Study of Birth Complications in Diabetic Mothers
Hafiz Hafeez Ullah1*, Hafiz Faheem Ullah Khan1, Hafiz Ghulam Murtaza Saleem1 and Wali Ullah2
1Department of Pharmacy, University of Lahore, Lahore, Pakistan
2Department of Physiology, Pakistan Red Crescent Medical and Dental College, Lahore, Pakistan
*Corresponding Author:
Hafiz Hafeez Ullah
Department of Pharmacy
University of Lahore
Lahore, Pakistan
E-mail: ullahhhafiz654@rediffmail.com
Received Date: July 29, 2020; Accepted Date: August 13, 2020; Published Date: August 20, 2020
Citation: Ullah HH, Khan HFU, Murtaza Saleem HG, Ullah W (2020) Study of Birth Complications in Diabetic Mothers. Endocrinol Metab Vol. 4 No.4:2. DOI: 10.36648/endocrinology-metabolism.4.4.2
Copyright: © 2020 Ullah HH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
The current study was being performed to evaluate the birth complications in diabetic mothers; including both maternal and foetal complications; miscarriages. The nature of study was observational cross-sectional study. The study was being taken place at different hospitals, clinical settings, and maternity homes of Lahore during September 2016 to November 2016. The demographic data, family history, socio-economic history, indications, examination findings, results, lab findings etc. were recorded. Total 200 pregnant diabetic patients were evaluated for this study. The age limit for this study was 18-40 years. The patients were being analyzed for their FBS/BSR or HbA1c findings and the type of diabetes was being recorded.
Out of 200 patients, 81% had GDM while the remaining patients were being presented with pregestational diabetes (type I 5%, type II 14% patients). Most of the GDM cases were being diagnosed during 5th to 8th week of pregnancy. Out of 200 pregnancies, 20.5% (41) of these patients had normal pregnancies, and had no major foetal complications except uncontrolled sugar level in mothers. Remaining 79.5% (159) pregnancies/deliveries were associated with some major complications including respiratory distress, macrosomia, hypoglycaemic babies, CVS malformations and still births or miscarriages.
The ratio of normal vaginal delivery to CS was found out to be 29% to 76%. The major indications for these CS deliveries were placental abruption (19.74%), dystocia (14.47%), uterine rupture (13.16%), breech position (6.58%), fetal distress (46.05%) and to some extent previous CS. The miscarriages were being associated with hypertension (41.5%), polyhydramnios (22%), Hughes syndrome (12.2%), and uncontrolled sugar level (24.3%). In our study population TT immunization status was good i.e. 76%. Diabetes is still a major problem of birth complications and miscarriages. Public awareness program is required to educate the people about reproductive health and to motivate them to undergo BSR/FBS during pregnancy prior to 24th gestational weeks to diagnose for GDM.
Keywords
Pregnancy; Complications; Diabetes; GDM, Neonate; Foetus; Miscarriage
Introduction
Definition
Diabetes mellitus (DM), commonly referred to as diabetes, is a group of metabolic disease in which there are high blood sugar levels over a prolonged period.
Overview
DM is a chronic disorder characterized by hyperglycemia and the late development of vascular and neuropathic complications. Regardless of its cause, the disease is associated with a common hormonal defect namely insulin deficiency that may be absolute or relative in the context of coexisting insulin resistance. The effect of insufficient insulin plays a primary role in the metabolic derangements linked to diabetes; hyperglycemia, in turn, plays an important role in disease-related complications [1].
Nomenclature and classification of diabetes
The first widely accepted classification of diabetes mellitus was published by WHO in 1980 [2] and, in modified form, in 1985 [3]. The 1980 Expert Committee proposed two major classes of diabetes mellitus and named them, IDDM or Type 1, and NIDDM or Type 2. In the 1985 Study Group Report the terms Type 1 and Type 2 were omitted, but the classes IDDM and NIDDM were retained, and a class of Malnutrition–related Diabetes Mellitus (MRDM) was introduced. In both the 1980 and 1985 reports other classes of diabetes included Other Types and Impaired Glucose Tolerance (IGT) as well as GDM. These were reflected in the subsequent International Nomenclature of Diseases (IND) in 1991, and the tenth revision of the International Classification of Diseases (ICD–10) in 1992. The 1985 classification was widely accepted and is used internationally [4].
The nomenclature of human DM has been revised, and this classification has been accepted throughout the medical world and literature. The major categories of diabetes are [5].
• Insulin-dependent DM, type I or IDDM
• Noninsulin-dependent DM, type II or NIDDM
• Secondary DM or type S
• Impaired glucose tolerance, IGT
• Gestational diabetes or GDM
• Previous abnormality of glucose tolerance PrevAGT
Types
The vast majority of cases of diabetes fall into two broad etiopathogenetic categories. In one category, type-1 diabetes, the cause is an absolute deficiency of insulin secretion. Individuals at increased risk of developing this type of diabetes can often be identified by serological evidence of an autoimmune pathologic process occurring in the pancreatic islets and by genetic markers. In the other, much more prevalent category, type-2 diabetes, the cause is a combination of resistance to insulin action and an inadequate compensatory insulin secretory response [6].
In a recent study the basic classification of diabetes was described as follows (Tables 1 and 2) [1].
| Major Class | Sub-Class | Cause |
|---|---|---|
| Primary Diabetes | Type 1 diabetes (IDDM or juvenile-onset diabetes) | β-cell destruction, usually leading to absolute insulin deficiency |
| Immune mediated Idiopathic Type 2 diabetes (NIDDM or adult-onset diabetes) | Range from predominant insulin resistance with relative insulin deficiency to predominant secretory defect with insulin resistance |
Table 1: Primary Diabetes and its Classification.
| Major class | Cause | Examples |
|---|---|---|
| Secondary Diabetes | Genetic defects of β-cell function | Maturity-onset diabetes of the young, types 1 to 9; point mutations in mitochondrial DNA |
| Genetic defects in insulin action | Type A insulin resistance, leprechaunism, Rabson-Mendenhall syndrome, lipoatrophic diabetes | |
| Disease of the exocrine pancreas | Pancreatitis, trauma, pancreatectomy, neoplasia, cystic fibrosis, hemochromatosis, fibrocalculous pancreatopathy | |
| Endocrinopathies | Acromegaly, Cushing’s syndrome, hyperthyroidism, pheochromocytoma, glucagonoma, somatostatinoma, aldosteronoma | |
| Drug or chemical induced Diabetes | Vacor, pentamidine, nicotinic acid, glucocorticoids, thyroid hormone, diazoxide, β-adrenergic agonists, thiazides, phenytoin, interferon-α | |
| Infections | Congenital rubella, cytomegalovirus | |
| Uncommon forms of immune-mediated diabetes | Stiff man syndrome, anti-insulin receptor antibodies | |
| Other genetic syndromes | Down syndrome, Klinefelter’s syndrome, Turner’s syndrome, Wolfram’s syndrome, Friedreich’s ataxia, Huntington’s disease, Laurence-Moon-Biedl syndrome, myotonic dystrophy, porphyria, Prader-Willi syndrome | |
| GDM |
Table 2: Secondary Diabetes and its Classification.
Etiology
The vast majority of human diabetics show no clear etiological analogy. But certain rare cases are clearly due to primary pancreatic disease which destroys insulin production, and to other endocrine factors which induce a diabetic state. These include:
Primary pancreatic destruction
• Total surgical pancreatectomy for widespread carcinoma or hyperinsulinism;
• calculus disease and chronic relapsing diabetes;
• haemochromatosis (these three forms are severely insulindeficient)
Primary disturbance of other endocrines (Table 3)
| Endocrinal Disturbance | Disease |
|---|---|
| Pituitary Disease | Acromegaly; severe diabetes. Cushing's basophilism; milder. |
| Adrenal disease | Phaeochromatoma; variable severity. Basophilism; variable severity. |
| Thyrogenic diabetes | With Disturbances of Fat Storage |
Table 3: Endocrinal disturbances during Diabetes.
Risk factors
Type-1 diabetes: The major genetic susceptibility to IDDM is determined by genes in the HLA chromosomal region. An increased relative risk for developing the disease is observed in subjects who are HLA A1, A2, B8, B18, B15, B40, CW3, Bfs, DW3, DW4, DRW3, and DRW4 positive. There is an additive relative risk in subjects who possess two “high risk” HLA B alleles which has an important influence on the prevalence of the disease in sibships and possibly on the concordance rate in diabetic identical twins [7].
Type-2 diabetes: Type II diabetes is a common disorder whose prevalence is increasing in the United States and throughout the world. Type II diabetes is also associated with several other metabolic abnormalities such as central obesity, hypertension, and dyslipidemia, which contributes to the very high rate of cardiovascular morbidity and mortality. The main pathologic defects in diabetes consist of excessive hepatic glucose production, peripheral insulin resistance, and defective beta-cell secretory function.
Treatment of type-1 and type-2 diabetes mellitus
Initiation of non-pharmacologic therapy should be started as soon as the diagnosis is made. Pharmacologic agents should be initiated if the glycemic goals are not met with a 3-month trial of diet and exercise. The cornerstone of therapy consists of a regular exercise routine along with a diet consisting of 40% to 50% complex carbohydrates, 10% to 20% protein, and monounsaturated fats such as canola oil and olive oil.
If non-pharmacologic therapy does not achieve adequate glycemic control, initiation of an oral anti-diabetic agent is warranted. In addition to the sulfonylureas, which work by stimulating insulin secretion, we now have metformin, which inhibits excessive hepatic glucose production; acarbose, which delays the absorption of carbohydrates in the gut; and troglitazone, which reduces insulin, resistance primarily in skeletal muscle [8].
Embryonic stem (ES) cells display the ability to differentiate in vitro into a variety of cell lineages. Using a cell-trapping system, we have obtained an insulin-secreting cell clone from undifferentiated ES cells. Clusters obtained from this clone were implanted (1*10(6) cells) in the spleen of streptozotocin-induced diabetic animals. Transplanted animals correct hyperglycemia within 1 week and restore body weight in 4 weeks. Whereas an intra-peritoneal glucose tolerance test showed a slower recovery in transplanted versus control mice, blood glucose normalization was same after a challenge meal. This approach opens new possibilities for tissue transplantation in the treatment of type-1 and type-2 diabetes and offers an alternative to gene therapy [9].
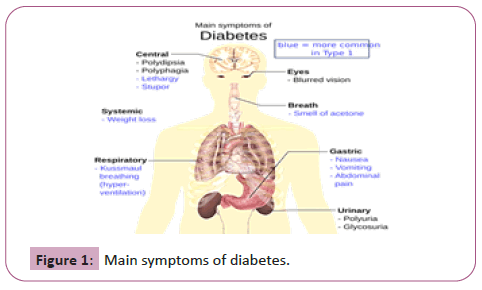
Signs and symptoms of type-1 and type-2 diabetes mellitus
Some of the signs and symptoms commonly experienced include (Figure 1)
• Frequent urination.
• Excessive thirst.
• Increased hunger.
• Weight loss, Tiredness.
• Lack of interest and concentration.
• A tingling sensation or numbness in the hands or feet.
• Blurred vision
Gestational Diabetes Mellitus (GDM)
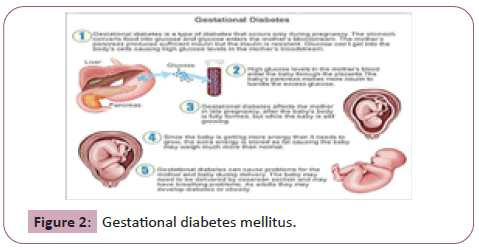
Overview: GDM represents a heterogeneous group of metabolic disorders, which result in varying degrees of maternal hyperglycemia and pregnancy-associated risk. The frequency of GDM is rising globally and may also increase further as lessstringent criteria for diagnosis are adopted [10].
Definition: GDM is defined as “Glucose intolerance that is first detected during pregnancy”. This simple definition belies the complexity of a condition that spans a spectrum of glycaemia, pathophysiology, and clinical effects and for which there is a wide diversity of opinion regarding detection and clinical management (Figure 2) [11].
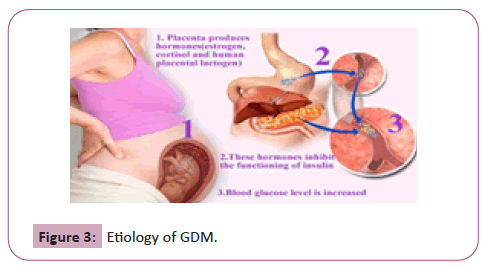
Etiology: During pregnancy, the placenta makes hormones that can lead to a buildup of sugar in blood. Usually, pancreascan make enough insulin to handle that. If not, blood sugar levels will rise and can cause GDM. A transient physiologic insulin resistance and hyperinsulinemia are characteristic of normal pregnancy. In women with β-cells that are not capable of maintaining the high insulin production, GDM develops. A restriction of high insulinogenic carbohydrate may help to prevent the development of GDM [12].
In pregnancy, several physiologic changes take place, the sum of which tends to reset the glucose homeostasis in the direction of diabetes. About 1-2% of all pregnant women develop an abnormal glucose tolerance in pregnancy, but most often glucose tolerance returns to normal postpartum. This condition is called GDM (Figure 3) [13].
Signs and symptoms: GDM typically does not cause any noticeable signs or symptoms. This is why screening tests are so important. Rarely, an increased thirst or increased urinary frequency may be noticed.
GDM has serious, long-term consequences for both baby and mother, including a predisposition to obesity, metabolic syndrome and diabetes later in life. Early detection and intervention can greatly improve outcomes for women with this condition and their babies. Unfortunately, screening and diagnostic tests are not uniform worldwide, which could lead not only to underdiagnosis but also undermanagement of the illness [14].
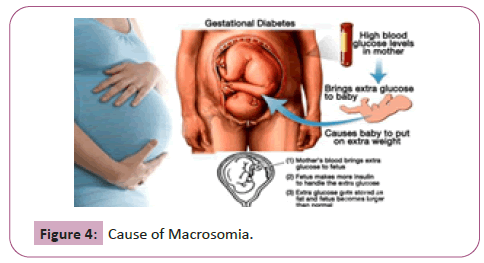
Complications of GDM (Table 4 and Figure 4):
| Major complications | Description |
|---|---|
| Hypoglycemic Babies | Babies of GDM positive mothers develop hypoglycemia shortly after birth because their own insulin production is high. It may provoke seizures in the baby. |
| Macrosomia | High glucose from mother’s blood crosses the placenta, which triggers foetal pancreas to make extra insulin. This can cause baby to grow too large (macrosomia). Very large babies (weigh 9 pounds or more) may become wedged in the birth canal, sustain birth injuries or require a C-section birth. |
| High blood pressure and Pre-Eclampsia | GDM raises risk of high blood pressure, as well as, preeclampsia. |
| Respiratory distress | It is a syndrome in premature infants caused by developmental insufficiency of pulmonary surfactant production and structural immaturity in the lungs. Operative delivery due to macrosomia also increases the risk for transient tachypnea of the newborn, whereas polycythemia predisposes the infant to persistent pulmonary hypertension of the newborn. |
| Cardiovascular anomalies | Cardiomyopathy with ventricular hypertrophy and outflow tract obstruction may occur in as many as 30% of neonates of diabetic mothers. |
Table 4: Major complications associated with GDM.
Case Study
Study design
The design of the current study was observational cross-sectional study. A questionnaire with the variables related to birth complications in diabetic mothers was designed with consensus of gynecologists/patients for the study. The demographic data, family history, previous medical history, reproductive history as well as the Tetanus Toxoid Vaccination status and drug profile was included in the questionnaire. This study was conducted in different Hospitals, Clinical settings, Maternity homes etc. in Lahore, Punjab Pakistan.
Data collection
The questionnaire was designed to collect information regarding various parameters associated with birth complications due to diabetes, directly by patient counselling. Record of patients having IDDM, NIDDM or GDM were evaluated for foetal status. The pathology reports like HbA1C were reviewed to determine the glucose control during previous months. The type of diabetes in patients, presenting signs and symptoms, family history of diabetes, other related pathological conditions, diabetes associated risk factors in mother and child, birth complications, treatment strategies, risk of diabetes in new-born, were evaluated.
Inclusion criteria
In this study, we included all those female patients who gave informed consent to be a part of this study, with positive diagnostic tests for diabetes like BSR or FBS or whose HbA1c value indicated hyperglycemia during pregnancy in the time period of September 2016 to November 2016. In this study, those female patients were also added with the age limit between 18-40 years.
Exclusion criteria
In this study those female patients were not included who refused to give informed consent to be a part of this study and those who left against medical advice after provisional diagnosis was made. In this study, those female patients were also excluded with the age less than 16 years or more than 45 years.
Data analysis
Information was compiled on the pre-designed questionnaire. Data was analyzed on MS Excel, 2010.
Results
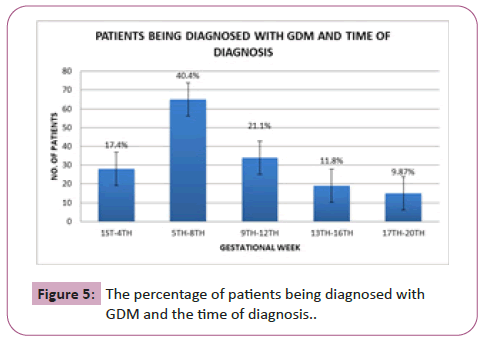
During the above mentioned period of September 2016- November 2016, a total of 200 patients were included in this study out of which 162 women were being identified to have GDM. Among the screened GDM positive women, majority of the women werein 5th to 8th gestational week (2nd month of pregnancy) i.e. 65 cases as shown in Figure 4. Then 34 cases were within 9th to 12th week, 28 cases were in 1st to 4th week and 19 cases were in 17th to 20th gestational week. The least number of cases i.e. only 15 were being diagnosed during 17th to 20th week (Table 5 and Figure 5).
| Gestational week | No. of patients | % of patients |
|---|---|---|
| 1st-4th | 28 | 17.4 |
| 5th-8th | 65 | 40.4 |
| 9th-12th | 34 | 21.1 |
| 13th-16th | 19 | 11.8 |
| 17th-20th | 16 | 9.87 |
Table 5: The percentage of patients being diagnosed with GDM and the time of diagnosis.
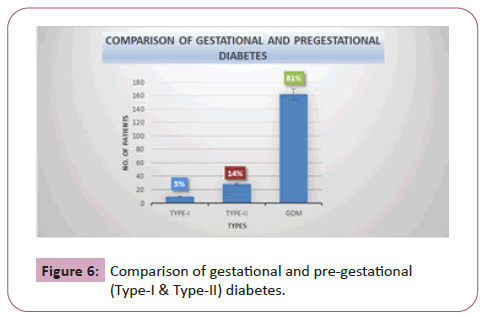
In the current study we compared the prevalence of gestational and pregestational diabetes in pregnant women. Out of 200 patients, majority of the cases were of GDM i.e. 162 (81%). The remaining cases (19%) were of pregestational diabetes i.e. type I or Type II DM. 28 (5%) cases were being presented with Type I DM while 10 (14%) patients with Type II DM as shown in Figure 6 (Table 6).
| Type of diabetes | No. of patients | % of patients |
|---|---|---|
| Type I | 10 | 5 |
| Type II | 28 | 14 |
| GDM | 162 | 81 |
Table 6: Comparison of pre-gestational (type I, type II) and gestational diabetes.
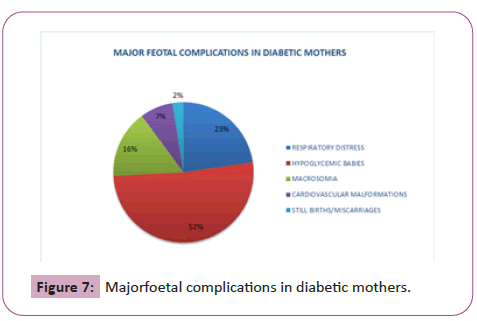
In our study population 159 patients had foetal/neonatal complications while the remaining pregnancies were normal and controlled. The major complicationsfound were macrosomia, hyperglycemia, CVS malformations, respiratory distress and still birth. Out of these, the most frequently occurring complication was hypoglycemic babies i.e. 52%. Then at second number was respiratory distress 23%, at third number wasmacrosomia 16%, at fourth number was CVS malformations 7% and the least prevailing complication was still birth/miscarriage i.e. 2% as shown in Figure 7 (Table 7).
| Major complications | No. of patients | % of patients |
|---|---|---|
| Respiratory distress | 36 | 23 |
| Hypoglycemic babies | 82 | 52 |
| Macrosomia | 25 | 16 |
| Cardiovascular malformations | 12 | 7 |
| Still births/Miscarriages | 4 | 2 |
Table 7: Major feotal complications in diabetic mothers.
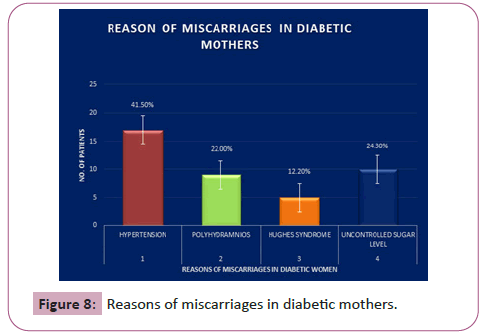
Out of 200 patients 41 patients had miscarriage due to one of the following reasons. The major reason of miscarriage in diabetic mothers was found to be hypertension and out of 41 cases there were 17 (41.5%) cases of miscarriage due to hypertension. There were 10 (24.3%) cases of miscarriage due extreme sugar level, 9 (22%) cases of miscarriage due to polyhydramnios and 5 (12.2%) cases of miscarriage due to Hughes syndrome as shown in Figure 8 (Table 8).
| Reasons of miscarriage | No. of patients | % of patients |
|---|---|---|
| Hypertension | 17 | 41.5 |
| Polyhydramnios | 9 | 22 |
| Hughes syndrome | 5 | 12.2 |
| Uncontrolled sugar level | 10 | 24.3 |
Table 8: Reasons of miscarriages in diabetic mothers.
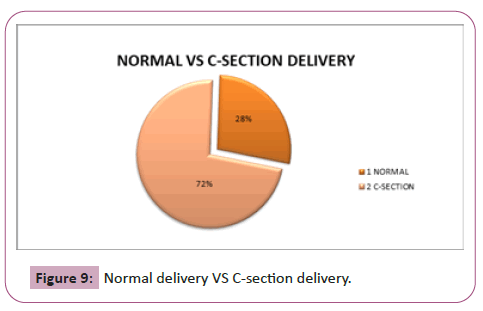
In our study population, the ratio of the normal and CS delivery was being determined.Out of 200 patients who were included in this study, 105 were being delivered during our study period 28% (29) cases were of normal delivery whereas 72% (76) cases were of C-section as shown in Figure 9 (Table 9).
| Mode of delivery | No. of patients | % of patients |
|---|---|---|
| Normal vaginal | 29 | 28 |
| Cesarean section | 76 | 72 |
Table 9: Normal delivery VS C-section delivery.
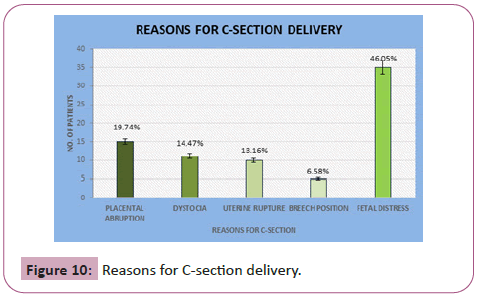
Out of 105 patients who were being delivered during our study period, there were 76 cases of CS. The major reasons of CS found out were as shown in the following figure. The major reason of CS was fetal distress and we found 35 (46.05%) such cases. Then at second place was the placental abruption with 15 (14.47%) cases, third major reason was dystocia with 11 (19.74%) cases and the fourth major reason was uterine rupture with 10 (13.16%) cases. The least reason of CS was breech position and we found only 5 (6.58%) such cases as shown in Figure 10 (Table 10).
| Reasons of CS | No. of patients | % of patients |
|---|---|---|
| Placental abruption | 15 | 14.47 |
| Dystocia | 11 | 19.74 |
| Uterine rupture | 10 | 13.16 |
| Breech position | 5 | 6.58 |
| Foetal distress | 35 | 46.05 |
Table 10: Reasons for C-section delivery.
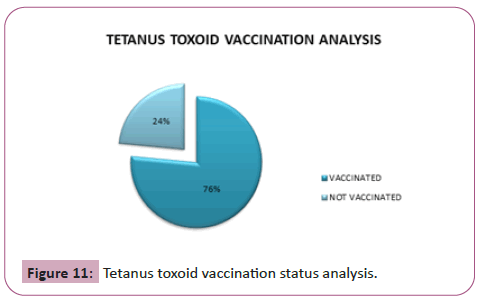
Our study population of 200 patients was also being analyzed to check their TT status. So 76% (153) of the pregnant ladies were found to be vaccinated for tetanus while 24% (47) of the pregnant women were not being vaccinated as shown in Figure 11 (Table 11).
| No. of patients | % of patients | |
|---|---|---|
| Vaccinated | 153 | 76 |
| Not vaccinated | 47 | 24 |
Table 11: Tetanus toxoid vaccination status analysis.
Discussion
This study was conducted to determine the occurrence of GDM and the birth complications in diabetic mothers. In the estimation of the prevalence of GDM during different gestational weeks, it was found out that although GDM manifests in all trimesters of pregnancy, but in majority of the cases GDM occur in early gestational weeks. Screening for GDM is usually performed around 24-28 weeks of gestational age. In a recent study a total of 4151 consecutive pregnant women irrespective of gestational weeks attending antenatal health posts across Chennai city underwent a 75 g OGTT (oral glucose tolerance test) recommended by WHO and diagnosed GDM if 2hr PG value ≥140 mg/dl. Observation in this study was that 38.7% women developed GDM even prior to 24th week of gestation [15]. Our results are very much similar to this study. So the OGTT must be performed in pregnant women prior to 24 weeks of gestation for better hyperglycemic control and to reduce the risk of birth complications.
During pregnancy, out of all types of diabetes most prevailing type is GDM. In the current study, 162 (81% of the total cases) women were presented with GDM, while with type I only 5% and with type II 14%. So the risk of GDM is more in Pakistan. A recent study analyzed 1,729,225 Canadian women and found that the prevalence of gestational and pregestational diabetes in 1996 was 2.7% and 0.4%, respectively [16]. In another study, rates of gestational diabetes (Class A1 combined with Class A2) and pregestational diabetes were 2.0% and 0.3% respectively [17]. Our results were similar to these studies in a sense that the ratio of gestational diabetes is more as compared to pregestational diabetes among pregnant women in Pakistan.
The maternal diabetes is associated with a large number of complications in foetus and neonate. Patients who cannot control their diabetes with diet and exercise only, require insulin, which leads to state of hyperinsulinemia in the foetus of such mothers. This and many other reasons lead to the foetal complications. Postnatal hypoglycemia, respiratory distress, macrosomia, CVS malformations and still births are major complications in the babies born to the diabetic mothers. The current study has shown that these complications are frequently occurring in the neonates and foetus of diabetic mothers. In recent years a study was performed to determine the range of complications occurring in infants of diabetic mothers. A total number of 40 babies were included in this study 35% new-borns presented respiratory distress and 8% were having CVS malformations. Hypoglycemia was noted in 50% [3]. Another study was being performed to compare the prevalence at live birth and the spectrum of cardiovascular malformations in infants born to diabetic mothers with that in infants of non-diabetic mothers. This study concluded that maternal diabetes is associated with a fivefold increase in risk of cardiovascular malformations. Transposition of the great arteries, truncus arteriosus, and tricuspid atresia are overrepresented to produce a substantial excess of these malformations [18]. All these previous studies strongly support our results.
Pregnancy affects both the maternal and fetal metabolism and even in non-diabetic women exerts a diabetogenic effect. Pregnancy loss is significantly higher among women with diabetes compared to the non-diabetic population. Neonatal mortality is also higher among infants of diabetic mothers in approximately 15-fold when compared to the general population [19]. Recently, a population-based cohort study conducted in the UK has shown that women with type1 diabetes have a higher risk of late fetal loss, presenting a four- to five-fold increase in perinatal death, and a four- to six-fold in stillbirth [20]. The major reasons of miscarriages in diabetic women include hypertension, Hughes syndrome, poly-hydramnios and uncontrolled sugar level; hypertension and preeclampsia being the root cause.
The prevalence of births worldwide complicated by DM is increasing. In the UK, for example, <25% of diabetic women have a non-instrumental vaginal delivery. Strikingly, more than half the CS in these patients was non-elective, but the reasons for this are not understood. This recent study tested the hypothesis that poor myometrial contractility as a consequence of the disease contributes to this high CS rate. There was significantly decreased contraction amplitude and duration in uteri from diabetic compared with control patients. There is poorer contractility even in the presence of oxytocin. The underlying mechanism is related to reduced Calcium channel expression and intracellular calcium signals and a decrease in muscle mass. This study concluded that these factors significantly contribute to the increased emergency CS rate in diabetic patients. It showed a high induction of labor rate (39%) and a high C-section rate (67%) in women with type I and type II DM as compared to 21% of the general maternal population [21]. These results strongly support our current study which showed that 72% of the total deliveries were through CS.
The rise in the rate of cesarean sections in diabetic mothers is due to widening of the relative indications, such as dystocia, previous cesarean, fetal distress and breech presentation. In a recent study increase in the cesarean rate of 6.2% points was partitioned according to five complications of delivery including previous cesarean delivery, breech presentation, dystocia, fetal distress, and all other complications. Nearly half (48%) of the increase was associated with previous cesarean delivery, 29 per cent with dystocia, 16 per cent with foetal distress, 5 per cent with breech presentation, and 2 per cent with all other complications [22]. In the current study we examined the recorded indications of the CS and most common of them were fetal distress, placental abruption, dystocia, uterine rupture and breech position respectively. Previous CS was also a reason of CS in index deliveries.
Tetanus is an acute, often fatal, disease caused by an exotoxin produced by Clostridium Tetani. It occurs in new-born infants born to mothers, who do not have sufficient circulating antibodies to protect the infant passively, by trans-placental transfer. Prevention may be possible by the vaccination of pregnant or non-pregnant women, or both, with tetanus toxoid, and the provision of clean delivery services. Tetanus toxoid consists of a formaldehyde-treated toxin which stimulates the production of antitoxin. Recently a study was conducted to determine the TT vaccination status for pregnant women, and to examine the effects of various factors on TT vaccination coverage during pregnancy in reproductive-age women in Turkey. Four-hundred and ninety-three postpartum women who had live births at a hospital in Ankara were interviewed and information was collected on the mothers' socio-demographic characteristics, TT vaccination history, and prenatal care during the pregnancy studied. The rates for no vaccination, one-dose vaccination, and two-dose vaccination were 53.3%, 18.9%, and 27.8%, respectively [23]. While in the current study, 76% of the screened women were being vaccinated with tetanus toxoid. This fact shows that maternal vaccination status is much better in Pakistan, but still more public awareness is required to boost up the rate of maternal vaccination in our country.
Conclusion
Diabetes is still a major problem of birth complications and miscarriages in Pakistan. In the current study we concluded that during pregnancy GDM is the most prevailing type of diabetes and it is associated with major birth complications including respiratory distress, hypoglycemic babies, macrosomia, CVS malformations and even miscarriages. Most of our patients were being diagnosed with GDM before 24th week of gestation. So a public awareness program is required to educate the people about reproductive health and to motivate them to undergo BSR/FBS during pregnancy prior to 24th gestational weeks to diagnose for GDM. This will lead to the better glycemic control during pregnancy and decreased incidence of birth complications and miscarriages as according to our current study the major reason of miscarriages in diabetic mothers are hypertension and uncontrolled sugar level. From the current study we also concluded that the women being vaccinated with TT are still at risk of GDM.
References
- Inzucchi SE, Sherwin RS (2011) Type 1 diabetes mellitus. Cecil Medicine (24th edn) Philadelphia, Pa: Saunders Elsevier.
- Al-Hakeem MM (2006) Pregnancy outcome of gestational diabetic mothers: Experience in a tertiary centre. J Fam Community Med 13: 55-59.
- Al-Qahtani S, Heath A, Quenby S, Dawood F, Floyd R, et al. (2012) Diabetes is associated with impairment of uterine contractility and high Caesarean section rate. Dabetologia 55: 489-498.
- Alam M, Raza SJ, Sherali A, Akhtar A (2006) Neonatal complications in infants born to diabetic mothers. JCPSP 16: 212-215.
- Stogdale L (1986) Definition of diabetes mellitus. The Cornell Veterinarian 76: 156-174.
- Association AD (2010) Diagnosis and classification of diabetes mellitus. Diabetes Care 33: S62-S69.
- Cudworth A (1978) Type I diabetes mellitus. Diabetologia 14: 281-291.
- Edelman SV (1997) Type II diabetes mellitus. Advances in Internal Medicine 43: 449-500.
- Soria B, Roche E, Berna G, León-Quinto T, Reig JA et al. (2000) Insulin-secreting cells derived from embryonic stem cells normalize glycemia in streptozotocin-induced diabetic mice. Diabetes 49: 157-162.
- Landon MB, Gabbe SG (2011) Gestational diabetes mellitus. Obstetrics and Gynecology 118: 1379-1393.
- Kjos SL, Buchanan TA (1999) Gestational diabetes mellitus. N Engl J Med 341: 1749-1756.
- Kopp W (2005) Role of high-insulinogenic nutrition in the etiology of gestational diabetes mellitus. Medical Hypotheses 64: 101-103.
- Kühl C, Hornnes PJ, Andersen O (1985) Review: Etiology and pathophysiology of gestational diabetes mellitus. Diabetes 34: 66-70.
- Reece EA, Leguizamón G, Wiznitzer A (2009) Gestational diabetes: The need for a common ground. The Lancet 373: 1789-1797.
- Seshiah V, Balaji V, Balaji MS, Paneerselvam A, Arthi T, et al. (2007) Gestational diabetes mellitus manifests in all trimesters of pregnancy. Diabetes Res. Clin 77: 482-484.
- Wen SW, Liu S, Kramer MS, Joseph K, Levitt C, et al. (2000) Impact of prenatal glucose screening on the diagnosis of gestational diabetes and on pregnancy outcomes. Am. J. Epidemiol 152: 1009-1014.
- Sheffield JS, Butler-Koster EL, Casey BM, Mcintire DD, Leveno KJ (2002) Maternal diabetes mellitus and infant malformations. Obstetrics and Gynecology 100: 925-930.
- Wren C, Birrell G, Hawthorne G (2003) Cardiovascular malformations in infants of diabetic mothers. Heart 89: 1217-1220.
- Hawthorne G, Robson S, Ryall E, Sen D, Roberts S, et al. (1997) Prospective population based survey of outcome of pregnancy in diabetic women: results of the Northern Diabetic Pregnancy Audit, 1994. BMJ 315: 279-281.
- Casson I, Clarke C, Howard C, Mckendrick O, Pennycook S, et al. (1997) Outcomes of pregnancy in insulin dependent diabetic women: results of a five year population cohort study. BMJ 315: 275-278.
- Al-Qahtani S, Heath A, Quenby S, Dawood F, Floyd R, et al. (2012) Diabetes is associated with impairment of uterine contractility and high Caesarean section rate. Dabetologia 55: 489-498.
- Taffel SM, Placek PJ, Liss T (1987) Trends in the United States cesarean section rate and reasons for the 1980-85 rise. Am. J. Public Health 77: 955-959.
- Maral I, Baykan Z, Aksakal FN, Kayikcioglu F, Bumin MA (2001) Tetanus immunization in pregnant women: Evaluation of maternal tetanus vaccination status and factors affecting rate of vaccination coverage. Public Health 115: 359-364.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences