Arthroscopic Bankart Lesion Repair with Special Handmade Pull out Suture
Emad Gaber Elbanna*, Ahmed Nabeel Mohamed Mahmoud, Atef Mohamed Morsy and Mohamed Ahmed Abdelkader
Department of Orthopaedics, Beni-Suef University, Beni Suef, Egypt
- *Corresponding Author:
- Emad Gaber Elbanna
Department of Orthopaedics,
Beni-Suef University,
Beni Suef,
Egypt
E-mail: elbanaemad@yahoo.com
Received: 15-Sep-2020, Manuscript No. M-6122; Editor assigned: 18-Sep-2020, PreQC No. P-6122; Reviewed: 5-Oct-2020, QC No. Q-6122; Revised: 28-June-2022, Manuscript No. R-6122; Published: 26-July-2022
Citation: Elbanna EG, Mahmoud ANM, Morsy AM, Abdelkader MA (2022) Arthroscopic Bankart Lesion Repair with Special Handmade Pull out Suture. J Orthop Disord Vol: 5 No: 3:6.
Abstract
Introduction: Anterior shoulder dislocation is a common injury causing detachment of the anterior glenoid labrum from its attachment (Bankart lesion). We introduce t h e ne w method of fixation of Bankart lesion by preparing the sutur e anchor using specific suture material (orthocord) to be used in reattachment of the glenoid larum.
Method: The technique applied on 40 patients (32 males, 8 females) with the traumatic anter iorshoulder instabil ity ( 17 right side and 23 left side),3 3 dominant sidew ith th e 24 months follow-up using constant score and quick dash score. 7 patients with 1st time dislocation, 29 patients with recurrent shoulder dislocations between 3 and 10 time and 4 patients more than 10 times of dislocations.
Results: Good postoperative results and good function and stabilization of the shoulder achieved from patie nts. Mean follow-up 20 months, recurrence rate 2.5% by re-injury . 17.5% of patients in the study has a regular sport activ ity and all return to sports within 6-10 months. 87.5% has ordinary work and return to work within 5-10 weeks. 12.5 % has a heavy work activity and return within 8-10 weeks.
Conclusion: our technique is effective for achieving stability as current used anchors technique and less cost, simple and easier than other transosseous techniques.
Keywords
Arthroscopic; Bankart; Lesion
Introduction
The glenohumeral joint of the shoulder is the most commonly joint liable to dislocation in the human body [1]. Acute dislocation is a surgical emergency and demands urgent relocation [2]. Anterior shoulder dislocation is a common injury that results in detachment of the anterior glenoid labrum from its attachment (Bankart lesion) [3]. It is commonly seen in accident and emergency and trauma clinics. If this neglected it will result in a recurrent shoulder dislocation [4].
Mechanism of injury is violent external rotation in abduction levers the head of the humerus out of the glenoid socket, avulsing anterior bony and soft tissue structures in the process [5]. The posterior part of the humeral head exits the joint, it often collides with the anterior rim of the glenoid, creating a bony indentation at the back of the humeral head (the Hill Sachs lesion) [6]. labrum and capsule around its rim (similar to a meniscus) [7]. The labrum is wedge-shaped and attaches almost completely around the edge of the glenoid [8]. This creates a deeper cup for the glenoid socket [9]. This is important because the glenoid socket is so flat and shallow that the ball of the humerus does not fit tightly [10].
The labrum creates a deeper cup for ball of the humerus to fit into [11]. This makes a contribution to the stability of the joint [12].
Arthroscopic repair of Bankart lesion is an effective primary treatment for Anterior shoulder dislocation, it provides successful outcomes without recurrence of instability [13]. it has advantages of, smaller incisions-less postoperative pain-shorter surgical times decreased complications-improved shoulder range of motion [14]. Arthroscopic techniques for reattaching the labrum can be divided into two categories a trans glenoid suture technique and arthroscopically delivered and tied suture anchors. The complication rate of arthroscopic stabilization is lower than that of open procedures. Extravasation of arthroscopy fluid is a rare and potentially life-threatening complication of fluid extravasation and airway compromise. Risk factors such as lateral decubitus positioning, obesity, high pump pressures, and long operative times may increase this risk [15].
Results of arthroscopic labral repair in the early days using staples or bioabsorbable tacks were discouraging, with a 30% rate of implant-related complications, including loosening, migration, and breakage. However, implant-related complication rates have decreased since the introduction of suture anchors as well as the development of various advanced arthroscopic instruments for secure insertion of the anchor in the glenoid. In a recent report, the failure rate was reported to be 0.3%.
Case Study
Prospective clinical study conducted in Beni Suef University hospital and governmental hospitals including 40 patients; with anterior shoulder instability a ter an initial episode of traumatic anterior shoulder dislocation, a Bankart lesion con irmed Magnetic Resonance Imaging (MRI) and clinical examination. 32 were males, and 8 were females, 17 had affected right side, 23 had affected left side. 17 had affected right side, 23 had affected left side. 7 patients presented with 1st time dislocation, 19 patients presented with (3-5) time of dislocation, 10 patients with (6-9) time of dislocation and 4 patients with more than 10 times of dislocation.
The mean age at the time of surgery was 26.95 ± 8.13 years (range 16-42 yeas). 8 were adolescents (16: 19 years), 26 were young adults (20: 35 years), and 6 cases were adults (36: 50 years). Patients with signi icant bony pathology (bony bankart), poor quality capsule-labral tissue, Multi directional instability or Ligamentous laxity were excluded from the study.
All patients received general anesthesia and may use an interscalene nerve block for analgesia during the perioperative and early postoperative period for shoulder arthroscopy. The patient position is in lateral decubitus with the arm hanging up (Figure 1).
Technical information
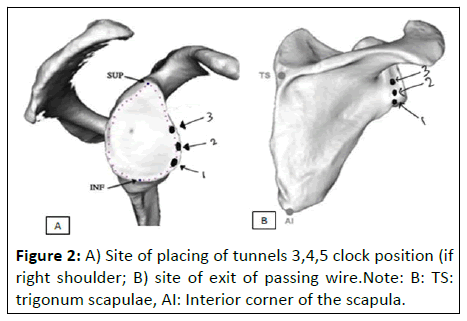
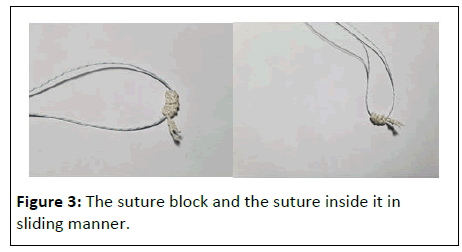
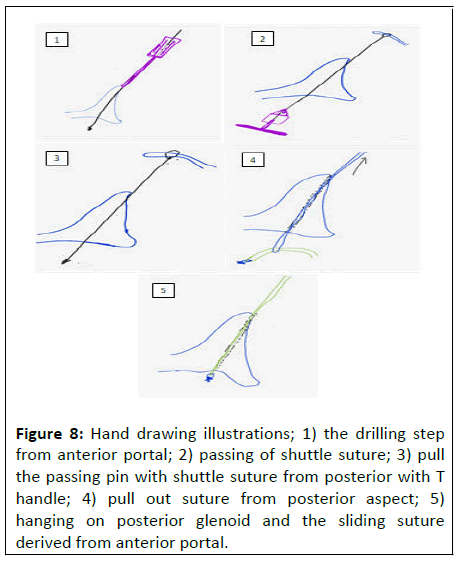
The key point in this technique which makes it unique is that the anchor used has a ring and a suture block, the suture block hangs on the posterior rim of the glenoid and the ring allow the suture wire to slide within the bony tunnel drilled from the anterior aspect of the glenoid directed posteriorly to exit at the scapular neck (Figures 2 and 3).
Now the suture block is rested posterior aspect of scapular neck and the two ends of the suture wire pass through the anterior end of the tunnel passing through the ring. The posterior portal is used to introduce the camera lens for visualization. The anterior portal is used as a working portal by passing a canula through it.
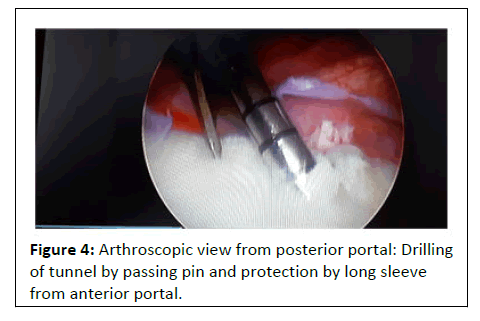
Step 1: Introducing a sleeve with sharp serrations at its end to hold it and prevents its slippage while manipulating it to change its inclination, it is hold at the most inferior point of the anterior border of the glenoid with an angle of 50 degree of the glenoid surface (Figure 4).
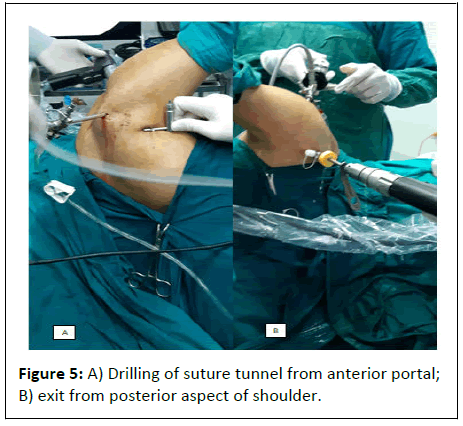
Step 2: Introducing a guide wire with a slot at its end the passing guide wire is 30 cm in length, it passes from anterior to posterior to exit posteriorly through the safe zone and pass through out the skin (7 cm-10 cm) below the acromion process (Figure 5).
Step 3: 1 cm skin incision is made over the exit point of the guide wire.
Step 4: The guide wire is drilled several times while pushing it and pulling it to make it easily pulled out in the next step.
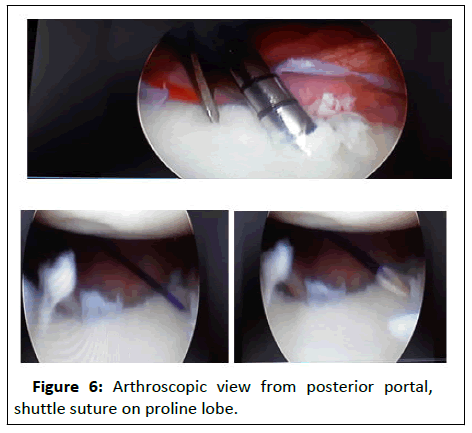
Step 5: The sleeve is removed, and a proline no. 2 thread is put in the slot at the end of the guide wire to act as a shuttle so that the two ends of the thread are out of the cannula anteriorly and the loop is pulled through the bony tunnel.
Step 6: A T-handle is used to pull out the guide wire from its posterior exit to pull it out of the joint posteriorly with the proline thread loop, till it appears from the posterior skin incision (Figure 6).
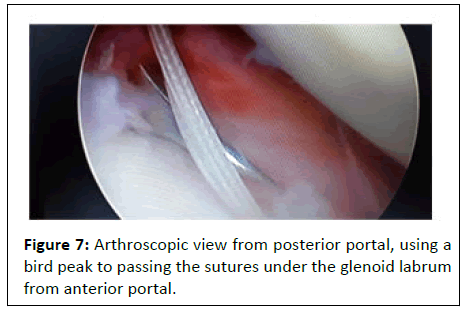
Step 7: The 2 ends of the orthocord wire of the anchor are passed through the proline loop, while the suture block of the anchor is hold by the surgeon hand (Figure 7).
Step 8: The 2 ends of the proline at the anterior portal is grasped with a kocher and is pulled anteriorly to take with it the orthocord wire to pass through the skin, muscles and to bony tunnel made till it exit through the anterior cannula. (Figure 8).
Figure 8: Hand drawing illustrations; 1) the drilling step from anterior portal; 2) passing of shuttle suture; 3) pull the passing pin with shuttle suture from posterior with T handle; 4) pull out suture from posterior aspect; 5) hanging on posterior glenoid and the sliding suture derived from anterior portal.
Step 9: The two ends of the orthocord wire is then grasped with a kocher from their ends and pulled out anteriorly to pull the suture block till it rests (hangs) over the posterior aspect of the bony tunnel at this point make sure that there is no so t tissue interposition between the suture block and the bone by repetitive pulling of the orthocord wire till no rebound happens.
Step 10: The kocher is removed and the sliding of the orthocord wire through the rings of the suture block is examined.
Step 11: A parrot peak or suture lasso is used to pass with a good grip through the labrum and then catch one thread of the orthocord.
Step 12: The parrot peak is passed out of the cannula catching one thread of the orthocord wire.
Step 13: A sliding knot is made to suture the labrum to the glenoid surface and then repeated two times and a reverse knot is done.
Step 14: Introduce a wire cutter to cut the wire 9 mm above the knot.
The technique used in 40 patients with mean follow-up 20 months. There were 32 males (80%) and 8 females (20%) with a mean age 26.9 ± 10.13 (range 16 years-46 years). There were 17 right shoulders, 23 left shoulders. 23 patients with dominant side affected and 17 patients with non-dominant side affected. All cases had history of traumatic events 7 patients with 1st time dislocation, 19 patients had recurrent shoulder dislocation 3-5 times, 10 patients dislocated times 6-9 and 4 patients had recurrent shoulder dislocation more than 10 times.
The patients functions was improving over time according to quick dash score, the mean score is 26.63 at 6 week follow-up with standard deviation 6.83 at 3 months post-operative the mean score 14.38 with standard deviation 12.28 and at 6 months post-operative the mean score 4.75 with standard deviation 6.09 with significant improving in function and stability.
The patients functions was improving over time according to constant score, the mean score is 71.85 at 6 week follow-up with standard deviation 6.61 at 3 months post-operative the mean score 83.93 with standard deviation 16.95 and at 6 months postoperative the mean score 92.65 with standard deviation 5.99. The patients functions was improving over time according to constant score, the mean score is 71.85 at 6 week follow-up with standard deviation 6.61 at 3 months post-operative the mean score 83.93 with standard deviation 16.95 and at 6 months postoperative the mean score 92.65 with standard deviation 5.99.
Only 18% of patients have a routine sport activity (football, swimming and weight lifting) and 83% of patients are nonsportive. All sportive patients return to sport activity after rehabilitation program in duration from 6 to 10 months postoperative.
Post-opera tive complication, 1 patient with post-operative infection managed by arthroscopic drainage and debridement and 1 patient have a shoulder dislocation by re-injury 10 months post-operative.
No patients reported with neurological complication either brachial plexus traction injury from lateral position or suprascapular nerve injury from exiting wire posterior.
Discussion
Traumatic unidirectional instability the most recent and most successful surgical procedures for unidirectional shoulder instability reattaching the detached labrum and associated glenohumeral ligaments with little disruption to the attachment of other structures around the shoulder (Bankart repair).
Different types of anchors are available with different sizes and shapes and way of fixation to bone e.g. threated or arrow anchors, conical or slotted, small sizes and larger size. And also, biodegradable, titanium, stainless steel or suture anchors. All of which are used to suture the labrum or capsule to the glenoid, they are inserted through the anterior portal to be buried in the bone (subcortical).
Morgan and Bodenstab have stated that the arthroscopic technique has general complications and carries the risk of suprascapular nerve injury.
It used a motorized drill as we use in our study, and there was no suprascapular nerve injury in their series and obtained sufficient stability and avoided crowding by using only 4 or 5 knots of #1 PDS sutures.
It recommended that AIGHL and the labral complex be repaired with 5-8 knots of #2 mono filamentous absorbable sutures.
It recommended that the entry point of a guide pin should be 2 o'clock on the right and 10 o'clock in the left shoulder and exit through the inferomedial aspect of the infraspinatus fossa, but found that a guide pin usually slipped in order to maintain the above-mentioned entry point because the shape of the glenoid was elliptical and the angle between the direction of the guide pin and the anterior glenoid neck was too acute. Actually, the guide pin couldn't exit the inferomedial aspect of the infraspinatus fossa through the glenoid neck because the infraspinatus fossa of the scapula formed a round curvature along the thoracic rib cage. So, the inferomedial placement of the guide pin in the infraspinatus fossa as Caspari recommended was difficult to determine in the glenoid neck. So kim inserted the guide pin at 1 o'clock of the glenoid neck on the right shoulder and 11 o'clock on the left shoulder, and tried to exit in the inferomedial aspect of the infraspinatus fossa. In 12 of 23 cases (52.2%), knots were formed at the super-medial or center of the infraspinatus fossa. Theoretically, the superomedial placement of the guide pin could hurt the suprascapular nerve. However, there was no suprascapular nerve injury in the followup period. Also, kim recommend the use of the anterosuperior portal instead of the anterior portal in order to insert the guide pin at 1 o'clock in the right shoulder and 11 o clock in the left shoulder.
Our study evaluates the clinical and functional results after arthroscopic bankart repair using handmade suture anchor using orthocord no. 2 and making a suture block through transosseous tunnel and hang on posterior aspect of the glenoid and tying by sliding knot from anterior portal. This technique upgrades the concept of transosseous sutures for bankart repair and made it easy to tie the knot under vision in sliding manner using the anterior portal and ensure the fixation technique. The use of the suture block acts as the anchor and it allowing a thread to pass and slide easily through it. Arthroscopic repair of bankart lesion by hand made suture anchors has advantages over other transosseous techniques in fixing the suture on the posterior neck of the glenoid and tying the labrum by traditional sliding knot easily and grantee a good repair of the labrum to the bone and avoid the possibility of suture laxity and failure of the repair. This technique allows anatomical reduction under vision and stable fixation of the labrum. This method of fixation doesn’t place implants other than fiberwire suture (orthocord) inside the joint (implant free fixation). Thus, avoid the risk of metal and biodegradable anchors and gain the advantages of all suture anchors and achieve the complete healing of the bony tunnels and preserve the glenoid bone stock. Also, the use of 2 mm passing pin helps in avoid the risk of glenoid bone loss.
Our method of fixation is cost effective technique using simple instruments and any surgeon can made the suture block easily inside the operation within two minutes.The lateral decubitus position is preferred in this technique to facilitate the exit of passing wire posterior through the scapula in the safe zone for supra-scapular nerve to avoid the nerve injury.In all patients in our study, no reported complication from nerve injury, but five patients suffered a post-operative numbness in the non-operating limb due to traction and resolved after 24 to 48 hours with no traction brachial plexus injury.We found that 70% of patients returns to normal daily activities after 6 weeks post-operative, the ordinary self-hygiene and wearing the clothes by themselves and 30% returns to daily activities in 7-8 weeks post-operative. About 87.5% of patients have ordinary paper work with no possible risk for reinjury and 22.5% have a heavy-duty work with high possible risk for reinjury. 52.5% of patients returned to their light work after 8 weeks postoperative, 37.5% returns to light and heavy work after 9 weeks post-operative. One patient returned to work at 7 weeks postoperative and 3 patients returned in 10 weeks post-operative.
None of the patients in our series had a sever hill sachs lesion, 29 patients have mild hill sachs lesion and 11 patients have moderate Hill sachs lesion.
The results of our study showed a statistically significant improvement in the mean of the postoperative constant and quick dash score at the final follow-up compared to that of the preoperative (p value<0.001).The technical pitfalls for our technique, the lateral decubitus position avoid the convergence of bony tunnels which may corrupt the other tied anchor. Beach chair position not achieve easy control of exit of passing wire on safe exit on posterior part of the scapula. We think this technique is also ideal for revision of off-loading of traditional anchors intraoperative by using the same fiber wire to make a handmade suture block with no additional cost. The limitation of our study is no available data on elite athletes in contact sport and only use of constant and quick dash scoring system for assessment of our patients and relative short follow-up period. We recommend a study on larger number of cases in multiple centers and with variable level of experience for surgeons between experts, seniors and junior surgeons and longer followup time for establishing the replacement of the current used anchors with our technique.
Conclusion
Arthroscopic bankart repair with hand-made suture anchor technique is less cost than the used anchors. It is simple procedure in suture handling and tying the suture in sliding manner as traditional anchors. In our series the technique achieve stability for the patients. The fact that lateral decubitus position requires relatively a long learning curve, and after training on the position the overall operative time can be reduced.
References
- Naredo E, Aguado P, De Miguel E, Uson J, Mayordomo L, et al. (2002) Painful shoulder: Comparison of physical examination and ultrasonographic findings. Ann Rheum Dis 60: 132-136.
- Bankart ASB (1923) The pathology and treatment of recurrent dislocation of the shoulder joint. Br J Surg 2: 23-29.
- Kuhn JE, Lindholm SR, Huston LJ, Soslowsky LJ, Blasier RB, et al. (2003) Failure of the biceps superior labral complex: A cadaveric biomechanical investigation comparing the late cocking and early deceleration positions of throwing. Arthroscopy 19.
- Hill HA, Sachs MD (1940) The grooved defect of the humeral head: A frequently unrecognized complication of dislocations of the shoulder joint. Radiol 35: 690-700.
- Kitayama S, Sugaya H, Takahashi N, Matsuki K, Kawai N, et al. (2015) Cinical outcome and glenoid morphology after arthroscopic repair of chronic osseous Bankart lesions: A five to eight-year follow-up study. J Bone Joint Surg 97: 1833-1843.
- Wright PB, Budoff JE, Yeh ML, Kelm ZS, Luo ZP, et al. (2006) Strength of damaged suture: An in vitro study. Arthroscopy: J Arthroscopic Relat Surg 22: 1270-1275.
- Pulavarti RS, Symes TH, Rangan A (2009) Surgical interventions for anterior shoulder instability in adults. Cochrane Database Syst Rev 4: Art No : CD005077.
- Owens BD, Harrast JJ, Hurwitz SR, Thompson TL, Wolf JM, et al. (2011) Surgical trends in Bankart repair an analysis of data from the American Board of Orthopaedic Surgery certification examination. Am J Sports Med 39: 1865-1869.
- Vier (2019) Patient Positioning in Shoulder Arthroscopy: Which is Best? Joints 7: 46-55.
- Privitera DM, Bisson LJ, Marzo JM (2012) Minimum 10-year follow-up of arthroscopic intra-articular Bankart repair using bioabsorbable tacks. Am J Sports Med 40: 100-107.
- Morgan CD, Bodenstab AB (1987) Arthroscopic: Bankart suture repair, technique and early results. Arthroscopy 3: 111-122.
- Kim SH, Ha KI, Kim SH (2002) Bankart repair in traumatic anterior shoulder in-stability: Open versus arthroscopic technique. Arthroscopy 18: 755-763.
- Caspari RB, Savoie FH, JB McGinty (1991) Arthroscopic reconstruction of the shoulder: The Bankart repair. Operative arthroscopy; New York: Raven Press 507-515.
- Caspari R (1988) Arthroscopic reconstruction for anterior shoulder instability. Oper Tech Orthop 3: 59-66.
- Mulder K, Marynissen H, Van Laere C, Lagae K, Declercq G, et al. (1998) Arthroscopic transglenoid suture of Bankart lesions. Acta Orthopaedica Belgica 64: 160-166.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences