ISSN : 2348-9502
American Journal of Ethnomedicine
Rare Case of Pyoderma Gangrenosum with Oral Involvement and Hepatitis
1Department of Internal Medicine, Allama Iqbal Medical College, Lahore, Pakistan
2Department of Internal Medicine, Rawal Institute of Health Sciences, Islamabad, Pakistan
3Department of Internal Medicine, King Edward Medical University, Lahore, Pakistan
4Department of Internal Medicine, Ameer-ud-Din Medical College, Lahore, Pakistan
5Department of Internal Medicine, Sinai Grace-Detroit Medical Center, Detroit, USA
- *Corresponding Author:
- Chaudhry Saad Sohail
Department of Internal Medicine
Allama Iqbal Medical College, Lahore, Pakistan
Tel: 13472488134
E-mail: chsaad105@yahoo.com
Received Date: September 27, 2018; Accepted Date: October 18, 2018; Published Date: October 22, 2018
Citation: Chaudhry SS, Inayat UA, Muhammad AZ, Naurez Q, Ali NK, et al. (2018) Rare Case of Pyoderma Gangrenosum with Oral Involvement and Hepatitis. Am J Ethnomed Vol.5 No.2:11
DOI: 10.21767/2348-9502.100011
Abstract
Pyoderma Gangrenosum is an autoimmune disease which is associated with number of other systemic diseases mainly ulcerative colitis, crohn’s disease, rheumatoid arthritis and few others. But the rare associations are PG with oral involvement and PG with liver abnormalities. Uniqueness of this case is that, it has both of these rare characteristics. A 20 year old patient presents with the diffuse involvement of skin ulceration along with the oral ulcers too. He was diagnosed on the basis of the ulcer’s biopsy report and all other associations were denied appropriately with the help of colonoscopy, endoscopy and Extractable Antigen Nuclear Profile. So, initially he was started on prednisone and he responded well but then he started to develop the Iatrogenic Cushing Syndrome so then his medication was changed to the cyclosporine. Later on, his Hepatitis-C, ELISA came to be positive, so then his medication for that was started too.
Keywords
Pyoderma gangrenosum (PG); Inflammatory bowel disease (IBD)
Introduction
Pyoderma Gangrenosum is a painful ulcerative disease which is just not only the dermatological complication of different diseases but it is itself an independent disease [1]. It may be related to IBD, arthritis, hematologic milagnancies and a few cases are also reported to be as a side effect of medication [2]. It is diagnosed clinically and through the biopsy. But the negative result on biopsy does not rule out the disease [3]. PG is also more commonly present in the women [4]. There are also typical and atypical forms of PG. Typical PG has mainly ulcers on the lower extremity and is more frequently associated with IBD as compares to atypical PG which is more on upper extremity and more frequently associated with hematological malignancy. For the treatment, corticosteroids and immunosuppressants are used mainly and for some cases monoclonal antibodies give the best result [5]. We are presenting this case because of the rare association of PG with hepatitis C and oral involvement of the lesions. We ruled out all other possible causes and associations. This is the unique case of PG with dual associations of its rarity.
Case Report
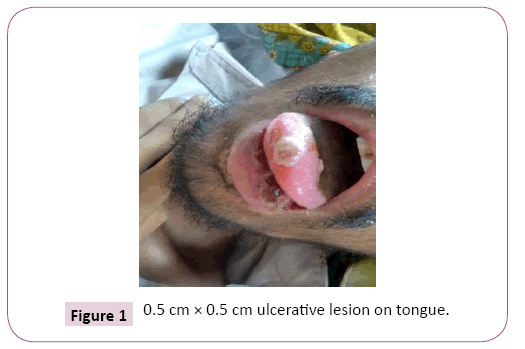
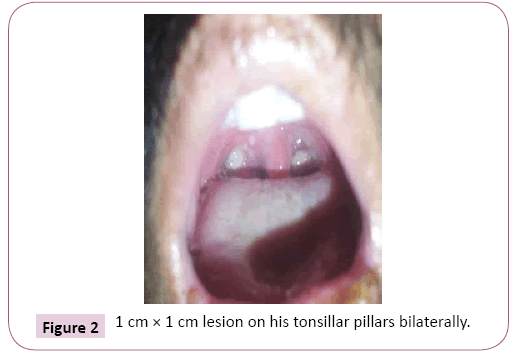
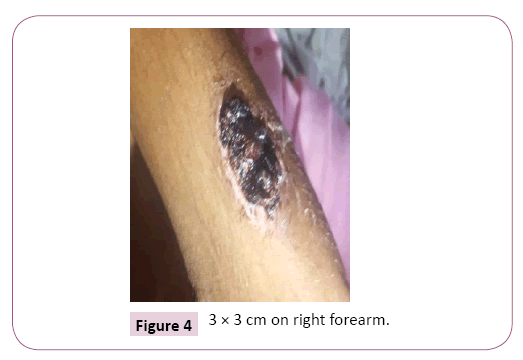
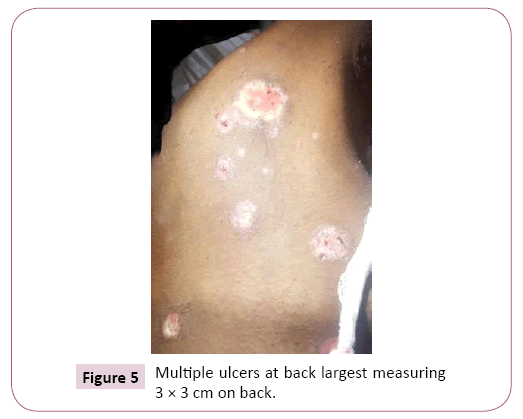
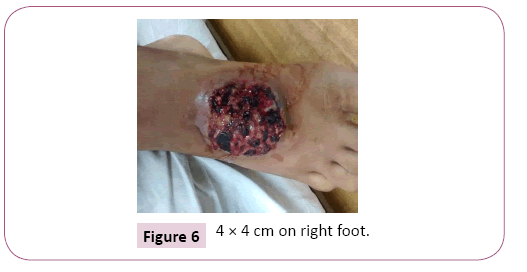
A 20 years old male reported in medical emergency of community hospital with high grade persistent fevers for one month duration with no associated rigors or chills. Fever was preceded by flu like illness and sore throat for one week. Patient also reported having diffuse skin lesions including his oral cavity that initially appeared as painful nodules that had progressed to ulcerative lesion by the time patient presented hospital. On initial presentation, patient had a fever of 102.6 degree Fahrenheit. Blood pressure was 110/67 with a heart rate of 110. On physical examination, patient was found to have a 0.5 cm × 0.5 cm ulcerative lesion on his tongue (Figure 1), 1 cm × 1 cm lesion on his tonsillar pillars bilaterally (Figure 2), large 3 × 3 cm lesion on dorsum of left hand (Figure 3), 3 × 3 cm on right forearm (Figure 4), multiple ulcers at back largest measuring 3 × 3 cm at back (Figure 5), 2 × 2 cm lesion on dorsum of scrotum, 4 × 4 cm on right foot (Figure 6). Surrounding area of ulcers was red and inflamed. Patient also had two swollen lymph nodes in the anterior cervical region that were mobile and tender on palpation. No other lymphadenopathy was noted. Rest of the physical examination was unremarkable. The patient was first treated as case of Diphtheria with skin lesions and was given Eryhtromycin course for 14 days and was discharged home after biopsy of the skin lesions, blood withdrawal for workup and urine sample was taken. A diagnostic punch biopsy was obtained from one of the lesions on left lower extremity. Elliptical biopsy from right foot measuring 0.5 × 0.5 cm is performed.
Investigations included complete blood picture, clotting profile, serum HBsAg and HCV antibody, liver function tests, blood and urine cultures, random blood sugar, urinalysis, rheumatology and Extractable Nuclear Antigen profile. Except Leukocyte count which was raised secondary to infection most probably, everything was normal. Blood reports and Urinalysis of the patients are given in the Tables 1-4. After 14 days patient were returned to ER with treatment failure. At that, we were with all his blood and urine reports and along with the biopsy result. Microscopic Examination of the specimen showed focal ulceration of epidermis with undermined edges, parakeratosis and mild hyperplasia with fusion of rete pegs. The papillary dermis showed swelling and necrosis of connective tissue with infiltration of neutrophils and few lymphocytes and eosinophils along with swollen necrosis blood vessels, multinucleated giant cells with vague granulomas and fibrinous leukocytoclastic vasculitis with extravasation of RBC’s. These features were consistent with pyoderma gangrenosum. So, we make a diagnosis of pyoderma gangrenosum and to rule out different associations, we scheduled him for colonoscopy and endoscopy and start with the appropriate treatment. His endoscopy and colonoscopy were unremarkable.
Table 1: Blood cells reports.
| Hb | 13.7 g/dL |
| RBCs | 4.6 million/mm3 |
| WBCs | 13000/mm3 |
| Platelets | 80-100 µm3 |
| Bilirubin, Total | 0.9 md/dL |
| PT/INR | 13 sec |
| PTT | 35 sec |
| Albumin | 4.3 g/dL |
Table 2: Blood reports.
| Blood Glucose | 109 mg/dL |
| ESR | 17 mm/hr |
| Alkaline Phosphatase | 71 IU/L |
| BUN | 13 mg/dL |
| Creatinine, Serum | 1.1 mg/dL |
| Cholestrol | 150 mg/dL |
| HBsAg | Negative |
| Anti-HCV antibody | Negative |
Table 3: Blood salts reports.
| Sodium | 135 mEq/L |
| Potassium | 4.3 mEq/L |
| Magnesium | 2.1 mEq/L |
| Phosphorus | 3.5 mg/dL |
| Chloride | 104 mEq/L |
| Calcium | 9.6 mg/dL |
| AST | 15 U/L |
| ALT | 19 U/L |
Table 4: Urinalysis.
| Color | Yellow |
| Clarity | Clear |
| pH | 5.2 |
| Glucose | 86 mg/dL |
| Ketones | None |
| Nitrites | Negative |
| Leuckocyte estrase | Negative |
| Blood | No RBCs |
We started prednisone and in about two days he responded to it. We covered the wounds with moist dressing and applied zinc oxide at wound edges. Patient was monitored for any infection and he was suspected to be infected because of his symptoms and wound condition. He was started on Doxycycline and amoxicllin to cover gram positive cocci and MRSA which can infect the wound. We continued the treatment for a month and directed him for follow up after that. After a month period the patient came back for follow up and there were still small lesions left in the areas affected and the patient had symptoms of Iatrogenic Cushing Syndrome so we decided in the best interest of patient to taper off the prednisone and started systemic immunosuppressant (Cyclosporine) as the mainstay of the treatment therapy and was advised to regularly get his kidney function checked. He was advised to take care of his ulcers, avoid any trauma to the skin and come to hospital if he notices his ulcer getting infected. He was given topical antibiotic (polyfax) to apply to his ulcer. We discharged him home after referral to Dermatology. Later on the Dermatology department ordered ELISA for the patient and found to be Hepatitis C positive case. Now the Patient has fully recovered and is on cyclosporine and Hepatitis C treatment.
Discussion
Pyoderma gangrenosum is an uncommon disease which mostly involves skin but can also involve other organs. The exact etiology is unknown but it is believed to be caused by autoimmune dysregulation [6]. PG can occur on its own but in around 50% of cases it is found to have an association with other disorders such as Inflammatory bowel disease, Arthritis, Hematological disorders, PAPA syndrome [7]. It can also be caused as a result of adverse reaction of drugs such as Cocaine, Isotretinoin, Sunitinib and propylthiouracil [8]. Pathogenesis of Pyoderma Gangrenosum remains unclear for the most part but it is mostly characterized as neutrophil-predominant infiltrates in the skin. The role of Neutrophil dysfunction in development of PG has been identified. The response of disease to antineutrophilic agents such as Dapsone also suggests the role of Neutrophil in PG [9,10]. In addition, some studies have also found some genetic predisposition to the development of PG [11,12]. Clinically PG is characterized by an inflammatory papule, pustule, vesicle or nodule that can expand and break into an ulcer which can be painful and can be associated with fever just like the case described [13]. Subtypes of PG include Ulcerative (classic) PG, Bullous (atypical) PG, Pustular PG, Vegetative PG. The most common is Ulcerative type which mostly involves lower extremities and trunk and develops ulcers. In bullous PG, arms and face are involved mostly and patients typically present with the rapid development of blue-gray, inflammatory bullae in the involved areas. Pustular PG is mostly present in inflammatory bowel disease and patients develop painful pustules surrounded by erythema. Vegetative PG presents as an indolent, mildly painful nodule, plaque, or ulcer [14]. Pyoderma Gangrenosum is diagnosed when other possibilities have been excluded but detailed history, Physical examination, Laboratory tests and skin biopsies should be performed in every suspected case which was done in the case described above. At least the major criterion and four minor criteria are necessary for diagnosis and this case fulfills one major and five minor criteria. So, the case described above met the criteria. No single, specific treatment exists. Immunosuppression is the mainstay of treatment, and the most commonly used drugs are corticosteroids and cyclosporine. Treatment is largely empirical and the choice of treatment often depends on local experience. This patient was first treated with corticosteroids and then with cyclosporine and his condition responded to treatment.
Conclusion
The patient we have described had classical lesions of Pyoderma gangrenosum of the hands, wrist legs, feet and trunk which were healed after corticosteroid therapy. There was no evidence of inflammatory bowel disease in this patient or any of the other described disease associations. The lesion on his tongue was consistent with chronic inflammatory lesion with neutrophils, a classical sign of PG. Its occurrence in association with Pyoderma gangrenosum and its very rapid resolution with systemic steroids suggests that it was also a manifestation of this disease. Since, hepatitis C is also positive, so this case is rare for these two reasons.
References
- Ahronowitz I, Harp J, Shinkai K (2012) Etiology and management of pyoderma gangrenosum: a comprehensive review. Am J Clin Dermatol 13: 191-211.
- Trevor B, Giles D, Chris P (2006) Diagnosis and treatment of pyoderma gangrenosum. BMJ 333: 181-184.
- Steuber CP, Culbert SJ, Ravindranath Y, Krischer J, Ragab A, et al. (1990) A Therapy of childhood acute nonlymphocytic leukemia: the Pediatric Oncology Group experience (1977-1988). Haematol Blood Transfus 33: 198-209.
- Binus AM, Qureshi AA, Li VW, Winterfield LS (2011) Pyoderma gangrenosum: a retrospective review of patient characteristics, comorbidities and therapy in 103 patients. Br J Dermatol 165: 1244-50.
- Brooklyn TN, Dunnill MGS, Shetty A, Bowden J, Williams JDL (2018) Infliximab for the treatment of pyoderma gangrenosum: a randomised, double blind, placebo controlled trial Inflammatory bowel disease BMJ 55: 25-65.
- Mark JJ, Jeffrey P (2018) Pyoderma Gangrenosum. Drugs & Diseases, Medscape.
- Eduardo CJ, Thomas B, Alexander JL, Phillip HM (2012) Pathology of the Skin E-Book, (12th edtn), Saunders press, USA.
- Wang JY, French LE, Shear N, Amiri A, Alavi A (2018) Drug-Induced Pyoderma Gangrenosum: A Review. Am J Clin Dermatol 19: 67-77
- Courtney S (2018) Pyoderma gangrenosum: Pathogenesis, clinical features, and diagnosis.
- Adachi Y, Kindzelskii AL, Cookingham G, Shaya S, Moore EC, et al. (1998 ) Aberrant neutrophil trafficking and metabolic oscillations in severe pyoderma gangrenosum. J Invest Dermatol 111: 259-68.
- Alberts JH, Sams HH, Miller JL, King LE Jr (2002) Familial ulcerative pyoderma gangrenosum: a report of 2 kindred. Cutis 69: 427-30.
- Khandpur S, Mehta S, Reddy BS (2001) Pyoderma gangrenosum in two siblings: a familial predisposition. Pediatr Dermatol 18: 308-312.
- Ahronowitz I, Harp J (2012) Etiology and management of pyoderma gangrenosum: a comprehensive review. Shinkai K.Am J Clin Dermatol 13: 191-211.
- Maverakis E, Ma C, Shinkai K, Fiorentino D, Callen JP (2018) Diagnostic Criteria of Ulcerative Pyoderma Gangrenosum: A Delphi Consensus of International Experts. JAMA Dermatol 154: 461-466.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences