Blast Scaling Parameters: Transitioning from Lung to Skull Base Metrics
Lucke-Wold B1*, Ryan CT1, Ogaga U1, Aric FL2 and Charles LR1
1Department of Neurosurgery, West Virginia University, Morgantown, WV, USA
2Department of Psychiatry, University of Washington, Seattle, WA, USA
- *Corresponding Author:
- Lucke-Wold B
Department of Neurosurgery, West Virginia University
Morgantown, WV, USA
Tel: 304 293-5041
E-mail: bwold@mix.wvu.edu
Received Date: December 22, 2016; Accepted Date: January 04, 2017; Published Date: January 10, 2017
Citation: Lucke-Wold B, Ryan CT, Ogaga U, et al. (2017) The Effects of Hepatic Ischemia-Reperfusion Injury on Postoperative Cognitive Function in Elderly Patients. J Surgery Emerg Med 1:1.
Copyright: © 2017 Lucke-Wold B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Neurotrauma from blast exposure is one of the single most characteristic injuries of modern warfare. Understanding blast traumatic brain injury is critical for developing new treatment options for warfighters and civilians exposed to improvised explosive devices. Unfortunately, the pre-clinical models that are widely utilized to investigate blast exposure are based on archaic lung based parameters developed in the early 20th century. Improvised explosive devices produce a different type of injury paradigm than the typical mortar explosion. Protective equipment for the chest cavity has also improved over the past 100 years. In order to improve treatments, it is imperative to develop models that are based more on skull-based parameters. In this minireview, we discuss the important anatomical and biochemical features necessary to develop a skull-based model.
Keywords
Blast traumatic brain injury; Skull-based scaling; Clinically relevant models; Anatomical correlates; Biomarkers
Introduction
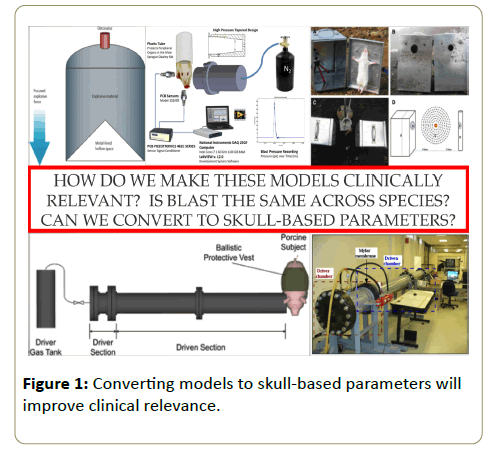
Blast traumatic brain injury (bTBI) has been deemed the hallmark of modern warfare [1]. Unfortunately, limited treatment options exist to help warfighters who sustain bTBIs during conflict. In order to improve treatment options, it is imperative that pre-clinical models be designed to emulate real-time injury as closely as possible (Figure 1). The current models are primarily based off of lung-based scaling parameters developed back in the early 20th century [2]. Modern day improvised explosive devices however produce a different type of injury than the mortar shell explosions typical of the World Wars. In this mini-review, we discuss the relevant parameters for switching from lung-based scaling to the more relevant skull base metrics. By establishing better models going forward, it will be possible to better test pharmaceutical treatments that will directly help patients with bTBI.
Anatomical Features
A recent literature review of blast exposure reports that 19.6 to 40% of victims, depending on the study, have injuries to the face [3]. Concurrent evidence from a porcine model also shows that face injury is common [4]. Head on blast exposure that injures the face in humans causes wave propagation through surrounding tissue into the brain [5]. Evidence of wave collision with the brain can be measured by increased intracranial pressure [6]. Singh and colleagues have shown that the location of exposure changes the extent of wave propagation into the brain [7]. The wave also dissipates as is travels throughout the brain indicating some intrinsic resistance [8]. Head orientation is also directly correlated with intracranial pressure changes following blast [9]. It is therefore imperative that when designing scaled blast models important variables should be addressed including distance from exposure, intensity of exposure, and location of primary impact [10]. Below we discuss scaling principles in accordance to anatomical features. We begin at the macroscopic level with consideration for the skull, brain, cerebrospinal fluid, and vasculature. The discussion progresses to a focus on the role of cell types in scaling including neurons, glia, and endothelial cells.
Skull dynamics
Characteristics of the skull tend to be more variable between species, particularly in regard to morphology and shape. For this reason, other skull characteristics must be considered when selecting the appropriate animal model to represent human skulls. It is most widely agreed that bone mineral density is the most important characteristic due to its direct correlation to bone elasticity and strength [11]. A recent study by Jean and colleagues investigated stress wave transmission through the skull interface of three species: mouse, pig, and human. They found distinct patterns of transmission based on skull density that correlated with observed spikes in intracranial pressure [12]. Other characteristics to consider are skull cavity volume, skull geometry, age, and structure [13,14]. Selection of an animal model with similar attributes to human bone density is required to be most accurate and clinically relevant. Studies show that the rabbit skull is the least comparable model to the human skull, with non-human primates being optimal [11]. Due to ethical and resource limitations, rodent models have emerged as the most feasible. Rodent models have many advantages such as low cost, ease of use, and available access. For scaling based on skull density, blast and shock waves must have low-amplitude and short duration for rodent models [2]. It is also important to consider the intensity of blast exposure. High-pressure and long-duration exposures can more readily transverse the bony cavity of the skull, but will not appropriately scale based on injury severity [15].
Cerebral spinal fluid space
In order to understand injury expansion, extended research must focus on skull flexure and how it influences cerebral spinal fluid (CSF) post-blast in different models [16]. Recent evidence suggests that volume fractions vary between locations following blast exposure indicating multiple sites of pia-arachnoid complex disruption [17]. Detecting these areas of specific change is vitally important in understanding injury severity. Blast TBI is often associated with acceleration and subsequent deceleration of the brain and skull. The CSF responds differently than the brain to this rapid change in momentum due to its unique density gradient. The momentary lack of CSF cushioning allows the brain to collide with the skull [18]. Similar coup and contra coup effects have been observed in animal models including rhesus monkeys and rats [19,20]. Increasing the use of high throughput imaging modalities may enhance the ability to detect acute changes to the cerebral spinal fluid space following injury [21]. The transmission of the wave through the CSF has been linked to cavitation at the contra coup site of injury [22]. Finite element modeling may be useful in predicting cavitation and CSF dynamics for different animal models of blast TBI [8].
Brain size and architecture
White and Gray matter delineation are conserved across mammals. Even whales have similar axonal shearing following blast due to acceleration/deceleration forces [23]. The key components of interest for appropriate scaling are hierarchical neuroanatomy and metabolism [24]. In veterans, cortical thickness is significantly altered following blast exposure [25]. Areas consistently disrupted in human blast exposure are the prefrontal cortex and hippocampus [26]. The change in brain volume affects fluid-structure interactions [27]. In order to maintain clinical relevance, deformation of tissue due to pressure differences following blast must be consistent with scaling [28]. It was recently shown that when the top of a rat’s head is facing the shock tube, skull flexure produces similar changes in intracranial pressure in the prefrontal cortex as that seen in human blast exposure [9]. The deformation of tissue was therefore conserved across species. Likewise, blast exposure in Macaca monkeys caused increased ICP that significantly damaged hippocampal cells and Purkinje neurons [29]. Although the use of non-human primates is ideal, the cost limitations and ethical considerations are prohibitive. In scaling for rodent models the key is using small blast tubes, which can focus the wave to more region specific areas of interest [15]. Finite element modeling done with computer simulation can be used to determine the peak pressure needed for deformation of tissue [30]. Tabletop blast models produce the short duration peak pressures necessary for sufficient scaling and are more reliable between trials than larger models [31].
Vascular considerations
Because the brain has such a high demand for nutrients and oxygen, an extensive vascular network exists within the brain of all mammals. Brain tissue across all species have similar metabolic demands, therefore capillary length and ratio to cortical neurons will be conserved across mammalian species to provide the same demands for blood flow [32]. It is therefore assumed that the brain vasculature of a rodent, mouse, or rat would be an acceptable option for scaling with human vasculature. Blast can cause disruption of the vasculature, especially at the level of the blood brain barrier [33]. Thoracic exposure leads to a surge in venous pressure that contributes to chronic inflammation [34]. Blood vessels are susceptible to blast injury due to enhanced wave transmission through different density gradients [35]. Fluid/ solid coupling algorithms can be used to map the temporal distributions of pressure across larger vessels following blast [36].
Capillary differences are also of interest in comparing mammalian species. Circulatory shock is common following blast exposure. The mismatch in ventilation/perfusion is prominently expressed at the capillaries where metabolic exchange occurs [37]. Damage to the endothelium of capillaries has been reported following blast exposure [38]. The damage can be indirectly observed through iron deposits in the parenchyma [39]. In addition to injury itself, other characteristics must be considered for appropriate scaling including capillary diameter, aging of vessel, endothelial cell and myocyte size differences between species, and coronary pressure. All of the aforementioned characteristics may vary between species [40]. For example, in humans, age leads to a widening of capillary diameter [41], but in rodents, age leads to a narrowing of capillary diameter [42]. Variability may be adjusted and accounted for with normalization to size, weight, or age using carefully organized mathematical equations.
Red blood cells
The mean size of RBCs in humans is 9.65 microns. The smallest capillary is 4 microns meaning that RBCs must fold to fit through the capillary lumen [43]. Following blast injury, red blood cells can become structurally damaged limiting their ability to fit through the capillary lumen. The result is increased risk for hemorrhage and a drop in mean arterial pressure [44]. Post injury transfusions are often necessary following combat related blast injury to restore metabolic exchange [45]. Rats and humans have similar capillary diameters making rodent models viable for scaling [46]. Mammalian species often have different shapes of RBCs causing change in flow rate [47]. In rats unlike humans, RBCs decrease in size with age allowing more successful folding in young adult animals than neonatal animals [48]. The low-shear viscosity of young-adult rodent blood has similar dynamics to human blood despite aggregation being slightly different between the species [49,50]. The key similarity is that rat models have similar multifoci microhemorrhages following blast exposure, which is also seen in humans [51]. Not surprisingly, hemin, a heme oxygenase 1 activator, decreased injury severity when administered post-blast [52]. This finding indicates that red cell rupture is necessary for appropriate scaling in blast injury.
Neurons
Neural tissue properties are more variable across species. Rodents gain white matter at a faster rate than primate species although relative neuronal density in gray matter is comparable [53]. Despite differences in neuron size and axonal connections between mammals, the cranial volume to brain volume ratio typically scales to the animal’s body size [54]. Age is a key factor to consider as well. Aging typically results in shrinkage of brain volume, so the appropriate age of the animal must be selected for translational studies. Also, as rodent’s age the brain gets larger but in aged humans the brain tends to shrink [55]. Blast injury in larger mammals results in periventricular and hippocampal damage [56]. The damage in rodents is found primarily within the cortex and white matter tracts. Occasionally neurons in the hippocampus become damaged resulting in abnormal function [57]. Despite differences in injury foci, neurons respond equally to injury across species by swelling and forming vacuoles [15]. A comparable amount of neuronal death also occurs across species [58]. Another important factor is that basal metabolic rate conservatively scales across mammalian species according to body size, indicating the same cellular needs and energy expenditure [32]. Basal metabolic rate supports the use of mice as an affordable and practical model. DNA methylation rates are likewise similar between rodents and humans suggesting the validity of scaled models [59]. Neurodegeneration can occur at comparable rates between species, and higher severity of blast has been associated with α-spectrin disruption in mice similar to the disruption seen in humans [60]. Of particular importance is the change within mitochondria post-blast. Mitochondrial dysfunction is common post-blast in mice, and recent human data supports disrupted mitchondria function as a mechanism of injury as well [61,62]. Select neuronal mitochondria genes are conserved between species indicating that the neuron may be an ideal cell to compare similar injury pathways across species [63].
Glia (astrocytes and microglia)
During injury, mouse brain tissue may behave similarly to human tissue. Inflammatory responses in both humans and mice can be activated by the release of similar chemokines [64]. Injury also leads to similar activation of glial cells, including astrocytes and microglia [65]. Because this reaction to neural injury has been shown to be similar in humans and mice, it can be further assumed that mice may be valuable for a translational model. Rats also have similar responses to humans. GFAP, a marker for astrocytosis, has been elevated within the rat hippocampus following blast exposure [66]. Astrocytosis and subsequent behavioral disturbance is most pronounced in rats at blast wave pressures greater or equal to 117 kPa [67]. Rat models show that astrocytic foot processes surrounding the blood brain barrier (BBB) swell following blast injury indicating damage [68]. Astrocytosis also plays an important role in human blast pathophysiology [69]. It may contribute to long-term degenerative disease such as chronic traumatic encephalopathy [70]. In humans, an acute response to blast exposure is often loss of consciousness. In rats, this transient response can be measured by loss of righting reflex. The loss of righting reflex is accompanied by microglia activation measured with IBA1 [71]. Similar microgliosis was observed in rats using the CD11b/c antibody. Activated microglia was found adjacent to areas of BBB disruption within the cortex [72]. Similar to humans, the pineal gland in rat serves as an exquisite sensor for microglia activation following neural injury [73]. Extended neuroinflammation mediated by microglia activation has been linked to cognitive decline in humans [74]. Understanding the mechanism of persistent microglia activation following axonal shearing, warrants the use of appropriately scaled rodent blast models [75].
Endothelial cells
Blast exposure can disrupt tight junction proteins that interconnect endothelial cells [76]. The disruption is mediated by a vascular pressure surge and subsequent oxidative stress [33]. In vitro modeling has proved beneficial in detecting changes to endothelial cells post-blast. Findings suggest that damage occurs acutely and persists over a few days [77]. The decrease in trans-endothelial electrical resistance is the result of the impulse transmitted instead of peak overpressure [78]. The use of in vitro modeling also enables blast to be directed to hippocampal slice sections allowing focused investigation into the vasculature in this area [79]. Another important consideration is that 30-80% of blast exposures result in some type of infection. The BBB is the primary defense for the brain and therefore disruption leads to increased risk for exposure to bacterial toxins [80]. Animal models allow focused investigation into the biochemical dynamics surrounding endothelial cells post-injury. Bacterial endotoxin has been shown to increase intracellular adhesion molecule 1 expression on endothelial cells post-injury allowing an influx of leukocytes [81]. Additionally, lipopolysaccharide can trigger an increase in adipokine genes following TBI [82]. In rabbits, the changes that occur to endothelial cells produce robust hemoconcentration post-blast [83]. Hemoconcentration has also been reported in sheep post-blast, which severly limits metabolic exchange and the clearance of toxins [84]. The use of appropriately scaled models will help elucidate these complex interactions that occur from endothelial cell damage post-blast.
Biomarkers
Biomarkers have recently emerged as an important indicator of traumatic brain injury. Immediately following TBI in a porcine model, a panel of markers was increased in the CSF. These markers included neurofilament heavy chain, von willebrand factor, glia fibrillary acidic protein, brain-specific creatine kinase, and neuron-specific enolase [85]. Of particular importance are metabolomic biomarkers because they are altered following TBI in humans [86]. Metabolomic biomarkers must be similar between species exposed to injury to confirm that blast causes replicable and scaled injury [87]. Changes in blood flow drastically alter metabolic output [88]. The larger the brain volume the more metabolic capacity it has [32]. Metabolomic markers of interest for mammals include ascorbate, glutamate, phosphocoline, and N-acetylaspartate [89]. Another pathway of interest is neuroinflammation. Interleukin-5 offers to be a promising biomarker that is similarly elevated in CSF post-blast in multiple species [90]. Levels of interleukin-1a and erythopoietin have been shown to change in the CSF following blast in rodents, but further validation must be performed in human samples [91]. The vascular space often provides an appropriate venue to sample biomarkers. Changes in small nucleolar RNA within blood components is an important indicator of blast injury and may help indicate the progression towards neuropsychiatric disease in veterans [92]. Tau and TNFα changes are also detectable in serum and can offer acute sensitivity for acute injury [93]. DNA fragmentation is detectable in plasma and has been validated in a mouse blast model [94]. Scaled animal models offer an ideal option to screen potential biomarkers, which can then be validated in humans using multimodal magnetic resonance imaging [95].
Conclusion
Moving forward, pre-clinical models will need to be based on skull-based parameters. In this mini-review, we discussed relevant features for scaling such as brain and skull anatomy, vascular considerations, and differences in response based on cell type. We highlighted relevant biomarkers that could be used to determine the appropriate outcomes of scaled preclinical models. By switching to skull-based models we will be better able to develop appropriate treatment options for warfighters. Skull-based models will provide the scientific community a better understanding of brain injury from blast exposure.
References
- Toyinbo PA, Vanderploeg RD, Belanger HG, Spehar AM, Lapcevic WA, et al. (2016) A systems science approach to understanding polytrauma and blast-related injury: bayesian network model of data from a survey of the Florida National Guard. Am J Epidemiol.
- Park E, Gottlieb JJ, Cheung B, Shek PN, Baker AJ (2011) A model of low-level primary blast brain trauma results in cytoskeletal proteolysis and chronic functional impairment in the absence of lung barotrauma. J Neurotrauma 28: 343-357.
- Dussault MC, Smith M, Osselton D (2014) Blast injury and the human skeleton: an important emerging aspect of conflict-related trauma. Journal of forensic sciences 59: 606-612.
- Sherwood D, Sponsel WE, Lund BJ, Gray W, Watson R, et al. (2014) Anatomical manifestations of primary blast ocular trauma observed in a postmortem porcine model. Investigative ophthalmology and visual science 55: 1124-1132.
- Wang C, Pahk JB, Balaban CD, Miller MC, Wood AR, et al. (2014) Computational study of human head response to primary blast waves of five levels from three directions. PloS one 9: e113264.
- Tan LB, Chew FS, Tse KM, Chye Tan VB, Lee HP (2014) Impact of complex blast waves on the human head: a computational study. International journal for numerical methods in biomedical engineering 30: 1476-1505.
- Singh D, Cronin DS, Haladuick TN (2014) Head and brain response to blast using sagittal and transverse finite element models. International journal for numerical methods in biomedical engineering 30: 470-489.
- Panzer MB, Myers BS, Capehart BP, Bass CR (2012) Development of a finite element model for blast brain injury and the effects of CSF cavitation. Annals of biomedical engineering 40: 1530-1544.
- Dal Cengio Leonardi A, Keane NJ, Bir CA, Ryan AG, Xu L, et al. (2012) Head orientation affects the intracranial pressure response resulting from shock wave loading in the rat. Journal of biomechanics 45: 2595-2602.
- Rajs J, Moberg B, Olsson JE (1987) Explosion-related deaths in Sweden-a forensic-pathologic and criminalistic study. Forensic science international 34: 1-15.
- Bagi CM, Berryman E, Moalli MR (2011) Comparative bone anatomy of commonly used laboratory animals: implications for drug discovery. Comparative medicine 61: 76-85.
- Jean A, Nyein MK, Zheng JQ, Moore DF, Joannopoulos JD, et al. (2014) An animal-to-human scaling law for blast-induced traumatic brain injury risk assessment. Proceedings of the National Academy of Sciences of the United States of America 111: 15310-15315.
- Gefen A, Gefen N, Zhu Q, Raghupathi R, Margulies SS (2003) Age-dependent changes in material properties of the brain and braincase of the rat. Journal of neurotrauma 20: 1163-1177.
- McElhaney JH, Fogle JL, Melvin JW, Haynes RR, Roberts VL, et al. (1970) Mechanical properties on cranial bone. Journal of biomechanics 3: 495-511.
- Turner RC, Naser ZJ, Logsdon AF, DiPasquale KH, Jackson GJ, et al. (2013) Modeling clinically relevant blast parameters based on scaling principles produces functional and histological deficits in rats. Exp Neurol 248: 520-529.
- Chavko M, Watanabe T, Adeeb S, Lankasky J, Ahlers ST, et al. (2011) Relationship between orientation to a blast and pressure wave propagation inside the rat brain. Journal of neuroscience methods 195: 61-66.
- Scott G, Coats B (2015) Microstructural characterization of the pia-arachnoid complex using optical coherence tomography. IEEE transactions on medical imaging.
- Svetlov SI, Prima V, Kirk DR, Gutierrez H, Curley KC, et al. (2010) Morphologic and biochemical characterization of brain injury in a model of controlled blast overpressure exposure. The Journal of trauma 69: 795-804.
- Ommaya AK, Grubb RL, Naumann RA (1971) Coup and contre-coup injury: observations on the mechanics of visible brain injuries in the rhesus monkey. Journal of neurosurgery 35: 503-516.
- Kilbourne M, Kuehn R, Tosun C, Caridi J, Keledjian K, et al. (2009) Novel model of frontal impact closed head injury in the rat. Journal of neurotrauma 26: 2233-2243.
- Hardman JM, Manoukian A (2002) Pathology of head trauma. Neuroimaging clinics of North America 12: 175-187.
- Goeller J, Wardlaw A, Treichler D, O'Bruba J, Weiss G (2012) Investigation of cavitation as a possible damage mechanism in blast-induced traumatic brain injury. Journal of neurotrauma 29: 1970-1981.
- Knudsen SK, Oen EO (2003) Blast-induced neurotrauma in whales. Neuroscience research 46: 377-386.
- Karbowski J (2014) Constancy and trade-offs in the neuroanatomical and metabolic design of the cerebral cortex. Frontiers in neural circuits 8: 9.
- Tate DF, York GE, Reid MW, Cooper DB, Jones L, et al. (2014) Preliminary findings of cortical thickness abnormalities in blast injured service members and their relationship to clinical findings. Brain imaging and behavior 8: 102-109.
- Karr JE, Areshenkoff CN, Duggan EC, Garcia-Barrera MA (2014) Blast-related mild traumatic brain injury: a Bayesian random-effects meta-analysis on the cognitive outcomes of concussion among military personnel. Neuropsychology review 24: 428-444.
- Panzer MB, Myers BS, Bass CR (2013) Mesh considerations for finite element blast modelling in biomechanics. Computer methods in biomechanics and biomedical engineering 16: 612-621.
- Panzer MB, Wood GW, Bass CR (2014) Scaling in neurotrauma: How do we apply animal experiments to people. Experimental neurology.
- Lu J, Ng KC, Ling G, Wu J, Poon DJ, et al. (2012) Effect of blast exposure on the brain structure and cognition in Macaca fascicularis. Journal of neurotrauma 29: 1434-1454.
- Zhu F, Mao H, Dal Cengio Leonardi A, Wagner C, Chou C, et al. (2010) Development of an FE model of the rat head subjected to air shock loading. Stapp car crash journal 54: 211-225.
- Courtney MW, Courtney AC (2010) Note: A table-top blast driven shock tube. The Review of scientific instruments 81: 126103.
- Karbowski J (2011) Scaling of brain metabolism and blood flow in relation to capillary and neural scaling. PloS one 6: e26709.
- Shetty AK, Mishra V, Kodali M, Hattiangady B (2014) Blood brain barrier dysfunction and delayed neurological deficits in mild traumatic brain injury induced by blast shock waves. Frontiers in cellular neuroscience 8: 232.
- Sima rd JMMDPD, Pampori A, Keledjian K, Tosun C, Schwartzbauer G, et al. (2014) Exposure of the thorax to a sublethal blast wave causes a hydrodynamic pulse that leads to perivenular inflammation in the brain. Journal of neurotrauma.
- Gama Sosa MA, De Gasperi R, Janssen PL, Yuk FJ, Anazodo PC, et al. (2014) Selective vulnerability of the cerebral vasculature to blast injury in a rat model of mild traumatic brain injury. Acta neuropathologica communications 2: 67.
- Zhu F, Skelton P, Chou CC, Mao H, Yang KH, et al. (2013) Biomechanical responses of a pig head under blast loading: a computational simulation. International journal for numerical methods in biomedical engineering 29: 392-407.
- Irwin RJ, Lerner MR, Bealer JF, Brackett DJ, Tuggle DW (1997) Cardiopulmonary physiology of primary blast injury. The Journal of trauma 43: 650-655.
- Wang ZG (1989) An experimental study of blast injury. Zhonghua yi xue za zhi 69: 7-12.
- Gorbunov NV, Asher LV, Ayyagari V, Atkins JL (2006) Inflammatory leukocytes and iron turnover in experimental hemorrhagic lung trauma. Experimental and molecular pathology 80: 11-25.
- Hicks P, Rolsten C, Brizzee D, Samorajski T (1983) Age-related changes in rat brain capillaries. Neurobiology of aging 4: 69-75.
- Bell MA, Ball MJ (1981) Morphometric comparison of hippocampal microvasculature in ageing and demented people: diameters and densities. Acta neuropathologica 53: 299-318.
- Villena A, Vidal L, Diaz F, Perez De Vargas I (2003) Stereological changes in the capillary network of the aging dorsal lateral geniculate nucleus. The anatomical record Part A, Discoveries in molecular, cellular, and evolutionary biology 274: 857-861.
- Filipe P, Emerit I, Vassy J, Levy A, Huang V, et al. (1999) Cellular penetration of fluorescently labeled superoxide dismutases of various origins. Molecular medicine 5: 517-525.
- Kirkman E, Watts S (2014) Haemodynamic changes in trauma. British journal of anaesthesia 113: 266-275.
- Starkey K, Keene D, Morrison JJ, Doughty H, Midwinter MJ, et al. (2013) Impact of high ratios of plasma-to-red cell concentrate on the incidence of acute respiratory distress syndrome in UK transfused combat casualties. Shock 40: 15-20.
- Laursen H, Diemer NH (1977) Capillary size and density in the cerebral cortex of rats with a porto-caval anastomosis. Acta neuropathologica 40: 117-122.
- Betticher DC, Geiser J (1989) Resistance of mammalian red blood cells of different size to hypertonic milieu. Comparative biochemistry and physiology A, Comparative physiology 93: 429-432.
- Engstrom KG, Ohlsson L (1990) Morphology and filterability of red blood cells in neonatal and adult rats. Pediatric research 27: 220-226.
- Baskurt OK, Farley RA, Meiselman HJ (1997) Erythrocyte aggregation tendency and cellular properties in horse, human, and rat: a comparative study. The American journal of physiology 273: 2604-2612.
- Baskurt OK, Meiselman HJ (1997) Cellular determinants of low-shear blood viscosity. Biorheology 34: 235-247.
- Kuehn R, Simard PF, Driscoll I, Keledjian K, Ivanova S, et al. (2011) Rodent model of direct cranial blast injury. Journal of neurotrauma 28: 2155-2169.
- Chavko M, Prusaczyk WK, McCarron RM (2008) Protection against blast-induced mortality in rats by hemin. The Journal of trauma 65: 1140-1145.
- Ventura-Antunes L, Mota B, Herculano-Houzel S (2013) Different scaling of white matter volume, cortical connectivity, and gyrification across rodent and primate brains. Frontiers in neuroanatomy 7: 3.
- Bayat PD, Ghanbari A, Chehreie S (2010) Relationship between body mass index and the development of cranium in Arak newborns (central Iran). Italian journal of anatomy and embryology-Archivio italiano di anatomia ed embriologia 115: 218-222.
- Rodefer JS, Baxter MG (2007) Neuropsychology of Cognitive Aging in Rodents. In: Riddle DR (ed.) Brain Aging: Models, Methods, and Mechanisms.
- Bandak FA, Ling G, Bandak A, De Lanerolle NC (2015) Injury biomechanics, neuropathology, and simplified physics of explosive blast and impact mild traumatic brain injury. Handbook of clinical neurology 127: 89-104.
- Effgen GB, Vogel EW, Lynch KA, Lobel A, Hue CD, et al. (2014) Isolated primary blast alters neuronal function with minimal cell death in organotypic hippocampal slice cultures. Journal of neurotrauma 31: 1202-1210.
- Miller AP, Shah AS, Aperi BV, Budde MD, Pintar FA, et al. (2015) Effects of blast overpressure on neurons and glial cells in rat organotypic hippocampal slice cultures. Frontiers in neurology 6: 20.
- Haghighi F, Ge Y, Chen S, Xin Y, Umali MU, et al. (2015) Neuronal DNA Methylation Profiling of Blast-related Traumatic Brain Injury (TBI). Journal of neurotrauma.
- Valiyaveettil M, Alamneh YA, Wang Y, Arun P, Oguntayo S, et al. (2014) Cytoskeletal protein alpha-II spectrin degradation in the brain of repeated blast exposed mice. Brain research 1549: 32-41.
- Arun P, Abu-Taleb R, Oguntayo S, Wang Y, Valiyaveettil M, et al. (2013) Acute mitochondrial dysfunction after blast exposure: potential role of mitochondrial glutamate oxaloacetate transaminase. Journal of neurotrauma 30: 1645-1651.
- Gajavelli S, Sinha VK, Mazzeo AT, Spurlock MS, Lee SW, et al. (2015) Evidence to support mitochondrial neuroprotection, in severe traumatic brain injury. Journal of bioenergetics and biomembranes 47: 133-148.
- Faure E, Delaye L, Tribolo S, Levasseur A, Seligmann H, et al. (2011) Probable presence of an ubiquitous cryptic mitochondrial gene on the antisense strand of the cytochrome oxidase I gene. Biology direct 6: 56.
- Lloyd E, Somera-Molina K, Van Eldik LJ, Watterson DM, Wainwright MS (2008) Suppression of acute proinflammatory cytokine and chemokine upregulation by post-injury administration of a novel small molecule improves long-term neurologic outcome in a mouse model of traumatic brain injury. Journal of neuroinflammation 5: 28.
- Duckworth JL, Grimes J, Ling GS (2013) Pathophysiology of battlefield associated traumatic brain injury. Pathophysiology 20: 23-30.
- Svetlov SI, Prima V, Glushakova O, Svetlov A, Kirk DR, et al. (2012) Neuro-glial and systemic mechanisms of pathological responses in rat models of primary blast overpressure compared to "composite" blast. Frontiers in neurology 3: 15.
- Vandevord PJ, Bolander R, Sajja VS, Hay K, Bir CA (2012) Mild neurotrauma indicates a range-specific pressure response to low level shock wave exposure. Annals of biomedical engineering 40: 227-236.
- Kaur C, Singh J, Lim MK, Ng BL, Yap EP, et al. (1997) Ultrastructural changes of macroglial cells in the rat brain following an exposure to a non-penetrative blast. Annals of the Academy of Medicine, Singapore 26: 27-29.
- Leung LY, VandeVord PJ, Dal Cengio AL, Bir C, Yang KH, et al. (2008) Blast related neurotrauma: a review of cellular injury. Molecular & cellular biomechanics: MCB 5: 155-168.
- Lucke-Wold BP, Turner RC, Logsdon AF, Bailes JE, Huber JD, et al. (2014) Linking Traumatic Brain Injury to Chronic Traumatic Encephalopathy: Identification of Potential Mechanisms Leading to Neurofibrillary Tangle Development. Journal of neurotrauma.
- Perez-Polo JR, Rea HC, Johnson KM, Parsley MA, Unabia GC, et al. (2015) A rodent model of mild traumatic brain blast injury. Journal of neuroscience research 93: 549-561.
- Readnower RD, Chavko M, Adeeb S, Conroy MD, Pauly JR, et al. (2010) Increase in blood-brain barrier permeability, oxidative stress, and activated microglia in a rat model of blast-induced traumatic brain injury. Journal of neuroscience research 88: 3530-3539.
- Kaur C, Singh J, Lim MK, Ng BL, Ling EA (1997) Macrophages/microglia as 'sensors' of injury in the pineal gland of rats following a non-penetrative blast. Neuroscience research 27: 317-322.
- Smith C (2013) Review: the long-term consequences of microglial activation following acute traumatic brain injury. Neuropathology and applied neurobiology 39: 35-44.
- Kou Z, Vandevord PJ (2014) Traumatic white matter injury and glial activation: From basic science to clinics. Glia.
- Lucke-Wold BP, Logsdon AF, Smith KE, Turner RC, Alkon DL, (2014) Bryostatin-1 restores blood brain barrier integrity following blast-induced traumatic brain injury. Molecular neurobiology.
- Hue CD, Cao S, Dale Bass CR, Meaney DF, Morrison B (2014) Repeated primary blast injury causes delayed recovery, but not additive disruption, in an in vitro blood-brain barrier model. Journal of neurotrauma 31: 951-960.
- Hue CD, Cao S, Haider SF, Vo KV, Effgen GB, et al. (2013) Blood-brain barrier dysfunction after primary blast injury in vitro. Journal of neurotrauma 30: 1652-1663.
- Effgen GB, Hue CD, Vogel E, Panzer MB, Meaney DF, et al. (2012) A multiscale approach to blast neurotrauma modeling: part ii: methodology for inducing blast injury to in vitro models. Frontiers in neurology 3: 23.
- Li J, Topaz M, Tan H, Li Y, Li W, (2013) Treatment of infected soft tissue blast injury in swine by regulated negative pressure wound therapy. Annals of surgery 257: 335-344.
- Eissner G, Lindner H, Behrends U, Kolch W, Hieke A, et al. (1996) Influence of bacterial endotoxin on radiation-induced activation of human endothelial cells in vitro and in vivo: protective role of IL-10. Transplantation 62: 819-827.
- Brown R, Thompson HJ, Imran SA, Ur E, Wilkinson M (2008) Traumatic brain injury induces adipokine gene expression in rat brain. Neuroscience letters 432: 73-78.
- Zhang B, Wang A, Hu W, Zhang L, Xiong Y, et al. (2011) Hemoconcentration caused by microvascular dysfunction after blast injuries to the chest and abdomen of rabbits. The Journal of trauma 71: 694-701.
- Januszkiewicz AJ, Mundie TG, Dodd KT (1997) Maximal exercise performance-impairing effects of simulated blast overpressure in sheep. Toxicology 121: 51-63.
- Ahmed F, Gyorgy A, Kamnaksh A, Ling G, Tong L, et al. (2012) Time-dependent changes of protein biomarker levels in the cerebrospinal fluid after blast traumatic brain injury. Electrophoresis 33: 3705-3711.
- Glenn TC, Hirt D, Mendez G, McArthur DL, Sturtevant R, et al. (2013) Metabolomic analysis of cerebral spinal fluid from patients with severe brain injury. Acta neurochirurgica Supplement 118: 115-119.
- Cernak I (2014) Blast-induced neurotrauma models and their requirements. Frontiers in neurology 5: 128.
- Hamilton NB, Attwell D, Hall CN (2010) Pericyte-mediated regulation of capillary diameter: a component of neurovascular coupling in health and disease. Frontiers in neuroenergetics, 2.
- Viant MR, Lyeth BG, Miller MG, Berman RF (2005) An NMR metabolomics investigation of early metabolic disturbances following traumatic brain injury in a mammalian model. NMR in biomedicine 18: 507-516.
- Siva Sai Sujith Sajja B, Tenn C, McLaws LJ, VandeVord P (2014) IL-5; a diffuse biomarker associated with brain inflammation after blast exposure. Biomedical sciences instrumentation 50: 375-382.
- Sajja VS, Tenn C, McLaws LJ, Vandevord PJ (2012) A temporal evaluation of cytokines in rats after blast exposure. Biomedical sciences instrumentation 48: 374-379.
- Ho L, Lange G, Zhao W, Wang J, Rooney R, et al. (2014) Select small nucleolar RNAs in blood components as novel biomarkers for improved identification of comorbid traumatic brain injury and post-traumatic stress disorder in veterans of the conflicts in Afghanistan and Iraq. American journal of neurodegenerative disease 3: 170-181.
- Liu MD, Luo P, Wang ZJ, Fei Z (2014) Changes of serum Tau, GFAP, TNF-alpha and malonaldehyde after blast-related traumatic brain injury. Chinese journal of traumatology 17: 317-322.
- Wang Y, Arun P, Wei Y, Oguntayo S, Gharavi R, et al. (2014) Repeated blast exposures cause brain DNA fragmentation in mice. Journal of neurotrauma 31: 498-504.
- Whipple E, Greene J, Biester R, Robinson K, Nucifora P (2014) C-58Using multimodal magnetic resonance imaging to explore biomarkers of veterans with post-traumatic stress disorder after blast injury. Archives of clinical neuropsychology 29: 595.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences