Challenges of Early Stroke Admission Management in Tropical Setting
1Neurology Department, University of Lome, Togo
2Neurology Service, Ignace Deen University Teaching Hospital of Conakry, Guinea
3Neurology Service, Campus University Teaching Hospital, Togo
4Neurology Service, University Teaching Hospital of Douala, Cameroon
- Corresponding Author:
- Komi Assogba
Neurology Department
University of Lome, Togo
Tel: +22890086646
E-mail: chocob400@gmail.com
Received Date: March 06, 2019; Accepted Date: March 21, 2019; Published Date: March 28, 2019
Citation: Assogba K, Cisse FA, Lamine S, Sidibe B, Foksouna S, et al. (2019) Challenges of Early Stroke Admission Management in Tropical Setting. Neurol Sci J Vol.3 No.1:1
Copyright: © 2019 Assogba K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Stroke remains the first leading cause of hospitalizations and adult disabilities, and second cause of death in Africa. The hyperacute management of stroke in tropical setting is still an enigma despite established guidelines.
Objective: To determine the gaps in the management of stroke, within a context of limited healthcare resources regarding the international stroke guidelines.
Methods: We have recorded all patients admitted to the neurology department of University Hospital via the Intensive Care Unit for stroke. The evaluation criteria were concerned the case notification, admission time, epidemiological data, clinical signs, CT scan performing and outcome.
Results: A total of 183 patients out of 340, were hospitalized for stroke, including 131 cases (71.58%) of cerebral ischemia and 52 cases (28.42%) of haemorrhage. Accessibility means to the CT scan was 53.82%. The average age was 63.96 ± 12.72 with a male predominance (102 men and 81 women). The admission average time was 3.7 days. The time of first clinical examination was noted in 154 cases (84.15%). The mean time to receive in hospital first cares was 25 minutes. The neurological evaluation by the NIHSS was done in 71 cases and Glasgow score scale in 106 cases. The brain CT scan was performed in all patients with 61 cases within 24 hours. The average time to perform brain imaging was 3.5 days. The hospital length of stay was 19.5 days. The hospital mortality rate was 52%.
Conclusion: The study let appear the wide gaps between our in local context practices and the international stroke guidelines.
Keywords
Admission; Epidemiology; Intensive care; Stroke management
Introduction
Stroke is a devastating disease and currently fallen from the third to the fourth leading cause of death in the world [1-3]. Epidemiological data are sparse and vary worldwide with an incidence of 58 to 243/100 000 [4,5]. Stroke accounted for 56% of hospitalizations, second level of death and first leading cause of adult disabilities in Africa [6-8].
Following the arrival of a potential stroke patient to the Intensive Care Unit (ICU), patients should be stabilized and undergo assessment for potential treatment [9,10]. The hyperacute management of stroke in tropical setting is still an enigma despite permanent revised established guideline [11,12]. Classically these difficulties are related to the absence of stroke registers, specialists, technical platform and stroke pathway system [13,14].
The stroke pathway emergency medical system as per new recommendation includes early admission, clinical exam and CT scan or MRI performing to establish stroke diagnostics with respect of timing goals treatment [15-17].
The neurological status at the initial presentation and the interval between onset and therapeutic intervention contribute to the prognosis and improve optimal patient outcomes [18,19]. The aim of this study was to report the gaps between our clinical daily practices regarding the stroke acute management recommendations.
Material and Methods
This study was conducted in the ICU and neurology departments of Ignace Deen University Hospital. This tertiary hospital is the national referral center for the management of neurological emergencies. A retrospective study was conducted from January to December 2017, by reviewing patient records from arrival in emergency room to discharge from hospital. The study involved all records of admitted patients to the neurology department via the Intensive Care Unit for brain imaging-confirmed stroke during the study period. The evaluation criteria were those established by previous authors [7,8,12]. Two residents performed data collection and data entry on the Excel table. The data were collected on a survey sheet using stroke emergency admission guideline. Patients excluded were those without brain imaging and or those with transient ischemic attack (TIA).
The SPSS 13.0 Software allowed the descriptive analysis of these data as well as the use of the Chi2 test (or the exact Fischer test required) for comparisons of qualitative variables; and Student test (or Mann-Whitney test if necessary) for comparisons of quantitative variables. The results are expressed as mean, +/- standard deviation or percentages. A value of P <0.05 was considered statistically significant.
Results
During the study period, 1423 patients were admitted at the emergency department of the tertiary of hospital. Three hundred and forty cases were clinically suspected for stroke. Only 183 had undergone the cerebral imaging, giving a CT scan accessibility rate of 53.82%. The stroke was confirmed with a prevalence of 5.27%. Patients aged from 23 to 100 years old (mean = 63.96 ± 12.72 years). The study population had included 102 men (55.74%) and 81 women (44.26%) with a sex ratio of 1.34. Thirty-six patients came from the big city (48%), 33.3% came from the semi-urban area and 18.7% came from the rural area. Ischemic strokes accounted for 75.58% (131 patients), cerebral hemorrhages were seen in 52 cases (28.42%).
Before admission
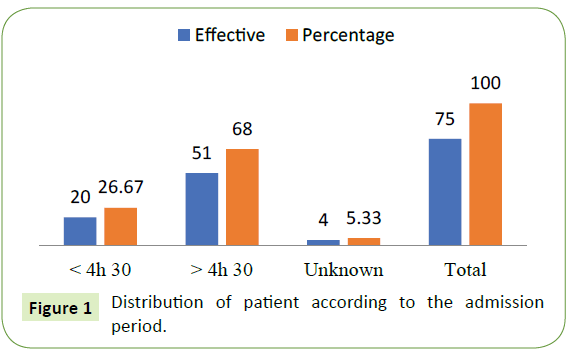
The notification cases by calling emergency toll-free number were carried out in 24 out of 183 cases (13.11%) after the onset of symptoms. Forty-nine (65.33%) patients arrived at the hospital by public transport, 58 cases (31.70%) by personal car and only 5 (2.73%) patients arrived with medicated ambulance. The average admission time was 3.7 Day (3D16h48') with a median of 7.5 days (7D12h), (Figure 1).
Intensive care unit (ICU)
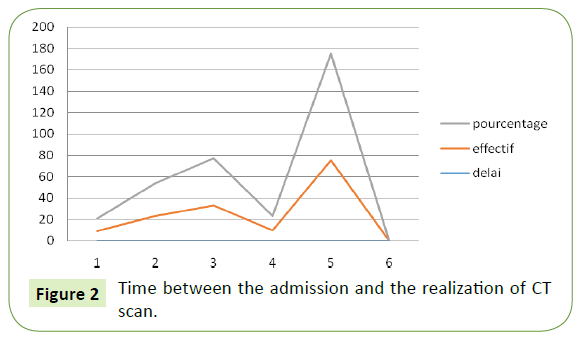
The brain CT scan was performed in all patients. No patient had the CT scan before 3 hours. Only 23 patients (12.57%) had CT scan within 24 hours, and 105 patients (57.38%) after 72 hours. The average time to perform brain imaging was 3.5 days, (Figure 2).
The time of the clinical examination was noted in 154 cases (84.15%). The admission time before 4:30 was respected in 49 cases (26.78%). The mean time to receive in hospital first cares was 25 ± 17 minutes. The vital parameters (blood pressure, temperature, breath and heart rates) were collected in all cases. Oxygen saturation was noted in only 32 cases (17.49%). At admission, the NIHSS score was noted in only 71 cases (38.80%). The swallowing test was assessed in 61 cases (33.33%). The Glasgow score scale was noted in 145 cases with 12% of stage 3.
Additional tests
The ECG recording was performed urgently in 105 cases (57.38%) and the analysis was included in the patient file in only 93 cases (50.82%). Holter ECG was done in 27 cases (14.75%). Ultrasonography of the supra aortic trunk was performed in 106 ischemic stroke patients (57.92%). No patient had performed a brain MRI during hospitalization period.
In hospital care and evolution
For ischemic stroke, blood pressure has been respected in 111 cases (60.65%) and decreased in 72 cases (39.34%) before admission to the ICU. For hemorrhagic stroke, the objective of 140/90 mmhg was only achieved in 24 cases (46.15%). The risk factors were dominated by high blood pressure with 151 cases (82.51%), followed by age> 50 years, 95 cases (51.91%), and smoking in 18.67% of cases. Diabetes and embolic heart disease accounted for 32 cases (17.49%) each. Only 50.6% of patients had received functional rehabilitation and speech therapy. Prevention of thromboembolic complications was only performed in 34 cases (18.18.58%). Thromboembolic drugs and aspirin therapy were administrated in ischemic stroke and symptomatic treatment in hemorrhagic stroke. All patients had received risk factors management controlled. No patient had met thrombolysis selected criteria.
The main complications were due to lung and skin sepsis, large brain hematomas and malignant cerebral infarct. The average length of stay was 19.5 days. In 54.7% the financial support was done by the family and only 14.7% of the patients had benefited from a health insurance. We had recorded 96 deaths (52.46%). A total of 81(44.26%) deaths were observed in ischemic stroke and 15 (8.2%) deaths in hemorrhagic stroke. There is no significant difference in the two groups, but this high mortality is correlated with the delayed in consultation, the age> 50 years, and the sepsis p <0.05.
Discussion
The study had shown that there are major gaps in stroke management in our country at all stages. The work had permitted to identify the weakness of all the care facilities management support system. The notification of stroke symptoms by free calling admission was only done in 10 cases, which explain why most patients arrived at the emergency by public transport without any medical support. This notification is a recent introduction in our country following the Ebola outbreak, but it is underused regarding serious and lethal pathologies such as stroke. Most of the time, acute cases may be drive to traditional healers and some of them may die during transfer to appropriated care facilities. The ignorance of the warning signs in the event of stroke by the populations and the lack of an organized stroke pathway medical system are the explanations of these insufficiencies and the underuse of the free calling tool. Another drawback of the retrospective studies is that care can be performed but not fulfilled in patient recorded file leave these sheets useless. The average time for intra-hospital first cares was 25 minutes despite the urgency of the pathology. The lack of an organized in hospital admission pathway system, long waiting time in the emergency unit due to technical insufficiency and unavailability of medicated transport equipment are the reasons for this delay in medical first care with heavy complications and deaths [14,20].
Two-point six percent of patients arrived at the hospital medicated ambulance. Public transport is the most used mode of patient transportation. An alternative to public transport is the transport by personal car by the entourage with 32% of the patients. Only 49 recorded patients (26.78%) were admitted before 4.30 hours, the required time for thrombolysis therapy, if the remains condition were achieved such as computed tomography, drugs accessibility and specialist availability. Population more education and awareness of stroke symptoms could be a solution for early first care delivery before 4.30 hours. The average admission time was 3.7 days whereas in the previous reported study from developed countries, this time was 15 hours [21,22]. The long admission time is related to many factors because more than half of patients travel from long distances to access emergency care unit, using of public transport in most cases, and the lack of knowledge regarding the awareness urgent signs of stroke condition by the population. This delay in consultation with unsafe transport has already been reported in several African countries, which was correlated at a very high mortality (82.9%) P <0.02. Of the 340 patients with clinically symptomatic stroke, 183(53.82%) had a brain scan. The health insurance is not obligatory in our country and the care in most of the cases is self-insured or by the family, and quite opposite to developed regions [17,21,23].
Etiological Assessments
The low rate of hemorrhagic strokes, 14.66%, in our series is related to a selection bias since half of the patients with clinically symptomatic stroke did not receive a CT scan examination and some patients die before admission to intensive care unit or those are admitted to traditional healers with to the seriousness of their clinical presentation. The average time to perform the brain imaging was 3.5 days while the guideline recommends a completion time <1 hour. At the time of the "Time is brain," efforts must be made to improve access to the CT scan, through universal medical coverage. CT scan is the cornerstone of stroke management in Africa. No patient received MRI for financial reasons. These insufficiencies remain the major challenge regarding stroke etiologies.
Concerning the management of the risk factors, for ischemic stroke, blood pressure has been controlled in 60.9%) and decreased in 39.06% before transferred to current in hospital.
These study findings raise the gaps regarding the diffusion of the international recommendations and their application in limited resources care facilities [12,24]. Frameworks with guidelines adapted to the developing countries seem necessary to improve the stroke first care considering the local conditions.
The hospital mortality rate of 52% was correlated with an age> 50 years, an admission delayed and the occurrence of sepsis with P<0.04. This mortality rate may be low if care facilities and caregivers followed the admission requirements criteria [11,25].
The stroke mortality rate is ranged from 33% to 46% per year in African countries, and this rate can reach 82.9% in comatose patients [18,26,27]. The prognosis of stroke in Africa is characterized by high mortality, heavy motor and cognitive impairment with variability of rates due to methodological differences, environmental conditions and duration of patient follow-up. At the discharge, 61% of patients had returned to their home after stroke and 24% to follow-up care unit and rehabilitation. Few studies exist on the conditions of return home and the after-hospital patient outcome. For many survivor patients, the alternative is to return home despite their bad feeling clinical condition in the absence of a follow-up care unit and rehabilitation facilities [12,13,19].
There is a great disparity between practices in developing University Hospital and the international recommendations task forces used in developed countries. The Neurovascular Unit or stroke center improves the vital and functional prognosis of patients suffering from stroke. This benefit is maintained until 10 years after the stroke. These units would also reduce the length of hospital stay, the direct cost of stroke management and the mortality from 28% to 23% [28,29].
Further studies are needed to better identify the shortcomings of stroke in our country and the establishment of the stroke medical pathway system to improve functional prognosis and reduce mortality rate in care facilities.
Conclusion
The study shows the close link between the quality of prehospital first cares and the poor prognosis of stroke patients in our country without stroke center system. It carried out all great disparities between our local practices in line with and international recommendations. It also raises the question of the feasibility of these guidelines in our local conditions and the need for recommendations adapted to developing countries.
References
- Boulanger JM, Lindsay MP, Gubitz G, Smith EE, Stotts G, et al. (2018) Canadian Stroke Best Practice Recommendations for acute Stroke Management: Prehospital, Emergency Department, and Acute Inpatient Stroke Care, 6th Edition, Update 2018. Int J Stroke 13: 949-984.
- Ogun SA, Oluwole O, Fatade B, Ogunseyinde AO, Ojini FI, et al. (2002) Comparison of Siriraj stroke score and the WHO criteria in the clinical classification of stroke subtypes. Afr J Med Sci 31: 13-6.
- Jauch EC, Huang AY, Gardner DJ, Blum JL (2018) Strategies for improving outcomes in the acute management of ischemic stroke in rural emergency departments: a quality improvement initiative in the Stroke Belt. Emergency Medicine 10: 53-9.
- Sarah Song (2013) Hyperacute Management of Ischemic Stroke. Semin Neurol 33: 427-435.
- Lackland DT, Roccella EdJ, Deutsch A, Fornage M, George MG, et al. (2014) Factors Influencing the Decline in Stroke Mortality: A Statement from the American Heart Association/American Stroke Association. Stroke 45: 315–20.
- Towfighi A, Saver JL (2011) Stroke declines from third to fourth leading cause of death in the United States: historical perspective and challenges ahead. Stroke 42: 2351–5.
- Schuberg S, Song S, Saver JL, Mack WJ, Cen SY, et al. (2013) Impact of emergency medical services stroke routing protocols on primary stroke center certification in California. Stroke 44: 3584–6.
- Damush TM, Ofner S, Yu Zh, Plue L, Nicholas Gl, et al. (2011) Implementation of a stroke self-management program, A randomized controlled pilot study of veterans with stroke. TBM 1: 561–72.
- Jovin TG, Albers GW, Liebeskind DS, STAIR IX Consortium (2016) Stroke Treatment Academic Industry Roundtable: The Next Generation of Endovascular Trials. Stroke 47: 2656–65.
- Khatri R, Vellipuram AR, Maud A, Cruz-Flores S, Rodriguez GJ, et al. (2018) Current Endovascular Approach to the Management of Acute Ischemic Stroke. Curr Cardiol Rep 20: 46-50.
- Higashida R, Alberts MJ, Alexander DN, American Heart Association Advocacy Coordinating Committee, Crocco TJ, et al. (2013) Interactions within stroke systems of care: a policy statement from the American Heart Association/American Stroke Association. Stroke 44: 2961–84.
- Alberts MJ, Latchaw RE, Jagoda A, Brain Attack Coalition, Walker MD, et al. (2011) Revised and updated recommendations for the establishment of primary stroke centers: a summary statement from the brain attack coalition. Stroke 42: 2651–65.
- Song S, Saver J (2012) Growth of regional acute stroke systems of care in the United States in the first decade of the 21st century. Stroke 43: 1975–8.
- Xian Y, Holloway RG, Chan PS (2011) Association between stroke center hospitalization for acute ischemic stroke and mortality. JAMA 305: 373–80.
- Rosamond WD, Gorton RA, Hinn AR, Hohenhaus SM, Morris DL, et al. (1998) Rapid response to stroke symptoms: The Delay in Accessing Stroke Healthcare (DASH) study. Acad Emerg Med 5: 45–51.
- Prabhakaran S, O’Neill K, Stein-Spencer L, Walter J, Alberts MJ, et al. (2013) Prehospital triage to primary stroke centers and rate of stroke thrombolysis. JAMA Neurol 70: 1126–32.
- Kim J, Thrift AG, Nelson MR, Bladin ChF, Cadilhac DA, et al. (2015) Personalized medicine and stroke prevention: where are we? Vascular Health Risk Management 11: 601–611
- Adoukonou TA, Vallat JM, Joubert J, Macian F, Kabore R, et al. (2010) Strokes management in sub-Saharan Africa. Rev Neurol (Paris) 166: 882–93.
- Sene-Diouf F, Mapoure NY, Ndiaye M, Ngahana HBM, Toure K, et al. (2008) Survival of comatose stroke in Dakar Rev Neurol (Paris) 16: 452-8.
- Danesi M, Okubadedjo N, Ojini F (2007) Prevalence of stroke in an urban and mixed-income community in Lagos, Nigeria. Neuroepidemiology 28: 216–23.
- Cisse A, Kourouma S, Barry SD, Cisse FA (2009) Stroke at University Hospital of Ignace Deen. Guinée Médicale 2: 33-9.
- Mathieu-Blondet A, Malet A, Devy R, Causeret M, Rouquette A, et al. (2008) Evaluation of care delivered to stroke patients in a French hospital. Santé publique 20: 561-74.
- Sagui E, M'Baye PS, Dubecq C, Ba FK, Niang A, et al. (2005) Ischemic and hemorrhagic strokes in Dakar, Senegal: a hospital-based study. Stroke 36: 1844-7.
- Miyahara M, Noda R, Yamaguchi S, Tamai Y, Inoue M, et al. (2018) New Prediction Score for Hematoma Expansion and Neurological Deterioration after Spontaneous Intracerebral Hemorrhage: A Hospital-Based Retrospective Cohort Study. J Stroke Cerebrovasc Dis 27: 2543-2550.
- Kidd L, Maggie L, Booth J, Rowat A, Russell S, et al. (2015) Development and evaluation of a nurse led, tailored stroke self-management intervention. BMC Health Services Research 15: 359.
- Woimant F, de Broucker T, Vassel P (2003) Management of stroke in France. Rev Neurol (Paris) 159: 543-551.
- Fonarow GC, Gregory T, Driskill M, Mark D, Stewart, et al. (2010) Hospital certification for optimizing cardiovascular disease and stroke quality of care and outcomes. Circulation 122: 2459–2469.
- Rost NS, Smith EE, Pervez MA, Mello P, Dreyer P, et al. (2012) Predictors of increased intravenous tissue plasminogen activator use among hospitals participating in the Massachusetts Primary Stroke Service Program. Circ Cardiovasc Qual Outcomes 5: 314–20.
- Diatewa JE, Kombate D, Dongmo J-J, Apetse K, Assogba K, et al. (2018) A Prognostic Challenge of Brainstem Stroke for the Countries of Sub-Saharan Africa: Case of Togo. Clinical Neurology and Neuroscience 2: 61-67.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences