Primary Vaginal Melanoma in a Young Woman
Asaggau S*, Badraoui MB, Zouita B, Basraoui D and Jalal H
Centre Hospitalier Universitaire Mohammed VI Marrakech, Gueliz, Morocco
- *Corresponding Author:
- Salma Asaggau
Junior Radiologist
Centre Hospitalier Universitaire Mohammed VI Marrakech
Gueliz, Morocco
Tel: 2120678968645
E-mail: salmaasaggau@gmail.com
Received Date: 30 August, 2018; Accepted Date: 24 September, 2018; Published Date: 01 October, 2018
Citation: Asaggau S, Badraoui MB, Zouita B, Basraoui D, Jalal H (2018) Primary Vaginal Melanoma in a Young Woman. J Oncopathol Clin Res 2:6.
Abstract
Primary vaginal melanoma is a rare and very aggressive tumor. It is most often diagnosed in late-stage menopausal women with visceral metastasis. We report an exceptional case of a 31-years-old woman with primary vaginal melanoma diagnosed at an early stage on pelvic MRI without revelation of a secondary lesion.
Objective: Interest of MRI in early positive diagnosis and loco-regional extension assessment of vaginal melanoma.
Keywords
Melanoma; Vagina; MRI; Extension assessment
Introduction
Primary vaginal melanoma is an extremely rare tumor. It accounts for about 3% of cases of vaginal cancer. It affects menopausal women with an average age of 55 years. We report the case of a primary vaginal melanoma in a young woman of 31 years.
Clinician Case
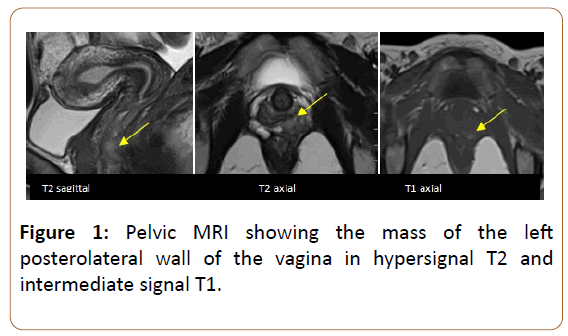
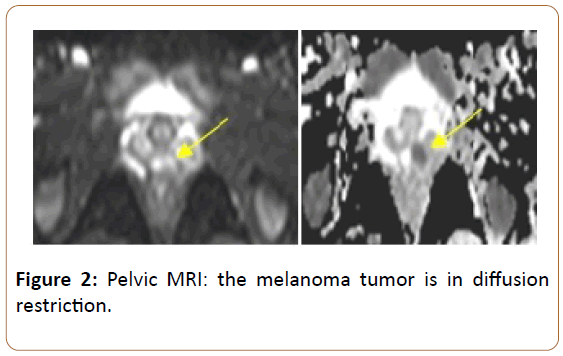
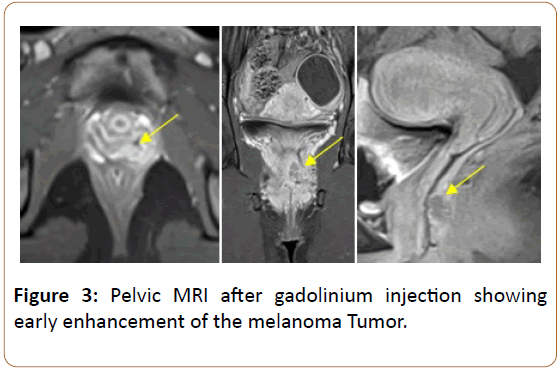
Old woman of 31-years without a notable personal or family history, particularly clinical dermatological examination is without particularity. She consulted for metrorrhagia of low abundance. The patient underwent pelvic MRI which revealed a small mass of the left posterolateral wall of the vagina at the 1/3 mid-1/3 lower junction, located 11 mm from the hymenal orifice, measuring 16 x 6 x 13 mm, fuzzy irregular outlines, T2 hypersignal, T1 intermediate signal, (Figure 1) and ADC restriction diffusion hypersignal (Figure 2), taking the contrast early after gadolinium injection (Figure 3).
Figure 2: Pelvic MRI: the melanoma tumor is in diffusion restriction.
This lesional process infiltrates the neighboring para-vaginal fat, and comes into contact with the anterior wall of the anal canal and the levator of the left anus, associated with bilateral iliac and inguinal ganglia. A mass biopsy was in favour of vaginal melanoma. The patient benefited from an enlarged partial colpectomy with a repeat of vaginal continuity followed by brachytherapy sessions. Radiological extension assessment included thoracoabdominopelvic CT and cerebral CT showed no secondary lesion.
Discussion
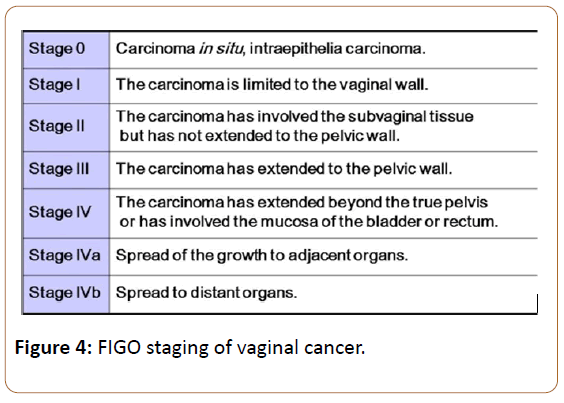
Malignant melanoma of the mucous membranes is an extremely rare and very aggressive tumor. It represents 0.03% of all cancers [1], less than 4% of vaginal cancers [2] and less than 1% of melanomas are located in the vagina. The tumor of vaginal melanoma is most often located in the lower third (58%), and in the anterior wall (45%) [3]. Call signs are varied and dominated by metrorrhagia and palpation of a mass. Clinically, the tumor may be uni or multifocal, sometimes pigmented. Analysis of cases of primary vaginal melanoma reported in the literature shows that they most often occur in the late fifties [4-8]. MRI is the adjuvant useful in lesional exploration in the initial diagnosis. It specifies the seat of the lesion, the size, the limits, its loco-regional relations, and the enhancement after injection of gadolinium. Differential diagnosis in imaging in front of a small, well-defined, single-vaginal mass in the vagina should first suggest the superinfected Gartner cyst, epidermoid inclusion cysts, and squamous cell carcinoma. The confirmation of the diagnosis is histological and uses the immunohistochemical study. The immunohistochemical characteristics are similar to those of cutaneous melanomas. The tumor markers used to confirm the diagnosis are the anti-Melan a antibody, anti-S100 protein, and the HMB45 antibody, the latter being more specific for the melanoma cell. The use of both antibodies is desirable. More recently, other more selective antibodies of the melanocyte line are used: NK1/C-3 and NK1BETEB [9]. Once the diagnosis of melanoma is made, it remains to prove its primitive nature. This involves the search for primary cutaneous, ophthalmological, digestive ENT or a history of previous excision of a pigmented skin lesion [9]. Pelvic MRI remains the gold standard for assessing loco-regional extension status and post-treatment surveillance. It is based on the TNM-FIGO classification (Figure 4). Most authors, such as Mordel et al. advocate the use of the International Federation of Gynecologists and Obstetricians (FIGO) system [9] for staging, as melanoma is often diagnosed at a late stage and has a clinical presentation and a mode of extension quite comparable to vaginal carcinoma. Thoracoabdominopelvic CT is useful in the assessment of extension to solid organs and the analysis of ganglionic areas. The prognosis of melanomas also depends on the thickness of the tumor according to the Breslow ++ index, the depth invasion (Clark or Chung levels) and the ganglionic status [6]. However, after a review of 115 cases of vaginal melanoma, Reid et al. retained size as the only prognostic factor with a threshold value of 3 cm [9]. Depending on the anatomical location and the technical possibilities, a large conservative excision followed by radiotherapy and/or brachytherapy in case of incomplete excision will be weighed against a hysterectomy with colpectomy [2,7]. INCa recommendations concerning treatments systemic (chemotherapies, targeted therapies, immunotherapy) and locoregional management of metastatic melanoma have been established. The genetic profile justifies the search for mutations of the c-KIT and NRAS genes in addition to BRAF. The presence of c-KIT mutations may justify the use of c-KIT-specific tyrosine kinase inhibitors, and that of NRAS mutations the use of MEK inhibitors [10,11]. Despite the different types of treatments proposed, the prognosis of vaginal melanoma remains reserved with a survival rate at 5 years of 5 to 10% [8]. This is due mainly to the richness of the vascular and lymphatic network in the vagin.
Conclusion
Primary vaginal melanoma is a rare condition. The diagnosis is most often at a late stage. Primary interest of pelvic MRI to positively diagnose spread assessment and thus improves prognosis.
References
- Patrick RJ, Fenske NA, Messina JL (2007) Primary mucosal melanoma. J Am Acad Dermatol 56: 828-834.
- Vaysse C, Pautier P, Filleron T, Maisongrosse V, Rodier JF, et al. (2013) A large retrospective multicenter study of vaginal melanomas: implications for new management. Melanoma Res 23: 138-146.
- Mihajlovic M, Vlajkovic S, Jovanovic P, Stefanovic V (2012) Int J Clin Exp Pathol 5: 739-753.
- McLaughlin CC, Wu XC, Jemal A, Martin HJ, Roche LM, et al. (2005) Incidence of non-cutaneous melanomas in the US. Cancer 103: 1000-1007.
- Buchanan DJ, Schlaerth J, Kurosaki T (1998) Primary vaginal melanoma: 13 year disease free survival after wide local excision and review of recent literature. Am J Obstet Gynecol 178: 1177-1184.
- Balch CM, Gershenwald JE, Soong SJ, Thompson JF (2009) Final version of AJCC melanoma staging and classification. J Clin Oncol 27: 199-206.
- Piura B (2008) Management of primary melanoma of the female urogenital tract. Lancet Oncol 9: 973-981.
- Gauthier T, Uzan C, Gouy S, Kane A (2012) Mélanome vaginal : une localisation particulièrement défavorable. Gynécologie Obstétrique et Fertilité 40: 273-278.
- Bennani A, El Fatemi H (2013) Le mélanome primitif de la muqueuse génitale féminine: à propos de trois observations et revue de literature. The Pan African Medical J 16: 58.
- Hars B, Dalac-Rat S (2015) Mélanomes muqueux vulvaires et vaginaux: étude clinique, histologique et moléculaire de 22 cas. Annales de Dermatologie et de Vénéréologie 142: p664.
- Wylomanski S, Denis M, Theoleyre S (2017) Profil mutationnel de mélanomes de la sphère génitale féminine: résultats d’une cohorte monocentrique. Annales de Dermatologie et de Vénéréologie 144: S312-S313.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences