia (guduchi) has been mentioned as a useful plant against ‘kamala’ (jaundice) [62].
The FMP used a paste prepared from roots of Rubia tinctorum, Glycyrrhiza glabra, Solanum nigrum, and Boerhavia repens to reduce swellings induced by filariasis (Table 1). G. glabra is considered in Ayurveda to have anti-edema properties [49], and so may be used to reduce filarial swellings; filariasis is known in Ayurveda as ‘shlipada’, and paste of Boerhavia repens is administered orally along with Triphala (Ayurvedic name for equal weight by weight combinations of dry powdered fruits of Terminalia bellirica, Terminalia chebula and Emblica officinalis) to treat filariasis [63]. Another formulation used by the FMP to treat filariasis or rather filarial swellings included roots of Schima wallichii, Datura metel, Vitex negundo, Boerhavia repens, and bark of roots of Moringa oleifera, which are made into a paste with Brassica juncea seeds and applied as poultice on swollen areas. Ethnomedicinal uses of S. wallichii are rare and to our knowledge, previously not reported from Bangladesh; fruit decoction is used for snake bite and insect bite in western Mizoram, India [64]. In Ayurveda, V. negundo (nirgundi) is used to reduce swellings; so is D. metel [65]. M. oleifera and B. juncea are also used in Ayurveda to reduce swellings and edema [41,66].
The use of Schleichera oleosa bark along with lac for treatment of tuberculosis has previously not been reported. Ethnomedicinal uses of S. oleosa include using bark for skin infections and seed oil for skin disorders and rheumatism by various tribes of Satna Forest Division in India [67]. This is possibly the first report of ethnomedicinal use of this plant for tuberculosis. Why lac was used along with remains a question. The FMP specifically mentioned that the combination of lac soaked water (scarlet in color) along with the bark of the plant was used for tuberculosis when accompanied by coming out of blood with vomit. FMPs of Jhalokati district, Bangladesh reportedly use flowers of H. rosa sinensis for hematemesis (coming of blood with vomit) [40]. In Kerala, India, flowers of H. rosa sinensis are used for treating menorrhagia [68]; in Bangladesh, flowers are used for menstrual irregularities like excessive bleeding during menstruation [69]. It is interesting that red flowers of the plant are used; apparently, these possibly are cases of ‘like replacing like’ or redness of flower or lac replacing redness of blood lost due to menstruation or coming out with vomit.
Relevant pharmacological activity reports on the plants and animals used by the FMP (scientific validation of uses)
Any ethnomedicinal study needs to answer the question as to whether the plants and animals or minerals used by any traditional medicinal practitioner(s) can be scientifically validated in their use on the basis of existing pharmacological activity and phytochemicals studies, for such scientific validation can help researchers work in the proper direction and strengthens the possibility of discovering new drugs from the plant or any other substances used. This type of scientific validation (including toxicological data) can also ensure safety of monoherbal and polyherbal formulations, and help eradicate the various questions on herbal medicine that may exist among scientists and allopathic medicine practitioners. Although herbal medicines (in the form of medicine or nutritional supplements) are regaining their lost importance, it is still the belief of many allopathic doctors and other general people (particularly the affluent people of Bangladesh) that herbal medicine is nothing short of quackery and should be banned by the health authorities. To determine how much of the present FMP’s phytotherapeutic knowledge can be scientifically validated, searches were conducted in the scientific literature for relevant reports, which can attest to the validity of the FMP’s therapeutic use of the plants and animals shown in Tables 1 and 2. The results are shown in Table 3 (to be noted is that not all relevant references have been quoted but only representative samples).
Interestingly, while none of the animal species can be scientifically validated as to their use(s) by the FMP, out of 44 plant species used by the FMP, 39 species of plant could be validated in their uses on the basis of available pharmacological studies or phytochemical constituent(s) and their bio-activities. This demonstrates the depth of knowledge of the FMP regarding the medicinal properties of plants [70-100]. It is to be noted that polyherbal formulations were used by the FMP, in which various plant species were used in combination to give synergistic effects. Just to give one example, leaves of Cassia fistula, Swertia chirayita (aerial parts containing leaves), Azadirachta indica, and Clerodendrum viscosum were mixed and advised to be taken orally by the FMP for treatment of diabetes. It can be seen from Table 3 that leaves of all four plant species has been scientifically shown to have hypoglycemic properties [101-120]. It is therefore very much possible that the synergistic hypoglycemic effect produced by the combination can lead to better control of elevated blood glucose levels arising during diabetes. Moreover, though yet to be studied in details, the plants may be giving anti-diabetic effect, each through different mechanisms, like less absorption of glucose from intestine, greater utilization of glucose, or stimulating pancreatic insulin secretion or overcoming insulin resistance, to name only a few, the net result being to synergize the desired effect. It is also possible that any adverse effect given by any of the four plant species used may be negated by the presence of other plant(s). For instance, leaves of A. indica have hepatotoxic properties, which can be mitigated by the hepatoprotective phytoconstituents of S. chirayita [120-123].
The scientific community needs to address the versatile modes of treatment by the FMPs of Bangladesh (like mode of experimentation of a new plant or formulation, if any, standardization of an herbal product containing possibly hundreds of phytochemicals) in the quest for new and better drugs. The versatility of this particular FMP demonstrated itself in several aspects, namely use of polyherbal formulations containing novel mixtures of plant parts (see Serial 14, Table 1); use of plants previously unreported in Bangladesh as ethnomedicinal plants, like Xeromphis spinosa, Schleichera oleosa or Schima wallichii; use of known medicinal plants for novel therapeutic uses (like Plantago ovata for erectile dysfunction); mixing of phytotherapy with zootherapy (Tables 1 and 2); borrowing or being influenced by established forms of traditional medicinal systems in the Indian sub-continent countries (India, Bangladesh, Pakistan) like Ayurveda, Unani or Siddha (like Mrityunjaya Rasa); and finally, the modifications made by the FMP in established formulations of Ayurveda, which appears on the surface to be for the better, like avoidance of heavy metals and addition of other plant parts as in Arogyavardhini Ras (see above). These are the versatilities, which needs to be addressed by the scientific community to come to a consensus on the suitability of a given folk medicinal formulation to successfully treat a given disease [123-186]. Also, it is possibly time for the current “one molecule” therapeutic strategy to be revised. The other important aspect of folk medicinal treatment not properly addressed by the scientific community thus far is evaluation of the efficacy of an animal product in treatment. In Ayurveda, as much as 15-20% of the medicines are based on animal products, while in Unani system, it has been reported that as many as 200 drugs have animal origins [187]. In traditional Chinese medicine (TCM), more than 1500 animal species have been recorded to be of some medicinal use [188]. This usage of animal parts in traditional medicines with more than several thousand years of history of usage strongly justifies scientific validations of their usage.
Potential lead compounds and drugs from the plants and animals used by the FMP
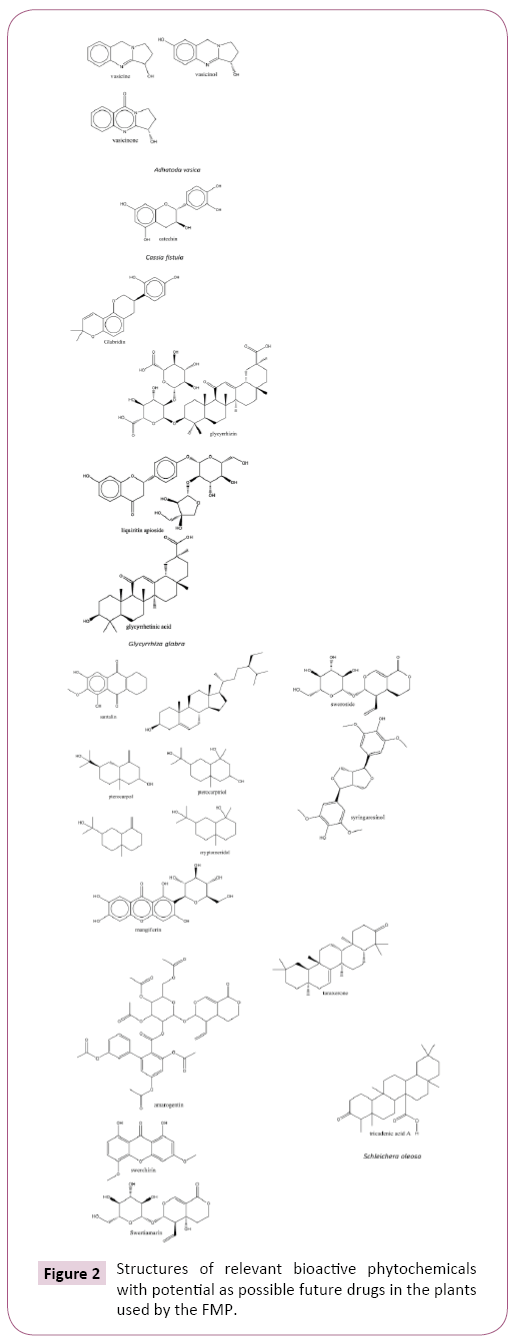
A number of relevant bioactive phytochemicals or compounds present in plants and animals used by the FMP and which can serve as potential lead compounds or future drugs have been given in Table 3 and their structures shown in Figure 2 (for instance vasicine, vasicinol, and vasicinone from A. vasica).
Table 3: Scientific validation of plants and animals used by the FMP.
| Serial Number | Scientific Name(English name) | Family Name | Local Name(Bengali) | Parts used | Ailments and mode of medicinal use |
|---|---|---|---|---|---|
| 1 | Anseranser(Graylag goose) | Anatidae | Raj hansh | Body fat | Accumulation of mucus in chest, pneumonia. The fat of the Indian domesticated goose (graylag goose, zoological name – Anseranser) is rubbed on and both sides of the chest. This can bring cough relief and prevent occurrence of pneumonia. |
| 2 | Capra aegagrushircus (Black Bengal goat) | Bovidae | Chagol | Milk | See Acoruscalamus, Glycyrrhizaglabra in the plant list (above). |
| 3 | Puntiusconchonius (Rosy barb), Puntiusphutunio (Spotted sail barb), Puntiussarana (Olive barb), Puntiussophore (Pool barb), Puntiusticto (Ticto barb) | Cyprinidae | Kanchanpunti, Phutanipunti, Sarpunti, Jatpunti, Tit punti (respectively) | Whole fish after taking off scales and clearing the insides | Night blindness (nyctalopia). Whole fish is fried in ‘ghee’ (clarified butter) and taken orally. The fish can be any Puntius species found in Bangladesh. |
| 4 | Pantheratigristigris (Bengal tiger) | Felidae | Bagh | Body fat | Cold. Body fat is rubbed all over the body to prevent catching cold. |
| 5 | Hemidactylusfrenatus (Common house gecko) | Geckkonidae | Tiktiki | Tail | See Musa sapientum in the plant list (above). |
| 6 | Kerrialacca (Indian lac insect) | Kerridae | Laksha | Secreted resin | See Schleicheraoleosa in the plant list (above). |
| 7 | Turbinellapyrum (Conch) | Turbinellidae | Shankha | Shell | See Acoruscalamus in the plant list (above). |
Figure 2: Structures of relevant bioactive phytochemicals with potential as possible future drugs in the plants used by the FMP.
Conclusions
Folk medicinal practice and folk medicinal practitioners in Bangladesh form a versatile group of practitioners with no single philosophy of practicing methods. Since such practice, although mainly dependent on phytotherapy, can also include diverse elements such as zootherapy, use of minerals or metals, as well be influenced by more established forms of traditional medicine like Ayurveda or Unani (along with innovations carried out on formulations in these two traditional medicinal systems), documentation of such practices can lead to scientific research and potential discovery of new and more efficacious medicines. As such, the phytotherapeutic and zootherapeutic practices of the FMP documented in the present study can prove useful in discovery of novel medicines against diseases like filariasis, diabetes, hypertension, heart problems, and bacterial infections. This is more so, because a review of the scientific literature demonstrated that most of the plants used by the FMP for therapeutic purposes are scientifically validated in their use(s) based on reported pharmacological activity studies or presence of relevant bioactive phytocontituents. These types of polyherbal or poly-product based therapeutic formulations can also help in a paradigm switch from the current one molecule therapeutic mode of treatment.
Acknowledgements
The authors thank the FMP and people of Domar Upazila in Nilphamari district for their support. Special thanks go to parents of one of the authors (SN) for introducing us to the FMP and to help build up rapport with the FMP and local population.
References
- Trueba G, Dunthorn M (2012) Many neglected tropical diseases may have originated in the Paleolithic or before: new insights from genetics. PLoS Neglected Tropical Diseases 6: e1393.
- Huffman MA (2001) Self-medicative behavior in the African great apes: An evolutionary perspective into the origins of human traditional medicine. BioScience 51: 651-661.
- Sofowora A (1982) In: Medicinal Plants and Traditional Medicinal in Africa. New York: John Wiley and Sons.
- Gilani AH, Rahman AU (2005) Trends in ethnopharmacology. Journal of Ethnopharmacology 100: 43-49.
- World Health Organization (2014) A brief guide to emerging infectious diseases and zoonoses.
- World Health Organization (2014) Antimicrobial Resistance: Global Report on Surveillance.
- Bloland PB (2001) Drug resistance in malaria 2001; World Health Organization.
- BIMSTEC (2015) Traditional Systems of Medicine of BIMSTEC Member States. Department of Thai Traditional and Complementary Medicine.
- Rahmatullah M, Pk SR, Al-Imran M, Jahan R (2013) The Khasia tribe of Sylhet district, Bangladesh and their fast disappearing knowledge of medicinal plants. Journal of Alternative and Complementary Medicine 19: 599-606.
- Rahmatullah M, Khatun Z, Barua D, Alam MU, Jahan S, et al. (2013) Medicinal plants used by traditional practitioners of the Kole and Rai tribes of Bangladesh. Journal of Alternative and Complementary Medicine 19: 483-491.
- Mukti M, Rahmatullah M (2013) Treatment with aquatic plants by a Bagdi tribal healer. Ancient Science of Life 33: 22-26.
- Kabir MH, Hasan N, Rahman MM, Rahman MA, Khan JA, et al. (2014) A survey of medicinal plants used by the Deb barma clan of the Tripura tribe of Moulvibazar district, Bangladesh. Journal of Ethnobiology and Ethnomedicine 10: 19.
- Bhuiyan P, Khatun Z, Jahan S, Morshed MT, Rahman S, et al. (2013) Use of Quranic verses, amulets, numerology, and medicinal plants for treatment of diseases: a case study of a healer in Narsinghdi district, Bangladesh. American Eurasian Journal of Sustainable Agriculture 7: 415-425.
- Sultana A, Rahmatullah M (2016) A critical analysis of some medicinal plants used by a folk medicinal practitioner in Savar, Dhaka district, Bangladesh. World Journal of Pharmacy and Pharmaceutical Science 5: 2157-2166.
- Akter MN, Tanny UT, Akter N, Ahmed KMI, Roknuzzaman M, et al. (2016) Folk medicinal practices of a village practitioner in Jessore district, Bangladesh. Journal of Chemical and Pharmaceutical Research 9: 209-213.
- Akter MH, Akter MH, Prodhan MT, Akter S, Akter N, et al. (2017) Documentation of plant-based remedies of a folk herbalist of Comilla district, Bangladesh. World Journal of Pharmacy and Pharmaceutical Sciences 6: 1-11.
- Rahman T, Roy PR, Chhanda NN, Seraj S, Rahmatullah M (2017) Combination of Ayurveda and folk medicine: plants and formulations of a traditional medicinal practitioner in Noakhali district, Bangladesh. Journal of Medicinal Plants Studies 5: 292-297.
- Mannaf MA, Islam MA, Akter S, Akter R, Nasrin T, et al. (2013) A randomized survey of differences in medicinal plant selection as well as diseases treated among folk medicinal practitioners and between folk and tribal medicinal practitioners in Bangladesh. American-Eurasian Journal of Sustainable Agriculture 7: 196-209.
- Martin GJ (1995) In: Ethnobotany: a ‘People and Plants’ Conservation Manual. London: Chapman and Hall.
- Maundu P (1995) Methodology for collecting and sharing indigenous knowledge: a case study. Indigenous Knowledge and Development Monitor 3: 3-5.
- Saha AK, Mohanta MK (2011) Bancroftian elephantiasis in Nilphamari, Bangladesh. Mymeningh Medical Journal 20: 40-44.
- Banu S, Rahman MT, Ahmed S, Khatun R, Ferdous SS, et al. (2017) Multidrug-resistant tuberculosis in Bangladesh: results from a sentinel surveillance system. The International Journal of Tuberculosis and Lung Disease 21: 12-17.
- Palbag S, Pal K, Saha D, Nandi MK, De BK, et al. (2013) Pharmaceutics, ethnopharmacology, chemistry and pharmacology of Ayurvedic marine drugs: A review. International Journal of Research in Ayurveda & Pharmacy 4: 437-442.
- Dandekar N, Shah N (2016) Goat milk: Boon for pulmonary tuberculosis patients. International Ayurvedic Medical Journal (IAMJ).
- Rasendra Sara Sangraha Kapharoga Chikitsa [https://ayurmedinfo.com/2012/07/11/mahalaxmi-vilas-ras-benefits-dosage-ingredients-side-effects/]. (A literal translation in English will be somewhat “Compilation of Rasas to treat Kapha diseases”).
- Sharma T, Ramamurthy A, Parul A, Malvika (2016) Hypertension: Management through Ayurveda herbs. World Journal of Pharmacy and Pharmaceutical Sciences 5: 468-480.
- Verma P, Galib, Patgiri BJ, Prajapati PK (2013) Tribulus terrestris Linn: A phyto-pharmacological review. Journal of Ayurveda and Holistic Medicine 1: 37-43.
- Sruthy PN, Anoop KR (2013) Healing hypertension: A focus on alternative systems of medicine. International Journal of Pharmaceutical Sciences Review and Research 21: 264-273.
- Dutta Sharma KS, Aravind BS, Vinaya TM, Lakshmi Prasanna AVK (2012) Review of Andhra Bhaishajya Ratnavali – An important Ayurveda text in Telugu language. Ayurpharm. International Journal of Ayurveda and Allied Sciences 1: 132-137.
- Virupaksha Gupta KL, Pallavi G, Patgiri BJ, Kodlady N (2011) Relevance of Rasa Shastra in 21st century with special reference to lifestyle disorders (LSDs). International Journal of Research in Ayurveda & Pharmacy (IJRAP) 2: 1628-1632.
- Pal SK (2015) The Ayurvedic Bhasma: The ancient science of nanomedicine. Recent Patents on Nanomedicine 5: 12-18.
- Kumar G, Srivastava A, Sharma SK, Gupta YK (2014) Safety evaluation of mercury based Ayurvedic formulation (Sidh Makardhwaj) on brain cerebrum, liver & kidney in rats. Indian Journal of Medical Research 139: 610-618.
- Narahari SR, Manjula K, Bose KS, Aggithaya MG, Swamy GK, (2016) Harmful traditional healing practices in the treatment of lymphatic filariasis. Indian Journal of Dermatology, Venereology and Leprology 82: 565-567.
- Bauri RK, Tigga MN, Kullu SS (2015) A review on use of medicinal plants to control parasites. Indian Journal of Natural Products and Resources 6: 268-277.
- Gangwar AK, Ghosh AK (2014) Medicinal uses and pharmacological activity of Adhatoda vasica. International Journal of Herbal Medicine 2: 88-91.
- Singh R, Sharma PK, Malviya R (2011) Pharmacological properties and Ayurvedic value of Indian Buch plant (Acorus calamus): A short review. Advances in Biological Research 5: 145-154.
- Vacha – Acorus calamus uses, research, side effects, remedy [https://easyayurveda.com/2015/01/06/vacha-acorus-calamus-uses-research-side-effects-remedy/], accessed May 30, 2017.
- Prasad PVV, Subhaktha PKJP (2002) Medico-historical review of drug Kustha (Saussurea lappa C.B. Clarke). Bulletin of the Indian Institute of History of Medicine: 79-92.
- Sawant DP, Parlikar GR, Binorkar SV (2013) Efficacy of Triphala Ghrita Netratarpan in Computer Vision Syndrome. International Journal of Research in Ayurveda and Pharmacy 4: 244-248.
- Rahmatullah M, Nuruzzaman M, Hossan MS, Khatun MA, Rahman MM, et al. (2010) An ethnomedicinal survey of folk medicinal practitioners of Shitol Para village, Jhalokati district, Bangladesh. Advances in Natural and Applied Sciences 4: 85-92.
- Ram Manohar P, Reshmi P, Rohini S (2009) Mustard and its uses in Ayurveda. Indian Journal of Traditional Knowledge 8: 400-404.
- Azad AK, Mahmud MR, Parvin A, Chakrabortty A, Akter F, et al. (2014) Medicinal plants of a folk medicinal healer of Rangpur district, Bangladesh. Journal of Medicinal Plants and Studies 2: 46-50.
- Saxena A, Prakash P, Porwal M, Sissodia N, Sharma P (2012) Erectile dysfunction: A review and herbs used for its treatment. International Journal of Green Pharmacy 6: 109-117.
- Chauhan NS, Sharma V, Dixit VK, Thakur M (2014) A review of plants used for improvement of sexual performance and virility. BioMed Research International.
- Akber M, Seraj S, Islam F, Ferdausi D, Ahmed R, et al. (2011) A survey of medicinal plants used by the traditional medicinal practitioners of Khulna city, Bangladesh. American-Eurasian Journal of Sustainable Agriculture 5: 177-195.
- Sarker MN, Mahin AA, Munira S, Akter S, Parvin S, et al. Ethnomedicinal plants of the Pankho community of Bilaichari Union in Rangamati district, Bangladesh. American-Eurasian Journal of Sustainable Agriculture 7: 114-120.
- Rahmatullah M, Hasan A, Parvin W, Moniruzzaman M, Khatun A, et al. (2012) Medicinal plants and formulations used by the Soren clan of the Santal tribe in Rajshahi district, Bangladesh for treatment of various ailments. African Journal of Traditional, Complementary and Alternative Medicine 9: 350-359.
- Khare CP (2007) In: Indian Medicinal Plants-An Illustrated Dictionary, Springer-Verlag.
- Gupta R (2016) Yastimadhu (Glycyrrhiza glabra) – An important plant of Ayurvedic system of medicine. Journal of Medicinal Plants Studies 4: 30-31.
- Sharma R, Prajapati PK (2016) Antidiabetic leads from Ayurvedic medicinal plants. International Journal of Advanced Complementary and Traditional Medicine 2: 24-41.
- Kumar SG, Dubey N (2015) Swertia chirayata: An Ayurvedic herb and its medicinal uses. International Ayurvedic Medical Journal (IAMJ) 3: 484-490.
- Rahmatullah M, Azam MNK, Khatun Z, Seraj S, Islam F, et al. (2012) Medicinal plants used for treatment of diabetes by the Marakh sect of the Garo tribe living in Mymensingh district, Bangladesh. African Journal of Traditional, Complementary and Alternative Medicine 9: 380-385.
- Lokhande PD, Jagdale SC, Chabukswar AR (2006) Natural remedies for heart diseases. Indian Journal of Traditional Knowledge 5: 420-427.
- Kumar V, Staden JV (2016) A review of Swertia chirayita (Gentianaceae) as a traditional medicinal plant. Frontiers in Pharmacology 6: 1-14.
- Rahmatullah M, Ferdausi D, Mollik MAH, Jahan R, Chowdhury MH, et al. (2010) A survey of medicinal plants used by Kavirajes of Chalna area, Khulna district, Bangladesh. African Journal of Traditional, Complementary and Alternative Medicine 7: 91-97.
- Central Council for Research in Ayurveda and Siddha: Management of Chikungunya through Ayurveda and Siddha – A Technical Report. Central Council for Research in Ayurveda and Siddha, Department of AYUSH, Ministry of Health and Family Welfare, Government of India, New Delhi, 2009, (GS Lavekar, Chief Editor).
- Badgujar SB, Patel VV, Bandivdekar AH, Mahajan RT (2014) Traditional uses, phytochemistry and pharmacology of Ficus carica: A review. Pharmaceutical Biology 52: 1487-1503.
- Hapsari L, Kennedy J, Lestari DA, Masrum A, Arini WL (2017) Ethnobotanical survey of bananas (Musaceae) in six districts of East Java, Indonesia. Biodiversitas 18: 160-174.
- Masood M, Arshad M, Qureshi R, Sabir S, Amjad MS, et al. (2015) Picrorhiza kurroa: An ethnopharmacologically important plant species of Himalayan region. Pure and Applied Biology 4: 407-417.
- https://ayurmedinfo.com/2012/07/10/arogyavardhini-vati-benefits-dosage-ingredients-side-effects/
- Chowdhury AR, Rahmatullah M (2012) Ethnomedicinal plants for treatment of jaundice by the folk and tribal medicinal practitioners of several districts in Bangladesh and review of their scientifically reported hepatoprotective activity. American-Eurasian Journal of Sustainable Agriculture 6: 360-370.
- Sinha K, Mishra NP, Singh J, Khanuja SPS (2004) Tinospora cordifolia (Guduchi), a reservoir plant for therapeutic applications: A review. Indian Journal of Traditional Knowledge 3: 257-270.
- Warrier PK (1995) Filariasis (Shlipada). Bulletin of the Indian Institute of History of Medicine (Hyderabad) 25: 38-45.
- Lalfakzuala R, Lalramnghinglova H, Kayang H (2007) Ethnobotanical usages of plants in western Mizoram. Indian Journal of Traditional Knowledge 6: 486-493.
- Ahuja SC, Ahuja S, Ahuja U (2015) Nirgundi (Vitex negundo) – Nature’s gift to Mankind. Asian Agri-History 19: 5-32.
- Agarwal V (2017) The Magical Moringa.
- Anuragi JL, Mishra RP (2017) Ethnomedicinal study of Schleichera oleosa among the tribals of Satna (M.P.). International Journal of Applied Research 3: 672-674.
- Rajith NP, Ambily DV, Dan VM, Devi PS, George V, et al. (2012) A survey on ethnomedicinal plants used for menstrual disorders in Kerala. Indian Journal of Traditional Knowledge 11: 453-460.
- Ahmed KMI, Bashar MS, Tanny UT, Akter N, Mandal BK, et al. (2017) Ethnomedicinal formulations of a Garo tribal healer in Haluaghat, Mymensingh district, Bangladesh. Journal of Medicinal Plants Studies 5: 219-223.
- Dhuley JN (1999) Antitussive effect of Adhatoda vasica extract on mechanical or chemical stimulation-induced coughing in animals. Journal of Ethnopharmacology 67: 361-365.
- Bhalla HL, Nimbkar AY (1982) Preformulation studies III. Vasicinone, a bronchodilatory alkaloid from Adhatoda vasica Nees (absorption, potency and toxicity studies). Drug Development and Industrial Pharmacy 8: 833-846.
- Amin AH, Mehta DR (1959) A bronchodilator alkaloid (vasicinone) from Adhatoda vasica Nees. Nature.
- Lahiri PK, Pradhan SN (1964) Pharmacological investigation of vasicinol, an alkaloid from Adhatoda vasica Nees. Indian Journal of Experimental Biology 2: 219.
- Sarkar C, Bose S, Banerjee S (2014) Evaluation of hepatoprotective activity of vasicinone in mice. Indian Journal of Experimental Biology 52: 705-711.
- Bhattacharyya D, Pandit S, Jana U (2005) Hepatoprotective activity of Adhatoda vasica aqueous leaf extract on D-galactosamine-induced liver damage in rats. Fitoterapia 76: 223-225.
- Kumar M, Dandapat S, Sinha MP (2015) Hepatoprotective activity of Adhatoda vasica and Vitex negundo leaf extracts against carbon tetrachloride induced hepatotoxicity in rats. Advances in Biological Research 9: 242-246.
- Vinothapooshan G, Sundar K (2010) Hepatoprotective activity of Adhatoda vasica leaves against carbontetrachloride induced toxicity. Pharmacologyonline 2: 551-558.
- Patel P, Vaghasiya J, Thakor A, Jariwala J (2012) Antihypertensive effect of rhizome part of Acorus calamus on renal artery occlusion induced hypertension in rats. Asian Pacific Journal of Tropical Disease.
- Jabbar-Shah A, Gilani A (2009) Blood pressure-lowering and vascular modulator effects of Acorus calamus are mediated through multiple pathways. Journal of Cardiovascular Pharmacology 54: 38-46.
- Singh R, Singh S, Jeyabalan G, Ali A (2012) An overview on traditional medicinal plants as aphrodisiac agent. Journal of Pharmacognosy and Phytochemistry 1: 43-56.
- Singh B, Gupta V, Bansal P, Singh R, Kumar D (2010) Pharmacological potential of plant used as aphrodisiacs. International Journal of Pharmaceutical Sciences Review and Research 5: 104-113.
- Sharma R, Thakur GS, Sanodiya BS, Savita A, Pandey M, et al. (2012) Therapeutic potential of Calotropis procera: A giant milkweed. IOSR Journal of Pharmacy and Biological Sciences 4: 42-57.
- Shahi M, Hanafi-Bojd AA, Iranshahi M, Vatandoost H, Hanafi-Bojd MY (2010) Larvicidal efficacy of latex and extract of Calotropis procera (Gentianales: Asclepiadaceae) against Culex quinquefasciatus and Anopheles stephensi (Diptera: Culicidae). Journal of Vector Borne Diseases 47: 185-188.
- Parihar G, Sharma A, Ghule S, Sharma P, Deshmukh P, et al. (2011) Anti inflammatory effect of Calotropis procera root bark extract. Asian Journal of Pharmacy & Life Science 1: 29-44.
- Suresh Babu AR, Karki SS (2011)Anti-inflammatory activity of various extracts of roots of Calotropis procera against different inflammation models. International Journal of Pharmacy and Pharmaceutical Sciences 3: 191-194.
- Akhtar MS, Bashir S, Malik MNH, Manzoor R (2013) Cardiotonic activity of methanol extract of Saussurea lappa Linn roots. Pakistan Journal of Pharmaceutical Sciences 26: 1197-1201.
- Mazumder A, Dwivedi A, du Plessis J (2016) Sinigrin and its therapeutic benefits. Molecules 21: 416.
- Pathan IB, Setty CM (2009) Chemical penetration enhancers for transdermal drug delivery systems. Tropical Journal of Pharmaceutical Research 8: 173-179.
- Sadeque MZ, Begum ZA, Umar BU, Ferdous AH, Sultana S, et al. (2012) Comparative efficacy of dried fruits of Carica papaya Linn. and Vitamin-E on preventing hepatotoxicity in rats. Faridpur Medical College Journal 7: 29-32.
- Shashidhara SC, Bharath Raj KC, Aswathanarayana BJ (2012) A comparative study of anti-cataract activity of Triphala and its constituents. International Research Journal of Pharmacy 3: 407-410.
- Anand KK, Singh B, Saxena AK, Chandan BK, Gupta VN (1994) Hepatoprotective studies of a fraction from the fruits of Terminalia belerica Roxb. on experimental liver injury in rodents. Phytotherapy Research 8: 287-292.
- Mishra S, Anuradha J, Tripathi S, Nathiya D, Kumar S (2016) In vitro effect of triphala constituent in sodium selenite-induced cataractogenesis. Int J Herbal Med 4: 193-197.
- Gupta PC (2012) Biological and pharmacological properties of Terminalia chebula Retz. (Haritaki) – An overview. International Journal of Pharmacy and Pharmaceutical Sciences 4: 62-68.
- Choi MK, Kim HG, Han JM, Lee JS, Lee JS, et al. (2015) Hepatoprotective effect of Terminalia chebula against t-BHP-induced acute liver injury in C57/BL6 mice. Evidence-Based Complementary and Alternative Medicine.
- Yeasmin T, Akhter QS, Tasnim M, Jahan S (2016) Hepatoprotective effect of Terminalia chebula (Haritaki) on serum bilirubin in paracetamol induced liver damage in Wistar albino rats. Dinajpur Medical College Journal 9: 78-83.
- Sulaiman C, Geetha SP, Indira B (2014) Identification of phenolic antioxidants in Ipomoea mauritiana Jacq. using spectrophotometric and mass spectroscopic studies. Avicenna Journal of Phytomedicine 4: 89-96.
- Ullah A, Khan A, Khan I (2016) Diabetes mellitus and oxidative stress – A concise review. Saudi Pharmaceutical Journal 24: 547-553.
- Zhao G, Kan J, Li Z, Chen Z (2005) Characterization and immunostimulatory activity of an (1→6)-ï¡-D-glucan from the root of Ipomoea batatas. International Immunopharmacology 5: 1436-1445.
- Pallavi KJ, Singh R, Singh S, Singh K, Farswan M, et al. (2011) Aphrodisiac agents from medicinal plants: A review. Journal of Chemical and Pharmaceutical Research 3: 911-921.
- Mahajan GK, Mahajan RT, Mahajan AY (2015) Improvement of sperm density in neem-oil induced infertile male albino rats by Ipomoea digitata Linn. Journal of Intercultural Ethnopharmacology 4: 125-128.
- Vasudeva K, Manoharan S, Panjamurthy K, Vellaichamy L, Chellammal A (2008) Evaluation of antihyperglycemic effect of Cassia fistula (Linn.) leaves in streptozotocin induced diabetic rats. Electronic Journal of Pharmacology and Therapy 1: 57-60.
- Silawat N, Jarald EE, Jain N, Yadav A, Deshmukh PT (2009) The mechanism of hypoglycemic and antidiabetic action of hydroalcoholic extract of Cassia fistula Linn. in rats. The Pharma Research 1: 82-92.
- Danish M, Singh P, Mishra G, Srivastava S, Jha KK, et al. (2011). Cassia fistula Linn. (Amulthus)- An important medicinal plant: A review of its traditional uses, phytochemistry and pharmacological properties. Journal of Natural Product and Plant Resoures 1: 101-118.
- Pitchai D, Manikkam R (2012) Hypoglycemic and insulin mimetic impact of catechin isolated from Cassia fistula: a substantiate in silico approach through docking analysis. Medicinal Chemistry Research 21: 2238-2250.
- Gupta VK, Fatima A, Faridi U, Negi AS, Shanker K, et al. (2008) Antimicrobial potential of Glycyrrhiza glabra roots. Journal of Ethnopharmacology 116: 377-380.
- Nair SS, Pharande RR, Bannalikar AS, Mukne AP (2015) In vitro antimycobacterial activity of acetone extract of Glycyrrhiza glabra. Journal of Pharmacy and Pharmacognosy Research 3: 80-86.
- Hikino H (1985) Recent research on oriental medicinal plants. In: Economic and Medicinal Plant Research, H Wagner, H Hikino, NR Farnsworth (Eds), London, Academic Press 1: 53-85.
- Kamei J, Nakamura R, Ichiki H, Kubo M (2003) Antitussive principles of Glycyrrhiza radix, a main component of Kampo preparations Bakumondo-to (Mai-men-dong-tang). European Journal of Pharmacology 69: 159-163.
- Maurya SK, Singh AK, Seth A (2015) Potential medicinal plants for lymphatic filariasis: A review. Journal of Critical Reviews 2: 1-6.
- Manjunatha BK (2006) Antibacterial activity of Pterocarpus santalinus. Indian Journal of Pharmaceutical Sciences 68: 115-116.
- Azamthulla M, Anbu J, Ashoka Babu VL, Rajkapoor B (2016) Isolation and characterization of Pterocarpus santalinus heartwood extract. Der Pharmacia Lettre 8: 34-39.
- Kesari AN, Gupta RK, Watal G (2004) Two aurone glycosides from heartwood of Pterocarpus santalinus. Phytochemistry 65: 3125-3129.
- Ododo MM, Choudhury MK, Dekebo AH (2016) Structure elucidation of ï¢-sitosterol with antibacterial activity from the root bark of Malva parviflora. Springerplus; Heidelberg 5: 1210.
- Kavitha KN, Dattatri AN (2013) Experimental evaluation of antidiabetic activity of Swertia chirata – aqueous extract. Journal of Public Health and Medical Research 1: 71-75.
- Sellamuthu PS, Muniappan BP, Perumal SM, Kandasamy M (2009) Antihyperglycemic effect of mangiferin in streptozotocin induced diabetic rats. Journal of Health Science 55: 206-214.
- Phoboo S, Pinto MDS, Barbosa ACL, Sarkar D, Bhowmik PC, et al. (2013) Phenolic-linked biochemical rationale for the anti-diabetic properties of Swertia chirayita (Roxb. ex Flem.) Karst. Phytotherapy Research 27: 227-235.
- Saxena AM, Bajpai MB, Mukherjee SK (1991) Swerchirin induced blood sugar lowering of streptozotocin treated hyperglycemic rats. Indian Journal of Experimental Biology 29: 674-675.
- Vaidya H, Rajani M, Sudarsanam V, Padh H, Goyal R (2009) Swertiamarin: a lead from Enicostemma littorale Blume. for anti-hyperlipidaemic effect. European Journal of Pharmacology 617: 108-112.
- Pardo-Andreu GL, Paim BA, Castilho RF, Velho JA, Delgado R, et al. (2008) Mangifera indica L. extract (Vimang®) and its main polyphenol mangiferin prevent mitochondrial oxidative stress in atherosclerosis-prone hypercholesterolemic mouse. Pharmacological Research 57: 332-338.
- Ya BQ, Nian LC, Li C, Gen XP (1999) Protective effect of swerchirin on hematopoiesis in 60Co–irradiated mice. Phytomedicine 6: 85-88.
- Liu J, Liu YP, Klaassen CD (1994) The effect of Chinese hepatoprotective medicines on experimental liver-injury in mice. Journal of Ethnopharmacology 42: 183–191.
- Luo YD, Chen J, Cao J, Wen XD, Li P (2009) Determination of sweroside in rat plasma and bile for oral bioavailability and hepatobiliary excretion. Chemical and Pharmaceutical Bulletin 57: 79–83.
- Chakravarty AK, Mukhopadhyay S, Moitra SK, Das B (1994) (-)-Syringaresinol, a hepatoprotective agent and other constituents from Swertia chirata. Indian Journal of Chemistry B 33: 405–408.
- Karan M, Vasisht K, Handa SS (1999) Antihepatotoxic activity of Swertia chirata on carbon tetrachloride induced hepatotoxicity in rats. Phytotherapy Research 13: 24-30.
- Akunna GG, Ogunmodede OS, Saalu CL, Ogunlade B, Akunna GG, et al. (2012) Laurus nobilis extract preserves testicular functions in cryptorchid rat. World Journal of Life Science and Medical Research 2: 91-99.
- Gomase PV, Rangari VD, Verma PR (2011) Phytochemical evaluation and hepatoprotective activity of fresh juice of young stem (tender) bark of Azadirachta indica A. Juss. International Journal of Pharmacy and Pharmaceutical Sciences 3: 55-59.
- Thompson EB, Anderson CC (1978) Cardiovascular effects of Azadirachta indica extract. Journal of Pharmaceutical Sciences 67: 1476-1478.
- Khosla P, Gupta A, Singh J (2002) A study of cardiovascular effects of Azadirachta indica (neem) on isolated perfused heart preparations. Indian Journal of Physiology and Pharmacology 46: 241-244.
- Prashanth GK, Krishnaiah GM (2014) Chemical composition of the leaves of Azadirachta indica Linn (neem). International Journal of Advancement in Engineering Technology, Management & Applied Science 1: 21-31.
- Dholi SK, Raparla R, Mankala SK, Nagappan K (2011) In vivo antidiabetic evaluation of Neem leaf extract in alloxan induced rats. Journal of Applied Pharmaceutical Science 1: 100-105.
- Gupta M, Banerjee D, Mukherjee A (2013) Studies of anti-inflammatory, antipyretic and analgesic effects of aqueous extract of traditional herbal drug on rodents. International Research Journal of Pharmacy 4: 113-120.
- Kumar V, Modi PK, Saxena KK (2013) Exploration of hepatoprotective activity of aqueous extract of Tinospora cordifolia – An experimental study. Asian Journal of Pharmaceutical and Clinical Research 6: 87-91.
- Stanca MH, Nagy A, Toşa M, Vlad L (2011) Hepatoprotective effect of orally administered melatonin & Tinospora cordifolia in experimental jaundice. Chirurgia (Bucharest, Romania) 106: 205-210.
- El-Shobaki FA, El-Bahay AM, Esmail RSA, Abd El Megeid AA, Esmail NS (2010) Effects of figs fruit (Ficus carica L.) and its leaves on hyperglycemia in alloxan diabetic rats. World Journal of Dairy & Food Sciences 5: 47-57.
- Pérez C, Domínguez E, Ramiro JM, Romero A, Campillo JE, et al. (1998) A study on the glycaemic balance in streptozotocin-diabetic rats treated with an aqueous extract of Ficus carica (fig tree) leaves. Phytotherapy Research 10: 82-83.
- Jeong WS, Lachance PA (2001) Phytosterols and fatty acids in fig (Ficus carica, var. Mission) fruit and tree components. Journal of Food Science 66: 278-281.
- Gaikwad SB, Krishna Mohan G, Sandhya Rani M (2014) Phytochemicals for diabetes management. Pharmaceutical Crops 5: 11-28.
- Kushwaha V, Saxena K, Verma SK, Lakshmi V, Sharma RK, et al. (2011) Antifilarial activity of gum from Moringa oleifera Lam. on human lymphatic filaria Brugia malawi. Chronicles of Young Scientists 2: 201-206.
- Stohs SJ, Hartman MJ (2015) Review of the safety and efficacy of Moringa oleifera. Phytotherapy Research 29: 796-804.
- Suvarna PI, Pramod LI, Anagha MJ (2009) To study analgesic activity of stem of Musa sapientum Linn. Journal of Pharmacy Research 2: 1381-1382.
- Tajuddin, Ahmad S, Latif A, Qasmi IA, Amin KMY (2005) An experimental study of sexual function improving effect of Myristica fragrans Houtt. (nutmeg). BMC Complementary and Alternative Medicine 5: 16.
- Kalpana P, Joseph S, Murthy Puvvada SR (2010) Plant products in the treatment and control of filariasis and other helminth infections and assay systems for antifilarial/anthelmintic activity. Planta Medica 77: 647-661.
- Vidhya Malar HL, Bai SMM (2009) Hepato-protective activity of Phyllanthus emblica against paracetamol induced hepatic damage in Wistar albino rats. African Journal of Basic and Applied Sciences 1: 21-25.
- Jayaweera DMA (1982) In: Medicinal Plants used in Ceylon. National Science Council of Sri Lanka, Colombo.
- Sarfaraz S, Najam R, Azhar I, Sarwar G (2016) Comparative evaluation of hypolipidemic effects of ethanolic extract of fruit of Piper chaba and Piper nigrum on albino rabbits. Journal of Forensic Biomechanics 7: 128.
- Chaudhary SK, Mukherjee PK, Maiti N, De AK, Bhadra S, et al. (2013) Evaluation of Angiotensin converting enzyme inhibition and anti-oxidant activity of Piper longum L. Indian Journal of Traditional Knowledge 12: 478-482.
- Taqvi SI, Shah AJ, Gilani AH (2008) Blood pressure lowering and vasomodulator effects of piperine. Journal of Cardiovascular Pharmacology 52: 452-458.
- Khushbu C, Roshni S, Anar P, Carol M, Mayuree P (2011) Phytochemical and therapeutic potential of Piper longum Linn: A review. International Journal of Research in Ayurveda and Pharmacy 2: 157-161.
- Sutyarso, Kanedi M, Rosa E (2015) Effects of Black Pepper (Piper nigrum Linn.) extract on sexual drive in male mice. Research Journal of Medicinal Plants 9: 42-47.
- Memudu AE, Akinrinade ID, Ogundele OM, Dare BJ (2015) Effects of crude extract of dry fruits of Piper guineense on male fertility parameters of adult Sprague Dawley rats. European Journal of Medicinal Plants 5: 297-303.
- Sinha S, Bhat J, Joshi MK, Ghaskadbi S (2011) Hepatoprotective activity of Picrorhiza kurroa Royle Ex. Benth extract against alcohol cytotoxicity in mouse liver slice culture. International Journal of Green Pharmacy 5: 244-253.
- Verma PC, Basu V, Gupta V, Saxena G, Rahman LU (2009) Pharmacology and chemistry of a potent hepatoprotective compound Picroliv isolated from the roots and rhizomes of Picrorhiza kurroa Royle ex Benth. (Kutki). Current Pharmaceutical Biotechnology 10: 1-9.
- Xiao W, Li S, Wang S, Ho CT (2017) Chemistry and bioactivity of Gardenia jasminoides. Journal of Food and Drug Analysis 25: 43-61.
- Hussain K, Nisar MF, Majeed A, Nawaz K, Bhatti KH (2010) Ethnomedicinal survey for important plants of Jalalpur Jattan, District Gujrat, Punjab, Pakistan. Ethnobotanical Leaflets: 807-825.
- Sharifzadeh M, Ebadi N, Manayi A, Kamalinezad M, Rezaeizadeh H, et al. (2014) Effect of Rubia tinctorum L. extracts on on carrageenan-induced paw edema in rats. Journal of Medicinal Plants 13: 62-70.
- Das BN, Saha A, Ahmed M (2009) Anti-inflammatory activity of bark of Xeromphis spinosa. Bangladesh Journal of Pharmacology 4: 76-78.
- Rahmatullah M, Islam MR, Kabir MZ, Chowdhury AR (2010) Folk medicinal practices in Vasu Bihar village, Bogra district, Bangladesh. American-Eurasian Journal of Sustainable Agriculture 4: 86-93.
- Prashanth Kumar GM, Shiddamallayya N (2016) Survey of wild medicinal plants of Hassan district, Karnataka. Journal of Medicinal Plants Studies 4: 91-102.
- Ghosh P, Chakraborty P, Mandal A, Rasul MG, Chakraborty M, et al. (2011) Triterpenoids from Schleichera oleosa of Darjeeling foothills and their antimicrobial activity. Indian Journal of Pharmaceutical Sciences 73: 231-233.
- Muthusamy P, Nivedhitha M, Jayshree N (2010) Analgesic and anti-inflammatory activities of Datura metel Linn. Root in experimental animal models. Research Journal of Pharmacy and Technology 3: 897-899.
- Arunachalam G, Subramanian N, Pazhani GP, Karunanithi N, Ravichandran V (2009) Evaluation of anti-inflammatory activity of methanolic extract of Solanum nigrum (Solanaceae). Iranian Journal of Pharmaceutical Sciences 5: 151-156.
- Govindan S, Viswanathan S, Vijayasekaran V, Alagappan R (1999) A pilot study on the clinical efficacy of Solanum xanthocarpum and Solanum trilobatum in bronchial asthma. Journal of Ethnopharmacology 66: 205-210.
- Govindan S, Viswanathan S, Vijayasekaran V, Alagappan R (2004) Further studies on the clinical efficacy of Solanum xanthocarpum and Solanum trilobatum in bronchial asthma. Phytotherapy Research 18: 805-809.
- Mahdi AA, Shukla KK, Ahmad MK, Rajender S, Shankhwar SN, et al. (2011) Withania somnifera improves semen quality in stress-related male fertility. Evidence-Based Complementary and Alternative Medicine.
- Bhattacharya SK, Muruganandam AV (2003) Adaptogenic activity of Withania somnifera: an experimental study using a rat model of chronic stress. Pharmacology Biochemistry and Behavior 75: 547-555.
- Dewanjee S, Maiti A, Sahu R, Dua TK, Mandal SC (2009) Study of anti-inflammatory and antinociceptive activity of hydroalcoholic extract of Schima wallichii bark. Pharmaceutical Biology 47: 402-407.
- Ahmed F, Rahman MS (2014) In vitro antidiabetic activity of Clerodendrum viscosum Vent. Journal of Pharmacreations 1: 47-51.
- Rifat-Ues-Sayeed, Hassan R, Anzum N, Rahman S, Rahmatullah M (2015) Antihyperglycemic and analgesic activity studies with Clerodendrum viscosum Vent. (Verbenaceae) leaves. World Journal of Pharmacy and Pharmaceutical Sciences 4: 216-224.
- Sahare KN, Singh V (2015) Antifilarial activity of methanolic extract of Vitex negundo L. leaves against Setaria cervi filarial parasite. Scholars Academic Journal of Pharmacy 4: 88-92.
- Sahare KN, Anandharaman V, Meshram VG, Meshram SU, Gajalakshmi D, et al. (2008) In vitro effects of four herbal plants on the motility of Brugia malayi microfilariae. Indian Journal of Medical Research 2008; 127: 467-471.
- Das PR, Islam MT, Jahan R, Rahmatullah M (2013) Ethnomedicinal plants used by the Nag clan of the Rai Ghatual tribe of Moulvibazar district, Bangladesh. Ancient Science of Life 32: 217-221.
- Raji Y, Udoh US, Oluwadara OO, Akinsomisoye OS, Awobajo O, et al. (2002) Anti-inflammatory and analgesic properties of the rhizome extract of Zingiber officinale. African Journal of Biomedical Research 5: 121-124.
- Mares WAAK, Najam WS (2012) The effect of ginger on semen parameters and serum FSH, LH and testosterone in infertile men. Tikrit Medical Journal 18: 322-329.
- Gauthaman K, Ganesan AP (2008) The hormonal effects of Tribulus terrestris and its role in the management of male erectile dysfunction-an evaluation using primates, rabbit and rat. Phytomedicine 15: 44-54.
- Tyagi RM, Aswar UM, Mohan V, Bodhankar SL, Zambare GN, et al. (2008) Study of furostenol glycoside fraction of Tribulus terrestris on male sexual function in rats. Pharmaceutical Biology 46: 191-198.
- Alves RRN, Alves HN (2011) The faunal drugstore: Animal-based remedies used in traditional medicines in Latin America. Journal of Ethnobiology and Ethnomedicine 7: 9.
- Falodun A, Imieje V (2013) Herbal medicine in Nigeria: Holistic overview. Nigerian Journal of Science and Environment 12: 1-13.
- In: Centuries of the traditional medicine in Hungary, Millenial exhibition organized by Peter Babulka, Tárnics Company for Consulting and Teaching, Budapest, Hungary.
- Zenebe T, Ahmed N, Kabeta T, Kebede G (2014) Review on medicinal and nutritional values of goat milk. Academic Journal of Nutrition 3: 30-39.
- Jamil S, Jabeen A, Ahmad S (2005) Pulmonary tuberculosis and its management in classical Unani literature. Indian Journal of Traditional Knowledge 4: 143-149.
- Padmanabhan P, Sujana KA (2008) Animal products in traditional medicine from Attappady hills of Western Ghats. Indian Journal of Traditional Knowledge 7: 326-329.
- Mohanty BP, Pati MK, Bhattacharjee S, Sharma AP. Small indigenous fishes and their importance in human health.
- Subramanean J, Vikram Reddy M (2012) Monitor lizards and geckos used in traditional medicine face extinction and need protection. Current Science 102: 1248-1249.
- Madhavan R, Murugesan M (2016) A review on medicinal uses of Sangu (Conch) with Siddha medicine perspectives. International Journal of Advanced Research in Biological Sciences 3: 304-307.
- Gopal R, Vijayakumaran M, Venkatesan R, Kathiroli S (2008) Marine organisms in Indian medicine and their future prospects. Natural Product Radiance 7: 139-145.
- Katsayal UA, Nadabo YA, Isiorho VJ (2008) Effects of methanol extract of Azadirachta indica leaves on the histology of liver and kidney of Wister rats. Nigerian Journal of Pharmaceutical Sciences 7: 9-14.
- Pushpangadan P, George V, Sreedevi P, Ijinu TP, Ninawe A (2014) Ethnozoological knowledge of Indian scheduled tribe, scheduled caste and rural communities. Indian Journal of Traditional Knowledge 13: 735-741.
- Alves RRN, Rosa IL (2005) Why study the use of animal products in traditional medicines? Journal of Ethnobiology and Ethnomedicine 1: 5.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences