Abstract
Neuraxial labor analgesia: A literature review
Labor is considered one of the most exciting experiences, but it is also one of the most painful experiences a woman can experience during her lifetime. Although labor pain does not threaten the life of a parturient, it has important consequences for the mother and fetus. Physiological responses to pain during vaginal delivery influence maternal and fetal well-being, as well as the evolution of labor. Therefore, the use of analgesic techniques to relieve labor pain has become more frequent, but the effects of neuraxial analgesia techniques on labor and its outcomes are still debatable. Analgesia does not seem to affect the incidence of Cesarean sections, but may increase the chance of instrumental vaginal delivery, in addition to prolonging the second stage of labor; however, without changing the prognosis. Non-pharmacological analgesic techniques such as hydrotherapy, acupuncture and transcutaneous electrical nerve stimulation are available. Pharmacological techniques include peripheral blockades (paracervical and pudendal), inhaled analgesia (nitrous oxide and halogenated), intravenous analgesia (opioids and non-opioids), and neuraxial analgesia. Among them, neuraxial analgesia (epidural, spinal anesthesia, and combined spinal-epidural anesthesia) is considered the most effective. The aim of this review is to discuss the main pharmacological techniques of labor analgesia available, among them the neuraxial, inhaled and intravenous (remifentanil) techniques, as well as to evaluate the advantages and disadvantages associated with each technique. We will also discuss
induction techniques (epidural, combined spinal-epidural, continuous spinal, dural puncture epidural) and maintenance of analgesia (intermittent epidural bolus, continuous epidural infusion, patient-controlled epidural analgesia, computer-integrated patient-controlled epidural analgesia).
Author(s): Fábio Farias de Aragão
Abstract | PDF
Share This Article
Google Scholar citation report
Citations : 6
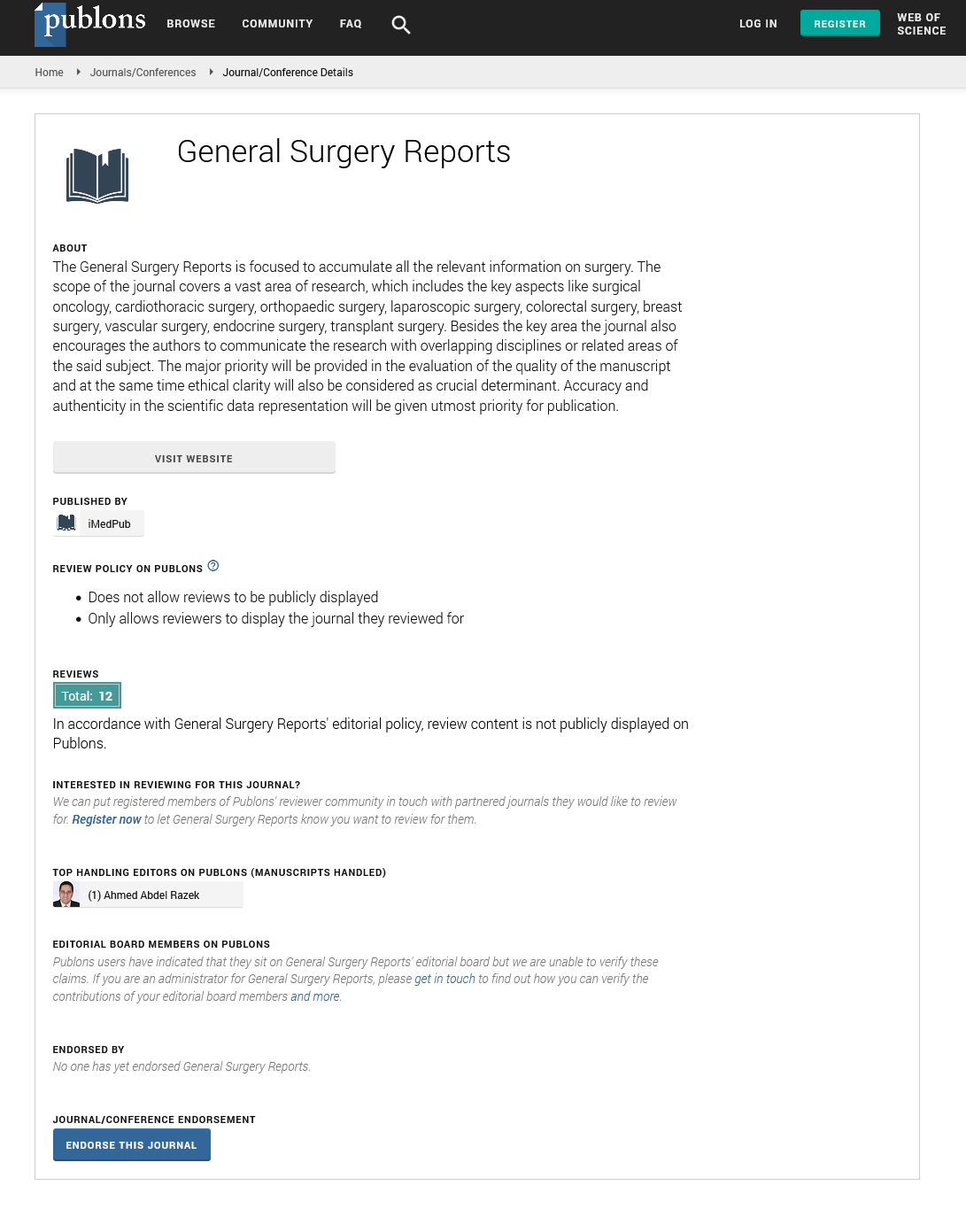
General Surgery Reports received 6 citations as per Google Scholar report
General Surgery Reports peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- Publons
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences