Effectiveness of Bobath Approach and Therapeutic Ultrasound on Spasticity among Patients with Stroke
Muhammad Ahmed Qureshi*
Department of Faculty of Allied Medical Sciences Isra University, Karachi
- *Corresponding Author:
- Muhammad Ahmed Qureshi
Department of Faculty of Allied Medical Sciences Isra University, Karachi
E-mail: mohammad.ahmed2192@gmail.com
Received date: January 28, 2023, Manuscript No. IPPR-23-10715; Editor assigned date: February 02, 2023, PreQC No. IPPR-23-10715 (PQ); Reviewed date: February 12, 2023, QC No. IPPR-23-10715; Revised date: February 22, 2023, Manuscript No. IPPR-23-10715 (R);Published date: February 28, 2023, DOI: 10.36648/J Physiother Res.7.1.715
Citation: Qureshi MA (2023) Effectiveness of Bobath Approach and Therapeutic Ultrasound on Spasticity among Patients with Stroke J Physiother Res Vol.7 No.1:715
Abstract
Background
Spasticity is a well-known complication after stroke. Spasticity can be defining as the velocity dependent hyper moodiness of the muscular system to stretch, characterized by the increase in the tendon reflexes, exaggerated resistance to passive movement. And increase in tone (Hypertonia) due to loss of upper motor neuron inhibitory control. According to the health care provider it is very important to find out the spasticity and assume it is common and can be manageable. On the other hand, prevalence of post stroke spasticity can neither be measure directly.
Methodology
The study design was experimental, 30 participants were selected, equally and divided by purposive sampling technique into therapeutic ultrasound and Bobath group 3 sessions per weeks were given into 5consecutive weeks. Outcome measures were goniometry for measuring range of motion and Ashworth scoring scale for measuring spasticity.
Results
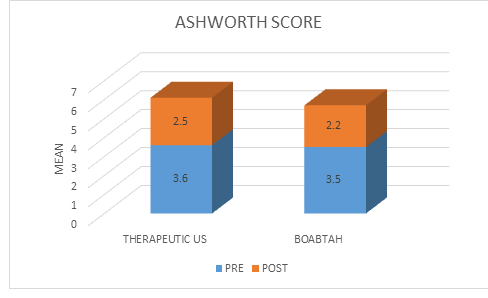
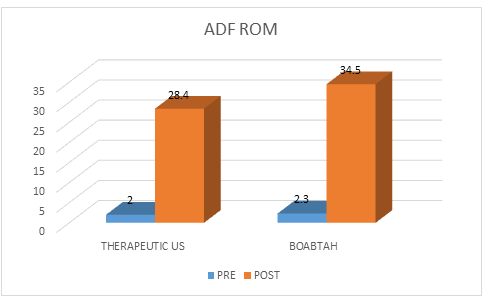
The mean pre and post of scores Ashworth score was in therapeutic ultrasound and Bobath were (3.6 to 2.5) and (3.5 to 2.2) and p-value for therapeutic ultrasound was <0.01 and for Bobath was <0.01. For range of motion (2.0 to 28.4) and (2.3 to 34.5) and p-value for therapeutic ultrasound was <0.01 and for Bobath was q<0.01 respectively.
Conclusion
Based on the results it is concluded that both techniques showed significant improvement in Ashworth scoring and goniometry for range of motion but Bobath was found to be most effective in managing spasticity.
Introduction
Stroke
Stroke can be defining as group of pathological condition which is categorized as the abrupt, non-convulsiveness functional loss of nervous system cause by loss of blood supply in brain and may be due to intracranial hemorrhages. Stroke can be classifying according to necrosis in the tissues, like anatomical position, causes, vasculatures involvement, oldness and non-hemorrhagic or hemorrhagic nature. Prof. czlonkwska said that cerebrovascular accident is a medical condition which is characterized as abrupt beginning of the central signs and general turbulences of functions in brain. Cerebrovascular accident is clinical disaster. Initial treatment can be helpful in lessen the damage to brain and other complication. The good news is that strokes can be treated and prevented [1].
Epidemiologic
According to the studies stroke is the third leading cause of death worldwide and majority of death due to strokes are occur in the low or middle income countries. Studies shows that 55 million people died from stroke worldwide in 2002 and 20% of this accident occurred in south Asia. Year to year death ratio is increasing, in 2015 it is recorded that 63 million death occurs and there will be 78 million deaths can occur in 2030 which is most of occur in poor countries in the world.
If we talk about the incidence of stroke in Pakistan it is five to ten times higher when compared with United Kingdom or United States. WHO estimated that death due to stroke in developing countries in 2001 accounted 85.5% worldwide?
According to the study which is carried out by Saleehen et al in Karachi stated that Pakistan people suffer from stroke in younger age if we compared it from western countries. Studies show that demographic difference in stroke disease pattern in developing and non-developing countries and highlight the increasing prevalence of atherosclerosis risk factor in poor reigns. These factors are hypertension 40% in Pakistan and 15-20% in west, diabetes 33% in Pakistan and 3-10% in west, smoking 21% in Pakistan and same in west.
Ayyub from Abbottabad shows in Pakistani women stroke occur in younger age when compared with the west and in Pakistan 46% of male stroke patients were 61-70 years of age and women from 51 to 60 years and the mean age of male is 64 and 49 for women. Hemorrhagic stroke appears to be more common in Pakistan compared with west; it’s about 10-15% of all strokes cases in west and 21-30% in Pakistan [2].
Risk Factors of Stroke
Risk factors of stroke includes: hypertension, diabetes, obesity, cardiovascular disease and smoking in Pakistan
Hypertension
Hypertension showed 18% of adult in 41 age group and 33% of 44 age group. And only 13% people of hypertension were on treatment.
Diabetes
10% of general population in Pakistan is suffering from diabetes. Stroke due to diabetes is about 20 to 30% with age group 25 to 40.
Obesity
Obesity is one of important risk factor causing stroke estimated about 25%. Female has affected more than male in Pakistan.
Smoking
It’s about 30% and more common in male which is 29% than female 3%. Highest prevalence of smoking is 49% in male with age 40 to 50 [3].
Complication of Stroke
Post stroke spasticity is a common complication can be associated with other sign and symptoms of UMN syndrome, includes antagonist/agonist co-contraction, lack ofcoordination and the weakness. The management of post stroke spasticity reduces muscle tone. It causes impairment and disabilities that cause negative impact on functional recovery causes gait abnormalities which may reduce quality of life, increase pain and joint contracture [4].
Types of Stroke
There are three type of stroke. Ischemic stroke, hemorrhagic stroke and transient ischemic stroke.
Ischemic Stroke
When there is an obstruction in a vessel than supply the blood to the brain. Fatty deposits in the vessels called as atherosclerosis are main cause of ischemic stroke. Fatty deposit causes two types of obstructions.
Cerebral Thrombosis
Causes blood clot made up of fatty plaque with in blood vessels.
Cerebral Embolism
Blood clot that forms at another location in the circulatory system, usually the heart and large arteries of the upper chest and neck. Part of the blood clot breaks loose, enters the bloodstream and travels through the brain’s blood vessels until it reaches vessels too small to let it pass.
Hemorrhagic Stroke
Occur when blood vessels ruptures. Common cause of this stroke is uncontrolled high blood pressure.
Transient Ischemic Attack
In this temporary blockage of blood flow to the brain. It doesn’t cause permanent damage [5].
Pathophysiology of Stroke
Path genetically, stroke integrates a heterogeneous group of diseases. Vessel occlusions account for 85% of all strokes, while primary intracerebral bleeding has a relatively low incidence of approximately 15%. Embolisms, of either arterio-arterial or cardiac genesis account for 75% of all cerebral vessel occlusions and are the most frequent cause for focally impeded blood flow within the brain [5].
We owe substantial insights into the pathophysiology of ischemic stroke to animal models, in particular to two fundamentally different rodent models of cerebral ischemia. In one model focal cerebral ischemia is induced, which clinically corresponds to ischemic stroke. In the other model, global cerebral ischemia is produced, which models the consequences of cardiac arrest. In this review, we will mainly discuss findings from models of focal cerebral ischemia, usually obtained in experiments using rats and mice. In these experiments, the middle cerebral artery is occluded. We further differentiate into models of permanent and transient focal cerebral ischemia, depending on whether perfusion is permanently cut off or only transiently. The latter also function as models for a spontaneous reperfusion, or for the state after successful lysis therapy with recombinant tissue plasminogen activator in humans, respectively [5].
How Stroke Causes Spasticity
There are three factors that results in increase muscle tone in patient having spasticity. Which are changes in the afferent input to spinal motor neurons, changes in reflex circuit’s motor neuron excitability and changes in the intrinsic properties of motor neurons? A definite quantity of tone or movement present in a muscles. A signals present in the brain that can control the tone of the muscle. If there is a damaged to the signal controlling system present in the brain by CVA, that causes increases in the muscle activity. This known as spasticity [6].
Spasticity
Spasticity is a well-known complication after stroke. Spasticity can be defining as the velocity dependent hyper moodiness of the muscular system to stretch, characterized by the increase in the tendon reflexes, exaggerated resistance to passive movement. And increase in tone (Hypertonia) due to loss of upper motor neuron inhibitory control. According to the health care provider measurement of spasticity is very chief and assumes that is very commonly occurring plus can be manageable. On the other hand, prevalence of post stroke spasticity can neither be measure directly [7].
Clinical features on the neurological examination, increased muscle tone, brisk reflexes, incoordination of the muscle and muscular weakness. According to the textbook spasticity is a clinical problem when it is interfering with the functions and patients care. Upper motor neuron syndrome can take days to months after the injury to central nervous system. Despite this presentation of one patient may different from the other patient having similar nervous system injury. No matter we know or don’t know about traumatic brain injury, multiple sclerosis, and spinal cord injury, the measurement of the spasticity and tone will be always unique to each individual. Incidence of spasticity is depending upon the cause of upper motor neuron lesion. When there is injury to the central motor pathways above there will be paralysis with changes in the brain and the spinal cord which causes changes in the motor behavior like, paresis, contracture, over activity of the muscle [8].
Spastic Muscle Pathophysiology
It is a complex phenomenon when we talk about the pathophysio of spastic muscle. While the accurate phenomena regarding pathophysiology of spastic muscle is uncertain, it is said that it is due to any disruption in descend pathway can cause spasticity. The upper motor neuron lesion has two traditional term sign and indications. A destructive symptom is low strength plus decreaseagility. The constructive points are considered through muscular over activity moreover increase in muscle toneor else wrong muscular activity. Others symptoms may be increase ligamentreactions, increase tone and spasm on flexor muscles. These altogether features called to be spasticity.
The point is that how these positive points come out. They are separated hooked on mainly 3 zones. One is vertebral responses inappropriate function of vertebral responses causes upper motor neuron lesion. These are afferent reliant, trusting on about type of bodily response beginning to the edge, just similar to muscle stretching, discomfort and subcutaneous and musclestimulus. Second is here a fiber which does not properly dependent on the peripheral afferent pathway although they contact with impulse movement in boundary of CNS. Third set of optimistic sign is voluntary muscle movement disorder. They are overlapping through adverse characteristic. On the other hand, this pathophysiology is mostlyattention on the constructive characteristic I:e feature considered throughover activeness of muscular group.
Upper motor neurons include supraspinal inhibitory and excitatory fibers, which descend to spinal cord using a balance control on spinal reflex activity. With pyramidal fibers but according to some study results reveals that wholesome lesion of pyramidalreasonsleastnervous deficit which can be called as pyramidal syndrome. Some ineptness in hand muscles, weakness, decrease reflexes of deep tendon follow through up limit in tendon reflex and signs of Babinski. Increase in tone and some additional form muscular activities not happen. Likewise, some low strength which happen due to cerebrovascular accident (CVA), pyramidal fibers is my not be the cause of it, may be due to upper motor neuron lesion fibers thatturns close to them. They called upper motor neuron (UMN) Para pyramidal not like extrapyramidal that have connotations in the basal ganglion.
An excitatory pathway also come from stem of brain, significant is what thatproduce fromtegmentumofbulbopontine.Thoseneuronsinclineonreticulospinaltract.Vestibulospinal fibers also has excitatory effect on spinal reflexes but somewhere separate from others and not looking as chief in increasing the tone of the muscle.
An incomplete lesion of the spinal cord, thatdevastated pathways of inhibitory however conserved pathways of excitatory, then they leftvertebral activates abandoned. These stimuli of excitatory are very powerful that can cause increase in muscle tone and increase in reflexes [9].
Measurement of Spasticity
When one uses the term measurement so if we talk about physiologic measurement, it refers to electrophysiological information that is related to muscle over activity. Examples of these are measuring the excitability of motor neural pool or measuring the decrease in length. Others are vibratory inhibitory reflex and Hmax/Mmax ratio noted tobe abnormal in spastic population.
Ashworth scale: Ashworth scale is a tool to measure the spasticity in muscles. It is universal scale to determine the spasticity. A researcher assign score ranging from 0 to 4 bases on resistance present in muscles which is passively perceive by the examiner by performing ROM. In this scale “0” is indicate that there is no increase in tone, and “4” is limb is rigid.
A study evaluated that Ashworth scale for planter flexor tone secondary to TBI shows minimal adequate just due to marginal interrater. Just like this study other study shows that Ashworth planter flexor of patients with stroke. And best correlation noted with score 0. The MAS was described by bohannon and smith in try to strengthen the previous Ashworth scale by adding 1+ measure. At last Ashworth and its cousin are well known easy to perform and having long use of history [10].
Modified Ashworth Scale for Grading Spasticity Grade Description
0 No increase in muscle tone
1 slight increase in muscle tone, manifested by a catch and release or by minimal resistance at the end of the range of motion when the affected part(s) is moved in flexion or extension
1+ slight increase in muscle tone, manifested by a catch, followed by minimal resistance throughout the remainder (Less than half) of the ROM
2 more marked increase in muscle tone through most of the ROM, but affected part(s) easily moved
3 considerable increases in muscle tone, passive movement difficult
4 affected part(s) rigid in flexion or extension [11].
RANGE OF MOTION
Measurement of range of motion is an essential component of a physical therapist. Range of motion is an important tool to measure the spasticity for many years. They are most widely used because easy to perform. The measurement can easily be obtained by using the goniometer. There is different type of goniometer are available in market but most usable is universal goniometer because it has low prize and easy to use. It has two arms and made up of transparent material and protector on it for measurement. One arm remains stationary and other arm moves across joint to measure range of motion [12].
Ultrasound
Spasticity impact negative influence on the function and activity of daily life. Spasticity can cause the pain, discomfort, fatigues, contracture and disturbance in the sleep. There are many options to manage the spasticity including the antispastic drugs, physical rehabilitation, physical modalities like infrared and ultrasound [13].
Ultrasound has thermal and mechanical effect on the tissues causing increase local metabolism, increase blood flow, tissue regeneration and reduce swelling and pain. Ultrasound not only provides viscoelastic changes in spasticity but can also be reduce the sensitivity of muscular spindle and motor neurons [13].
Ultrasound Energy
It’s about seventy ages meanwhile communication among highest sound waves frequencies and alive tissues stayed monitoredplususage of this verve for the purpose of treatment. Ultrasound is now using to treat wide variety of disorder. Ultrasound consist of highest frequencies powered vibration madeat what time initiator produce electrical power that will transformed into auditory vigorover automatic distortion of a crystal named piezoelectric that is placed in the transducer. Waves which manufactured are transmitted through broadcast through molecular accidentplus vibration through reformist damage of amount of power throughout channel over asoft tissue by the immersion, diffusion or smattering waves. Over-allquantity of vigor present in a beam said to be its energy which can be called as watts [14].
Therapeutic ultrasound has 0.75 to 3 MHz frequency range but most of the machines set with the frequency from 1 to 3 MHz’s low frequency ultrasound have more potential to penetration. Ultrasound with frequency 1 MHz is primary absorb by the tissues at depth 3 to 5 cm that is why recommended for deeper injuries. Ultrasound with frequency 3 MHz is recommended for superficial injuries which having depth only 1 to 2 cm [14].
Ultrasonic Rays
Frequency
The amount of spellsan element capability a wholeseries in 1sec. Classically, one and three megahertz [15].
Wavelength
A space among 2 equal facts in waveform with specific medium. Normally the wavelength in the tissues one megahertz conducting 1.5 millimeter when three megahertz it may be 0.5 millimeter [15].
Velocity
It is defining as the traveling of waves over the medium. on a saline fluid, aspeed of ultrasonic rays is about fifteen hundred meter/second whenassociated with aboutthree hundred and fifty meter/sec. as we know acoustic rays moves with more speed in denser medium.speed of waves mostly in tissues is supposed to bealike to that in saline [15].
Dose
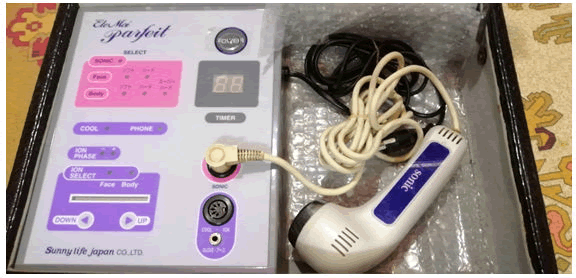
The equipment’s were operating at frequency 1 MHz, using continuous mode at 1.5 W/CM2. Duration of the treatment was 10 minutes on the spastic muscle [15].
Technical Details of Equipment Used
| Frequency | Frequency | mode | intensity | |
|---|---|---|---|---|
| Ultrasound Therapy | 1 | 10 | Continuous | 1.5 |
Physiological Effect of Ultrasound
Therapeutic ultrasound has thermal and non-thermal physiologic effect in the tissues. We can have achieved non-thermal effect with or without thermal effect. Thermal effect of therapeutic ultrasound on the tissues is the increase blood flow, reduce muscular spasm, and improve extensibility of muscle fibers and inflammationreaction. It’s said to be that thermal effect occurs byraises tissues heat by forty to four hundred fifty caimed at minimal five minutes. Higher the ultrasound intensity more will be thermal effect that can cause the damage to the tissue [16].
On other hand ultrasound non-thermal effects includes auditory microstreaming plus cavitation are very significant in management. Cavitation occur at what time bubbles filled with a gasenlarge plus collapse for ultrasonic encouraged stress variations on the material fluid due to which rise in stream in the adjoining material. When we talk about the effect of cavitation and microstreaming it stimulates the fibroblast reparation plus collagen mixture, materialrestoration and the bone remedial. According to the research study tendon healing is a minimal effect of therapeutic ultrasound [14].
Neurodevelopmental Treatment Bobath Concept
A famous physical therapist karel Bobath and Berta was described the Bobath concept. The Bobath concept also known as the neuro developmental technique spread rapidly because it has influenced physical, occupational and speech therapist for the sake of children. Neuro developmental treatment (Bobath concept) is used in the stroke rehabilitation in world wide. The aim of this approach is to improve recovery of the hemiplegic side by normalizing tone and pattern of the movement by the therapist using the handling techniques. In America physiotherapist experienced positive outcomes by using this concept in clinical setting. Many of the author’s concepts on the importance of identifying theoretical assumptions under the practice to formulate the hypothesis which can be related to the treatment that will can be tested in studies. Some scientist finds out by the help of nine semi structured interviews that the Bobath concept is used because it can have facilitated normal movement. Bobath said that the motorized difficulties in cerebral palsy are riseas from central nervous system malfunctioning that interfere of posture and muscular activities. Bobath goal is to develop normal motor development and prevent from contracture and reduces spasticity. This technique focus on the motor component of tone in muscle and reactions and irregular motor pattern, controlling the posture, feeling, and awareness. Bobath called it as handling technique that works on when giving stimuli were used to prevent increases in muscle tone, irregular impulses and irregular motor pattern. Conclusion of Bobath is that it promotes the rigid following of normal developmental sequence [15].
Role of Bobath in Rehabilitation
Physical therapist who attended a neuro developmental technique exercise way enduring instruction in bobath management on other hand they can merged bobath link. Neurodevelopmental practice in the pitch has not essentiallysavedbound with the appraisal which is qualified by bobath plus hisclassmates. According to works reproduces a mutable state of training in this ground along with misunderstanding around present bobath philosophies. There is a controversy in some articles that bobath management subjective primarily via impulse plus categorized models movement control was effective in up-to-date reproductions that cannot attention on neurological explanation or movement presentation [15].
Motor Control of Bobath Approach
Motor control on systems provides the groundwork of up-to-date theoretical reinforcement of Bobath concept. This theory on the system is based on the work of Bernstein (1967). Bernstein acknowledged that it was significant to have aconsiderate on thespecific of the movement system, and internal and the external forcesstand-in on the body, in order to improve an understanding of the neural regulator of the movement. As of a biomechanical perspective, he well-thought-out the many degrees of the autonomy provided by the several joints within the body and the regulator desired to enable them to work collected as a functional unit [15].
The Bobath Concept Scientific Presentation
Bobath concept in controlling motor activities involves in the whole patient, including sensual, adoptive behavior, cognitive and movement’s problems with management deliver to the client’sessentials. The concept of Bobath is an interactive process for both patient and the physical therapist. Therapist should be skillful in movement analysis and should be able to understand the component of the human body movements. It is a technique which involves in motor learning, neurophysiology and human movement which promotes the individual to optimize the functions. Patient is assessed according to the present of the injury, client’s motormanifestation and likely to get the most out of their effortproductivity [15].
When applying Bobath approach it must be continuous adopt to individual changing response rather than stereotype or repetitive (partridge et al 1997).
Neurodevelopmental technique is area oriented and mission specific by which a person cans taskprofessionally orexcellently [15].
In Bobath approach the interaction between patient and the therapist simplificationchiefs to improve functions. A duty of a practicnaire isexplain the movement pluscreate movement potential. The aim of treatment is to improve the effectiveness of motor component in individual having UMN lesion [15].
Therapy with the Bobath approach is a learning process to regain motor and advancement of reimbursement that happencertainly due to injury. (Raine 2007) [15].
Literature Review
Emilia Miko ajewska in 2012 conducted a Study to assess the results of rehabilitation for normalization the tone of muscle with the help of neurodevelopmental technique (Bobath). 60 patients are included in this study which develops spasticity after ischemic cerebrovascular accident (CVA). Ten session of Bobath approach provided in two weeks. According to results regaining in sixteen patients is (25.68%), deterioration in one patient which is estimated as (1.68%), in 8 individuals there is no changes which estimated as (13.32%). Results showed that major variations noticed in tone when assessing with Ashworth scale [16].
According to the study conducted by Sheila Lennon et al in 2010 that aimed to providing an expert knowledge about bobath approach on the spasticity developing after stroke. 52 individuals with age range of 40-50 were participated in this study. Results concluded that the study reveals that bobath tends to be effective more in early ages [17].
A study is conducted by Kenneth Monaghan et al in 2011 to compare the bobath and therapeutic ultrasound efficacy in post stroke spasticity. 30 patients participated with inclusion criteria patient’s age is over 18 of any gender. Result revealed that bobath is more effective than therapeutic ultrasound in management of spasticity after stroke [18].
NN Ansari et al conducted a study on the Bobath approach effect on the excitability of the spinal alpha motor neurons in the CVAindividuals with increasing tone. The study was randomized control trial, 10 patients with the age of 37 to 70 years have been taken in this study which has average 60 having ankle planter flexion spasticity. NN Ansari and its colleagues were giving 10 sessions and 3 sessions per week. Result showed increase in ankle planter flexion range of motion by applying bobath approach [19].
According to the study conducted by the Charlene Butler et al on Effects of neurodevelopmental treatment (NDT) for cerebral palsy. He took 18 months to 22 years of children having spasticity. According to the result of study showed that when apply the bobath approach to the children with 20 sessions improves dynamic range of motion but not facilitate the social, emotional and cognitive development [20].
A study conducted by Dianne B et al on Review of Physical Therapy Alternatives for Reducing Muscle Contracture. Neurodevelopmental technique is used in this research to reduce muscle contracture. Participant in this study is ranging from 20 to 40 age group. When applying the bobath technique on patients having 20 sessions, it is found no significant changes in the muscle contracture, only 2-5 range of motion have been achieved by this approach [21].
Ayla Fil et al conducted a study in 2010. The aim of this research is findout efficiency bobath approach with transcutaneous electrical nerve stimulator in increase in tone after stroke. A prospective randomized control trail selected 48 patients. Application of bobath application with the electrical stimulation on the antagonist muscle proved to be efficient in preventing the spasticity [22].
Another study conducted by Susan Ronan et al in 2007 on Non-operative management of spasticity in children. Study works on range of motion by using bobath approach to modify the abnormal reflexes associated with tone. In this study 239 children were treated. According to this study reduces the spasticity in the gastrocnemius muscle and increase in range of motion about 15-250 [23].
According to the study conducted by the Sheila Lennon on re-education of gait which is built on Bobath approach. This study using bobcat approach by reducing sparsity to improve gait. Age group ranging from 65-71 years was going through 30 physical therapy sessions in 15-week period. Therapy demonstrates improvement in the range and reduces the tone and improved mobility [24].
M. Abo, Y in 2013 conducted randomized control trail on neurorehabilitation home based functional training in post stroke patients. The study includes 295 patients providing neurodevelopmental approach on home rehabilitation to improve tone and function with age ranging from 20-50 years. Results revealed that increase in active motor function by improving range of motion [25].
A study is conducted by the Sheila Lennon on the Bobath concept: a critical review of the theoretical assumptions that guide physiotherapy practice in stroke rehabilitation. Sheila uses bobath technique in stroke rehabilitation. By the help of Bobath approach Sheila works on CNS motor control activities by reducing the tone. 50 participants were selected for this study. Conclusion revealed that by applying Bobath on the patients during stroke rehabilitation it correct abnormal signal arising from, brain ultimately reduces the spasticity [26].
Study is conducted by Noureddin et al on effectiveness of ultrasound and infrared in spastic muscle. The aimed of this study is to compare the effects of therapeutic ultrasound and infrared in spasticity of muscle and range of motion in hemiplegic subject on planter flexion muscle spasticity. A cross sectional study includes 21 patients in this study in which 13 are male and 8 are females with age group 27-78 years old. 15-20 minutes’ session were provided to the patients. Results showed that neither therapeutic ultrasound nor infrared reduces the spasticity in the muscles [27].
N. Smania et al in 2010 conducted an experimental study on the rehabilitation procedures in the management of the spasticity. They worked on to find out the best possible modalities for the treatment of muscle spasticity. 30 patients were selected in this study with age group is 30-57 years old. According to the results ultrasound showed positive result in reducing spasticity, pain and increase range of motion of spastic muscle [28].
A randomized control trail study is conducted by N.N Ansari et al on the effect of physiotherapeutic ultrasound on muscle spasticity in patient with hemiplegic. Purpose of study is to find out efficacy of therapeutic ultrasound on muscle spasticity. In this study four patient with mean age 57 after first ever stroke were included. Results showed passive minor range of motion in ankle joint is improved by treating with ultrasound but no significant changes noted in spasticity [29].
The study is conducted by the N.N Ansari et al on therapeutic ultrasound in the treatment of ankle planter flexion spasticity in a unilateral stroke population. The aim of this randomized control trail is to find out the effectiveness of continuous ultrasound therapy on ankle planter flexion spasticity. Twelve patients have been selected in which 6 are male and 6 are female and 15 treatment session were provided in 3 days per week. Result of this study showed that reduce in tone and improve in planter flexion [30].
A randomized control study is conducted by the Sahin et al on 2011 on efficacy of therapeutic ultrasound in the treatment of spasticity. The main motive of research to determine effect of therapeutic ultrasound on spastic muscle of anklenamed planter flexor after cerebrovascular accident. They took hemiplegic patients with grade 2-3 ankle planter flexor spasticity. He divided the subjects into two groups and passive stretching were applied to both groups along with 10 min therapeutic ultrasound applied to one group using continuous mode to the calf muscles according to the results ultrasound applied with combination of passive stretching of ankle was said to be effected in minimizing spasticity [31].
A study is conducted by the jean. Michel gracias et al on physical modalities other than stretch in spastic hypertonia. The purpose of this study is to find out the efficiency of physical modalities like ultrasound, heating pad, cold pack, and TENS. 30 patients were included in this study and ages ranging from 25-55 years old. The potential capacity of therapeutic ultrasound in reducing the hypertonia of muscle is satisfactory [32].
Another study conducted by the Alessandro Picelli et al in 2015 on efficacy of therapeutic ultrasound and TENS related with botulinum toxin type A in the management of spastic equines in adulthood following stroke. Purpose of randomized control test is to determine efficiency of ultrasound and transcutaneous electrical nerve stimulatorthrough type a botulinum toxin. Thirty patients with chronic stroke were randomly selected. patients were divided into 3 groups. Therapeutic ultrasound is applied on one group and TNES and botulinum toxin on other groups. Results showed botulinum injection have better effect than therapeutic ultrasound in the spasticity of calf muscle [33].
According to the study the role of therapy in spastic management conducted by the Thomas Watanabe. Thomas use variety of modalities to determine the effect of physical modalities in spasticity. He applied the ultrasound for 15-20 minutes in 50 participants. The result concluded the study is physical modalities including ultrasound therapy is essential to minimize the spasticity [34].
Bobath Berta conducted a randomized control trail on the importance of the reduction of muscle tone and the control of mass reflex action in the treatment of spasticity. In this study Berta give the importance of tone reduction to increase range of motion. He described Bobath approach as a tone reducing therapy. Berta took 30 patients in this study. Results revealed that bobath approach can reduce the spasticity of a muscle that can possibly improve range of motion [35].
The study is conducted by D. Richardson on physical therapy in spasticity. The aim of this cross sectional study is to identify key component of a physical therapy approach and outline specific techniques for reducing the spasticity. He took 50 patients foe their study with age group 25-50 years. According to the study Bobath approach can be helpful in reducing muscle tone along with increase range of motion [36].
Another study is conducted by Eileen g fowler et al on the result of strengthening exercises on quadriceps femoris muscle on spasticity in child with C.P. Twenty-four subject with mean age 15-20 were selected for this study which is subdivided into two groups. Bobath approach is applied to group one and muscle strengthening on group two. Results showed than strengthening exercise do not facilitate in reducing the muscle tone although some changes can be seen in tone when applying Bobath approach [37].
C.A Speed conducted a study on ultrasound on the lesions that occurs in soft tissues. Ultrasound used mostly when management of laxmuscleinjuries like pain, injury, increase soft tissue mobility and spasticity. He took 35 participants with age 30-60 years old randomly. According to the result it is stated that ultrasound therapy useful in reducing pain, spasticity, and increase range of motion [38].
A study is conducted by the Pippa shanks in 2010 on the effectiveness of therapeutic ultrasound for musculoskeletal conditions of lower limb. The aimed of this study is to evaluate the effectiveness of therapeutic ultrasound for musculoskeletal conditions of lower limbs. 15 participants are included in this study. According to the results there is no quality evidence suggest that therapeutic ultrasound is effective in treatment of spasticity and other musculo skeletal conditions [39].
Antonino Naro et al is conducted a study in 2017 on advances in the tone decreases management: A treatment by non-Pharmacological. Aim of this study is to determine non-pharmacological treatment to reduce spasticity. He uses different modalities to treat spasticity. Result showed ultrasound can be effective in treating spasticity [40].
Another study is conducted by the Bhasker Amatya in 2013 on spasticity in multiple sclerosis by non-pharmacological management. Aimed of this study is to measure the efficacy of numerous non pharmacological treatments for the management of decreases tone in adults with multiple sclerosis. The study includes 301 participants over 18 years old and applied different modalities like TENS, body vibrator, and ultrasound. Result showed that among these modalities ultrasound is more beneficial in reducing the spasticity in MS [41].
Julie Vaughan Graham et al conducted a study on the Bobath concept in contemporary practice in clinical side. Aimed of research is provide the benefits of neuro developmental technique. This cross sectional study showed that bobath approach is very useful in normalize tone, regain motor control, improve posture and lengthen tight muscles [42].
According to the study does electrical stimulation reduce spasticity after stroke? A randomized controlled study conducted by Amir H Bakhtiary et al. the aim of this study is to inspect theoutcome of TENS in spastic planter flexor muscle in CVA patients. Forty stroke patients (aged from 42 to 65 years) with ankle plantar flexor spasticity. Results revealed that when applying the Bobath approach combine with TENS can helpful in reducing the tone in spastic muscle in CVA patients [43].
Sue Raine conducted the study on the defining the bobath concept using the Delphi technique. The aim of the present study was to use the Delphi technique to enable experts in the field to define the current Bobath concept. Data was collected from about 150 participants and sent out to the group of experts. Result concluded by the experts is that bobath approach is useful in decrease spasticity [44].
Albert t et al conducted a study on the physiotherapy of spasticity. The aim of this study is to find out the physiotherapy technique in reducing spasticity in stroke patients. According to the study Albert tries to prevent the paralysis due to spasticity plus improve voluntary motor activity of limbs. Although electrical stimulation can reduce spasticity if placed on antagonist muscle [45].
A study is conducted by YounanZhang et al in 2012 on the incidence, prevalence and mortality of stroke in France, Germany, Italy, Spain, UK and US. The purpose of this study is to find out the epidemiology of stroke in above mention countries. Data is collected by literature database and online sources to identify mortality, prevalence and incidence of CVA from 2000 year onwards. Results concluded that the study is 23 sources said incidence, mortality and prevalence from stroke increase with age and are more in male than females [46].
S.R. Belagaje et al conducted a study in 2014 on The Adverse Effect of Spasticity on 3-Month Post Stroke Outcome Using a Population-Based Model. The aimed of this study is to find out the adverse effect of spasticity from stroke in three months. In this study 460 ischemic patients were included with age average is 67 years old. Results revealed that after stroke spasticity is develop in to three months which causes functional independence [47].
A cross sectional study is conducted by the Bruce Ovbiagele et al in 2014 on post stroke outcomes. The purpose of this study is to find out the complication occur after the stroke. In this study data is collected from different data based. Results showed there is an evidence of post stroke complications like vascular events, recurrent stroke, spasticity, upper extremities impairment and several walking disabilities [48].
A study Prevalence of Stroke and Associated Risk Factors in Sleman District of Yogyakarta Special Region, Indonesia is conducted by Ismail Setyopranoto et al in 2019. The purpose of the study is to find out the prevalence of CVA and its risk factors in sleman district. Data is collected from community based data by sleman health and demographic surveillance system. Simply socio economic and demographic data was collected. According to the results of the study there is higher prevalence of stroke which is increases with age, hypertension and diabetes [49].
Thibaut A conducted a study on Spasticity after stroke: physiology, assessment and treatment in 2013. An aimed of this study is to find out the physiology, assessment and treatment option for spasticity after the stroke. Data is collected from different articles which show that spasticity occurs after stroke 30% of patients. Results show that assessment of spasticity can be done with neuro imaging and treatment usually is drug and rehabilitation. Results showed that more studies are require finding out the efficacy of treatment [50].
Mesequer AB conducted a study in 2018 on Inter and intra-rater reliability of the Modified Ashworth Scale: a systematic review and meta-analysis. The purpose of this study is to find out the validity and reliability of the Ashworth scale. Concerned data about thirty-three studies was collected from PubMed, Embase and CINAHL. Results showed this study was Ashworth scoring scale has significant satisfactory in assessment of the muscle tone [51].
A study goniometric reliability in a clinical setting. Subtalar and ankle joint measurement is conducted by Elveru RA et al in 1998. This study is done for find out the reliability and validity of goniometer in the measurement of subtalar joint of ankle. In this study 43 patients were included for the measurement of ankle dorsiflexion. Results of this study reveal that goniometer is reliable device in measurement of ankle range of motion [52].
Ward AB conducted a study in 2012 on Aliterature reviewof the pathophysiology and onset of post-stroke spasticity. Data is extract from online data base. Results reveal that when there is brain injury that cause imbalance of excitatory and inhibitory pathways that causes UMN symptoms ultimately spasticity occur. Spasticity can be occurring by weakness of muscle, decrease activities of daily life and history of smoking [53].
A study is conducted by Michiel L. Bots in 1996 on prevalence of stroke in the general population. A purpose of this study is find out the incidence between self-reported, medically confirmed and hospitalization stroke. In this cohort study 7983 participant were included with age average 55 years old. Results showed self-reported were 47% and 53% was medically confirmed [54].
Kim DH et al conducted a study on validity and reliability of ankle dorsi flexion measures in children. Purpose of this study was to compare the goniometer with tape measures methods. 50 participants were included in this study with age average about 20. According to the results it is stated that tape method is more reliable than goniometer [55].
Objective of the Study
The objective of this study is to determine the effectiveness of bobath and therapeutic ultrasound on spasticity among patient with stroke.
Hypothesis
H1 Hypothesis
Bobath concept is more effective than therapeutic ultrasound in reducing the spasticity among patient with stroke.
H2 Hypothesis
Therapeutic ultrasound is more effective than the Bobath approach in spasticity among patients with stroke.
Rational of the Study
Bobath is common treatment option for spasticity in patient with stroke. There is lack of literature on effectiveness of Bobath and therapeutic ultrasound on spasticity of calf muscle in stroke patient and there was no any literature found on comparison of effectiveness of therapeutic ultrasound and Bobath in spasticity on calf muscle.
Significance of the Study
Spasticity is the measure complains in the stroke. Spasticity significantly impair one’s activities of daily living and social life. Various treatment techniques in physical therapy have been applied to treat spasticity in calf muscle in stroke but still best and standard technique in unclear. Results will help to identify which technique among both of them has better efficacy for the management of spasticity in calf muscle in patient with stroke. This study helps the professionalist to practice in clinical setting to better improvement and also benefits to patients for improving quality of life.
Material and Methods
STUDY DESIGN
This study was experimental.
STUDY SETTING
Participants were conducted from “ISRA hospital”, “Majee hospital”, “Al Shifa private clinic”, and “Imam Physiotherapy center”, Hyderabad.
DURATION OF THE STUDY
Six months after the approval of synopsis.
Sampling technique
Purposive sampling was used
Sample size
Participants were selected for the study.
Inclusion Criteria
• Diagnosed cases of stroke.
• Stroke more than 6 months.
• Spasticity of grade 3 and 4 according to Ashworth scoring scale.
• Spasticity in the calf muscle.
• Both male and female participants were selected.
• Patients who were agree to participate in the study.
Exclusion Criteria
• Flaccid paralysis.
• Presence of fracture bone in lower limb.
• Open wound in calf muscle.
• If any metal implant in tibia or fibula.
• Patient who was not agree to participate in the study.
• Antispastic drug user.
• Unconscious patients.
Data Collection Tool
• Ashworth scale.
• Goniometer.
• Therapeutic ultrasound.
• Towel.
• Bed.
• Assessment Performa.
Ashworth scoring scale
The degree of muscle spasticity of the ankle planter flexion was assessed clinically with Ashworth scale. The resistance to the passive stretch was measured at the ankle joint of affected limb with the patient in supine position. This test considered in rapid manual ankle dorsiflexion flexion over duration about 1 sec by continuing one thousand and one. The degree of the resistance ti the passive muscle stretch that was felt by the examiner was scored on a five-point scale ranging from 0 to 4.
Ashworth Scoring Scale
0 normal muscle tones
1 minor muscle tone is increases, showed by a catch and release or by minimal resistance at the end of the range of motion when the affected part(s) is moved in flexion or extension
1+ slight increase in muscle tone, manifested by a catch, followed by minimal resistance throughout the remainder (Less than half) of the ROM
2 more marked increase in muscle tone through most of the ROM, but affected part(s) easily moved
3 considerable increases in muscle tone, passive movement difficult
4 affected part(s) rigid in flexion or extension
Goniometry
Patient affected knee in extension, Therapist: stood, facing lateral aspect of the limb and grasp the calcaneus firmly used his forearm to apply the maximum dorsiflexion force to planter surface of foot. At the end of PROM therapist maintained the pressure for a few sec. Until no further motion was detected. Universal goniometer proximal arm was placed on fibula bone head. Axis of universal goniometer was place one and half cm beneath to lateral side malleolus. Distal arm was allied parallel to a pretend line joining the projected point of the heel and base of fifth metatarsal.
Data Collection Procedure
The 30 Patients with spasticity in calf muscle were randomly separated into two groups of fifteen individuals each. All participants who fulfilled inclusion criteria were selected. Informed consent was taken from patients. In both groups assessment Performa was filled up by the therapist and ankle range of motion assessed by universal goniometer and spasticity was assessed by "ASHWORTH SCORING" as base track capacity on a day 1 (score of pre-test) earlier to starting the management.
For the individual in group A plus B received following treatment
• GROUP A_Therapeutic ultrasound
• GROUP B _Bobath approach
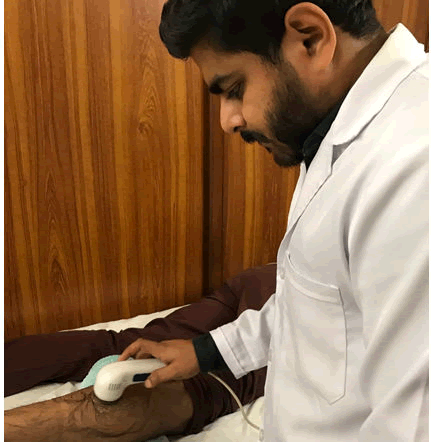
Procedure of Technique of therapeutic ultrasound
Patients with spasticity in calf muscle received 5weeks’ treatment of therapeutic ultrasound
Protocol
The study was divided into 3 phases
Step (1)
Pre-treatment assessment: Baseline outcome measure was Ashworth scale and range of motion.
Step (2)
Intervention phase: therapeutic ultrasound was given for 3 days in a week for 5 weeks.
Step (3)
Post- treatment assessment outcome measures were recorded at the end of 4 -weeks. (11)
For Group “A” Following 10 minutes of therapeutic ultrasound application. Starting position, the Position in prone, therapist stood on lateral side of the affected limb,towel place below the anterior surface of tibia, knee is full extension and the hips at full extension. Therapist were applied ultrasoundon the calf muscle with the equipment’s were operating at frequency 1MHz, using continuous mode at 1.5 W/CM2 and with circular movement. Duration of the treatment was 10 minutes on the spastic muscle [55].
Procedure of Technique of Bobath
For group “B” Following for the Bobath is use tone inhibiting method.
Starting position of a patient is supine, Knee in extension.
Therapist position
Standing in front of affected ankle joint.
Hand Placement of therapist
Grasp the patient’s ankle joint with both hand, maintain the subtalar joint in a neutral position. Flex the hip 20 to 30o, Dorsi ex the talocrural joint of the ankle by pulling the ankle joint to the superior side while this position is maintaining for at least 20 to 30 seconds.
Frequency
10 to 12 repetitions.
Intensity
20 to 30 seconds [56].
Data Analysis Procedure
Data was analyzed by Statistical Package for Social Sciences (SPSS) version 21. Descriptive statistics; frequency and percentage, mean and standard, deviation was used to assess baseline measurement.
Ethical Consideration
Confidentiality of data was secured and the identity of patients was coded. Informed consent from each participant was taken.
Budget
The budget of the study was around 60000 PKR.
Results
Data were stored and analyzed by using SPSS, version 21.0, mean and standard deviation were reported for age of participants, mean value of the goniometry at pre- post treatment for measuring range of motion of ankle joint among both groups were measured using paired t-test. Mean value of Ashworth scoring scale pre- post treatment of spasticity of calf muscle was measured using paired t-test. P-values less than 0.5 were considered as significant. Bar charts were also used to give the graphical presentation of mean scores. Intergroup comparison of mean value of goniometry and Ashworth scale were measured using independent t-test.
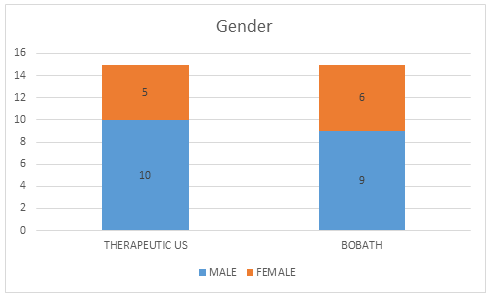
Table IV-1. Represent gender of participant which is in therapeutic ultrasound group 10 were males and 5 females. In Bobath group 9 were male and 6 were females. It also showed that equal numbers of participants were recruited in each group [15].
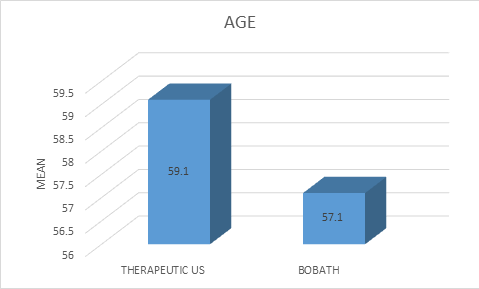
Table IV-2Represent mean age of patients which is 59.1 years in therapeutic ultrasound group and 57.7 years in Bobath group. It also showed that equal numbers of participants were recruited in each group [15].
Table IV-3 Showed mean, standard deviation and p value comparisons of Ashworth scores of therapeutic us and bobath patients at pre and post level of treatment. Results show that Ashworth value of therapeutic ultrasound and bobath greatly improved after treatment with p-values less than 0.01. The pre-treatment therapeutic ultrasound score was 3.6 ± 0.50 and post 2.5 ± 0.51. In bobath pre- treatment score is 3.5 ± o.51 and post 2.2 ± 0.45.
Table IV-4. Explains mean, standard deviation and p- value comparisons of ADFrom of therapeutic us and Bobath patients at pre and post level of treatment. Results showed that Dorsi-Flexion (ADF) value of therapeutic ultrasound and Bobath greatly improved after treatment with p-value less than 0.1. The pre-treatment ADF value of therapeutic ultrasound were 2.0 ± 2.53 and post-treatment value is 28.4 ± 4.28. In Bobath group ADF value in pre-treatment was 2.3 ± 2.58 and post-treatment value is 34.5 ± 5.71.
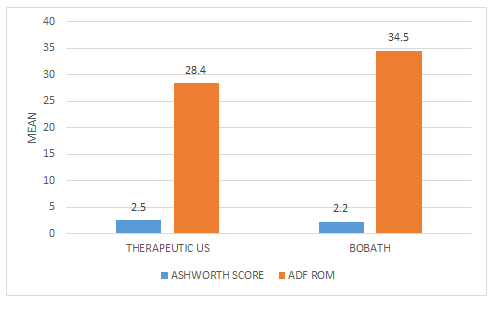
Table IV-5. Gives the post mean comparisons ofankle dorsi-flexion (ADF) rom andAshworth scores between therapeutic us and Bobath patients after treatment. Results shows that all two parameters are significantly improved among both groups. But dorsi-flexion (ADF) greatly improved in Bobath group and Ashworth score is decrease in Bobath.
| N | Percent | Male | Female | |
|---|---|---|---|---|
| Gander of participants in Therapeutic US group | 15 | 100.0% | 10 | 5 |
| Gander of participants in Bobath Group | 15 | 100.0% | 9 | 6 |
Table 1: Gender of the participants.
| N | Percent | Mean | SD | |
|---|---|---|---|---|
| Age of participants in Therapeutic US group | 15 | 100.0% | 59.1 | 8.59291 |
| Age of participants in Bobath Group | 15 | 100.0% | 57.7 | 8.11935 |
Table 2: Age of the participants.
| Ashworth Scores | Pre | Post | p-value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Therapeutic US Patients (n=15) | 3.6 | 0.50709 | 2.5 | 0.51640 | <0.01* |
| Bobath Patients (n=15) | 3.5 | 0.51640 | 2.2 | 0.45774 | <0.01* |
Table 3: Mean comparisons of Ashworth Scores of therapeutic US and Bobath patients at pre and post level of treatment.
| ADF ROM | Pre | Post | p-value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Therapeutic US Patients (n=15) | 2.0 | 2.53546 | 28.4 | 4.28952 | <0.01* |
| Bobath Patients (n=15) | 2.3 | 2.58199 | 34.5 | 5.78010 | <0.01* |
Table 4: Mean comparisons of ADFROM of therapeutic US and Bobath patients at pre and post level of treatment.
| Post Treatment | Therapeutic US | Bobath | p-value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Ashworth Scores | 2.5 | 0.51640 | 2.2 | 0.45774 | <0.05* |
| ADF ROM | 28.4 | 4.28952 | 34.5 | 5.78010 | >0.05* |
Table 5: Mean comparison of ADF ROM andAshworth Scores between therapeutic US and Bobath patients after treatment.
Discussion
Spasticity is most common complication after the stroke and causes considerable personal, community, financial burden globally. According to a study worldwide prevalence of spasticity in calf muscle shows that spasticity is the one of major problem throughout the world which is common after the cerebrovascular accident which is common in males as compare to females in all groups [51].
The purpose of the study was to compare the effect of therapeutic ultrasound and Bobath approach in spasticity of calf muscle. This research intended to review the influence of two treatments and the degrees of change in range of motion and spasticity of calf muscle. When compared the purpose with this study was effectiveness of bobath approach and therapeutic ultrasound on spasticity on calf among patient with stroke.
For ankle dorsiflexion angle, patient with calf muscle spasticity have decrease range of motion as compare to those without spasticity of calf muscle. The result of this study showed that ankle dorsi-flexion range of motion of calf muscle were measured by using universal goniometer and it is found improved in range of motion of ankle dorsi-flexion. After Bobath pre-treatment value is 2.3 ± 2.58 to post treatment 34.5 ± 5.7. Another study. Another study is conducted by Emilia mikolajewska sates that Bobath approach showed significant improvement in ankle dorsi-flexion range of motion from is 2.9 ± 3.1 to post treatment 31.2 ± 5.5. Shelia Lennon sates that after performing Bobath on calf muscle spasticity ankle dorsi-flexion improved from 110 to 350 [16]. N.N Ansari et al states that after performing Bobath approach magnitude changes in ankle dorsi-flexion angle post treatment was higher in the Bobath group which may be due to the tone inhibiting technique which cause reduces in the muscular tone in calf muscle [19].
According to this study results showed that Results showed that dorsi-flexion (ADF) value of therapeutic ultrasound and Bobath greatly improved after treatment with p-value less than 0.1. The pre-treatment ADF value of therapeutic ultrasound were 2.0 ± 2.53 and post-treatment value is 28.4 ± 4.28. In Bobath group ADF value in pre-treatment was 2.3 ± 2.58 and post-treatment value is 34.5 ± 5.7.
Spasticity is measure by using Ashworth scoring scale according to the study pre-treatment spasticity in therapeutic ultrasound group in mean value is 3.6 of 4 and post treatment is 2.5. On the other hand, pre-treatment spasticity score in Bobath group 3.5 and post-treatment is 2.2. Another study is conducted by Charlene butler ET AL states that spasticity in calf muscle is reducing after applying the Bobath approach to the subject and pre-treatment mean value was 3.1 and post-treatment 2.0. Another study. [20].
According to my study Results showed that Ashworth value of therapeutic ultrasound and Bobath greatly improved after treatment with p-values less than 0.01. The pre-treatment therapeutic ultrasound score was 3.6 ± 0.50 and post 2.5 ± 0.51. In Bobath pre- treatment score is 3.5 ± o.51 and post 2.2 ± 0.45.
The study shows that when applying the Bobath to the participant having the spasticity in the in the calf muscle there is significant positive changes occur in the muscle which causes reducing in the spasticity. Another study conducted by David Buxtor et al states that Bobath approach is said to be best way in the restoring the movement and normal muscle function when compare to theother treatment approaches in term of both cost to health service and effectiveness [17].
According to my study when bobath is applied to patient with spasticity in calf muscle among stroke patients there is significant reduced in muscle tone
According to the current study post-treatment p-value when applying the Bobath on spasticity of calf muscle is <0.01. P-value was considered significant using paired sample t-test. According to graham et al it is stated that post treatment effect of Bobath treatment. Highest amount of recovery was detected as ingrade one according to the scoring on Ashworth. Bobath approach is very efficient in cases of increased muscle tension. The modification in the effects of pre plus post treatment is statistically significant (0=0.001).
According to my study when applying the bobath to the patient with spasticity in calf muscle in stroke p value is <0.01. Which is considered as significant when used paired sample t-test.
The study shows among 30 patients 60% improvement were notice when applying the therapeutic ultrasound to the spasticity in calf muscle and 70% improvement were noted when apply neurodevelopmental technique to the spastic patient. Another study by Ayla fill et al there were significantly changes were noted when applying Bobath among 60 patients 16 cases recovery, 1 case relapse, no measurable changes in 8 cases and others have normal muscle tone. Another study by Noureddin Nakhostin et al stated that when applying the therapeutic ultrasound to the patients having spasticity reduce the muscle tone about 40% from the initial condition [22].
According to my study when applied bobath and therapeutic ultrasound to the patient with spasticity in calf muscle in stroke then bobath was consider to be more effective than therapeutic ultrasound in reducing the spasticity of calf muscle.
According to the current study tension in the tone is reducing by using therapeutic ultrasound so it is said to be efficient modalities among all. When applying the therapeutic ultrasound to the spasticity in calf muscle mean value of pre-treatment and post-treatment by using Ashworth scoring was 3.6 to 2.5. Another study by Amatya et al the effect of therapeutic ultrasound after 5-week period reduced the muscle tone with p-value pre 0.41 ± 0.19 and post 0.19 ± 0.22 and Ashworth score mean is pre is 3 and post is 2 in the stroke patients who had spasticity in planter flexion muscle group [41].
According to results of study when applied the therapeutic ultrasound to the patient with spasticity in calf muscle. Post value of therapeutic ultrasound were is 28.4 ± 4.28
The study shows that 15 participants were selected and when applying the therapeutic ultrasound to spasticity of calf muscle it reduce the muscle tone with p-value is <0.01. Another study conducted by the Ulku kerimoglu 48 patients were selected for the study and it is stated that ultrasound therapy improves the muscle tone with the p-value 0.002. Its means application of therapeutic ultrasound proved to be efficient in preventing spasticity of calf muscle [22].
According to my study 30 participant were selected in study in which bobath were applied to15 patients and therapeutic ultrasound was applied to 15 patients.
In this study participant are 10 males and 5 females with mean age of therapeutic ultrasound group is 59.1.Therapeutic applied to the to the males and females are respond similar as therapeutic ultrasound increases the range of motion and help in reducing the spasticity. Another study conducted by Alessandro Picelli he took thirty adult patients in which nineteen were male and eleven were female with mean age is 64.0 ± 9.4ages having equines spasticity on feet as complication by using therapeutic ultrasound to the participant no significant change was observed but change in 5 to 10 degree of range of motion [28].
According to my study gender of the participant for bobath is nine were male and six were female and in therapeutic ultrasound ten were male and five were females.
According to the current study range of motion which is measure by the universal goniometer. Range of motion were increase by applying the therapeutic ultrasound and Bobath. But Bobath having different range of motion and mean value. In therapeutic ultrasound range of motion is increased by mean value 2.0 to 28.4 and for Bobath approach range of motion significantly increased as 2.3 to 34.5. According to the other study conducted by Soofia Naghdi a measurement of ROM is by universal goniometer he follows standardized range of motion method. Soofia said when applying the therapeutic ultrasound to the patient with spasticity there is increase in the range of motion. With the mean value recorded as 5.6 to 35.7 degree range of motion [27].
In my study goniometer were used to assess range of motion of ankle dorsi-flexion at pre and post treatment. At pre level range of motion was in bobath is about 2 and post was 34 and in therapeutic ultrasound pre level of range of motion was 2 and post was 28 when assessed by universal baseline goniometer.
Conclusion
This study compared the effectiveness of therapeutic ultrasound and Bobath approach on spasticity among stroke patients. Based on the results it is concluded that both techniques showed significant improvement in range of motion and Ashworth scoring scale, but Bobath approach was found to be most effective in managing spasticity.
References
- Emilia Miko ajewska (2012) NDT-Bobath Method in Normalization of Muscle Tone in Post-Stroke Patient. Adv Clin Exp Med 21:513–517
- Farooq MU, Majid A, Reeves MJ, Birbeck GL (2009) The epidemiology of stroke in Pakistan: past, present, and future. Int J Stroke 4:381–389
- Gerard E Francisco, John R McGuire (2012) Post stroke Spasticity Management. Strokeaha 43:3132–3136
- Mergenthaler, Dirnagl, Meisel, Mergenthaler, Meisel (2004) Pathophysiology of Stroke. Metab Brain Dis 19:151–167
- David Burke, Jorg Wissel and Geoffrey, Donnan A (2013) Pathophysiology of spasticity in stroke. Neurology 80:20-26
- Watkins C L, Leathley M J, Gregson J M, Moore A P, Smith T L, et al. (2002) Prevalence of spasticity post stroke. Clin Rehabil 16:515
- Allison Brashear, Elie Elovic Spasticity 1st ed (2011) Spasticity Diagnosis and Management 34:161-170
- Sheean G (2002) The pathophysiology of spasticity. Eur J Neurol 182:3-9
- Allison Brashear, Elie Elovic (2011) Spasticity. 1st ed. Spasticity Diagnosis and Management 45:148-157
- Lea R D, Gerhardt J J (1995) Range-of-motion measurements. J Bone Jt Surg 77:784-798
- Emilia Miko ajewska (2012) NDT-Bobath Method in Normalization of Muscle Tone in Post-Stroke Patient. Adv Clin Exp Med 21:513–517
- Farooq MU, Majid A, Reeves MJ and Birbeck GL (2009) The epidemiology of stroke in Pakistan: past, present, and future. Int J Stroke 4:381–389
- Gerard E Francisco, John R McGuire (2012) Post stroke Spasticity Management. Strokeaha 43:3132–3136
- David Burke, Jorg Wissel and Geoffrey A Donnan (2013) Pathophysiology of spasticity in stroke. Neurology 80:20-26
- Emilia Miko ‚ajewska (2012) NDT-Bobath Method in Normalization of Muscle Tone in Post-Stroke Patient. Adv Clin Exp Med 21:513–517
- Sheila Lennon, David Baxter, Ann Ashburnce (2010) Physiotherapy based on the Bobath concept in stroke rehabilitation. Disabil Rehabil 23:254-262
- Kenneth Monaghan, Frances Hogan, Catherine Blake, Catherine Cornell, Paula PM Hickey, et al. (2011) Physical treatment interventions for managing spasticity after stroke. Cochrane Database Syst Rev 6:48-56
- Ansari NN, Naghdi S (2017) The effect of bobath approach on the excitability of the spinal motor neurons in stroke patients with muscle spasticity. Electromyogr Clin Neurophysiol 47:29-36
- Charlene Butler, Johanna Darra (2001) Effects of neurodevelopmental treatment (NDT) for cerebral palsy. Dev Med Child Neurol 11:778-790
- Dianne B, Cherry (1998) Review of Physical Therapy Alternatives for Reducing Muscle Contracture. Cleveland OH 60:877–881
- Ayla Fil, Kadriye Armutlu, Ahmet Ozgur Atay, Ulku Kerimoglu, Bulent Elibol (2011) The effect of electrical stimulation in combination with Bobath techniques in the prevention of spasticity in acute stroke patients. Clin Rehabil 25:51–59
- Susan Ronan, Joan T Gold (2007) Non operative management of spasticity in children. Childs Nerv Syst 23:943–95
- Sheila Lennon (2001) Gait re-education based on the bobath concept. Phys Ther 81:924-935
- M Abo, Y Sase, S Watanabe, W Kakuda, K Taguchi, T Takekawa, et al. (2013) Neuro rehabilitation home based functional training in post stroke patients. Journal of the Neurological Sciences 16:537-578
- Sheila Lennon (1996) Bobath concept: a critical review of the theoretical assumptions that guide physiotherapy practice in stroke rehabilitation 1:35-45
- Noureddin Nakhostin Ansari, Soofia Naghdi, Scott Hasson,Maryam Rastgoo (2009) Efficacy of therapeutic ultrasound and infrared in the management of muscle spasticity. Informa healthcare 23:632–638
- Smania N, picelli dA, Munari, Geroin C, ianes P, et al. (2010) Rehabilitation procedures in management of the spasticity. Eur j phys rehabil med 46:423-38
- Ansari NN, Adelmanesh, naghdi S, tabtaaei A (2006) The effect of physiotherapeutic ultrasound on muscle spasticity in pateint with hemiplegia. Electrography and clinical neurophysiology 46:247-252
- Ansari NN, Naghdi S, Bagheri H, Ghassabi H (2007) Therapeutic ultrasound in the treatment of ankle planter flexion spasticity in unilateral stroke population. Clin Neurophysiol 47:137-143
- Sahin, Nilay, Ugurlu, Hatice, Karahan, et al. (2011) Efficacy of therapeutic ultrasound in the treatment of spasticity. Neuro rehabilitation 14:61-66
- Jean Michel Gracies (2001) Physical modalities other than stretch in spastic hypertonia. Elsevier journal 48:769-792
- Alessandro Picelli, Francesca Dambruoso, Manoj Bronzato, Martina Barausse, Marialuisa Gandolfi, et al.(2015) Efficacy of therapeutic ultrasound and transcutaneous electrical nerve stimulation compared with botulinum toxin type A in the treatment of spastic equines in adult with chronic stroke. Stroke Rehabil 21:8-16
- Thomas watanabe (2004) The role of therapy in spastic management. Am J Phys Med Rehabil 83:45-49
- Bobath Berta (1948) The importance of the reduction of muscle tone and the control of mass reflex action in the treatment of spasticity. J Occup Rehabil 5:371-383
- Richardson D (2002) Physical therapy in spasticity. Eur J Neurol 1:17-22
- Eileen g fowler, Teresa w Ho, Azuka I Nwigwe, Fredrick j Dorey (2001) The effect of quadriceps femoris muscle strengthening exercise on spasticity in children with cerebral palsy. J Phys Ther 6:1215-1223
- A Speed (2001) Therapeutic ultrasound in soft tissue lesions. J Rheumatol 4:1331-1336
- Pippa shanks, Michel curran, Paul fletcher, Richard Thompson (2010) The effectiveness of therapeutic ultrasound for musculoskeletal conditions of lower limb. Elsevier sci 4:133-139
- Antonio naro, Antonio leo, Margherita russo, Carmela casella, Antonio buda, et al. (2017) Breakthroughs in the spasticity management: are non-pharmacological treatments. J Clin Neurosci 39:16-27
- Amatya B, Khan F, La Mantia L, Demetrios M, Wade DT (2013) Non pharmacological interventions for spasticity in multiple sclerosis. The Cochrane Library 2:23-29
- Julie Vaughan Graham, Catherine Eustace, Kim Brock, Elizabeth Swain, and Sheena Irwin-Carruthers (2009) The Bobath Concept in Contemporary Clinical Practice. Stroke Rehabil 1:853-868
- Amir H Bakhtiary, Elham Fatemy (2008) Does electrical stimulation reduce spasticity after stroke? A randomized controlled study. Clin Rehabil 22:818-825
- Sue Raine (2006) The defining the bobath concept using the Delphi technique. Physiother Res Int 1: 4-13
- Albert t, Yelnik A (2003) physiotherapy for spasticity. Neurochir 49:239-246
- Younan Zhang, Ann Marie Chapman, Melanie Plested, Daniel Jackson, Francis copurroy (2012) The Incidence, Prevalence and Mortality of Stroke in France, Germany, Italy, Spain, the UK, and the US: A Literature Review. Stroke Res Treat 43:11-24
- Belagaje SR, Lindsell C, Moomaw CJ, Alwell K, Flaherty M, et al. (2014) The Adverse Effect of Spasticity on 3-Month Poststroke Outcome Using a Population-Based Model. Stroke Res Treat 69:60-89
- Bruce Ovbiagele, Steve Kautz, Wayne Feng, De AnnaL Adkins (2014) Post stroke outcomes. Stroke Res Treat 35:82-84
- Ismail Setyopranoto, Halwan Fuad Bayuangga, Andre Stefanus Pangga bean, Sarastiti Alifaningdyah, Lutfan Lazuardi, et al. (2019) Prevalence of Stroke and Associated Risk Factors in Sleman District of Yogyakarta Special Region, Indonesia. Stroke Res Treat 26:42-45
- Thibaut A,Chatelle C,Ziegler E,Bruno MA,Laureys S, et al. (2013) Spasticity after stroke: physiology, assessment and treatment. Brain Inj 27:93-105
- Meseguer Henarejos AB, Sanchez Meca J, Lopez Pina JA, Carles Hernandez R (2018) Inter and intra-rater reliability of the Modified Ashworth Scale: a systematic review and meta-analysis. Eur J Phys Rehabil 54:576-590
- Elveru RA, Rothstein JM, Lamb RL (1998) Goniometric reliability in a clinical setting. Subtalar and ankle joint measurements J Physm Ther 68:672-677
- Ward AB A literature reviewof the pathophysiology and onset of post-stroke spasticity. Eur J Neurol 2012; 19: 21-27
- Kim DH1, An DH2, Yoo WG (2018) Validity and reliability of ankle dorsi flexion measures in children. J Back Musculo skeleton Rehabilitation 31:465-468
- Michiel L Bots, Sophia J, LoomanPeter J, Koudstaal Albert Hofman (1996) Prevalence of stroke in general population. Home stroke 27: 1488-1501
- Noureddin nakhostin ansari, Soofia naghdi, Scott hasson, Maryam rastgoo (2009) Efficacy of therapeutic ultrasound and infrared in the management of muscle spasticity. Inform a healthcare 23:632–638
- Bente e bassoe Gjelsvik (2008) The bobath concept in adult neurology. 1st ed. Bobath handling. Germany 25:116-122
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences