Coarse and Zealous-Keloid
Anubha Bajaj*
Department of Histopathology, A. B. Diagnostics, A-1, Rajouri Garden, New Delhi (110027), India
- *Corresponding Author:
- Anubha
Bajaj
Consultant Histopathologist,
A. B. Diagnostics, A-1, Rajouri Garden,
New Delhi (110027),
India,
Tel No: 00911141446785
E-mail: anubha.bajaj@gmail.com
Received Date: November 12, 2021; Accepted Date: November 26, 2021; Published Date: December 03, 2021
Citation: Bajaj A (2021) Coarse and Zealous- Keloid. J Med Oncol Vol.4 No.5: 07.
Abstract
Keloid is denominated as a benign, fibro-proliferative neoplasm arising due to anomalous wound healing or a fibroblastic connective tissue reaction to diverse contributory factors such as surgical intervention, burns, trauma, inflammation, foreign body reaction or endocrine dysfunction. Occasionally, keloid may occur spontaneously. As keloid emerges due to aberrant wound healing, in contrast to stages of normal wound healing, keloid demonstrates a prolonged fibroblastic phase with unchecked fibroblastic proliferation. Scars with keloid are benign and mandate therapy due to relief of clinical symptoms or cosmetic concerns. Although multiple therapeutic modalities are adopted, a singular, optimal treatment option for alleviating keloid remains an enigma.
Keywords
Benign tumor; Keloid; Skin scar
Introduction
Disease characteristics
Keloid emerges as a benign, dermal growth appearing due to preceding cutaneous trauma or inflammation. Lesions arise within one month to up to one year following initial cutaneous injury which may be insignificant. Spontaneous lesions may appear [1,2]. Although no site of lesion emergence is exempt, keloid commonly arises upon sites of enhanced cutaneous tension such as earlobe, neck, jaw, shoulder, deltoid, presternal thoracic region or upper dorsal region. Infrequently, keloid may emerge upon the eyelids, genitalia, palms or soles. Keloid is engendered due to diverse genetic or environmental factors. African population demonstrates an ethnic predilection wherein Blacks appear predisposed to configuration of keloid. Dark skinned individuals of African, Asian or Hispanic origin demonstrate an enhanced incidence of keloid [1,2]. Overactive fibroblasts generate significant collagen and growth factors which consequently engender enlarged, anomalous, hyalinised fascicles of collagen. Aforesaid fascicles of collagen fibers are designated as “keloidal collagen” and admixed with innumerable fibroblasts [1,2]. Commonly, keloid emerges in predisposed individuals following cutaneous trauma such as surgical intervention, body piercing, acne, tattooing, insect bites, burns, lacerations, abrasions, vaccinations, infected skin lesions or procedures initiating cutaneous inflammation.
De novo lesions are infrequent. Elevated cutaneous tension within a wound contributes to configuration of keloid. Incidence of keloid is significantly enhanced during pregnancy and puberty. Family history of keloid is associated with enhanced possibility of keloid emergence although a specific gene responsible for occurrence of keloid remains to be identified. Exceptional genetic syndromes may elevate possible appearance of keloid such as Rubinstein-taybi syndrome or Goeminne syndrome [1,2].
Literature Review
Keloidal fibroblasts demonstrate enhanced proliferative activity, persist for significant duration and depict minimal apoptosis. Consequently, excessive secretion of cytokines and configuration of collagen ensues. Collagen synthesis within keloid is approximately twenty times than collagen synthesis observed within healthy skin and three times than a hypertrophic scar [1,2]. Preponderantly, Transforming Growth Factor-β (TGF-β) and Platelet Derived Growth Factor (PDGF) contribute to configuration of keloid. Transforming growth factor-β is an integral constituent of wound healing and cytokines promote chemotaxis of fibroblasts towards site of inflammation in order to articulate collagen. Dysregulation of aforesaid pathway initiates fibrosis and an anomalous scar response [3,4].
Clinical elucidation
Keloid represents as a firm, rubbery nodule which frequently projects beyond subjacent stratified squamous epithelial layer. Lesions depict a narrow base, arise as pedunculated lesions or may demonstrate broad-based plaques [3,4]. Keloid appears as an erythematous, flesh-coloured or hyper-pigmented nodule wherein the countenance may alter with evolution of lesion. Although asymptomatic, keloid can frequently engender pruritus and tenderness. Occasionally, keloid may be painful. Keloid is an infiltrative lesion associated with a localized tissue reaction accompanied by pain and inflammation. The essentially benign lesions are frequently symptomatic and may exhibit pruritus or pain. Tenderness or burning may ensue. Keloid may enlarge and is associated with significant cosmetic disfiguration [3,4]. Clinically, keloid represents as a firm, rubbery nodule within an area of preceding cutaneous injury. Keloid frequently expands beyond the site of initial cutaneous trauma. The lesion is associated with pain, itching or burning. Appropriate clinical examination is optimal for evaluation of keloid. Cogent tissue sampling with relevant immunohistochemistry is warranted for assessing lesions with a controversial diagnosis. Additional evaluation is usually unnecessary [3,4].
Histological elucidation
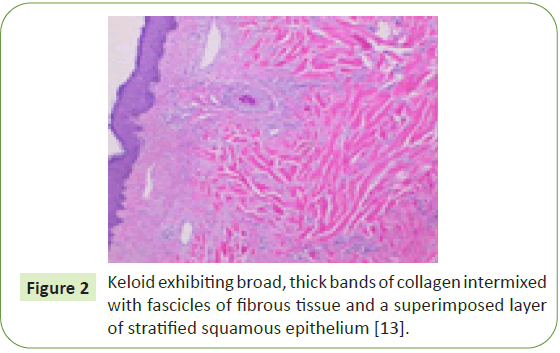
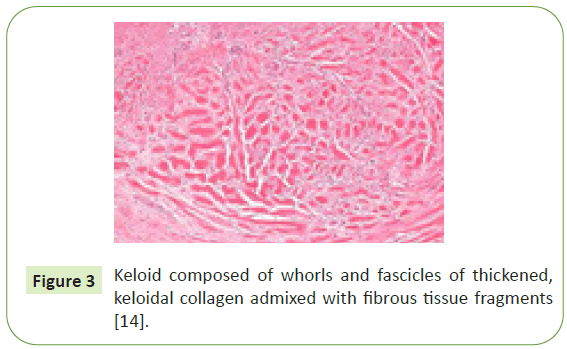
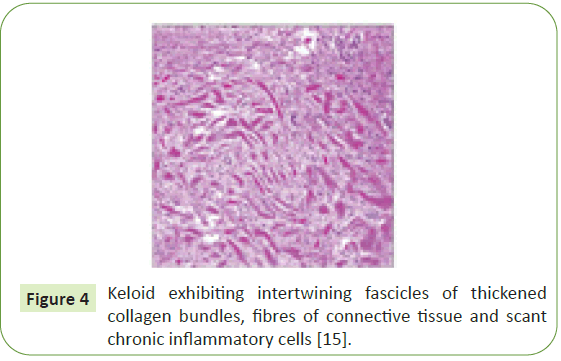
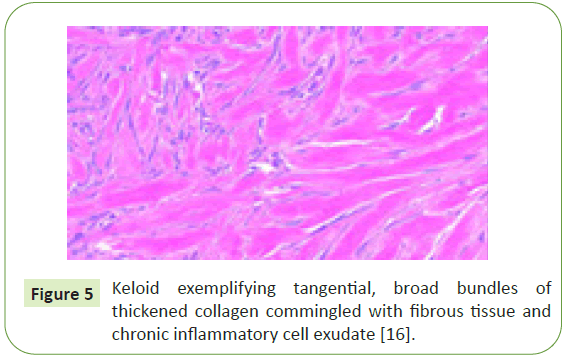
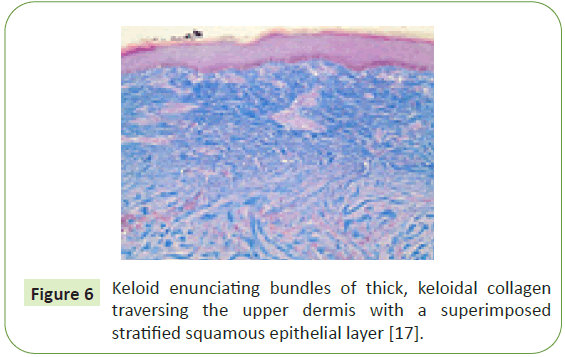
Upon microscopy, broad bands of collagen are discerned which are composed of enlarged, brightly eosinophilic, glassy collagen fibres. Disseminated fibroblasts appear as arranged parallel to superimposed cutaneous surface and are admixed with myofibroblasts. Intralesional injectable corticosteroids induce accumulation of mucinous pools within the lesion. Characteristically, keloid demonstrates innumerable whorls of thickened, hyalinised fascicles of collagen denominated as keloidal collagen. Additionally, keloid is associated with an acanthotic superimposed stratified squamous epithelial layer, an unremarkable papillary dermis, “tongue-like” progressive edges of epithelium extending beneath the papillary dermis, horizontally articulated fibrous bands confined to upper reticular dermis and prominent fascia-like collagenous bands confined to deep-seated dermis. Upon cytogenetic analysis, epigenetic alterations are observed within Deoxyribonucleic Acid (DNA) of fibroblasts which are accompanied by acetylation of histone proteins [5,6].
Differential diagnosis
Keloid requires segregation from conditions such as:
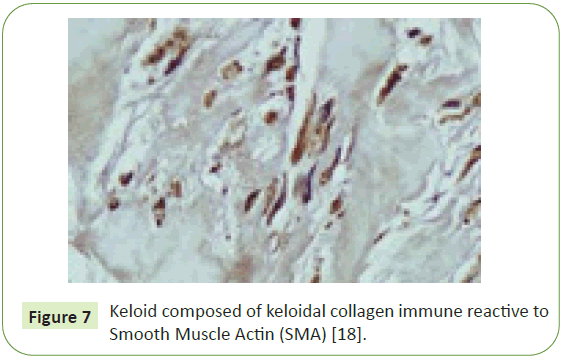
• Hypertrophic scar which simulates a keloid and commonly occurs subsequent to cutaneous trauma. Hypertrophic scar is a miniature lesion usually confined to specific zones of cutaneous injury. Hypertrophic scar usually lacks projection above subjacent cutaneous surface or extension beyond initial site of injury [5,6]. Hypertrophic scar is composed of enhanced quantity of fibroblasts admixed with thickened collagen bundles arranged parallel to superimposed cutaneous surface. Vascular articulations appear oriented vertically. Hypertrophic scar is devoid of keloidal collagen. However, immunoreactivity to smooth muscle actin (SMA) is an inaccurate methodology for demarcating hypertrophic scar from keloid.Cogent tissue biopsy can segregate the lesions [6,7].
• Dermatofibroma emerges as an aberrant scar reaction. Typically, a flesh-coloured or hyper-pigmented papule or nodule is discerned. Clinically, a centric depression is observed during the application of lateral pressure, denominated as “dimple sign” [6,7].
• Dermatofibrosarcoma protuberans is an exceptional, locally aggressive neoplasm composed of spindle-shaped cells and an irregular tumor perimeter. Tumefaction commonly arises upon the trunk or proximal extremities. Generally, young adults are incriminated. Lesions of dermatofibrosarcoma protuberans are devoid of preceding trauma [6,7].
• Morphea and scleroderma emerge as a progressive disease in the absence of a specific, inciting factor. Clinical signs of associated connective tissue diseases may ensue [6,7].
• Xanthoma disseminatum is an exceptional disorder of histiocytic proliferation associated with cutaneous lesions simulating keloid. An acute emergence of disseminated lesions display a diffuse, symmetric configuration. Diabetes insipidus may ensue due to systemic involvement [6,7].
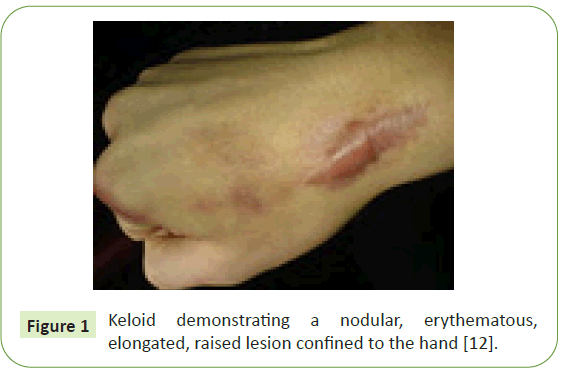
• Lobomycosis is a deep-seated fungal infection engendered by organism Lacazia loboi. Lesions manifest as a gradually progressive, keloid-like nodule commonly emerging upon distal extremities. The fungal infection occurs due to exposure to dolphins or rural soil and especially emerges within Central and South America. Additionally, keloid requires a distinction from conditions such as complicated acne or keloidal dermatofibroma (Figures 1-7) [6,7].
Figure 1: Keloid demonstrating a nodular, erythematous, elongated, raised lesion confined to the hand [12].
Figure 2: Keloid exhibiting broad, thick bands of collagen intermixed with fascicles of fibrous tissue and a superimposed layer of stratified squamous epithelium [13].
Figure 3: Keloid composed of whorls and fascicles of thickened, keloidal collagen admixed with fibrous tissue fragments [14].
Figure 5: Keloid exemplifying tangential, broad bundles of thickened collagen commingled with fibrous tissue and chronic inflammatory cell exudate [16].
Figure 6: Keloid enunciating bundles of thick, keloidal collagen traversing the upper dermis with a superimposed stratified squamous epithelial layer [17].
Figure 7: Keloid composed of keloidal collagen immune reactive to Smooth Muscle Actin (SMA) [18].
Discussion
Therapeutic options
Besides being challenging to treat, inadequate therapy of keloid may ensure worsening and progression of lesion. Therefore, primary prevention is optimal and recommended. Predisposed individuals require circumvention of elective surgical procedures as ear piercing or tattooing. Multiple therapeutic sessions are required irrespective of treatment modality adopted. Besides, retrogression of keloid may not be comprehensive or uniform. Surgical intervention for accidental trauma necessitates minimizing of cutaneous wound tension, rapid primary closure and adequate haemostasis as exemplified in tension-free wound closure [8,9].
Prolonged wound stabilization with the employment of silicone sheeting decimates wound tension. Compression therapy with pressures of 15 millimeters to 45 millimeters of mercury (Hg) adopted for a duration exceeding >23 hours per day for minimally a period of 6 months is recommended for decimation of keloid configuration [8,9]. Several therapeutic agents can be employed to alleviate clinical symptoms of pre-existing keloids. Common therapeutic manoeuvers for treating keloid are intralesional or topical steroids, cryotherapy, surgical extermination of the lesion, radiotherapy or laser therapy. Intralesional steroids can be utilized singularly or in combination with diverse treatment strategies. Topical ointments and steroid impregnated tapes are employed to decimate clinical symptoms such as pruritus and burning. Cryotherapy requires adoption of multiple treatment cycles although is associated with post-treatment pigmentary alterations. Laser therapy is employed in order to induce flattening and retrogression of keloids [10,11].
Keloid can be appropriately managed with comprehensive surgical eradication. Keloid frequently reoccurs following cogent surgical resection. On account of enhanced proportion of lesion reoccurrence following surgical extermination, combination with adjuvant therapies such as post-surgical radiation or intralesional injectable steroids is recommended. Radiotherapy for treating keloids is indicated in instances with enlarged lesions, unfavourable site of lesion occurrence or reoccurrence following pertinent surgical resection and marginal or incomplete surgical excision. Post-Operative Radiotherapy (PORT) or adjuvant radiotherapy for treating keloids can be initiated within 24 hours of surgical resection. Generally, field of radiotherapy requires inclusion of the scar and one centimetre wide perimeter of soft tissue. Circumvention of radiotherapy in subjects below <18 years or radiotherapy of susceptible areas as the head and neck or breast is mandated on account of an inherent, possible occurrence of carcinogenesis [12-18].
Conclusion
Keloids subjected to radiotherapy can display hyperpigmentation, pruritus or erythema. Emergence of malignant neoplasms following radiotherapy for keloids is extremely exceptional. Typically, following postoperative radiotherapy, reappearance of keloid appears in an estimated 10% to 35% instances contingent to aetiology, magnitude and location of lesion, extent of surgical resection and associated factors. Adoption of radiotherapy for keloid emerging in young subjects or lesions arising in the chest or breast tissue of young females warrant serious deliberation.
Additional efficacious modalities for treating keloid appear as application of topical imiquimod following surgical excision, injectable corticosteroids, fluorouracil or verapamil, pressure earrings, intralesional injectable botox, intralesional bleomycin, intralesional 5-fluorouracil or silicone gel sheeting. Aforesaid therapeutic methodologies can be adopted singularly or in combination.
References
- McGinty S, Siddiqui WJ (2021) Keloid. StatPearls [Internet].
- Huang C, Liu L, You Z, Du Y, Ogawa R (2019) Managing keloid scars: From radiation therapy to actual and potential drug deliveries. Int Wound J 16: 852-859.
- Wang M, Chen L, Huang W, Jin M, Wang Q, et al. (2019) Improving the anti-keloid outcomes through liposomes loading paclitaxel–cholesterol complexes. Int J Nanomedicine 14: 1385.
- O’Boyle CP, Shayan-Arani H, Hamada MW (2017) Intralesional cryotherapy for hypertrophic scars and keloids: A review. Scars, burns & healing. 3: 2059513117702162.
- Lee YI, Kim J, Yang CE, Hong JW, Lee WJ, et al. (2019) Combined therapeutic strategies for keloid treatment. Dermatol Surg 45: 802-810.
- Palko JR, Arfeen S, Farooq AV, Reppa C, Harocopos GJ (2019) Corneal keloid presenting forty years after penetrating injury: Case report and literature review. Surv Ophthalmol 64: 700-706.
- Kang S, Hur JK, Kim D (2019) Advances in diagnostic methods for keloids and biomarker-targeted fluorescent probes. Analyst 144: 1866-1875.
- Chen Y, Chen Y, Liu Y (2019) Abnormal presentation of aggressive fibromatosis after radiotherapy for keloids: Case report and brief literature review. Ann Plas Surg 83: 104-107.
- Lei R, Shen J, Zhang S, Liu A, Chen X, et al. (2019) Inactivating the ubiquitin ligase Parkin suppresses cell proliferation and induces apoptosis in human keloids. J Cell Physiol 234: 16601-16608.
- Coentro JQ, Pugliese E, Hanley G, Raghunath M, Zeugolis DI (2019) Current and upcoming therapies to modulate skin scarring and fibrosis. Adv Drug Deliv Rev 146: 37-59.
- Greywal T, Krakowski AC (2018) Pediatric dermatology procedures and pearls: Multimodal revision of earlobe keloids. Pediatr Dermatol 35: 268-270.
- Poetschke J, Gauglitz GG, et al. (2016) Current options for the treatment of pathological scarring. JDDG 14: 467-477.
- Shanmugaratnam K (2012) Histological typing of tumours of the upper respiratory tract and ear. SSBM.
- Lee JY, Yang CC, Chao SC, Wong TW (2004) Histopathological differential diagnosis of keloid and hypertrophic scar. Am J Dermatopathol 26: 379-384.
- Rekhtman N, Baine MK, Bishop JA (2019) It looks like what? an illustrated glossary of histopathologic descriptors. InQuick Reference Handbook for Surgical Pathologists 165-188.
- Mills SE, Carter D, Greenson JK, Reuter VE, Stoler MH (2012) Sternberg's diagnostic surgical pathology. LWW.
- Carter K, Rutherford M (2020) Building a Medical Terminology Foundation.
- Santucci M, Borgognoni L, Reali UM, Gabbiani G (2001) Keloids and hypertrophic scars of Caucasians show distinctive morphologic and immunophenotypic profiles. Virchows Arch 438: 457-463.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences