Sniffing Position: Is it Just a Gas?
Department of Anaesthesiology and Critical Care, Tata Medical Center, Kolkata, West Bengal, India
- Corresponding Author:
- Arunangshu Chakraborty
Consultant, Department of Anaesthesiology and Critical care, Tata Medical Center
14 MAR (EW) Newtown, Kolkata-700156, India
Tel: 03366057219, 9007733776
E-mail: arunangshu.chakraborty@tmckolkata.com
Received date: August 25, 2018; Accepted date: October 4, 2018; Published date: October 12, 2018
Citation: Chakraborty A (2018) Sniffing position: Is it Just a Gas? J Anaesthesiol Crit Care. Vol 1 No.3:12
Copyright: © 2018 Chakraborty A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Abstract
Optimal positioning of the head and neck is crucial for a favourable laryngeal visualization. Sniffing Position (SP) is known to provide good visualization of the glottis during direct laryngoscopy, facilitating intubation. Various studies have however, challenged the superiority of sniffing position. We did a literature search and reviewed various studies comparing the sniffing position with simple head extension to study the glottic view and difficulty in intubation during direct laryngoscopy. Several factors such as ease of bag mask ventilation, intubation difficulty, laryngoscopic views and posture of the anaesthesiologist during laryngoscopy and tracheal intubation were noted in the reviewed studies. Most of the studies noted that simple head extension needed more lifting force, increased use of External Laryngeal Manipulation (ELM), and an increased use of alternate techniques during intubation when compared to the sniffing position. Based on the review of available literature we concluded that compared to head extension only position, the sniffing position should be used as a standard head position for intubation attempts under general anaesthesia.
Keywords
Tracheal intubation; Sniffing position; General anaesthesia
Introduction
Good alignment of the airway that comes out of optimal positioning of the head and neck is essential for an adequate laryngeal view during direct laryngoscopy. The major determinant of easy tracheal intubation is the ability to have an optimum visualization of the glottis and the ability to pass a tracheal tube easily.
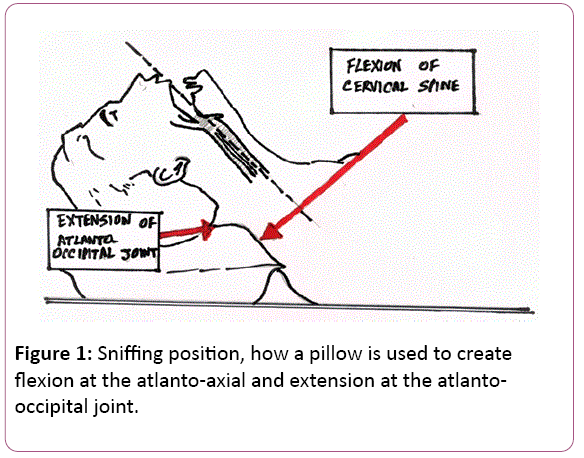
The combination of flexion at the atlanto-axial joint and extension at the atlanto-occipital joint is also known as the Sniffing Position (SP). It is traditionally recommended for induction of general anaesthesia unless contraindicated. SP is known to provide better laryngeal view during direct laryngoscopy than Simple Head Extension (SHE) or a neutral head position more, so in obese persons [1,2]. Added to the various advantages in direct laryngoscopy, SP also helps to maintain the patency of the airway during induction of general anaesthesia, facilitating good bag-and-mask ventilation. This is of special importance in obese patients with Obstructive Sleep Apnea (OSA) who have narrow pharyngeal airways and may develop hypoxia rapidly without proper mask ventilation due to reduced Functional Residual Capacity (FRC) [3,4]. Knowledge of influences of SP on pharyngeal airway patency in anaesthetized and paralyzed persons is vital, but generally lacking [5].
Review of Literature
Ivan Magill, in 1936, suggested that the sniffing position is the best position for laryngeal exposure [6]. Bannister and Macbeth recommended the Three Axes Alignment Theory (TAAT) highlighting that SP causes alignment of the laryngeal, pharyngeal and oral axises causing line of vision to fall on the glottis [7]. Horton et al. proposed the concept of angle for neck flexion as 35° and the plane of face extension with the horizontal at 15° [8]. Other possible alternatives to TAAT were put forward by Chou and Wu [9] and Isono [10]. Chou and Wu [9] pointed out that the airway is a three-dimensional space. They noted that in most patients with slight head extension, the tongue could be displaced easily and laryngeal exposure was good enough. The “Obstacle theory” is the gold standard for laryngoscopy, which highlights that head elevation in SP moves the anterior obstacles upward, head extension moves posterior obstacle downward, and laryngoscopy moves anterior obstacle upward, thus enabling the line of vision to pass through the created space [10].
Adnet et al. could not find any alignment of axis in a radiograph obtained during intubation in the SP, thus challenging SP [11]. However, these findings were criticized subsequently as it was noted that the neck flexion angle in the radiograph was barely 5° [12]. Benumof noticed that the inability by Adnet et al. to observe the alignment may have been a result of failure to position the patients head in a proper SP [12]. This criticism led to further studies by Adnet et al. [11]. They found that the difficulty in intubation, as measured by the Intubation Difficulty Scale (IDS) was similar between the patients in SP and SHE [13]. However, laryngoscopy in these patients was done without administering a muscle relaxant. This could have led to suboptimal conditions for laryngoscopy. Most of the studies [14-16] have studied the Cormack-Lehane grading or percentage of glottic opening scoring [17] as a predictor for the ease of intubation. The aim of our review was to evaluate the differences between SP and SHE position, with regard to the difficulty of bag mask ventilation, difficulty in laryngoscopy and difficulty of intubation in adult patients undergoing elective surgery under general anaesthesia with co-administered muscle relaxant.
Neck position changes from the neutral position to the SP enlarges both retroglossal and retropalatal airways. The size of the pharyngeal airway is determined by a precise interaction between neural regulation of the activity of the pharyngeal dilator muscles (e.g. genioglossus) (neural mechanisms) and structural properties of the pharyngeal airway (anatomical mechanisms) [18,19]. The pharyngeal passage is surrounded by soft tissue such as the tongue and soft palate and enclosed by bony structures such as the mandible, maxilla, and cervical vertebrae. Amongst the soft tissue, important role is played by the dilator muscles of pharynx, such as genioglossus and palatal muscles. Various studies have shown that the pharyngeal collapsibility, which is an important factor that dictates whether the pharyngeal airway remains patent or not under conditions such as sleep or sedation, is influenced by both obesity as well as craniofacial structural abnormalities [20] The anatomical balance between the amount of soft tissue within the bony enclosure and the size of the bony enclosure determines the bore of the pharyngeal airway lumen. For example, an obese person with normal shaped bony structures can have reduced pharyngeal passage due to increased amount of soft tissue. On the other hand an otherwise lean person can have reduced airway passage due to abnormal bone structure such as short mandible, inferiorly placed hyoid bone, inferior maxilla etc.
Neuromuscular mechanisms are of central importance in the balance model and contraction of pharyngeal dilator muscles shift the balance to the left, compensating for the anatomical unbalance in the neutral Neck Position (NP) during wakefulness [21]. Muscle paralysis during general anaesthesia eliminates the neural compensatory mechanisms and creates anatomical unbalance and therefore narrows the pharyngeal airway in the neutral neck position [18,21]. The bony enclosure size varies with head and mandible positioning changes even within one subject. Thus optimization of airway can be effected by modification of the head position. Although the alterations in arrangement of bony structures surrounding the pharyngeal airway is not evaluated often, an increase in the distance between cervical column and mentum can result from extension of the atlanto-occipital joint with bite closure in the SP, consequently leading to an increased bony enclosure size. Adnet et al. [22] conducted an MRI study to demonstrate this effect. Thus, SP improves bony enclosure size and improves the anatomical balance, resulting in the increase of pharyngeal airway size.
It was found that the SP influences airway collapsibility at both retroglossal and retropalatal segments. The tongue musculature, namely genioglossus, originates from and is enclosed by the mandible. Therefore, tilting the mandible increases the retroglossal space. On the other hand, soft tissue at the level of the retropalatal airway is not bound by the mandible, and there is no direct structural connection between the soft tissue and mandible, implying less or no influence of the SP on the retropalatal airway patency however, this position enables the mechanical load relief of the tongue soft tissue from the soft palate, which may be a probable explanation for the retropalatal airway patency improvement [23].
Mechanical influences of the SP differed slightly from those of simple neck extension, whereas both neck positions increased A max and decreased P close to approximately the same extent [23]. Increased longitudinal force along the airway, probably due to airway lengthening during simple neck extension [22,23] may be counterbalanced by the flexion of atlanto-axial joint in the SP (Figure 1).
A review of earlier studies showed that the more patients had easier intubations in SP as compared to simple head extension. The position used by the anaesthesiologists was upright in most instances when the patients were intubated in SP than the SHE group. Studies have shown that a significant number of patients intubated by head extension only needed more than one attempt at intubation, use of External Laryngeal Manipulation (ELM) and alternate techniques, and use of greater force during direct laryngoscopy compared to those intubated in the SP. Hence, it was easier to intubate in the SP than after simple head extension. The results observed by Levitan et al. [24] showed that glottic opening scores measured between 31% in the head flat and 64% in mid-elevation to 87% with maximal elevation positions. Park et al. [25] compared the glottic views after laryngoscopy in the neutral position and with different pillows heights of 3, 6 and 9 cm in adult patients. The view after laryngoscopy was best with 9 cm elevated pillow and it further improved with the addition of pillows in short-necked patients. They found a notable correlation between the neck length and the height of the pillow needed to provide optimal view.
In a study conducted by Brindley et al. [26] “win with the chin” analogy resulted in optimal airway positioning in novices being trained for airway management. In a study done by Johnson and Goodman, [27] many variabilities were seen by the anaesthesiologists in mimicking SP; hence, there is a need to standardize the SP. This lack of standardization may lead to the points observed by Adnet et al. [1]. That sniffing position did not really facilitate better glottic visualization and easier intubation.
Singhal et al. [15] and Sahay et al. [17] did studies similar to each other comparing the IDS scores between the SP and simple head extension. For muscle relaxation Singhal et al. [15] used suxamethonium in a dose of 1.5 mg/kg while Sahay et al. [17] used vecuronium. Studies showing similar results to Singhal et al. [15] with better glottis visualization and lower intubation difficulty scores to facilitate tracheal intubation with the use of atracurium (0.5 mg/kg) were done as well [28]. This study also showed reduced lifting force on the laryngoscope when the patients were intubated in SP than the simple head extension group.
Recent studies by Greenland et al. [29] based on MRI of the airway proposed the two-curve theory-a primary oropharyngeal curve and secondary pharyngo-glotto-tracheal curve instead of three axes alignment theory. The authors have shown the superiority of SP on the basis of MRI study done in extension neutral, head left, and SP in adult volunteers [29]. A reduction in the area between the line of sight and the airway curve in the SP as compared with the neutral position was seen. SP may not result in complete axis alignment, however, it brings the axis as close as possible in preparation for complete alignment to be achieved during laryngoscopy [30].
Conclusion
Direct laryngoscopy is a dynamic procedure, and multiple manipulations are needed to improve the glottic view. Many factors such as size and type of the blade, laryngoscopic lifting force, experience of the anaesthesiologist, and patient airway anatomy influence the degree of glottis exposure and need to be individualized to avoid the bias arising from these factors. SP improves maintenance of the passive pharyngeal airway at both retropalatal and retroglossal segments in patients may be beneficial for both bag mask ventilation and tracheal intubation during induction of anaesthesia. The available literature on this topic shows that SP is better for optimal laryngeal exposure and ease of intubation. Thus we conclude that the sniffing position should be used as a standard head position for intubation attempts under general anaesthesia till definitive alternate results are available from larger multicentric trials.
References
- Adnet F, Baillard C, Borron SW, Denantes C, Lefebvre L, et al. (2001) Randomized study comparing the “sniffing position” with simple head extension for laryngoscopic view in elective surgery patients. Anesthesiol 95: 836-41.
- Cormack RS, Lehane J (1984) Difficult tracheal intubation in obstetrics. Anaesth 39: 1105-11.
- Isono S, Remmers JE, Tanaka A, Sho Y, Sato J, et al. (1997) Anatomy of pharynx in patients with obstructive sleep apnea and in normal subjects. J Appl Physiol 82: 1319-26.
- Langeron O, Masso E, Huraux C, Guggiari M, Bianchi A, et al. (2000) Prediction of difficult mask ventilation. Anesthesiol 92: 1229-36.
- Shorten GD, Armstrong DC, Roy WI, Brown L (1995) Assessment of the effect of head and neck position on upper airway anatomy in sedated paediatric patients using magnetic resonance imaging. Paediatr Anaesth 5: 243-8.
- Magill IW (1936) Endotracheal anesthesia. Am J Surg 34: 450-5.
- Bannister FB, Macbeth RG (1944) Direct laryngoscopy & tracheal intubation. Lancet 2: 651-4.
- Horton WA, Fahy L, Charters P (1989) Defining a standard intubating position using “angle finder”. Br J Anaesth 62: 6-12.
- Chou HC, Wu TL (2002)A reconsideration of three axes alignment theory and sniffing position. Anesthesiol 97: 753-4.
- Isono S (2001) Common practice and concepts in anesthesia: Time for reassessment: Is the sniffing position a “gold standard” for laryngoscopy? Anesthesiol 95: 825-7.
- Adnet F, Borron SW, Lapostolle F, Lapandry C (1999) The three axis alignment theory and the “sniffing position”: Perpetuation of an anatomic myth? Anesthesiol 91: 1964-5.
- Benumof JL (2000) Patient in “sniffing position” Anesthesiol 93: 1365-6.
- Adnet F, Baillard C, Borron SW, Denantes C, Lefebvre L, et al. (2001) Randomized study comparing the “sniffing position” with simple head extension for laryngoscopic view in elective surgery patients. Anesthesiol 95: 836-41.
- Ambardekar M, Pandya S, Ahuja P (2008) Comparison of the sniffing position with simple head extension for laryngoscopic view in elective surgical patients. Internet J Anesthesiol 17: 15.
- Singhal SK, Malhotra N, Sharma S (2008) Comparison of sniffing position and simple head extension for visualization of glottis during direct laryngoscopy. Indian J Anaesth 52: 546-50.
- Bhattarai B, Shrestha SK, Kandel S (2011) Comparison of sniffing position and simple head extension for visualization of glottis during direct laryngoscopy. Kathmandu Univ Med J 9: 58-63.
- Sahay N, Samaddar DP, Chatterjee A, Sahay A, Kant S, et al. (2016) Sniff to see. Comparing sniffing position versus simple head extension position for glottic exposure-A prospective, randomized cross over study. J Health Spec 4: 212-8.
- Isono S, Remmers JE, Tanaka A, Sho Y, Sato J, et al. (1997) Anatomy of pharynx in patients with obstructive sleep apnea and in normal subjects. J Appl Physiol 82: 1319-26.
- Kuna S, Remmers JE (2000) Anatomy and physiology of upper airway obstruction: principles and practice of sleep medicine, 3rd edition. Kryger MH, Roth T, Dement WC. Philadelphia, WB Saunders (Eds), pp: 840-58.
- Watanabe T, Isono S, Tanaka A, Tanzawa H, Nishino T (2002) Contribution of body habitus and craniofacial characteristics to segmental closing pressures of the passive pharynx in patients with sleep disordered breathing. Am J Crit Care Med 165: 260-5.
- Mezzanotte WS, Tangel DJ, White DP (1992) Waking genioglossal electromyogram in sleep apnea patients versus normal controls: A neuromuscular compensatory mechanism. J Clin Invest 89: 1571-9.
- Adnet F, Borron SW, Dumas JL, Lapostolle F, Cupa M, et al. (2001) Study of the “sniffing position” by magnetic resonance imaging. Anesthesiol 94: 83-6.
- Isono S, Tanaka A, Tagaito Y, Ishikawa T, Nishino T (2004) Influences of head positions and bite opening on collapsibility of the passive pharynx. J Appl Physiol 97: 339-46.
- Levitan RM, Mechem CC, Ochroch EA, Shofer FS, Hollander JE (2003) Head-elevated laryngoscopy position: Improving laryngeal exposure during laryngoscopy by increasing head elevation. Ann Emerg Med 41: 322-30.
- Park SH, Park HP, Jeon YT, Hwang JW, Kim JH, et al. (2010) A comparison of direct laryngoscopic views depending on pillow height. J Anesth 24: 526-30.
- Brindley PG, Simmonds MR, Needham CJ, Simmonds KA (2010) Teaching airway management to novices: A simulator manikin study comparing the “sniffing position” and “win with the chin” analogies. Br J Anaesth 104: 496-500.
- Johnson C, Goodman NW (2006) Time to stop sniffing the air: Snapshot survey. BMJ 333: 1295-6.
- Akhtar M, Ali Z, Hassan N, Mehdi S, Wani GM, et al. (2017) A randomized study comparing the sniffing position with simple head extension for glottis visualization and difficulty in intubation during direct laryngoscopy. Anesth Essays Res 11: 762-66.
- Greenland KB, Edwards MJ, Hutton NJ, Challis VJ, Irwin MG, et al. (2010) Changes in airway configuration with different head and neck positions using magnetic resonance imaging of normal airways: A new concept with possible clinical applications. Br J Anaesth 105: 683-90.
- Candido KD, Ghaleb AH, Saatee S, Khorasani A (2001) Reevaluating the “cornerstone of training in anesthesiology” Anesthesiol 95: 1043-4.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences