FROM SURGICAL TO CONSERVATIVE- HAS THE COVID PANDEMIC REVERSED OUR STANDOFF TO ORTHOPAEDICS
D.K.Jha( M.S)1* and Dr. Suuhasish Ray(M.Ch)2
1(M.S Orthopaedic surgery)- Professor and Head of the Department- Department of Orthopaedic surgery, Ramakrishna mission seva pratishthan and Vivekananda institute of medical sciences, Sishumangal hospital, Sarat Bose Road, Kolkata, India.
2(M.Ch- ORTHOPAEDICS M.Sc Diploma in Orthopaedics Spine Fellow- SRS,USA Cert. In Orthopaedic Oncology Cert. In Orthopaedic Rheumatology)Consultant Orthopaedic And Spine Surgeon- Department Of Orthopaedic Surgery Ramakrishna Mission Seva Pratishthan and Vivekananda institute of medical sciences, Sishumangal hospital, Sarat Bose Road, Kolkata, India.
*Corresponding author: Dr. Suuhasish Ray Professor and Head of the Department- Department of Orthopaedic surgery, Ramakrishna mission seva pratishthan and Vivekananda institute of medical sciences, Sishumangal hospital, Sarat Bose Road, Kolkata, India, E-mail:suhasishray@gmail.com.
Received date: November 21, 2020 ; Accepted date: August 13, 2021; Published date: August 24, 2021
Citation: Prof. D.K.Jha(M.S) (2021) From Surgical To Conservative- Has The Covid Pandemic Reversed Our Standoff To Orthopaedics J Orthop Disord Vol.1 No.1.
Abstract
COVID- 19 pandemic has brought the need to revisit the conservative management of orthopaedic injuries back into sharp focus. Over the years as trauma and orthopaedics have evolved, operatives techniques have been developed, along with refinement of implants and instruments with an aim of transforming contemporary treatment of fractures to provide anatomical or near anatomical alignment of the fractures, stable fixation, with early pain free range of motion and rehabilitation. [1]. The current Coronavirus outbreak has refocussed orthopaedic minds on managing many injuries conservatively, which would have otherwise been managed with operative fixations. It is mainly because of the restraints put on by this viral infection, limited availability of resources including personnel and operating theatre slots (whilst they were redirected to manage urgent clinical priorities including respiratory emergencies due to COVID- 19 infections on the frontline) and due to reluctance of undertaking operative intervention in an atmosphere of increased risk of viral transmission, responsibility of protecting staff and ‘social distancing’ guidelines [2].
INTRODUCTION
COVID- 19 pandemic has brought the need to revisit the conservative management of orthopaedic injuries back into sharp focus. Over the years as trauma and orthopaedics have evolved, operatives techniques have been developed, along with refinement of implants and instruments with an aim of transforming contemporary treatment of fractures to provide anatomical or near anatomical alignment of the fractures, stable fixation, with early pain free range of motion and rehabilitation.[1]. The current Coronavirus outbreak has refocussed orthopaedic minds on managing many injuries conservatively, which would have otherwise been managed with operative fixations. It is mainly because of the restraints put on by this viral infection, limited availability of resources including personnel and operating theatre slots (whilst they were redirected to manage urgent clinical priorities including respiratory emergencies due to COVID- 19 infections on the frontline) and due to reluctance of undertaking operative intervention in an atmosphere of increased risk of viral transmission, responsibility of protecting staff and ‘social distancing’ guidelines [2]. Traditional conservative treatment of fractures is based on three basic principles of fracture management; namely, reduction of fracture, holding the fracture reduced and keeping it reduced in a supported environment (such as a cast or splint) till the fracture heals. “Closed treatment of fractures” was very elaborately and scientifically described by Sir John Charnley is his monograph in 1950.[3]. The current pandemic situation has exposed us to the situation faced by Sir Robert Jones in the midst of chaos of World War- I, with limitations posed by the shortage of resources both personnel and equipment but the need to manage orthopaedic injuries in a safe manner whilst protecting patients including staff. Surgical specialties face unique challenges caused by COVID- 19[4]. For many urgent surgical procedures, additional steps are required to protect both patients and healthcare workers from the virus.5–7Articular and peri- articular fractures may provide a challenge, since principles of fracture fixation (anatomical reduction, rigid fixation, early range of joint motion) and avoidance of posttraumatic arthritis are not possible with conservative management in most of these injuries and hence operative measurements would be required at a later date.
Table 1: Suggested Indications and Contraindications for conservative management of Paediatric fractures and dislocations, during COVID-19 Pandemic.
| Limb injuries in Children Preferred indications and Adolescents | Equivocal indications | Contraindications | |
|---|---|---|---|
| Upper Limb trauma | Clavicle fractures | Displaced fractures e.g., Supracondylar humerus, lateral condyle humerus, neck radius, distal radius and fractures radius and ulna. | Un reduced dislocations |
| Proximal humerus fractures | Fracture-dislocations | Compartment syndrome | |
| Shaft humerus fractures with angulation of less than 45 | Dislocations | Fractures with vascular deficits | |
| Supracondylar fractures (Undisplaced/minimally displaced) | Compound fractures | ||
| Extra articular distal radius fracture | Crush injuries | ||
| Hand fractures | |||
| Reducible dislocations | |||
| Lower Limb trauma | Shaft femur fractures with acceptable angulation and displacements | Fracture- dislocations | Un reduced dislocations |
| Fractures around the knee | Dislocations | Compartment syndrome | |
| Shaft tibial fractures | Displaced fractures e.g. neck of femur, shaft femur, fractures around the ankle | Fractures with neurovascular deficits | |
| Metatarsal and phalanx fractures | Compound fractures | ||
| Calcaneus fractures | Crush injuries | ||
| Reducible dislocations | Compound fractures | ||
| Pelvic-Acetabular trauma | Stable/minimally displaced fractures | Open book type of injuries | |
| Unstable fractures | |||
Table 2: Suggested Indications and Contraindications for Conservative Management of fractures and dislocations in adults, during COVID-19 pandemic.
| Limb and Spinal injuries in Adults | Preferred Indications | Equivocal Indications | Contraindications |
|---|---|---|---|
| Upper Limb | Clavicle fractures | Fractures with significant displacement e.g., proximal humerus, humeral shaft, intercondylar humerus, olecranon | Severe compound fractures |
| AC joint dislocations | Radius and ulna shaft fractures | Severe crush injuries | |
| Scapula fractures | Intra articular distal radius fractures | Fractures with vascular | |
| Fractures without gross displacements e.g. proximal humerus, humeral shaft, Humeral supra-condylar | Periprosthetic fractures | injuries | |
| Extra articular distal radius fractures | Pathological fractures | Compartment syndrome | |
| Scaphoid fractures | Grossly comminuted and | ||
| Metacarpal fractures | displaced intra articular | ||
| Phalanx fractures | fractures | ||
| Reducible dislocations | Irreducible dislocations | ||
| Spine | Stable fractures | Unstable spine fractures with neural deficit | Stable spine fractures |
| Fractures with Progressive/acute neurologic deficit | |||
| Lower limb | Pubic rami fracturesLower limb | Pelvic-acetabular fractures with significant displacement | Fracture neck of femur |
| Undisplaced pelvic-acetabular fractures | Inter trochanteric fractures | Femur shaft fractures | |
| Undisplaced fractures around knee | Intercondylar fractures | Severe compound fractures | |
| Calcaneus fractures without gross displacement | Tibial shaft fractures | Severe crush injuries | |
| Metatarsal fractures | Tibial condyle fractures | Fractures with vascular injuries | |
| Phalanx fractures | Patella fracture | Compartment syndrome | |
| Taller fractures | Grossly comminuted and displaced intra articular fractures | ||
| Calcaneus fractures with gross displacement | Irreducible dislocations | ||
| Lis franc injuries | |||
| Peri prosthetic fractures | |||
| Pathological fractures |
Table 1 and 2: It is obvious from this table that a majority of paediatric injuries can be adequately managed with conservative treatment.
Operative management is needed in articular and periarticular fractures most in the adult fractures.
However, there are certain absolute indication for the surgery of fractures and dislocation, even in the pandemic times (Table 2), which are also the contraindications for conservative management. The aim should be to minimise risk of viral transmission by avoiding Aerosol Generating Procedures (AGP) and minimising risk of infection with appropriate use of Personal Protective Equipment (PPE). These principles are critically engrained in our current orthopaedic response to the pandemic.
CONTRARY TO THE SITUATION AND EVIDENCE
Within orthopaedics, previous research has demonstrated that postponing major elective surgery, such as total joint arthroplasty or surgical non- union management, causes a considerable decrease in a patients’ quality of life [8- 11] A significant deterioration of patient quality of life may occur over the course of their pre- operative waiting period.[10,11] Globally, a vast number of patients are at risk of suffering major quality of life deterioration as a result of their elective surgery being postponed or cancelled. the current guidance on elective surgery during the COVID- 19 pandemic, assess how this guidance may impact orthopaedic care, to identify current elective surgery guidance globally as a result of the COVID- 19 pandemic within MEDLINE, EMBASE, Global Health and Emcare from the databases from inception until 6 April 2020.[12]
Elective surgery guidance
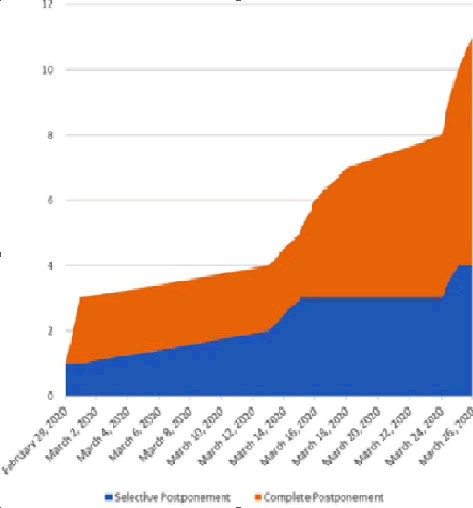
There were seven (63.6%) guidance reports that suggested a complete postponement of non- elective surgical procedures, whereas four (36.4%) reports suggested the use of selective postponement of these procedures. Throughout the month of March, elective surgery guidance became increasingly strong in its suggestions for completely postponing all elective surgery.
Figure 1 provides an overview of the cumulative number of guidance documents within these categories over time. The guidance for postponement of elective surgeries typically suggested that procedures should be rescheduled to a time after the COVID- 19 pandemic is over; however, it is unclear as to when this will be. Guidance from the British National Health Service (NHS) has suggested elective surgery will postponed until at least mid- July, as guidance suggested a 3 monthpostponement starting 15 April.[13,14]
Stronger recommendations against elective surgery throughout the month of Marchis highlighted by two guidance reports provided by the American College of Surgeons on 13 and 24 March 2020. Guidance on 13 March 2020 suggested to “reschedule elective surgeries as necessary”2 weeks later, guidance from the same organization strengthened their guidance to provide athree- phase plan, which ends in “phase III: to eliminate all elective practice”. This trend was seen across guidance groups. Table 3 provides a brief summary of each report’s guidance on elective surgery in light of the COVID- 19 pandemic.
| Organization | Country | Date published | Details regarding elective surgery | Details regarding non operative management |
|---|---|---|---|---|
| CDC | US | 29-Feb-20 | Reschedule elective surgeries as necessary. Shift elective urgent inpasione diagnostic and surgical procedures to seining’s, when Reasible. | None |
| Tao et al. [Overview of National Health Commission of the People's Republic of China | China | 01-Mar-20 | For pasions undergoing elective surgery it is recommended not 10 perform surgical for the time being, and they can be elecive alter the opidemic is under conical. | None |
| Royal Australasian College DF Surgeons | Australia | 01-Mar-20 | Series Di from elective specialey associations: Non-urgent and elective surgeries to be suspended immediately. | Non operative treatment naments will conler advantage over operative naments If similar cuicomes, or aven slightly downgraded outcomes are expensed. |
| American College of Surgeons | US | 13-Mar-20 | Reschedule elective surgeries as necessary. Shift elective urganit inpasione diagnostic and surgical procedures 10 curpasione seining’s, when Reasible. List by subspecialty declaring which surgeries should be schedule or reschedule depending the phase of COVID-19 pandemic. Phase Il (curial elective practice), phase II (eliminaes elective practice). Full lisa by subspecialist in document. | None |
| 24-Mar-20 | Consider non operative management whenever it is dinically appropriate for the patient. | |||
| Caners for Medicare and Medicaid Services | US | 15-Mar-20 | CMS urges healthcare facilities and cinicians 10 consider using a siered appreach 10 cursaling non- emergent, elective medical services and treatement. | None |
| NHS | UK | 16-Mar-20 | The elective component of trauma and or rehopaedic work may be curialled. Elective resources should be repurposed 10 suppon influx of COVID cases. | A number of injuries can be managed eiher operatively or nori-aperasively. Clinical decisions during a serious incident must sako into accounts the available laciliey for the impact this may have on the whole community. |
| 18-Mar-20 | NHS hospitals in England have been told 60 suspend all non-urgent elective surgery for at lease 3months from 15 April 2020 | None | ||
| British Onhopaedic Association | UK | 24-Mar-20 | Pationis should have consuliant-delivered, delinitive locision-making at Brst amendance and, in panicular, should not be scheduled for surgery without senior input. | Aim for non-operative management for the majoriey of injuries where this is possible and sale. |
| WHO | International | 25-Mar-20 | Many routine and elecive services may be posipaned or suspended. Establishing effective passion How (including screening eriage, and targeted referral Di COVID-19 and cases) is essential at all levels. | None |
| Royal College of Surgeons | UK | 26-Mar-20 | Acuso/omergancy pationis are priority. Only emergency endoscopic procedures should be performed. | Where non-operaive management is possible and reasonable Isuch as for early appendicitis and acute cholecysanis) this should be implemented. |
Table 3: Elective surgery guidance from health organization.
DISCUSSION
Based on the guidance documents included in this review, it is apparent that elective surgical practices are being postponed globally. Transitions from selective rescheduling to complete rescheduling of all elective patients has been occurring throughout the month of March. Major guidance groups such as the Centers for Disease Control and Prevention
(CDC), NHS, and WHO, have provided guidance on elective surgery, which has been disseminated by smaller organizations and local governments.[15]. The Royal Australasian College of Medicine suggested that “Non operative treatments will confer advantage over operative treatments if similar outcomes, or even slightly downgraded outcomes are expected”, as even slightly worse outcomes than what would be expected with surgery may still be a better option than providing no treatment at all.[16].
CONCLUSION
Global guidance from major medical associations are in agreement that elective surgical procedures require postponement in order to minimize the risk of COVID- 19 spread, as well as increase available hospital resources for managing the influx of COVID- 19 patients. For patients that have their elective surgery postponed, there is no clarity as to how long it will be before their elective surgeries will be rescheduled. It is imperative that clinicians and patients consider non- operative, conservative treatment options in order to manage conditions and symptoms until surgical management options become available again, and to manage the increased surgical waitlists caused by the elective surgery shutdowns.
REFERENCES
- Matter P. (1998) History of the AO and its global effect on operative fracture treatment Clin Orthop Relat Res 347:11- 18
- (10May 2020) Public Health England COVID 19 Infection Prevention and Control (IPC) 2020 accessed.
- Charnley J (2003) The Closed Treatment of Common Fractures Cambridge Cambridge University Press
- Swiontkowski M (2 April 2020) COVID 19 pandemic and JBJS J Bone Joint Surg Am Epub ahead of print.
- Vannabouathong C, Devji T, Ekhtiari S (1 April 2020) Novel coronavirus COVID 19 current evidence and evolving strategies J Bone Joint Surg Am Epub ahead of print.
- Brindle M and Gawande A (23 March 2020) Managing COVID 19 in surgical systems Ann Surg Epub ahead of print.
- Wong J, Goh QY, Tan (11 March 2020) Preparing for a COVID 19 pandemic a review of operating room outbreak response measures in a large tertiary hospital in Singapore Can J Anesth Can Anesth Epub ahead of print.
- Brinker MR, Trivedi A and OConnor DP (2017) Debilitating effects of femoral nonunion on health- related quality of life J Orthop Trauma 31, e37â??e42
- Ostendorf M, Buskens E, van Stel H (2004) Waiting for total hip arthroplasty avoidable lossin quality time and preventable deterioration J Arthroplasty 19: 302â??309.
- Scott CEH, MacDonald DJ and Howie CR (2019) â??Worse than deathâ? and waiting for a joint arthroplasty Bone Joint J 101â??B: 941â??950.
- Brinker MR, Hanus BD, Sen M (2013) The devastating effects of tibial nonunion on healthrelated quality of life J Bone Joint Surg Am 95: 2170â??2176.
- Prada C, Chang Y, Poolman R (14 April 2020) Best practices for surgeons COVID 19 evidence based scoping review Version 2 OrthoEvidence.
- Iacobucci G (2020) Covid 19 all non- urgent elective surgery is suspended for at least three months in England. BMJ 368: m1106
- (14 April 2020) National Health Service Clinical guide for the management of trauma and orthopaedic patients during the coronavirus pandemic.
- Sarac NJ, Sarac BA, Schoenbrunner AR (13 April 2020) A review of state guidelines for elective orthopaedic procedures during the COVID 19 outbreak J Bone Joint Surg Am Epub ahead of print.
- (14 April 2020) Royal Australasian College of Surgeons COVID 19 information hub RACS.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences