ISSN : 2347-5447
British Biomedical Bulletin
The Impact of Psychological Treatment on Catastrophization and Pharmacological Response in Chronic Migraine: A Single-Center Experience
Federica Nicoletta Sepe1*, Claudia Lanni2, Daniele Michelis2 and Giacomo Lancia3
1Department of Emergency Neurology and Stroke Unit, IRCCS C. Mondino Foundation, Pavia, Italy
2Department of Neurology, Universitaria SS. Antonio e Biagio e Cesare Arrigo, Alessandria, Italy
3Department of Basic and Applied Sciences for Engineering (SBAI), Sapienza University, Rome, Italy
- *Corresponding Author:
- Federica Nicoletta Sepe,
Department of Emergency Neurology and Stroke Unit, IRCCS C. Mondino Foundation, Pavia, Italy
E-mail: federica.sepe@mondino.it
Received date: November 14, 2024, Manuscript No. IPBBB-24-19954; Editor assigned date: November 18, 2024, PreQC No. IPBBB-24-19954 (PQ); Reviewed date: December 02, 2024, QC No. IPBBB-24-19954; Revised date: December 09, 2024, Manuscript No. IPBBB-24-19954 (R); Published date: December 16, 2024, DOI: 10.36648/2347-5447.12.4.64
Citation: Sepe FN, Lanni C, Michekis D, Lancia G (2024) The Impact of Psychological Treatment on Catastrophization and Pharmacological Response in Chronic Migraine: A Single-Center Experience. Br Biomed Bull Vol.12 No.4: 64.
Abstract
Background: This study aimed to evaluate how pain catastrophizing, measured by the Italian Pain Catastrophizing Scale (PCS), influences clinical outcomes in chronic migraine patients. It employed a multidisciplinary approach, including psychological treatment.
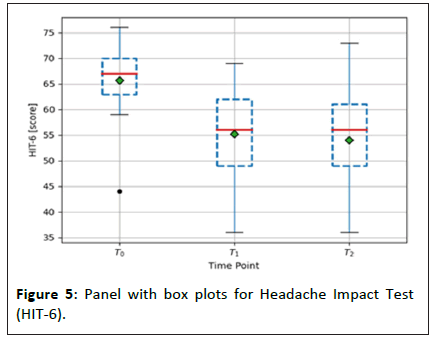
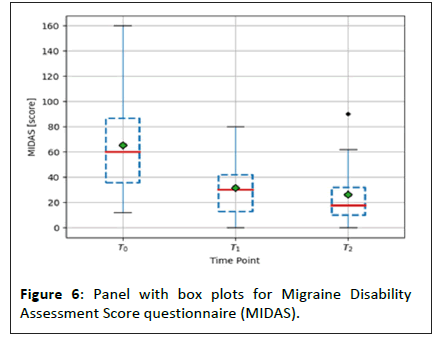
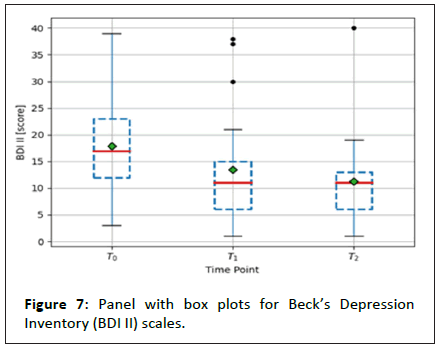
Methods: Twenty-five outpatients from the SS. Antonio e Biagio e Cesare Arrigo headache clinic were randomly assigned Galcanezumab, Erenumab, or Fremanezumab. Over six months, their responses were assessed by measuring monthly migraine day reductions and improvements in quality of life using Headache Impact Test (HIT-6), Migraine Disability Assessment Score questionnaire (MIDAS) and Beck’s Depression Inventory (BDI) II scales for comorbid depression evaluation.
Results: We identified a robust correlation between HIT-6 and PCS, showing coefficients of 0.81 at T1 and 0.88 at T2. Additionally, we did not observe any other significant correlations.
Conclusion: This study seeks to elucidate the impact of a multidisciplinary approach, which includes psychological follow-up, on a specific clinical phenotype of chronic migraines characterized by a heightened tendency to catastrophize however, more extensive data are required.
Keywords
Psychological treatment; Chronic migraine; Catastrophization; Pain catastrophizing scale
Introduction
The Pain Catastrophizing Scale (PCS) is a 13-item self-report measure of catastrophizing in pain and a well-validated measure of maladaptive thinking patterns related to pain. The PCS is composed by 3 subscales: Rumination (e.g, “I can't stop thinking about how much it hurts”), magnification (e.g, “I worry that something serious may happen”) and helplessness (e.g, “There is nothing I can do to reduce the intensity of the pain”) [1]. People affected by chronic headache, defined accordingly to the 3rd edition of the International Classification of Headache Disorders (ICHD III) [2], represent a consistent group of patients suffering by chronic pain. Give the best medical response to those patients, affording the considerable economic costs and psychological burden related to chronic pain, is a huge healthcare challenge. Since the 90s, researchers focused on the role of anxiety and mood disorders as comorbidities in migraine, without describing the specific role of patient’s personality in the processing of pain [3-5]. Catastrophizing can be considered as a maladaptive cognitive response at a painful stimulation that influences negatively pain perception [6]. In high frequency migraine patients evoked pain-related activity in the white matter structure of the insula correlate with pain catastrophizing and migraine severity [7]. Furthermore, in patients with Medication-Overuse Headaches (MOH), higher total PCS score was associated with decreased in gray matter density in precentral and inferior temporal gyrus as an increased restingstate functional connectivity between middle temporal gyrus and cerebellum [8]. An abnormal reward mechanisms dopamine mediated can explain these structural changes: High frequency migraine attacks induced a sustained increase in dopaminergic trafficking that override homeostatic feedback control. This massive dopaminergic tone in reward could lead a motivation and learning centers to actuate abnormal coping strategies such as catastrophizing for pain [8,9]. Even if the role of pain-related cognitive processes and emotional state on pain-related disability is well established [10], how catastrophizing can influence therapeutical response in the Calcitonin-Gene Related Peptide (CGRP-mAbs) antibodies era is still debated. Interestingly, refractory migraine patients to CGRP-mAbs showed higher baseline PCS scores representing an independent negative predictor to CGRP-mAbs response [11-13].
This study aims to assess the potential impact of pain catastrophizing on the clinical response to CGRP-mAbs in a reallife setting at a tertiary headache center in Northern Italy.
Materials and Methods
Study population
In this monocentric observational study, we enrolled 25 consecutive outpatients who visited the "SS. Antonio e Biagio e Cesare Arrigo" headache clinic between July 2021 and 2023. These were diagnosed with chronic migraine, with or without medication overuse, based on the ICDH III criteria. They were randomly assigned to receive one of three medications Galcanezumab (120 mg), Erenumab (140 mg), or Fremanezumab (225 mg) following the local and European Academy of Neurology (EAN) guidelines [14].
The therapeutical response was assessed using two criteria: A >50% reduction in the frequency of a number of days with migraine per month and a decrease in disability using the Migraine Disability Assessment Test (MIDAS) scale [15] and the Headache Impact Test-6 (HIT-6) scale [16] according to local and EAN guidelines. We also evaluated comorbid depression using the Beck Depression Inventory-II (BDI II) scale (BDI II >13) [17]. Patients were assessed at the beginning of therapy (T0) and again at three months (T1) and six months (T2) after the start of treatment (Supplementary Tables 1).
Each patient was treated by a neurologist and a psychologist specializing in the field. The study excluded individuals with medical, psychiatric, or cognitive limitations, as well as those suffering from chronic pain conditions or with a history of substance abuse. The sociodemographic and clinical characteristics of patients are reported in Supplementary Tables 2-4.
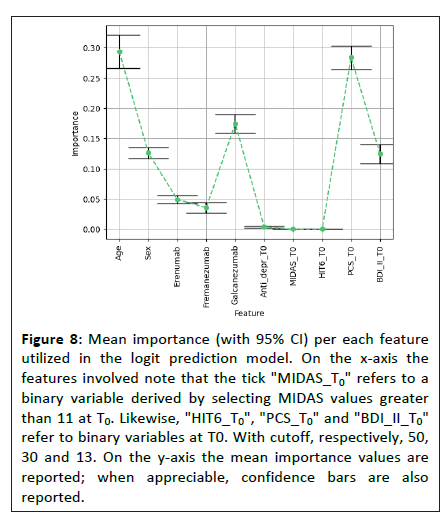
Statistical analysis
As a primary outcome, we investigated the correlation between PCS and HIT-6 at T0, T1 and T2 using Spearman’s correlation test. We also examined the association between PCS and MIDAS and PCS and BDI II at these time points. We also assessed the reduction in MIDAS and HIT-6 using Wilcoxon’s test. Using the Jaccard Index, we investigated the similarity of subgroups of patients showing severe catastrophization (PCS >30) as headache-related disability, considering HIT-6 >50 and MIDAS >11 separately. Depression at T0 was controlled using BDI II (>13) as the antibody assigned. Using a logit approach, we explored the red baseline information at T0. The outcome variable was defined as a relative reduction of MIDAS >50% between T0 and T2. Permutation importance identified the most impactful features for improving quality of life.
To determine the sample size, we focused on the primary outcome of PCS and HIT-6 correlation through Spearman’s test. We estimated a sample size of 21, adjusted to 25 for a 15% dropout rate.
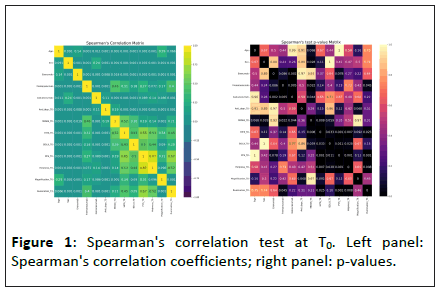
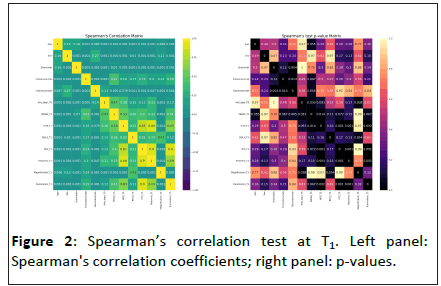
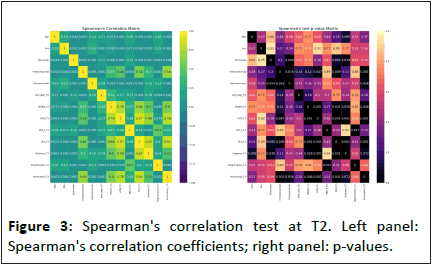
We used a simple randomization scheme to assign antibody therapy, ensuring equal assignment probabilities. Despite more patients receiving Galcanezumab, the chi-squared test confirmed no significant distribution difference among patients as given by Figures 1-3 (Supplementary Tables 5 and 6).
Results
The null hypothesis of no correlation between PCS and HIT-6 was rejected at T0, T1 and T2. Spearman’s correlation coefficients were 0.65, 0.81 and 0.88 at T0, T1 and T2, respectively. These results describe a robust positive timedependent correlation between PCS and HIT-6 scores.
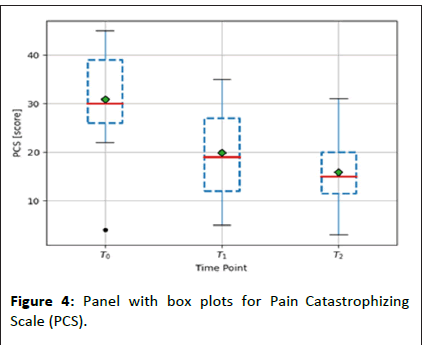
For PCS and MIDAS, the null hypothesis of no correlation could only be rejected at T2, with a correlation coefficient of 0.81. So, as expected, a reduction in the tendency to catastrophize will directly impact the quality of life and the number of attacks per month measured by the MIDAS scale. We noticed a significant difference in all the scale scores between T0 and T1 and between T0 and T2. Look at Figures 4-7 for a detailed breakdown.
Figure 7: Panel with box plots for Beck’s Depression Inventory (BDI II) scales.
These four figure colors are indicated into the interquartile range is enclosed within the box, while the red dashed line is the median value. The green diamond is the average value. Black dots denote outliers.
At the beginning of the study (T0), the Jaccard index indicated a 47% agreement between the reduction of severe catastrophization scores and the other scales. This result suggests that 47% of patients with high PCS scores will respond positively (the highest reduction in monthly migraine days) to both psychological and pharmacological treatments. This reduction occurred regardless of the type of antibody, except for a slight correlation with Galcanezumab treatment. Our model suggests that comorbid depression and antidepressant therapy at T0 have no influence.
The logit-based model had an AUROC of 0.75 (95% CI 0.73-0.78), i.e., with a probability of 75% of one patient at six months from the beginning of the therapy to have an excellent clinical response as previously defined.
The logit-based model was inspected through the permutation importance method, age, Galcanezumab and PCS score at T0 were the main factors in the clinical response, with importance scores of 0.29, 0.17 and 0.28 (95% CI 0.26-0.32, 0.15-0.18, 0.26-0.30) respectively.
Missing values resulted from right censoring, affecting six patients at either T1 or T2. We handled the missing data by analyzing all available data we excluded patients whose therapy was interrupted and for whom no further information was available (Figure 8).
Figure 8: Mean importance (with 95% CI) per each feature utilized in the logit prediction model. On the x-axis the features involved note that the tick "MIDAS_T0" refers to a binary variable derived by selecting MIDAS values greater than 11 at T0. Likewise, "HIT6_T0", "PCS_T0" and "BDI_II_T0" refer to binary variables at T0. With cutoff, respectively, 50, 30 and 13. On the y-axis the mean importance values are reported; when appreciable, confidence bars are also reported.
Discussion
Our hypothesis posits that rumination, as a self-psychological condition, may directly influence the clinical efficacy of CGRP antibodies, particularly in cases deemed refractory. We propose that a multidisciplinary approach incorporating psychological support can significantly improve clinical response, especially for those exhibiting an inadequate response to treatment. However, identifying the specific patient phenotype that will benefit the most from this approach remains challenging. Surprisingly, patients with the best clinical response appear to be female and younger, with higher PCS scores at baseline, regardless of comorbid depression. Galcanezumab seems to be more effective. There is a significant time-dependent correlation between the reduction in PCS and HIT6 scores, particularly when longer medical and psychological therapies have been administered. This is independent of the number of attacks reported as of antidepressant previous therapies or depression. This suggests that a holistic treatment approach combining pharmacological and psychological interventions is more likely to improve the quality of life for chronic migraine patients.
In a recent study, the HIT-6 score was found to have a weak correlation with PCS scores [18]. However, no investigation was made into the correlation between any therapy and these variables. Another multicentric study also found that helplessness and anxiety are linked to the social quality of life of migraine patients when compared to controls. However, no correlations to Abs treatment were identified. We agree with previous theses that pain catastrophizing may indicate a clinical phenotype with heightened expression of altered central sensitization and consequential coping mechanisms leading to an overall decrease in quality of life [19]. Identifying the various factors that drive the progression of chronic migraine is vital to developing effective prevention strategies [20]. Other real-world studies demonstrated that CGRP antibodies were able to exert an excellent clinical response across subgroups of migraine patients with comorbid psychological traits, mainly anxiety and depression [21,22].
Unfortunately, this study has several limitations, mainly due to its observational monocentric design: The small sample size, the absence of a control group and the short observation time. Further data of a more extensive nature is imperative to substantiate our findings.
Conclusion
Treatment-related and individual factors contribute to the development of chronic migraine. A comprehensive approach is essential for individuals, encompassing both pharmacological and non-pharmacological interventions, as well as the management of behavioral and psychological factors. The development of personalized tools for predicting chronification represents a significant research priority. This study aims to delineate a clinical phenotype of chronic migraine patients characterized by a propensity to catastrophize. It advocates for a combined therapeutic strategy utilizing CGRP monoclonal antibodies alongside psychological counseling to enhance quality of life. Further investigation is necessary to assess the clinical implications of this integrative approach.
Ethical Approval
The local clinical research ethics committee approved the study (number of approval ASO.NEURO.21.02) and all patients signed informed consent forms.
Acknowledgements
The authors wish to express their gratitude to the Azienda Sanitaria SS. Antonio e Biagio e Cesare Arrigo for their support.
Conflict of Interest
The authors have no conflicts of interest.
References
- Monticone M, Baiardi P, Ferrari S, Foti C, Mugnai R, et al. (2012) Development of the Italian version of the Pain Catastrophising Scale (PCS-I): Cross-cultural adaptation, factor analysis, reliability, validity and sensitivity to change. Qual Life Res 21: 1045-1050.
[Crossref] [Google Scholar] [Indexed]
- Headache Classification Committee of the International Headache Society (IHS) (2013) The international classification of headache disorders, 3rd edition. Cephalalgia 33: 629-808.
- Pelzer N, de Boer I, van den Maagdenberg AMJM, Terwindt GM (2023) Neurological and psychiatric comorbidities of migraine: Concepts and future perspectives. Cephalalgia 43: 1-15.
[Crossref] [Google Scholar] [Indexed]
- Lipton RB, Buse DC, Nahas SJ, Tietjen GE, Martin VT, et al. (2023) Risk factors for migraine disease progression: A narrative review for a patient-centered approach. J Neurol 270: 5692-5710.
[Crossref] [Google Scholar] [Indexed]
- Klonowski T, Kropp P, Straube A, Ruscheweyh R (2022) Psychological factors associated with headache frequency, intensity and headache-related disability in migraine patients. Neurol Sci 43: 1255-1266.
[Crossref] [Google Scholar] [Indexed]
- Mathur VA, Moayedi M, Keaser ML, Khan SA, Hubbard CS, et al. (2016) High-frequency migraine is associated with lower acute pain sensitivity and abnormal insula activity related to migraine pain intensity, attack frequency and pain catastrophizing. Front Hum Neurosci 10: 489.
[Crossref] [Google Scholar] [Indexed]
- Kocakaya H, Say B, Yörübulut S, Ergün U (2023) Emotion dysregulation in migraine patients: Can it be a hallmark of the probability of the transformation from episodic to chronic? Neurol Res 45: 610-618.
[Crossref] [Google Scholar] [Indexed]
- Christidi F, Karavasilis E, Michels L, Riederer F, Velonakis G, et al. (2020) Dimensions of pain catastrophizing and specific structural and functional alterations in patients with chronic pain: Evidence in medication-overuse headache. World J Biol Psychiatry 21: 726-738.
[Crossref] [Google Scholar] [Indexed]
- Maizels M, Aurora S, Heinricher M (2012) Beyond neurovascular: Migraine as a dysfunctional neurologic pain network. Headache 52: 1553-1565.
[Crossref] [Google Scholar] [Indexed]
- Å?entürk IA, Turan SA, Eyigürbüz T, Å?entürk E, Içen NK (2023) Pain-related cognitive processes, pain interference and alexithymia in patients with primary headaches. Cureus 15: e39688.
[Crossref] [Google Scholar] [Indexed]
- Alvarez-Astorga A, García-Azorín D, Hernández M, de la Red H, Sotelo E, et al. (2021) Pain catastrophizing in a population of patients with migraine. Neurologia 36: 24-28.
[Crossref] [Google Scholar] [Indexed]
- Silvestro M, Tessitore A, di Clemente FS, Battista G, Tedeschi G, et al. (2021) Refractory migraine profile in CGRP-monoclonal antibodies scenario. Acta Neurol Scand 144: 325-333.
[Crossref] [Google Scholar] [Indexed]
- Mitsikostas DD, Edvinsson L, Jensen RH, Katsarava Z, Lampl C, et al. (2014) Refractory chronic cluster headache: A consensus statement on clinical definition from the European headache federation. J Headache Pain 15: 79.
[Crossref] [Google Scholar] [Indexed]
- Sacco S, Amin FM, Ashina M, Bendtsen L, Deligianni C, et al. (2022) European headache federation guideline on using monoclonal antibodies targeting the calcitonin gene-related peptide pathway for migraine prevention-2022 update. J Headache Pain 23: 67.
[Crossref] [Google Scholar] [Indexed]
- Stewart WF, Lipton RB, Dowson AJ, Sawyer J (2001) Development and testing of the Migraine Disability Assessment (MIDAS) questionnaire to assess headache-related disability. Neurology 56: S20-28.
[Crossref] [Google Scholar] [Indexed]
- Rendas-Baum R, Yang M, Varon SF, Bloudek LM, DeGryse RE, et al. (2014) Validation of the Headache Impact Test (HIT-6) in patients with chronic migraine. Health Qual Life Outcomes 12: 117.
[Crossref] [Google Scholar] [Indexed]
- Schotte CK, Maes M, Cluydts R, de Doncker D, Cosyns P (1997) Construct validity of the beck depression inventory in a depressive population. J Affect Disord 46: 115-125.
[Crossref] [Google Scholar] [Indexed]
- Kim S, Bae DW, Park SG, Park JW (2021) The impact of pain-related emotions on migraine. Sci Rep 11: 577.
[Crossref] [Google Scholar] [Indexed]
- Sciruicchio V, Simeone M, Barbaro MGF, Tanzi RC, Delussi MD, et al. (2019) Pain catastrophizing in childhood migraine: An observational study in a tertiary headache center. Front Neurol 10: 114.
[Crossref] [Google Scholar] [Indexed]
- Bottiroli S, Renzi A, Ballante E, De Icco R, Sances G, et al. (2023) Personality in chronic headache: A systematic review with meta-analysis. Pain Res Manag 2023: 1-19.
[Crossref] [Google Scholar] [Indexed]
- Driessen MT, Cohen JM, Thompson SF, Patterson-Lomba O, Seminerio MJ, et al. (2022) Real-world effectiveness after initiating fremanezumab treatment in US patients with episodic and chronic migraine or difficult-to-treat migraine. J Headache Pain 23: 56.
[Crossref] [Google Scholar] [Indexed]
- Smitherman TA, Tietjen GE, Schuh K, Skljarevski V, Lipsius S, et al. (2020) Efficacy of galcanezumab for migraine prevention in patients with a medical history of anxiety and depression: A post hoc analysis of the phase 3, randomized, double-blind, placebo-controlled REGAIN and pooled EVOLVE-1 and EVOLVE-2 studies. Headache 60: 2202-2219.
[Crossref] [Google Scholar] [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences