Malassezia Folliculitis: Prevalence, Clinical Features Risk Factors and Treatment: A Prospective Randomized Comparative Study
Emna Bahlou1*, Masmoudi Abderrahmen1, Frikha Fatma1, Khadija Sellami1, Boudaya Sonia1, Madiha Mseddi1, Mariem Amouri1,Hamida Turki1, Cheikhrouhou Fatma2 and Ali Ayedi2
1Department of Dermatology, Hedi Chaker Hospital, Sfax, Tunisia
2Fungal and Parasitic Molecular Biology Laboratory, Sfax, Tunisia
- Corresponding Author:
- Emna Bahloul
Department of Dermatology
Hedi Chaker Hospital, Sfax, Tunisia
Tel: +21692020209
Fax: 0021674244511
E-mail: emnabahloul86@gmail.com
Received date: May 03, 2018; Accepted date: May 15, 2018; Published date: May 20, 2018
Citation: Bahlou E, Abderrahmen M, Fatma F, Sellami K, Sonia B, et al. (2018) Malassezia Folliculitis: Prevalence, Clinical Features Risk Factors and Treatment: A Prospective Randomized Comparative Study. J Immunol Microbiol Vol.2 No.1:5
Copyright: © 2018 Bahlou E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Malassezia folliculitis (MF) is an opportunistic fungal infection of the sebaceous glands caused by yeasts of the genus Malassezia. The objective: The aim is to review the epidemiological and clinical characteristics of MF focusing particularly on therapeutic features of Itraconazole (ITZ) and Ketoconazole shampoo (KTZ). Methods: We performed a prospective randomized comparative study conducted over a period of 10 months. The diagnosis of MF was suspected clinically and confirmed by mycological examination. Patients were put in turn under KTZ 2 times per week for 2 months, ITZ 200 mg per day for a week, or both. A clinical and mycological assessment was carried out on 15th day, 30th day and 60th day. Results: 41 patients (mean age: 24 years) were included in the study. The ratio of men to women was 0.46. Skin lesions were pustular in all cases, papulopustular in 87% and keloid in 7%. MF was located at the back in 78%, the arm (70.7%), the chest (61%), and associated with acne (61%) dandruff (58%) and pityriasis versicolor (26.8%). Seborrhea was noted in 97% and excessive exercise in 29%. Hair removal and daily shaving were the main precipitating factors incriminated. Only 2 patients were immuno-compromised. The outcome of patients after treatment was assessed in 85.4%. All patients were improved with complete recovery in 45.7% and partial improvement in 54.3%. Mycological sample were performed in 19 patients and it were negative in 10 cases. Patients treated with ITZ alone or with the KTZ had similar results of complete recovery and partial improvement. Our patients treated only with KTZ had more regression cases. Conclusion: The hot and wet climate, excessive sweating and seborrhea are the main predisposing factors for MF. Hair removal and daily shaving may also be precipitating factors. KTZ and ITZ are efficacious in MF treatment.
Keywords
Folliculitis; Malassezia; Causality; Ketoconazole shampoo; Itraconazole
Introduction
Malassezia folliculitis (MF) is an opportunistic fungal infection of the sebaceous glands caused by yeasts of the genus Malassezia. In MF, there is an occlusion of the follicle and a yeast’s replication and hydrolysing of free fatty acids in triglycerides which are responsible for the inflammatory reaction in the follicle [1,2]. This disease, first reported in 1969, was usually described in immuno-compromised patients. Currently, an increasing number of MF in immunocompetent patients is described [3]. Given the paucity of literature on MF and the multitude of differential diagnosis, this condition is likely under-recognized [4]. The aim of the present study is to review the epidemiological and clinical characteristics of MF focusing particularly on therapeutic features of Itraconazole (ITZ) and Ketoconazole shampoo (KTZ).
Method
Patients
We performed a prospective randomized comparative study conducted over a period of 10 months at the Department of Dermatology. We included all patients in whom MF was suspected by clinical examination and then was confirmed by cytological examination and fungal culture. We suspected MF in patients with follicular pustules and papules. The exclusion criteria included antifungal drug allergy, systemic antifungal treatment during the past 3 months, current pregnancy or lactation and liver failure.
Study design
Patients were examined by an expert dermatologist to confirm the signs of infectious folliculitis. Cytological samples were then taken in fungal and parasitic molecular biology laboratory using a scraping method with a scalpel blade. The smear was stained with potassium hydroxide. Subsequently, the cytological samples were microscopically evaluated and then additional samples were taken from pustular lesions and nonlesional regions for fungal culture.
The MF patients were questioned regarding predisposing factors, concomitant and predisposing diseases; drug intake and subjective complaints. The distribution and clinical morphology of the skin lesions were evaluated and clinical photographs were taken before and after treatment. Lesion’s distribution was divided according to 11 areas of the body. Concerning clinical morphology, the skin lesions were divided into papules, pustules and papulopustular and keloid lesions.
Treatment
MF patients were put in turn under KTZ 2 times per week for 2 months, ITZ 200 mg/day for a week or both. Participants were informed of the fact that they are randomly treated and they agree with it. Their clinical and mycological treatment responses were assessed on 15th day, 30th day and 60th day after treatment.
The patients' clinical outcome was assessed using these categories:
• complete recovery (no folliculitis)
• partial improvement (folliculitis with some improvement)
• no improvement or deterioration
Statistical analysis
• The software SPSS for Windows version 20.0 was used for the statistical analysis.
• Chi square tests were used to test the differences in patients' clinical treatment responses.
• Statistical significance was defined as a P value of less than 0.05.
Results
Over a 10 month period, 41 patients were diagnosed with MF and included in the study. The mean age was 24.46 years (range 14-48 years). There were 28 women and 13 men with a sex ratio (M/ W) 0.46. All patients were living in the south of Tunisia.
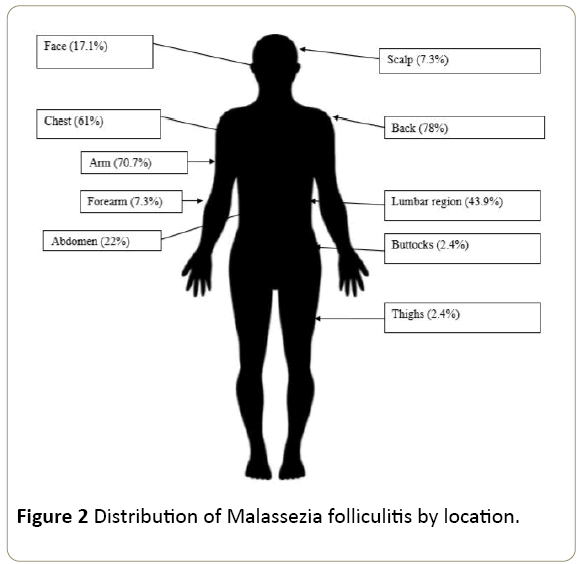
Skin lesions were pustular in all cases, papulopustular in 36cases (87.8%) and keloid in 3 cases (Figure 1). Several locations have been identified (Figure 2). In most cases (82.9%), the lesions were found in more than one region. MF were located at the back in 32 cases (78%), the arm in 29 cases (70.7%), the chest in 25 cases (61%), the lumbar region in 18 cases (43.9%), the abdomen in 9 cases (22%), the face in 7 cases (17.1%), scalp and forearm each in 3 cases (7.3%) and thighs and buttocks each in one case (2.4%). Thirty-five patients (85.4%) complained of pruritus.
MF was associated with acne in 25 cases (61%), dandruff in 24 cases (58.8%) a Pityriasis versicolor in 11 cases (26.8%) and seborrhoeic dermatitis in 2 cases (4.9%). The majority of the patients (40 cases 97.6%) had seborrhea and sweating was classified level 1 and 2 in 34 cases (82.9%) according to HDSS. Twelve patients (29.3%) were involved in excessive exercise.
Many precipitating factors were incriminated. We noted hair removal in 8 cases (19.5%) and daily shaving (1 case). Five patients (12.2%) worked in hot and wet working environment and two (4.9%) wear frequently occlusive clothing.
Two of our patients were immuno-compromised: one patient was kidney transplanted taken oral corticosteroids and immunosuppressant drugs and one other patient had keratitis and was taken oral corticosteroids. Table 1 summarizes the various factors associated with the MF in our patients.
| Associated factors | Patient’s number and percentage |
|---|---|
| Acne | 25 cases (61%) |
| Dandruff | 24 cases (58.8%) |
| Pityriasis versicolor | 11 cases (26.8%) |
| Seborrhoeic dermatitis | 2 cases (4.9%) |
| Hyperseborrhea | 40 cases (97.6%) |
| Sweating classified level 3 and 4 ( HDSS) | 7 cases (17.1%) |
| Sports | 12 cases (29.3%) |
| Hair removal | 8 cases (19.5%) |
| Daily shaving | 1 case (2.4) |
| Hot and wet working environment | 5 cases (12.2%) |
| Occlusive clothing | 2 cases (4.9%) |
| Oral corticosteroids | 2 cases (4.9%) |
| Immunosuppressant drugs | 1 case (2.4%) |
Table 1: Associated factors with Malassezia folliculitis in our patients.
In summary, 14 patients were treated with KTZ 2 times per week for 2 months, 14 patients were treated with ITZ 200 mg/day for a week and 13 patients were treated with KTZ 2 times per week for 2 months associated to ITZ 200 mg/day for a week.
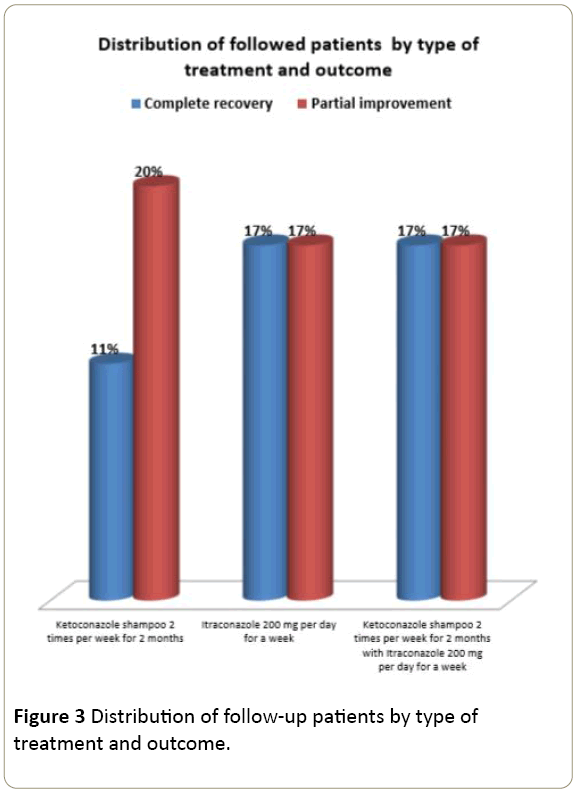
The outcome of patients after treatment was assessed in 35 patients (85.4%). Six patients were lost to follow up. These follow-up patients were treated with ITZ alone in 12 cases, KTZ alone in 11 cases, and the association in 12 cases. The complete recovery was noted on the 60th day in 16 patients (45.7%) and partial improvement was noted in 19 patients (54.3%).
Thirty-three samples were obtained from 19 patients during the study. Fourteen of these examinations were made on the 15th day, nine on the 30th day and ten on the 60th day. The negativity of mycological sample was obtained in 10 cases including three on the 15th day, three on the 30th day and four on the 60th day. MF extended in 7 patients with negative mycological sample.
All follow-up patients had clinical improvement. Patients treated with ITZ alone or with the KTZ had similar results of complete recovery and partial improvement (6 patients). Our patients treated only with KTZ had more cases of partial improvement (7 cases) than complete recovery (4 cases). Chi square test did not reveal significant difference between the patients' clinical outcome and the type of treatment (p>0.05) (Figure 3).
For keloid folliculitis, keloid lesions persist however pustular lesions regressed under KTZ alone (2 cases) and associated with the ITZ (1 case).
Discussion
Although yeasts of the genus Malassezia belong to the normal flora of the skin, in some situations the organisms may cause or aggravate diseases, including pityriasis versicolor, pityrosporum, seborrheic dermatitis and folliculitis [2,5,6]. MF‘s prevalence is estimated at 2.5 to 16% in countries owing to heat and humidity like our region in the south of Tunisia [7,8]. It is demonstrated that higher humidity and sebum levels provide a better environment for Malassezia yeasts in the skin, leading to disruption of the skin barrier [9]. First MF’s cases were almost in patients who are immuno-suppressed due to underlying disorders or therapy such as AIDS patients, transplant patients ,diabetes mellitus, antibiotic therapy, use of corticosteroids and immunosuppressant [10]. Currently, this concept was overcome [3,11]. In our study, only 4.9% were immuno-suppressed patient. Predisposing factors of MF in our patients include primarily seborrhea, excessive sweating and excessive exercise. These factors are comparable with those published in the literature. The hair removal and daily shaving were not already mentioned in previous reports but it can be explicated by skin barrier’s alteration triggering. In the present study, MF is affecting mostly young women. This is similar to the results reported in Turkey by Durdu who described a predominance in females with a sex ratio of 1.72 and average age of 26 years [11]. Clinically, lesions are of the follicular papule-pustular type usually accompanied by intense pruritus [3,7]. keloid folliculitis is rarely described and its physiopathological mechanisms are unknown [12]. Here we insist on the role of Malassezia in keloid folliculitis’ genesis and its possible regression by antifungal therapy. Especially we noted that our patients had no other keloid lesions in other sites.
Similar to previous reports, in our study, MF predominantly involved the trunk, whereas facial, scalp and lower limb involvement rates were relatively low. This distributional discrepancy can be attributed to the differences in the skin environment such as sweating, seborrhea and the distribution of Malassezia species on body region [9,11]. Park et al. [13] reported in their studies that higher humidity and sebum levels provide a better environment for Malassezia yeasts in the skin, leading to disruption of the skin barrier.
The documentation for the treatment of MF is sparse and most published studies include only few patients. Many treatments are used including topical treatment (Selenium Disulphide, Propylene glycol, Miconazole, Ketoconazole and Econazole) and systemic treatment (Itraconazole, Fluconazole and Isotretinoin). Topical antifungal treatment are described as safe and beneficial for MF [14], can be sometimes difficult to use specially for old patient with chronic diseases. In these patients, some authors emphasize on the role of care managers [15]. Systemic antifungal treatment is probably more efficacious than topical treatment, since it eliminates Malassezia located deeply within the hair follicles [16]. The absence of significant correlation between the complete recovery and the type of treatment in our study can be explicated by the limitation of small population and difficulties of following up.
Ketoconazole shampoo is an anti-fungal agent with topic action. It is demonstrated that this topical treatment is efficacious against yeasts of the genus Malassezia. It’s in vivo efficacy was proven in the treatment of seborrhoeic dermatitis as well as Pityriasis versicolor [16]. In MF, few studies were conducted to evaluate KTZ. Immunotherapy with KTZ have response rates of 10-12% in two previous studies done in France and in Saudi Arabia [7,17]. According to the Danish guidelines for the treatment of Malassezia related skin diseases Ketoconazole shampoo is classified grade B (moderately supports a recommendation for use) with IV level of evidence in the treatment of MF [16]. In addition, the safety, the low cost and easy procuration encouraged us to use this treatment in our study. Our results in the treatment of MF with KTZ confirm the conclusions of the previous studies. Systemic Itraconazole treatment was used in the present study because of its favourable in vitro activity against lipophilic Malassezia, its safety, and its high concentration excreted in the sebum. In addition, treatment with Itraconazole 200 mg daily was associated with clinical improvement in 84% in the Indian study of Parsad after one week of treatment [18] and in 91.8% in the Turkish study of Durdu after two weeks of treatment [11]. In our study, one half of the patients treated with ITZ had partial improvement and the other half had complete recovery. As for combined treatment, complete recovery was reported in 100% of MF patients in a randomized study that combined topical (Ketozole shampoo) and systemic antifungal treatments (Ketozole 200 mg twice daily) [17]. In the present study, combined treatment was used in order to avoid relapses and to assess the efficacy. We demonstrate that the combined treatment ITZ and KTZ gave the same results. The limitations of our study are mainly due to its small sample size and difficulties of following up. Further prospective and large studies are needed to precise the incidence risk factors and therapeutic features of MF.
Conclusion
In summary, Malassezia folliculitis predominates in young women and it is characterized by follicular papulopustular lesions especially located at the back and arm. Hot and wet climate, excessive sweating and seborrhoea are the main predisposing factors. Hair removal and daily shaving may also be precipitating factors. KTZ and ITZ are efficacious in MF treatment. Further prospective and large studies are needed to precise the best treatment of MF.
Conflict of Interest
None.
References
- Triana S,Cock DH, Ohm RA, Danies G, Wösten HAB, et al. (2017) Lipid Metabolic Versatility in Malassezia spp. Yeasts Studied through Metabolic Modeling. Front Microbiol.
- Affes M, Ben Salah S, Makni F, Sellami H, Ayadi A (2009)Molecular identification of Malassezia species isolated from dermatitis affections. Mycoses 52: 251-256.
- Prindaville B, Belazarian L, Levin NA, Wiss K (2018) Pityrosporum folliculitis: A retrospective review of 110 cases. J Am Acad Dermatol 78: 511-514.
- Tsai YC, Wang JY, Wu YH, Wang YJ (2018) Atypical presentations of Malassezia folliculitis: a retrospective analysis of 94 biopsy-proven cases. Int J Dermatol 57: 19-20.
- Prohic A, Sadikovic TJ, Krupalija FM, Kuskunovic VS (2015) Malassezia species in healthy skin and in dermatological conditions. Int J Dermatol 55: 494-504.
- Gaitanis G, Magiatis P, Hantschke M, Bassukas ID, Velegraki A (2012) The Malassezia genus in skin and systemic diseases. Clin Microbiol Rev 25: 106-141.
- Lévy A, Feuilhade de Chauvin M, Dubertret L, Morel P, Flageul B (2007) Malassezia folliculitis: Characteristics and therapeutic response in 26 patients. Ann Dermatol Venereol 134: 823-828.
- Masmoudi A, Ben Salah H, Makni F, Chikrouhou F, Boudaya S, et al. (2010) Malassezia folliculitis: 21 cases. Ann Dermatol Venereol 137: 305-306.
- Kim SY, Lee YW, Choe YB, Ahn KJ (2015) Progress in Malassezia research in Korea. Ann Dermatol 27: 647-657.
- Weary PE, Russell CM, Butler HK, Hsu YT (1969) Acneform eruption resulting from antibiotic administration. Arch Dermatol 100: 179-183.
- Durdu M, Güran M, Ilkit M (2013) Epidemiological characteristics of Malassezia folliculitis and use of the May-Grünwald-Giemsa stain to diagnose the infection. Diagn Microbiol Infect Dis 76: 450-457.
- Bonkevitch F, Souza PRM (2014) Nape keloid folicullitis and pruritus. Med Hypotheses 82: 502.
- Park HJ, Lee YW, Choe YB, Ahn KJ (2012) Skin characteristics in patients with pityriasis versicolor using non-invasive method, MPA5. Ann Dermatol 24: 444-452.
- Suzuki C, Hase M, Shimoyama H, Sei Y (2016) Treatment outcomes for Malassezia folliculitis in the Dermatology Department of a University Hospital in Japan. Med Mycol 57: 63-66.
- Ciccone MM, Aquilino A, Cortese F, Scicchitano P, Sassara M, et al. (2010) Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo). Vasc Health Risk Manag 6: 297-305.
- Hald M, Arendrup MC, Svejgaard EL, Lindskov R, Foged EK, et al. (2015) Evidence-based Danish guidelines for the treatment of Malassezia-related skin diseases. Acta Derm Venereol 95: 12–19.
- Abdel-Razek M, Fadaly G, Abdel-Raheim M, al-Morsy F (1995) Pityrosporum (Malassezia) folliculitis in Saudi Arabia - Diagnosis and therapeutic trials. Clin Exp Dermatol 20: 406-409.
- Parsad D, Saini R, Negi KS (1998) Short-term treatment of pityrosporum folliculitis: a double blind placebo-controlled study. J Eur Acad Dermatol Venereol JEADV 11: 188-190.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences