State of Art of the French Telemedicine Projects in the Field of Chronic Heart Failure
E Andres1,2*, S Talha2,3, M Hajjam4 and A Hajjam5
11Department of Internal Medicine, Diabetes and Metabolic Diseases, Medical Clinic B, Strasbourg University Hospitals, Strasbourg, France
22Faculty of Medicine of Strasbourg, University of Strasbourg, Strasbourg, France
33Department of Physiology and Functional Explorations, Strasbourg University Hospitals, Strasbourg, France
44PREDIMED Technology, Strasbourg, France
5University of Technology Belfort-Montbéliard, Belfort-Montbéliard, France
- *Corresponding Author:
- Prof. Emmanuel Andrès
Department of Internal Medicine, Diabetes and Metabolic Diseases, Medical Clinic B
Strasbourg University Hospitals, Strasbourg, France
Tel: 33388115066
E-mail: emmanuel.andres@chru-strasbourg.fr
Received date: April 25, 2018; Accepted date: May 11, 2018; Published date: May 18, 2018
Citation: Andres E, Talha S, Hajjam M, Hajjam A (2018) State of Art of the French Telemedicine Projects in the Field of Chronic Heart Failure. J Clin Med Ther. 3:8.
Copyright: © 2018 Andres E. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: This is a narrative short review of the literature pertaining to telemedicine projects developed in the field of chronic heart failure (CHF), with special attention to the French projects.
Results: Numerous telemedicine projects, based on connected objects or information and communication technology (ICT), have emerged over the last five years or are under development in the field of CHF. This is the case of the telemedicine projects: SCAD, OSICAT, PIMS, MEDICA and E-care. The E-care project is a French telemonitoring project of new generation. This project support patients returning home after hospital. It fits perfectly within the framework of telemedicine 2.0 projects, including for the first time artificial intelligence (AI). This project has been specifically designed to automatically detect situations at risk for CHF. The potential contribution of these French projects (OSICAT, Ecare) is currently under study or documentation, especially in terms of mortality or morbidity, in addition to number of hospitalizations avoided, or economic benefits.
Keywords
Telemedicine; Artificial intelligence; Information and communication technology; Heart failure
Introduction
The rising prevalence of chronic disease like chronic heart failure (CHF) combined with population aging now represents a very real problem for public health [1]. In France, between 120 000 and 150 000 new cases are diagnosed every year [2]. The cost of this chronic disease has rocketed, and is estimated at several billion dollars in developed countries [1]. The management of CHF patients is a challenge for healthcare professionals. Their needs eat up large amounts of medical resources, just as a shortage in the time careers can provide is beginning to be felt, with medical deserts and a lack of access to healthcare professionals, among other problems.
CHF remains a serious disease in terms of their functional or survival prognosis, and morbidity and mortality are high [1]. Thus, the mortality rate of CHF patients with NYHA stage III-IV is 50% at 5 years (although closer to 30% in more recent studies) [2,3]. In this setting, CHF patients frequently present for emergency hospitalization and re-hospitalization [1,2]. CHF is responsible for more than 100 000 hospitalizations per year in France [2]. It accounts for 5% of all hospitalizations and is the main cause of hospitalization among elderly subjects [2]. Some of these hospitalizations could be avoided if patients have a better followed [1]. This last point has been particularly well documented in CHF [1,4]. In this setting, telemedicine may be of really aid. Indeed telemedicine may even optimize the management of such chronic disease, particularly by preventing emergency and repeat hospitalizations [2,4].
In this article we review the literature on French telemedicine projects developed in the area of CHF.
Search Strategy
A literature search was performed on the PubMed database of the US National Library of Medicine and on Scholar Google. We searched for articles published between January 2010 and April 2018, using the following key words or associations: “heart failure”, “telemedicine”, “e-Health”, “telemedicine in heart failure” and “e-Health in heart failure”; restrictions included: English- or French-language publications; published from January 1, 2010, to April 1, 2018; human subjects; clinical trials, review articles or guidelines. All of the English and French abstracts were reviewed by at least two senior researchers from our work group. After rigorous selection, only 20 papers and fewer than 4 projects under study were selected and analyzed. The latter (references [4-35]) were used to write this paper in the form of a narrative short review. Information gleaned from international meetings was also used, as information gleaned from commercial sites on the web.
Results of Published Telemedicine Projects
General data on structured telephone support and first generation telemonitoring
Since the beginning of the 2000’s, numerous telemedicine projects have been conceived and developed in the area of CHF [6-22]. Practically, all of them have investigated “telemonitoring” (or tele management, as it is also known in the literature), as defined under French legislation [23]. To our knowledge, no completed projects have been published on “tele-consultation” and “tele-expertise” in the area of CHF. Some of the projects have very specifically investigated CHF subjects aged over 75 or over 80 [24,25]. It is worth bearing in mind that those projects, particularly the earlier ones, more closely resembled telephone follow-up with care providers (such as a nurse) traveling to the patient's home, rather than telemedicine as we think of it nowadays with nonintrusive, automated, smart telemonitoring using remote sensors via modern communication technology or even artificial intelligence (AI) [4,21]. Hence in our opinion those studies represent the first generation of telemedicine projects [4,15].
Clinical impact of first generation telemedicine projects
As we will see, the results of telemedicine projects in the field of CHF differed from study to study and were fairly inconclusive regarding any potential clinical benefit in terms of, for instance, re-hospitalization or a decrease in morbidity and mortality (Table 1) [6-22]. This particularly applied to the statistical significance of the results. Because of this, the experts had divided opinions about the real utility of telemedicine in the management of CHF patients. Nevertheless, telemedicine is recommended with a low level of evidence for such patient follow-up by the European Society of Cardiology. In this setting, it should also be pointed out that the studies were conducted with sometimes inappropriate methodologies, in unsuitable patient groups (such as NYHA stage I) and, above all, in small patient samples (of between 50 and 1000 patients) with very short follow-up periods (of between 3 months and 1 year). In our opinion, this made any clinical benefit they demonstrated illusory [4,21]. Despite these limitations, several reviews and meta-analyses seem to have shown an undeniable utility for telemedicine [3,17].
| Global mortality | Therapeutic education |
| Heart failure mortality | Hygiene-dietary and therapeutic observance |
| Hospitalization for heart failure | Optimization of food and sports hygiene |
| Iterative hospitalization for heart failure | Self-patient management |
| Number of hospitalization days | Optimization of the fitness trail |
| Health cost | Structuring of the fitness trail |
| Heart failure management cost | City-hospital relations |
| Number of days off work | Information sharing within heath professional |
| Quality of life | System use by health professionals |
Table 1: Potential studied parameters for impact documentation of telemedicine in chronic heart failure patient.
For instance, Inglis, et al. [17] found that telemedicine had an effect on all-cause mortality, which fell significantly by 34% (p<0.0001). In that study, the authors also revealed that rehospitalization for CHF fell by 20%, that the quality of life of patients and cost of management improved, and that the system was well accepted. In the meta-analysis by Anker et al. [4], 11 studies were analyzed as part of a comparison between the effects of telemonitoring and routine care (non-invasive telemedicine). Their research revealed that telemonitoring led to a reduction of all-cause mortality (10.4% vs. 15.4%; p < 0.0001), all-cause hospitalization (47.2% vs. 52.1%; p = 0.02), and hospitalization for CHF (22.4% vs. 28.5%; p = 0.008).
Conversely, two prospective clinical trials, the “gold standard”, have produced results that contradict the previous ones and question the potential utility of telemedicine in CHF [18,19]. The Tele-HF study randomized patients hospitalized for CHF to telemonitoring (n=826) or standard care (n=827) [18]. Patients were randomized to either voice-based interactive structured telephone support or usual care. Those in the intervention arm were advised to call a toll-free telephone system and answer a series of questions regarding their general health, weight, and HF symptoms on a daily basis. A clinician then analyzed the information. The study found no significant difference between the telemonitoring and standard management groups in terms of all-cause readmission or all-cause mortality in the 180 days after inclusion (odds ratio [OR]: 1.04 [CI95%: 0.91-1.19]). The primary outcome, all-cause readmission or death within 180 days after enrollment occurred in 52.3% of the telemonitoring group and 51.5% of the usual care group. However, there was poor adherence despite system generated reminders: 14% of patients in the telemonitoring arm of the study never used the system. By the final week, only 55% of the patients were using the system at least three times a week.
The TIM-HF study in Germany randomly compared two groups of patients with stable CHF, namely those followed by telemonitoring (n=354) and those receiving standard care (n=356) [19]. The TIM-HF trial studied 710 stable CHF patients randomized to either remote monitoring and telephone support or usual care. Patients were given a personal digital assistant (PDA) with a wireless Bluetooth interface. The system collected electrocardiogram data, blood pressure readings, and body weight; this information was then communicated wirelessly to a central location with physician presence 24 h a day, 7 days a week. In that study, the all-cause mortality rate was 8.4 per 100 patient-years of follow-up in the telemedicine group and 8.7 per 100 patient-years of follow-up in the standard care group (OR: 0.97 [CI95%: 0.67-1.41]; p=0.87). The TIM-HF trial was underpowered to detect a significant difference in mortality between the two groups. The composite secondary outcomes of hospitalization for HF and death due to a cardiovascular cause (14.7% vs. 16.5%) highlight the stable nature of the patients recruited in the study given population- and trial-based observations of readmission rates closer to 50%.
Financial impact of first generation telemedicine projects
Aside from these medical considerations, it is worth noting that all the studies seem to agree that using telemedicine solutions in the management of CHF was at least economically beneficial (Table 1) [6-21]. Depending on the study, the savings were calculated to be between $5,000 and more than $50,000/year/patient depending on the stage of CHF and the setting of the study. For instance, in the study by Scalvini et al. [22] the cost of managing CHF patients fell by 24%, and hospital costs fell by €45,186/patient/year.
In this setting, the study by Burdese et al. [25] is one of the most convincing for illustrating the utility of tele management in CHF elderly patients. In this study, a significant fall was observed in re-hospitalization (35 without vs. 12 with telemedicine, p = 0.0001), in visits to the emergency department for an acute episode of HF (21 vs. 5/y, p = 0.0001) and in the cost of management (€116,856 vs. €40,065/y). What's interesting is that only 8.6% of the patients discontinued tele management, showing that it was well accepted.
Results of French Telemedicine Projects Currently Underway
General data
Over the last 4 to 5 years, a second generation of projects has emerged in the CHF area, particularly in France [21,26-31]. These projects are known as "telemedicine 2.0", because they utilize the new “Information and Communication Technology” (ICT) and the web. They satisfy the conditions of telemedicine as laid out in France in Article 36 of the Social Security Financing Act (Table 1) [5]. Most of these projects rely on the usual connected tools for monitoring CHF, such as blood pressure meters, weighing scales, and pulse oximeters, which relay the information collected via Bluetooth, 3G or 4G and incorporate tools for interaction between the patient and healthcare professionals like telephone support centers, tablets, and websites [21]. Some of them also provide tools for motivation and education, and occasionally, questionnaires about symptoms, such as dyspnea, palpitation and edema as experienced by the patient.
The main new telemedicine projects currently being developed in France are:
• SCAD: “Suivi CArdiologique à Distance” [remote cardiological follow-up], first initiated in 2005, deployed in the low Normandie, France between 2009 April and May 2012, developed by Caen University Hospital [26].
• PIMPS: “Plateforme Interactive Médecins patients Santé” [doctor-patient interactive health platform], initiated in 2013, developed by René-Dubos hospital in Pontoise, France, and Professor Jourdain [27].
• OSICAT: “Optimisation de la Surveillance ambulatoire des Insuffisants CArdiaques par Télécardiologie” [optimization of outpatient monitoring in heart failure patients using telecardiology], initiated in 2012, involving 12 local investigation centers coordinated by Toulouse University Hospital and Professors Galinier and Pathak [28].
• MEDICA: “Monitorage Electronique à Domicile de l’Insuffisance CArdiaque chronique” [electronic homemonitoring of chronic heart failure], initiated in 2014, developed by the REUNICA domicile and GMC-solutions santé groups working in social protection of the elderly [29].
• E-care: “Détection des situations à risque de décompensation cardiaque chez les patients insuffisants cardiaques de stade III de la NYHA” [detection of risk situations for cardiac decompensation in heart failure patients with NYHA stage-III disease], initiated in 2014, the medical aspects of which were developed by Strasbourg University Hospital [30,31].
All these projects are run with the aid of the telemedicine 2.0 tools discussed above. The PIMPS project also comprises laboratory monitoring of natriuretic peptide [27]. These projects center on cohorts of CHF patients or prospective studies. They have enrolled relatively large patient samples, and most of them are based on data from evidence-based medicine. The OSICAT study seems the most advanced [28]. It was launched in 2013 and has enrolled 990 patients divided into two groups, remote home-monitoring and controls receiving standard care.
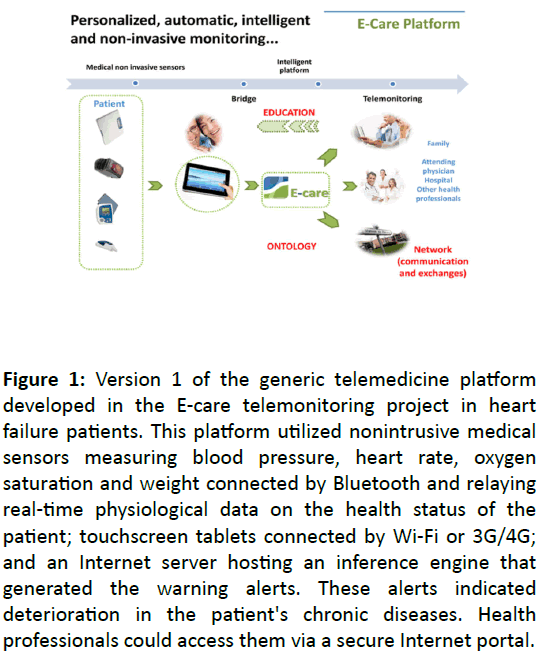
The results will include an assessment of medical efficacy and cost-effectiveness, and are expected in 2018. To our knowledge, only E-care project includes artificial intelligence tools [30,31]. The E-care telemonitoring project in Strasbourg falls under this category of telemedicine 2.0. It has been developed to optimize the home-monitoring of CHF patients. It detects situations in which there is a risk of cardiac decompensation and re-hospitalization, and it does this via a telemonitoring 2.0 platform. The E-care platform automatically generates indicators of a worsening of the patient's health status. These "warning alerts" are generated for any decompensation of a chronic disease, particularly CHF, which may lead to hospitalization if not treated. To our knowledge, it is the first project that used artificial intelligence (AI) in addition to information and communication technologies. The platform includes connected nonintrusive medical sensors, a touchscreen tablet that is connected by Wi-Fi and a router or 3G/4G, making it possible to interact with the patient and provide education on treatment, diet and lifestyle (Figure 1). The E-care system includes a server that hosts the patient's data and a secure Internet portal to which the patient and the various hospital- and non-hospital-based healthcare professionals can connect. E-care is based on a smart system comprising an inference engine and a medical ontology for personalized synchronous or asynchronous analysis of data specific to each patient and, if necessary, the sending of an alert generated by AI [32].
Figure 1: Version 1 of the generic telemedicine platform developed in the E-care telemonitoring project in heart failure patients. This platform utilized nonintrusive medical sensors measuring blood pressure, heart rate, oxygen saturation and weight connected by Bluetooth and relaying real-time physiological data on the health status of the patient; touchscreen tablets connected by Wi-Fi or 3G/4G; and an Internet server hosting an inference engine that generated the warning alerts. These alerts indicated deterioration in the patient's chronic diseases. Health professionals could access them via a secure Internet portal.
Clinical impact of the French telemedicine projects
To date, clinical results are only available for SCAD and Ecare projects [26,31]. In the SCAD project, 90 patients were randomized from 2009 April to 2011 May (n=45 for each group) (Thesis from the Faculty of Medicine from Caen, France). The population is elderly, with a mean age of 78 ± 6 years, mostly male (78%) and at high risk of re-hospitalization (mean BNP level of 1,025 ± 950 pg/mL). At 12 months, 1,040 days of hospitalization for acute heart failure were recorded. Monitoring by educational telemedicine significantly reduced the number of hospital days for acute heart failure: 590 days in the “control group” vs. 450 days in the “telemedicine group” (p=0.044). The criterion "death or hospitalization for acute heart failure" occurred less frequently in the telemedicine group: 57.8% in the “control group” vs. 35.6% in the “telemedicine group” (p <0.05). During CHF readmissions, telemedicine-treated patients had lower intra-hospital mortality: 18.2% vs. 0% (p <0.02).
Between February 2014 and April 2015, 175 patients were given the chance to use the E-care platform [30]. During this period, the E-care platform was used on a daily basis by patients and healthcare professionals according to a defined protocol of use specific to each patient. The mean age of these patients was 72 years and the ratio of men to women was 0.7. The patients suffered from multiple concomitant diseases and had a mean Charlson index of 4.1. The five main diseases were: CHF in more than 60% of the subjects, anemia in more than 40%, atrial fibrillation in 30%, type II diabetes in 30%, and chronic obstructive pulmonary disease in 30%. During the study, 1500 measurements were taken in these 175 patients, which resulted in the E-care system generating 700 alerts in 68 patients [33]. Some 107 subjects (61.1%) had no alerts during follow-up. Analysis of the follow-up of these 107 patients revealed that they had no clinically significant events that might eventually have led to hospitalization. Analysis of the warning alerts showed that the E-care platform automatically and non-intrusively detected any worsening of the patient's health, particularly CHF. Indeed, it was in this last setting that the system yielded the best sensitivity, specificity, and positive and negative predictive values, respectively 100%, 72%, 90% and 100%. The E-care platform also showed its ability to detect a deterioration in health status via the multiple diseases of the patients studied, with sensitivity, specificity, and positive and negative predictive values of, respectively 100%, 30%, 89% and 100%.
Perspectives on new telemedicine projects in France
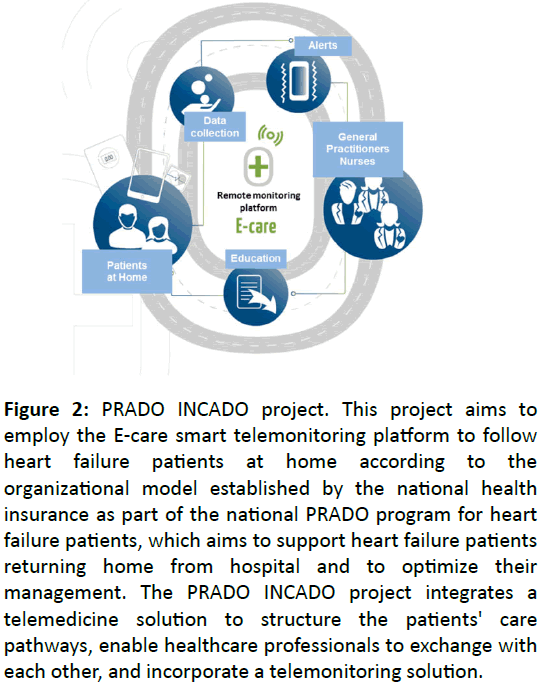
As discussed above, the E-care platform appears to be capable of preventing hospitalization by detecting any deterioration in the patient's health status early and by making it possible for the care providers in charge of the patient to be warned and, above all, to intervene [30,31]. The E-care platform as others’ currently underway is also capable of structuring the patients’ cares pathways, a major theme in medicine for our governments and authorities (Table 1). It is also capable of providing a means for the various healthcare professionals to exchange with each other; and of facilitating access to medical resources. With this in mind, an enhanced version of the E-care platform will be experimented in the homes of heart failure patients as part of a project called PRADO INCADO (Figure 2) [32].
Figure 2: PRADO INCADO project. This project aims to employ the E-care smart telemonitoring platform to follow heart failure patients at home according to the organizational model established by the national health insurance as part of the national PRADO program for heart failure patients, which aims to support heart failure patients returning home from hospital and to optimize their management. The PRADO INCADO project integrates a telemedicine solution to structure the patients' care pathways, enable healthcare professionals to exchange with each other, and incorporate a telemonitoring solution.
The project is being run by a group bringing together Strasbourg University Hospital, the Alsatian regional health agency, the Bas-Rhin branch of France's national health insurance, and the company PREDIMED Technology. This project will allow us to conduct an in-depth study so as to improve diagnosis by aiding machine learning and, therefore, detect abnormalities early. This is in keeping with the research of Mortazavi et al. on the utility of AI in managing CHF patients, particularly the possibility afforded by artificial intelligence of predicting re-hospitalization for CHF [34].
Telemedicine Projects in other Field of Chronic Diseases
Diabetes
Diabetes and metabolic disorders are other fields of priority investigation of telemedicine in France, outside CHF. Innovative projects are being developed or deployed, such as the PLASIDIA platform, run by the European Center for the Study of Diabetes [35]. It is in this setting, we developed an up graduate version of the E-care platform to follow patients suffered from diabetes mellitus under the DIABETe project. The new version of the E-care platform should be deployed in “complex diabetic” patients; e.g. diabetic patients with high cardiovascular risk or diabetic patients treated with multiple injections [36]. The objective of the DIABETe project is to detect early the risk of hospitalization of diabetic patients with a very high cardiovascular risk: personal history of stroke, IDM, amputation and cardiomyopathy, with intensive insulin therapy (minimum of 3 injections per day or pump), through a personalized follow-up and accompany the patient in the knowledge of his illness and his management. This population is interesting because it allows targeting poly-pathology and poly-medication. It requires global support. It represents 50% of diabetics hospitalized in departments of Diabetology and Internal Medicine. Apart from cardiovascular complications (IDM, PAO, etc.), they are also hospitalized for hypoglycemia, imbalance of diabetes, iatrogenic, infections, etc. The DIABETe project is based on an intelligent platform that will assist the medical profession by automating the processing of information from non-intrusive medical sensors (blood glucose meter, blood pressure monitor, actimeter, connected scale, etc.) as well as subjective information from the patient himself (questionnaires) and its behavior (compliance) to detect and report these situations at risk of hospitalization early. Therapeutic education tools adapted to the patient and the situation will be made available to the individual. Communication to the subject will be provided by a touch pad. Alerts testifying to a deterioration of the patient's condition will be generated by AI and reported to health professionals in charge of the patient, to anticipate the decompensation and to afford the means of care outside the emergency setting. These solutions, derived from new technologies, will be innovative and original to offer the best acceptability by patients. It will allow the sharing of medical data between health professionals as part of a city-hospital network. Ultimately, it should also lead to an improvement in the quality of life of the patient.
DIABETe does not compete with Diabeo or other expert systems whose purpose is to optimize the glycemic balance, which in itself is one of the essential objectives of diabetes mellitus [37]. The DIABETe project aims at "global" management of the diabetic patient through the detection of situations at risk of hospitalization: infection, cardiac decompensation, diabetic foot, etc. but also of course hypoglycemia and hyperglycemia leading to hospitalizations. It should also be noted that the remote monitoring platform used in DIABETe is likely to integrate or interface with expert systems such as Diabeo. As a reminder, the Diabeo application, carried by SANOFI, was tested as part of the Télésage clinical trial for 700 patients with DT1 and DT2, under a basal bolus regimen (multi-injection or pump) [28]. The main criterion of the Télésage study is the variation of HbA1c (glycemic control) at one year. A previous study, Télédiab1, conducted between 2007.
Chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease (COPD) is another field of interest of telemedicine. In fact, remote in-home monitoring of symptoms and physiological variables may allow early detection and treatment of exacerbations of COPD. However to date, it is unclear whether telemonitoring improves patient outcomes or healthcare resource utilization. Several “proofs of concept” studies were fairly inconclusive regarding any potential clinical benefit in terms of, for instance, re-hospitalization or a decrease in morbidity and mortality [38-39]. Two randomized trials and several assessments of remote surveillance were included (for review see the reference [39]). Generally, the studies were low-power, had heterogeneous populations, and showed a lack of detailed descriptions of interventions and care management processes accompanying telemonitoring. There were results in terms of measurement but no economic evaluation. Remote monitoring interventions differed widely in each study. Some contained an educational element that could explain the differences between the groups. Despite these reservations, the study reports seem to be positive. From the literature, the best telemonitoring outcomes come from programs dedicated to aged and very sick patients, frequent exacerbators with multi-morbidity and limited community support; programs using 2.0 or 3.0 telemonitoring systems providing constant analytical and decision making support (24 h/day, 7 days/ week); countries where strong community links are not available; and zones where telemonitoring and rehabilitation can be delivered directly to the patient's location (for review see the reference [39]). In regard of the published results, the key to optimizing the use of telemonitoring in COPD is to correctly identify who the ideal candidates are, at what time they need it, and for how long. The time course of disease progression varies from patient to patient; hence identifying for each patient a 'correct window' for initiating telemonitoring could be the correct solution.
Conclusion
Although many telemedicine projects have been conducted in the CHF area, relatively few have been conducted in the setting of telemedicine 2.0 with aid of ICT and the Internet. The E-care telemonitoring project is one that wholly falls under this category. Their potential utility in terms of morbidity, mortality and avoidance of hospital admissions is being studied or documented. Their impact in terms of health savings is also being assessed. The telemedicine 2.0 projects are perfectly compatible with the care pathways being developed in chronic diseases by the French health authorities (including the French ministry of health and the regional branch of the national health insurance). What's more, all these findings should be analyzed with regard to the benefit of these telemedicine solutions (Table 1). This experience may lead us to witness the birth of the medicine of tomorrow. In the field of chronic diseases, given the epidemiology and expected shortage of time careers can provide, what we need is better follow-up and better education, improved prevention and anticipation, but, above all, better selection of the patients whose use of the healthcare system will be indispensable.
Declaration
Competing Interests: M. Hajjam is the scientific Director of PREDIMED Technology.
Funding: None declared.
Ethical approval: Not applicable.
Guarantor: EA.
Contributor ship: EA and ST designed the study and conducted the searches. EA, ST and AH composed the results and parts of the discussion. ST, MH and AH provided critical analysis and revising of all portions of the manuscript and authorised the final version for publication. EA is responsible for all revisions and maintains contact with the rest of the review team with status reports.
Acknowledgements
Fondation de France. Agence Nationale pour la Recherche (ANR) Technologie. Agence Régionale pour la Santé (ARS) du Grand Est.
References
- https://invs.santepubliquefrance.fr/publications/etat_sante_2017/ESP2017_Ouvrage_complet_vdef.pdf
- https://www.has-sante.fr/portail/upload/docs/application/pdf/2012-04/guide parcours de soins ic web.pdf
- Jessup M, Brozena S (2003) Heart failure. N Engl J Med 348: 2007-2018.
- Anker SD, Koehler F, Abraham WT (2011) Telemedicine and remote management of patients with heart failure. Lancet 378: 731-739.
- Puricel SG, Ruiz J (2014) Le diabète et l’ère de la télémédecine. Rev Med Suisse 10: 1246-1248.
- Rosen D, McCall JD, Primack BA (2017) Telehealth Protocol to Prevent Readmission Among High-Risk Patients With Congestive Heart Failure. Am J Med 130: 1326-1330.
- Burdese E, Testa M, Raucci P, Ferreri C, Giovannini G, et al. (2018) Usefulness of a Telemedicine Program in Refractory Older Congestive Heart Failure Patients. Diseases 6: 10.
- Feltner C, Jones CD, Cené CW, Zheng ZJ, Sueta CA, et al. (2014) Transitional care interventions to prevent readmissions for persons with heart failure: a systematic review and meta-analysis. Ann Intern Med 160: 774-784.
- Martínez-González NA, Berchtold P, Ullman K, Busato A, Egger M. (2014) Integrated care programmes for adults with chronic conditions: a meta-review. Int J Qual Health Care 2014;26:561-570.
- Achelrod D (2014) Policy expectations and reality of telemedicine-a critical analysis of health care outcomes, costs and acceptance for congestive heart failure. J Telemed Telecare 20: 192-200.
- Pandor A, Thokala P, Gomersall T, Baalbaki H, Stevens JW, et al. (2013) Home telemonitoring or structured telephone support programmes after recent discharge in patients with heart failure: systematic review and economic evaluation. Health Technol Assess 17: 1-207.
- Kraai IH, Luttik ML, de Jong RM, Jaarsma T, Hillege HL (2011) Heart failure patients monitored with telemedicine: patient satisfaction, a review of the literature. J Card Fail 17: 684-90.
- Dendale P, De Keulenaer G, Troisfontaines P, Weytjens C, Mullens W, et al. (2012) Effect of a telemonitoring-facilitated collaboration between general practitioner and heart failure clinic on mortality and rehospitalization rates in severe heart failure: the TEMA-HF 1 (TElemonitoring in the MAnagement of Heart Failure) study. Eur J Heart Fail 14: 333-340.
- Di Lenarda A, Caloso G, Gulizia MM, Aspromonte N, Scalvini S, et al. (2015) The future of telemedicine for the management of heart failure patients: a Consensus Document of the Italian Association of Hospital Cardiologists (A.N.M.C.O), the Italian Society of Cardiology (S.I.C.) and the Italian Society for Telemedicine and eHealth (Digital S.I.T.) Health Inform Res 21: 223-229.
- https://www.thecochranelibrary.com/userfiles/ccoch/file/Telemedicine/CD007228.pdf
- Willemse E, Adriaenssens J, Dilles T, Remmen R (2014) Do telemonitoring projects of heart failure fit the chronic care model? Int J Integr Care 14: e023.
- Inglis SC, Clark RA, McAlister FA, Ball J, Lewinter C, et al. (2010) Structured telephone support or telemonitoring programmes. Cochrane Database Syst Rev 8: CD007228.
- Chaudhry SI, Mattera JA, Curtis JP, Spertus JA, Herrin J, et al. (2010) Telemonitoring in patients with heart failure. N Engl J Med 363: 2301-2309.
- Koehler F, Winkler S, Schieber M, Sechtem U, Stangl K, et al. (2011) Impact of remote telemedical management on mortality and hospitalizations in ambulatory patients with chronic heart failure: the telemedical interventional monitoring in heart failure study. Circulation 123: 1873-1880.
- Kitsiou S, Paré G, Jaana M (2013) Systematic reviews and meta-analyses of home telemonitoring interventions for patients with chronic diseases: a critical assessment of their methodological quality. J Med Internet Res 15: e150.
- Andrès E, Talha S, Hajjam M, Hajjam J, Ervé S, et al. (2015) E-care project: a promising e-plateform for the optimizing management of chronic heart failure and other chronic diseases. Heart Res Open J 1: 39-45.
- Scalvini S, Capomolla S, Zanelli E, Benigno M, Domenighini D, et al. (2005) Effect of home-based telecardiology on chronic heart failure: costs and outcomes. J Telemed Telecare 11: 16-18.
- https://www.legifrance.gouv.fr/eli/arrete/2017/4/25/AFSH1711560A/jo/texte/fr
- Kaladjurdjevic M, Antonicelli R (2016) Evaluation of motivation and attitude for Telehomecare among caregivers of elderly patients affected with congestive heart failure. Digital Medicine 2: 149-156.
- https://www.telesante-basse-normandie.fr/l-enrs-et-les-projets/scad,1642,1346.html
- https://www.pimps.fr/
- https://www.osicat.fr/
- https://www.groupe.reunica.com/files/live/sites/reucorp/files/VousInformer/EspacePresse/Dossiers/DossierdepresseReunicaDomicileDispositifdetelemedecineadomicilepourinsuffisancecardiaquechronique.pdf
- Andrès E, Talha S, Ahmed Benyahia A, Keller O, Hajjam M, et al. (2016) Expérimentation d'une plateforme de détection automatisée des situations à risque de décompensation cardiaque (plateforme E-care) dans une unité de Médecine Interne. Rev Med Interne 37: 587-593.
- Andrès E, Talha S, Benyahia AA, Keller O, Hajjam M, et al. (2015) e-Health : a promising solution for the optimized management of chronic diseases. Example of a national e-Health project E-care based on a e-plateform in the context of chronic heart failure. European Research in Telemedicine/La Recherche Européenne en Télémédecine 4: 87-94.
- Ahmed Benyahia A, Hajjam A, Talha S, Hajjam M, Andrès E, et al. (2014) E-care : évolution ontologique et amélioration des connaissances pour le suivi des insuffisants cardiaques. Med Ther 20: 79-86.
- Andrès E, Talha S, Hajjam M, Hajjam J, Ervé S, et al. (2018) Experimentation of 2.0 telemedicine in elderly patients with chronic heart failure: a study prospective in 175 patients. Eur J Intern Med. S0953-6205: 30082-30087.
- Mortazavi BJ, Downing NS, Bucholz EM, Dharmarajan K, Manhapra A, et al. Analysis of Machine Learning Techniques for Heart Failure Readmissions. Circ Cardiovasc Qual Outcomes 2016;9:629-40.
- https://www.lesechos.fr/pme-regions/innovateurs/030831110105-plasidia-la-plate-forme-de-telemedecine-personnalisee-pour-les-diabetiques-2128914.php#GfMgmMDeCZSb5mUC.99
- https://www.predimed-technology.fr/
- Charpentier G, Benhamou PY, Dardari D, Clergeot A, Franc S, et al. (2011) The Diabeo software enabling individualized insulin dose adjustments combined with telemedicine support improves HbA1c in poorly controlled type 1 diabetic patients: a 6-month, randomized, open-label, parallel-group, multicenter trial (TeleDiab 1 Study). Diabetes Care 34: 533-9.
- Antoniades NC, Rochford PD, Pretto JJ, Pierce RJ, Gogler J, et al. (2012) Pilot study of remote telemonitoring in COPD. Telemed J E Health 18: 634-40.
- Vitacca M, Montini A, Comini L (2018) How will telemedicine change clinical practice in chronic obstructive pulmonary disease? Ther Adv Respir Dis 12: 1753465818754778.
- Alcazar B, de Lucas P, Soriano JB, Fernández-Nistal A, Fuster A, et al. (2016) The evaluation of a remote support program on quality of life and evolution of disease in COPD patients with frequent exacerbations. BMC Pulm Med 16: 140.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences