Acinetobacter Baumanii Bleb-Related Endophthalmitis
Mark A McAllister1, Spencer M Moore1 and April E Harris2*
1Department of Ophthalmology and Vision Science, University of Arizona College of Medicine, Alvernon Way, Tucson, Arizona, USA
2Department of Ophthalmology, Retina Associates Southwest, Tucson, Arizona, USA
- *Corresponding Author:
- April E Harris
Department of Ophthalmology,
Retina Associtaes Southwest, Tucson, Ariozna,
UAS,
E-mail: Aeharris49@gmail.com
Received date: May 11, 2022, Manuscript No. IPCIID-22-13815; Editor Assigned date: May 13, 2022, PreQC No. IPCIID-22-13815 (PQ); Reviewed date: May 24, 2022, QC No. IPCIID-22-13815; Revised date: June 3, 2022, Manuscript No. IPCIID-22-13815 (R); Published date: June 10, 2022, DOI: 10.36648/Ipjciid.6.3.4
Citation: McAllister MA, Moore SM, Harris AE (2022) Acinetobacter Baumanii Bleb-Related Endophthalmitis. Clin Immunol Infect Dis Vol.6 No.3: 4
Abstract
The purpose of this article is to describe a single case of acute post-trabeculectomy bleb-related endophthalmitis secondary to Acinetobacter baumannii. A 74-year-old man with a history of trabeculectomy with adjunctive mitomycin C was referred by his glaucoma specialist to a private retina specialist for intraocular inflammation concerning for blebitis versus bleb-associated endophthalmitis. Anterior chamber paracentesis and vitreous tap for cultures were performed, which grew the gram-negative coccobacillus Acinetobacter baumannii on culture. He was treated with intravitreal vancomycin, ceftazidime, and dexamethasone with significant clinical improvement. Two months after initial injection, he had resolution of vitreous opacities and underwent cataract surgery with final visual acuity of 20/25 on post-surgical month one visit. Acinetobacter baumannii is an atypical cause of infectious endophthalmitis and has been reported in the literature to develop multidrug resistance and form biofilms. This rare infection poses challenges to the physician in both prompt diagnosis and appropriate treatment. Awareness of Acinetobacter baumannii and its challenges including the potential for multidrug resistance may assist in clinical decision making to provide rapid and effective care for patients.
Keywords
Acinetobacter baumannii endophthalmitis; Gram negative endophthalmitis; Atypical endophthalmitis; Multidrug resistant endophthalmitis; Bleb-related endophthalmitis
Introduction
Endophthalmitis is a sight-threatening ocular complication most frequently attributed to intraocular surgery, recent trauma, or sepsis. Despite timely diagnosis and treatment, endophthalmitis can have devastating consequences on vision. It most commonly occurs after anterior segment surgery. Early reports of endophthalmitis after trabeculectomy with and without mitomycin C are 0.2-9.6% and 2.6%, respectively [1]. Various factors influence the final outcomes in patients with recent endophthalmitis, among these include the types of organisms involved and their antimicrobial resistance patterns.
Acinetobacter baumannii, a Gram-negative, non-motile, oxidase negative coccobacillus, is classified under the family Moraxellaceae [2]. It is a rare cause of infectious endophthalmitis with few case series and reports in the literature. Many of these cases reported complex antimicrobial resistance patterns. The ability of this organism to develop multidrug resistance, in addition to formation of biofilms, allows it to persist in nosocomial settings [3]. As such, it presents unique challenges in treatment. It is also emerging as an important cause of community-acquired infection [4]. We report here a case of trabeculectomy bleb-related endophthalmitis from which A. baumannii was isolated in culture. Of note, the patient was chronically using daily difluprednate 0.05% in both eyes, and the endophthalmitis presented 2 years after the initial trabeculectomy with mitomycin C. There were no recent systemic infections, trauma, antibiotic use, hospitalizations, recent ophthalmic procedures, nor any other known risk factors. To the best of our knowledge, this represents the first case reported in the literature of bleb-related endophthalmitis secondary to Acinetobacter baumannii.
Case Report
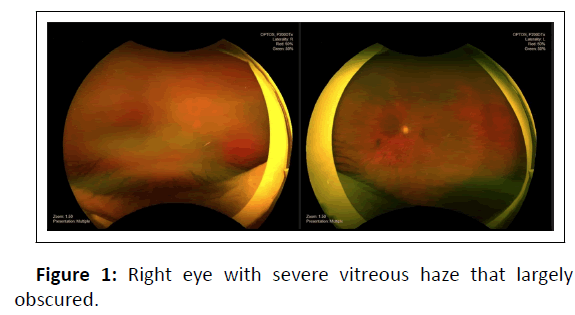
A 74-year-old male with primary open angle glaucoma and bilateral trabeculectomy presented to a retina specialist as a referral for right eye uveitis versus infectious blebitis or endophthalmitis. The inflammation was first noted by the glaucoma specialist in the operating room while preparing the eye for cataract surgery and had newly developed since the patient’s preoperative cataract evaluation. Upon further questioning, the patient noted approximately 1 week of pain, redness, floaters, and gradually worsening vision in the right eye. He had self-discontinued his home difluprednate in both eyes for the past month, which he had been prescribed for bleb maintenance by his glaucoma specialist. Review of systems was otherwise negative, including no systemic infectious symptoms. There was no history of malignancy, diabetes mellitus, nor ocular trauma. He had undergone an uncomplicated trabeculectomy in the right eye with mitomycin C two years prior to presentation and was maintained on daily difluprednate 0.05% for bleb maintenance. Visual acuity with correction was count fingers at 3 feet in the right eye and 20/40 in the left eye. Intraocular pressure was 10 mmHg and 13 mmHg by pneumotonometer in the right and left eyes, respectively. No afferent pupillary defect was observed. Anterior segment examination revealed conjunctival injection, bleb injection without purulence, 1+ corneal edema with Descemet folds, 2+ cell and flare in the anterior chamber without hypopyon, and a significant combined senile cataract in the right eye of 3+ nuclear sclerosis and 3+ posterior subcapsular cataract. The left eye was unremarkable except for the presence of 2+ nuclear sclerosis. Right eye fundus examination was significant for vitritis with severe vitreous haze that largely obscured the view posteriorly in the right eye (Figure 1). B-scan showed vitreous opacities and posterior vitreous detachment in the right eye but no retinal detachment or mass.
Vitreous tap/biopsy and anterior chamber paracentesis for culture were performed. He was treated with intravitreal dexamethasone 1 mg/0.1 mL, vancomycin 2.25 mg/0.1 mL, and ceftazidime 400 mg/0.1 mL. He was started on topical difluprednate 0.05% four times daily, topical moxifloxacin 0.5% every hour and oral moxifloxacin 400 mg.
On day 1 after tap and injection, he had decreased corneal edema and vitritis with subjective improvement in pain and vision, though visual acuity remained at ‘count fingers’ at 3 feet. He was continued on the drop regimen as noted above but with a decrease in the moxifloxacin to four times daily. After one-week, vitreous tap cultures grew Acinetobacter baumannii. Unfortunately, resistance patterns were unable to be obtained as the lab reported that they did not regularly perform susceptibility testing on these types of isolates as there are not “achievable antibiotic levels for the eye.” At this one-week follow-up visit, the patient reported decreased pain and subjective improvement in vision. The anterior chamber inflammation was minimal. He finished the seven-day course of oral moxifloxacin but continued the topical difluprednate and moxifloxacin four times daily. By three weeks after the tap and injection, his vision improved slightly to count fingers at 5 feet. He had resolution of anterior chamber cell/flare and only mild persistent vitreous haze on B-scan
Approximately two months after treatment for endophthalmitis, he underwent uncomplicated cataract surgery with his glaucoma specialist. At the postoperative month one visit after cataract surgery, his vision remarkably improved to 20/25 in the right eye with no residual anterior chamber cell/flare and no vitreous haze
Discussion
Acinetobacter baumannii is a gram-negative bacterium rarely known to cause endophthalmitis and has increasing multidrug resistance. There are only a few case series and reports in the literature describing this form of gram negative endophthalmitis. In many case reports, the patients recently had trauma, recent illness, or surgery such as cataract surgery or intravitreal injection. However, we report a case of A. baumannii bleb related endophthalmitis in which the patient had a distant history of trabeculectomy two years prior without recent illness, hospitalization, use of antibiotics, or other known risk factors. It is possible that either our case represents a delayed-onset postoperative endophthalmitis or a community-acquired endogenous infection, as no other sources (i.e., trauma) were identified in this patient. To our knowledge, this is the first case report of bleb-related endophthalmitis from A. baumannii. Additionally, this patient’s infection resolved with intravitreal vancomycin and ceftazidime, which is not always the case given frequent A. baumannii resistance patterns.
The Acinetobacter genus represents gram0negative aerobic, catalase positive and oxidase negative bacteria with 54 known species [5]. In humans, Acinetobacter are known to cause pneumonia, sepsis, meningitis, and skin and soft tissue infections; colonization of indwelling vascular and urinary catheters in nosocomial settings is increasingly reported. Pathogenesis has been attributed to biofilm formation and cell surface adhesion. A. baumannii was reported to develop increasing antimicrobial resistance in the 1980s, with 18% of isolates currently showing resistance to all first-line agents. A. baumannii resistance mechanisms include extended-spectrum beta-lactamases, bacterial cell wall porins, efflux pumps, aminoglycoside-modifying enzymes, and mutations in quinolone resistance-determining regions of bacterial DNA. Treatment is targeted based on local resistance patterns and culture susceptibility results, though multidrug resistance often requires combination therapy and input from an infectious disease specialist.
To our knowledge, the first report of A. baumannii endophthalmitis was a case series of two patients reported by Chen and colleagues [4]. Their first patient had abdominal pain and diarrhea for one week followed by a sudden onset of blurry vision and eye pain secondary to A. baumannii endophthalmitis. Their second case was endophthalmitis secondary to trauma. The first patient had minimal antimicrobial resistance, but the second had significant resistance to nearly every antibiotic tested, except for imipenem. Although carbapenems are not routinely used in intravitreal formulation, their use has been reported as nontoxic to retina and has even been used in treating multidrug resistant Klebsiella and is now being used in one arm of a prospective postoperative endophthalmitis clinical trial [6,7]. Additionally, carbapenem resistance amongst A. baumannii is emerging, creating more challenges in treatment [8,9].
Roy and colleagues described four cases of A. baumannii endophthalmitis, three of which occurred shortly after cataract surgery and one of which occurred in a seven-year-old after traumatic ocular injury [2]. One patient required evisceration, while two others underwent vitrectomy with IOL removal and intravitreal antibiotics. Unfortunately, the seven-year-old ended up phthisical despite vitrectomy, lensectomy and intravitreal injections. Each patient grew A. baumannii on vitreous culture. Susceptibility testing showed ceftazidime resistance in all cases, a commonly used cephalosporin in endophthalmitis treatment providing broad-spectrum gram-negative coverage. All cases were ciprofloxacin sensitive; as such, the authors concluded that A. baumannii endophthalmitis might be best treated with ciprofloxacin first line. Ciprofloxacin susceptibility, however, has not been supported by other case reports.
Intravitreal injections have also been recognized as a potential mechanism of A. baumannii infectious endophthalmitis. Bukhatwa et al. published a case series of 13 of 14 patients with A. baumannii endophthalmitis secondary to intravitreal injections with bevacizumab from two consecutive days, found to be due to a contaminated lot of bevacizumab. All patients in this study had vision of 20/80 or worse at 1 month follow-up [10]. In addition to the potential for outbreak, this case series also highlights the increasing presence of this organism in healthcare settings and a potential cause for nosocomial endophthalmitis.
Conclusion
In conclusion, Acinetobacter baumannii is increasingly reported in the literature as a severe cause of endophthalmitis with frequent reports of microbial resistance. This creates significant challenges for treatment and usually results in severely decreased vision for patients who suffer from this infection, often leading to globe loss. To the best of our knowledge, this is the first case of A. baumannii bleb-related endophthalmitis in the literature. It is important for the ophthalmologist to be aware of this organism as a possible cause of endophthalmitis with a high index of suspicion for possible multidrug resistance, to provide the best possible patient care.
Patient Consent
Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Acknowledgements and Disclosures
Funding
No funding or grant support.
Conflicts of interest
The authors have no financial disclosures.
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Acknowledgements
None
References
- Higginbotham EJ, Stevens RK, Musch DC (1996) Bleb-related endophthalmitis after trabeculectomy with mitomycin C. Ophthalmology 103(4): 650-656.
[Crossref], [Google Scholar], [Indexed]
- Roy R, Panigrahi P, Malathi J (2013)Endophthalmitis caused by Acinetobacter baumanni: a case series. Eye (Lond) 27(3): 450-452.
[Crossref], [Google Scholar], [Indexed]
- Talreja D, Kaye KS, Yu FS, Walia SK, Kumar A (2014) Pathogenicity of ocular isolates of Acinetobacter baumannii in a mouse model of bacterial endophthalmitis. Invest Ophthalmol Vis Sci 55(4): 2392-2402.
[Crossref], [Google Scholar], [Indexed]
- Chen KJ, Hou CH, Sun MH, Lai CC, Sun CC, et al. (2008) Endophthalmitis caused by Acinetobacter baumannii: Report of two cases. J Clin Microbiol 46(3): 1148-1150.
[Crossref], [Google Scholar], [Indexed]
- Bleb-related endophthalmitis after trabeculectomy with mitomycin C
- Sanghi S, Pathengay A, Jindal A, et al. (2014) Acute-onset postoperative endophthalmitis caused by multidrug-resistant Klebsiella pneumoniae. Clin Ophthalmol 8: 1783-1785.
[Crossref], [Google Scholar], [Indexed]
- Das T, Dave VP, Dogra A, Joseph J, Sharma S, et al. (2021) Endophthalmitis management study. Report #1. Protocol. Indian Journal of Ophthalmology 69(7): 1936-1941.
[Crossref], [Google Scholar], [Indexed]
- Hsueh PR, Teng LJ, Chen CY, et al. (2002) Pandrug-resistant Acinetobacter baumannii causing nosocomial infections in a university hospital, Taiwan. Emerg Infect Dis 8(8): 827-32.
[Crossref], [Google Scholar], [Indexed]
- Lopez-Hernandez S, Alarcon T, Lopez-Brea M (2000) Evolution of antimicrobial susceptibility of Acinetobacter baumannii clinical isolates. Rev Esp Quimioter 13(4): 394-400.
[Google Scholar], [Indexed]
- Bukhatwa S, Eldressi SS, Metmoah E-SG, Bukhatwa SA (2021) An outbreak of endophthalmitis following Intravitreal Injection of Bevacizumab in a referral center. Egyptian Journal of Ophthalmology 1(2): 85-90.
[Crossref], [Google Scholar]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences