Additive Manufacturing for Economical, User-Accessible Upper-limb Prosthetics
Collin Baker, Denikka Brent, Charles Wilson, Jiajun Xu and Lara A Thompson*
University of the District of Columbia, School of Engineering and Applied Sciences, Department of Mechanical Engineering, Washington DC, United States
- *Corresponding Author:
- Lara A Thompson
University of the District of Columbia, School of Engineering and Applied Sciences
Department of Mechanical Engineering, Washington DC, United States
Tel: (202) 274-5046
E-mail: lara.thompson@udc.edu
Received date: January 18, 2017; Accepted date: April 21, 2017; Published date: April 27, 2017
Citation: Baker C, Brent D, Wilson C, Xu J, Thompson LA (2017) Additive Manufacturing for Economical, User-accessible Upper-limb Prosthetics. Pro Ort Open J 1:8.
Copyright: © 2017 Baker C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: The purpose of this paper is to briefly describe the initial stages of our efforts towards the development of easy to manufacture, low-cost, three-dimensional (3D) printed prosthetics. Specifically, here we describe the design of an upper-limb prosthetic for youths. When private insurance and public funding are insufficient, financial resources are limiting factors in obtaining quality prosthetics for the amputee. The need for cost-effective, economical solutions for prosthetics is particularly important for children in that they frequently outgrow them and costs are prohibitively expensive. Thus, 3D printed prosthetics may pose as a potential solution. In parallel to the above objective, additive manufacturing (or three-dimensional (3D) printing) knowledge and training, within the rapidly growing field of Biomedical Engineering (or BME), is becoming increasingly important in that it may provide solutions for numerous medicallyrelated applications. As such, it is imperative that 3D printing exposure be incorporated, for research-based, as well as experiential project-based, contexts.
Methods: Well-known mechanical design processes and quality function deployment were implemented here to design a prosthetic that could aid youths suffering from upper-limb loss. Computer-generated designs were used to in conjunction with a Cubify 3D printer to create the prosthetic hand components.
Results: A simple, accessible, affordable design for an upper-limb was assembled that costed only $25.
Conclusions: In the near-future, commercially available 3D printers may make developing one’s own prosthetics an easy to accomplish task within their home environment. In essence, this process would create a tighter coupling between how a product is conceived, developed,
Keywords
Additive manufacturing; Prosthetics; 3D printing; Upper-limb; Amputee.
Introduction
The need for life-like, upper-limb prosthetics for children
Approximately 1.9 million individuals in the United States are currently living with limb loss [1], with veterans and children being the leading recipients of prosthetics. In the United States, approximately 32,500 children have undergone major amputations and 1,500 children are born with upper-limb reductions. As opposed to disease, upper-limb amputations are typically due to a traumatic event, in that upper-limb amputations account for 69% of trauma-related amputations and 58% of congenital amputations [2-4]. Lower-limb amputations account for 82% of limb-loss and are typically related to vascular diseases (e.g., having a defective blood supply due to diabetes). The diabetic population accounts for approximately 80,000 amputations performed yearly and those who have already had one amputation are 28 to 51% more likely to have a second amputation within five years following their initial amputation [5,6]. Although limb loss affects various populations (e.g., veterans, diabetic patients, and children), the development of prosthetics for children and young adults is especially important.
Due to their rapid growth, children and youths require multiple prosthetics. When an adult is fitted with a prosthetic, growth patterns are relatively unchanging and only infrequent adjustments are required. However, for a growing child, the dimensions of a prosthetic requires near constant adjustment. Children 1-5 years of age need a new prosthetic each year, children 5-12 years old require a new prosthetic every 1-2 years, and adolescents to young adults (i.e., individuals aged 12-21 years old) must be fitted for a new prosthetic every 3-4 years [7]. The cost of un-powered, upper-limb prosthetics range from $4,000-$20,000 [2]. Due to the high cost of prosthetics, and the rate at which children, adolescents, teenagers, and young adults outgrow them, economical and accessible prosthetics are needed. Because the frequent need for newly-fitted prosthetics are required for children and young adults, “low-tech” hooks with a basic grasping mechanism are typically suggested for usage, however, these come with major limitations [8,9]. In particular, the hook mechanism is not aesthetic, nor life-like, and therefore unappealing to the end-user (amputee). Although the hook may provide the child with (some) added functionality, they will not use the mechanism. Over the past 2.5 decades, rejection of all prosthetics was observed in approximately 1 of every 5 individuals with upper limb deficiency [9]. However, we speculate that this number may in fact be even higher when limited to solely the child and youth population. Children often times would rather expose their amputated limb than wear their prosthetic, and there are only few designs that incorporate the aesthetic aspect. Despite the increased functionality when using the prosthetic, previous studies have shown that as many as half of children fitted with prosthetics would chose to not wear their prosthetics due to cosmetic reasons and in order achieve social integration [10,11]. Therefore, consideration of acceptance or rejection when fitting individuals with prosthetics is of utmost importance. Children, adolescents, and young adults, are developing psychosocially (as well as physically) and are faced with the desire to have acceptance from their peers. Thus, the willingness of the amputee to use their prosthetic device is something to be especially mindful of when designing a prosthetic limb.
Residual limb capture versus (new) additive manufacturing techniques
A common method of fitting a residual limb for a prosthetic involves a negative-plaster casting by a medical professional [12]. While the cast is drying, pressure is applied in specific areas to ensure correct load points. The negative cast is then used to create a positive cast that is formed typically using thermoforming styrene or a polyurethane liner that is then joined with the remainder of the prosthetic. However, additive manufacturing (described below) reduces the human interaction that had been previously needed for the development of, for example, casted prosthetics.
Additive manufacturing (a process by which digital 3D data is used to print a component by material deposition layer by layer) offers the creation of prosthetic components that would counteract some of the hurdles that youth, upper-limb amputees encounter (e.g., costs, the frequent need for newlysized prosthetics, and the desire to have functional/realistic prosthetics). Computer-aided design (CAD) programs, additive manufacturing (or three-dimensional (3D) printing), and image software may offer an economical and accessible solution. More recently, integration of Magnetic Resonance Imaging (MRI) and Computer Tomography (CT) has been used to build a model of the amputee’s stump [13]. Further, laser scanners can document (limb) contours and render them in a CAD program. These technologies can be implemented to compliment 3D printing. Editing image programs (e.g., ImageJ) can be used to assess dimensions (e.g., hand length, palm width, and forearm length). Further, Maker Ware software can be used to scale the prosthetic to the desired size [2].
Affordable prosthetic devices would broadly impact all amputees’ quality of life, regardless of their socioeconomic conditions. The resizing costs (due to the youth outgrowing the prosthetic) are reduced using 3D printing as opposed to methods previously used. Prosthetics that utilize a basic mechanical grasping mechanism are commercially available at a minimum cost of $4,000. The high costs of electric-powered and body-powered prosthetic hands make them inaccessible to children from low-income, uninsured families, within the United States, as well as those living within developing countries. However, 3D printing allows for a cost that is markedly less (e.g., previously designed Raptor, Talon, and Cyborg Beast are ~ $35- $50). Further, entry-level 3D printers are now similar in price point to laser printers, when they had become desktop fixtures, and prices on high-end machines are dropping.
Three-dimensional printed prosthetics can be more readily aesthetically designed than previous methods. Open Bionics Incorporated utilizes 3D printing to create superhero-inspired prosthetic upper-limbs for children (e.g., with concepts from Iron Man, Frozen, and Star Wars) [14]. These designs evoke a positive feeling of confidence, empowerment and independence in young amputees while using their prosthetic limb. Another innovative approach is the use of Legos to personalize designs [15]. Children can personalize their arm with Legos while having a fun, unique design that is personal to them. Further, Nike has created prosthetic aesthetic designs that may appeal, in particular, to children with an interest in sports. These above approaches take into account aesthetics, as well as functionality, and propose a solution that will encourage and facilitate children’s acceptance and use of prosthetics.
Excellent, 3D printing open-source designs are available to the online community via “Enable”. The users then have the capacity to implement minor changes to prosthetic designs and use their 3D printers to print (manufacture) their designs. Printing one’s own prosthetics will have major effects in terms of the nature of design in that it increases the interactions between design and production, and it will radically localize manufacturing of one’s own prosthetic [16]. Further, online community forums allow users to remotely connect with others from across the globe. Because the designs are digital, they can be sent via the Internet to the user’s location, where he/she can then print it. Thus, designing and printing of devices can happen in locations, remote to one another worldwide.
Here, our short-term goal was to show that one can design and print their own prosthetic. In our proof-of-concept work, our main objective was to use a commercially available 3D printer to fabricate an affordable upper-limb prosthetic. A longer-term goal is to further iterate on our current design and obtain end-user feedback via surveys. We also aim to investigate the notion that when the end-user takes part in designing their own prosthetic, this encourages independence in amputees, specifically, the ability to accomplish a prosthetic design in one’s home environment.
The need for additive manufacturing experiential learning in Biomedical Engineering contexts
In parallel with improving quality of life of amputees and broadening societal knowledge of 3D printing for prosthetics, educational, as well as research-related, exposure to additive manufacturing of biomedical devices is critical to enhancing the Biomedical Engineering workforce. The University of the District of Columbia (UDC) is a historically black college and university (HBCU), and the only public institute of higher education within the District of Columbia. Although HBCUs comprise a minute number of colleges and universities nationwide (slightly over 2%), they have led in awarding baccalaureate degrees to African American students in the life sciences, physical sciences mathematics, and engineering. HBCUs award 33.3% of bachelor degrees in science and engineering to African Americans [17]. Of approximately 100 HBCUs across the United States, UDC is only 1 of 3 HBCUs to offer a distinctive Bachelor of Science in BME degree [2]. At UDC, new courses, activities, research facilities and experiential design projects, such as the one discussed here, have emerged.
The UDC BME program is targeted towards rehabilitation engineering, specifically aimed at the assistance of individuals with mobility-related impairments. A newly renovated Biomedical Engineering research laboratory (the Center for Biomechanical & Rehabilitation Engineering, CBRE) focuses on human postural control/mobility and assistive devices to aid individuals, such as amputees, discussed here. Further, our new Additive Manufacturing Laboratory will be used to create various devices (e.g., to assist impaired individuals). Aside from plastic 3D printers, the lab will also soon be furnished with an EOS metal-based 3D printer. To the best of our knowledge, UDC will be the only HBCU nationwide that will own such a printer, enhancing our future capacity to produce metal-based prostheses, implants, and devices for both research and education purposes. A novel and unique aspect to the activities described within our paper, is that we are using additive manufacturing for education, as well as research-infrastructure building, within an HBCU-setting.
In our paper, we describe our initial works towards in-house design of a plastic, 3D printed upper limb prosthetic which overlaps both our BME and Additive Manufacturing initiatives. We are targeted at exposing and cultivating students towards cutting-edge equipment, resources, and techniques, for Biomedical Engineering and beyond.
Methods
Design of 3D printed upper-limb prosthetic
At UDC we designed and manufactured a 3D printed upperlimb prosthetic. We utilized the mechanical design process as shown in [18]. Specifically, we first identified our end-users, generated customers’ requirements, evaluated competition, and generated engineering specifications.
Customers for our design project were children requiring upper limb prosthetics. A child can rapidly outgrow their prosthetic. Thus, having access to a design that can be scaled up to accommodate their growth and printed at low cost was deemed desirable. In regard to customer requirements, we decided to research scholarly articles that examined youth opinions of their prosthetics, and crafted a survey to be administered to amputees. UDC is located near many medical research labs, such as the Walter Reed Hospital and the MedStar National Rehabilitation Hospital.
Although it will not be discussed further here, the scope of our future work is to utilize surveys on amputees to assess their needs, including how acceptable the aesthetics of the patient’s current prosthetic are, what tasks they commonly use their prosthetic for, and how comfort plays a role in use of their prosthetic (or nonuse). In terms of evaluation of the competition, prosthetics that utilize a basic mechanical grasping mechanism are commercially available cost at least $4000, but can range much higher, 3D printing allows for cost to be nearly two magnitudes less than this amount. Further, ease of resizing, due to patient growth, further enhances cost savings for the targeted children and youth end-users.
Engineering specifications for our design were generated using a Quality Function Deployment (QFD) approach [18]. In this approach, a list of desirable attributes (e.g., mechanical grasping ability, low cost, aesthetics, fast print time, and ease of assembly) were weighted based on importance, along with the specifications to meet desirables (e.g., motion similar to natural motions, total cost less than $30, life-like aesthetic, printable in less than 1 day, and fewer number of parts required) were incorporated.
A weighted scale of 1, 3, and 9 (corresponding to a weak, moderate, and strong correlation) was then marked in the chart to observe how each engineering specification related to the desirable criteria. The result of this process indicated that we placed design emphasis on the grasping-mechanism motion and low cost (a cost under $30 would be cheaper than current Enable models).
This project focused on 3D printed prosthetics of the variety that are available to the Enable community [19]. Enable allows users to download the stl files for free in order to 3D print the designs. Typically, in 3D printing, a computer-generated design of a component is first created. This file was then uploaded for printing such the material was deposited, horizontally, line- byline, to build the prosthetic from the bottom up.
Printing was conducted in the UDC Additive Manufacturing Laboratory in Building 32, equipped with three, 3D printers: a powder printer, a medium sized plastic printer (Cubify, 3DSystems, Inc.), and a small plastic printer (Cubify, 3DSystems, Inc.).
The powder printer designed by 3D Systems uses a bed system that layers glue into the shape of the design. This system is good for demonstration purposes, however, the deposited material tends to be brittle. The two, plastic printers made by Cubify use acrylonitrile butadiene styrene (or ABS) and polylactic acid (or PLA).
As stated above, an EOS metal-based 3D printer is currently being acquired for the Additive Manufacturing lab, but is unavailable at present. Further, nylon would be a desirable material to print with due to its low cost, relatively low melting point, and high tensile strength. At this stage of the project, we were more focused on proof-of-concept, but would have explored Nylon as an option had the resources been available.
At the present time, only printers capable of printing either ABS (Acrylonitrile butadiene styrene) or PLA (Polylactic acid) plastics could be used. PLA has a higher density, tensile strength, and slightly lower cost compared to ABS. However, due to materials available in the lab both ABS and PLA were utilized in this project.
There are a few other positive and negative material qualities to note of ABS and PLA. ABS can absorb water from humidity in the air that can cause prints to vary slightly (e.g., on high versus low humidity days). PLA is slightly stronger and stands up well to post-processing via sandpaper to smooth edges. Although ABS can be sanded, smaller parts run the risk of disintegrating. However, acetone can be used on ABS to smooth rough areas. We used the small Cubify printer and ABS material, predominantly based on accessibility.
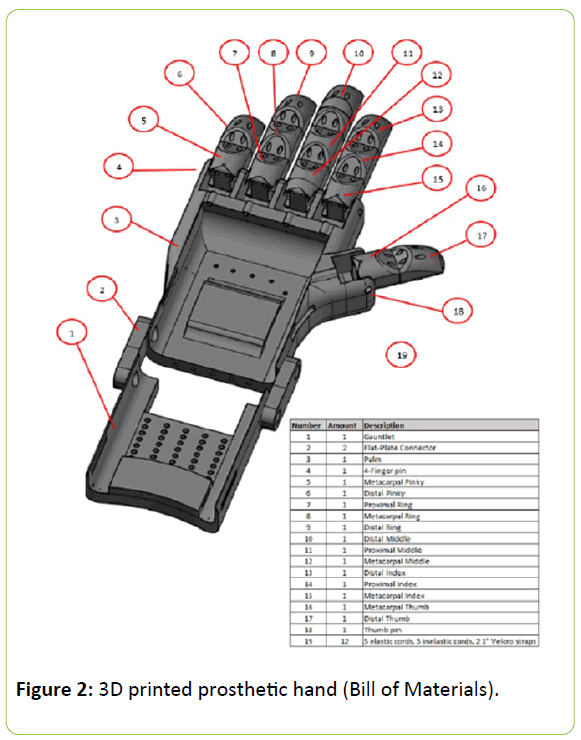
We were able to print and assemble our design for only $25 (low-cost compared to the designs previously described). The assembled design is shown in Figure 1 and a bill of materials is shown in Figure 2.
Conclusion
This paper overviews the need for a low-cost, 3D printable prosthetic for children and proof-of-concept in terms of the user printing their own prosthetic, as well as motivates the need for additive manufacturing training. This paper serves our first, initial step, towards demonstrating the feasibility of printing one’s own prosthetic. Future works may implement different materials and processes, as well as incorporate feedback from amputees within the surrounding hospitals. A review of other available previous prosthetics demonstrating how 3D printed prosthetics (such as the one shown here) may serve as an economical option in that we were able to print and assemble a prosthetic hand for just $25. But more importantly, 3D printed prosthetics may encourage independence in amputees (ability to partake in the design process). In the near-future, commercially available 3D printers, may make developing one’s own prosthetics an easy to accomplish task in one’s home environment.
Conflict of interest
None
Acknowledgements
We would like to acknowledge the National Science Foundation (NSF) for supporting this work via our awarded grant (Award Abstract #1533479) entitled: “Targeted Infusion Project: Integration, Cultivation, and Exposure to Biomedical Engineering at the University of the District of Columbia”; and equipment and supplies were funded in-part by Department of Energy – National Nuclear Regulatory Agency [Award No. 0007701-1000043016]. We would like to thank Dr. Pawan Tyagi for aiding the 3D printing effort at UDC. We would also like to thank School of Engineering and Applied Sciences Dean Devdas Shetty and Mechanical Engineering Chairperson (Dr. A. Segun Adebayo). Further, we would like to thank the UDC School of Engineering and Applied Sciences faculty and UDC staff and administration for their support.
References
- https://www.amputee†coalition.org/wp†content/uploads/2014/09/lsp_Roadmapfor†Limb†Loss†Prevention†and†Amputee†Care†Improvement_241014†092312.pdf
- Zuniga J, Katsavelis D, Peck J, Stollberg J, Petrykowski M, et al. (2015) Cyborg beast: a low-cost 3d-printed prosthetic hand for children with upper-limb differences. BMC Res Notes 8: 1-9.
- Cignini P, Giorlandino C, Padula F, Dugo N, Cafa EV, et al. (2012) Epidemiology and risk factors of amniotic band syndrome, or ADAM sequence. J Prenatal Med 6: 59–63.
- Parker SE, Mai CT, Canfield MA, Rickard R, Wang Y, et al. (2010) Updated National Birth Prevalence estimates for selected birth defects in the United States, 2004–2006. Birth Defects Res A Clin Mole Teratol 88: 1008–1016.
- https://www.centeropcare.com/Portals/COPC/Amputation%20Statistics.pdf
- https://www.amputeeâ€ÂÂcoalition.org/fact_sheets/preventingamp.html
- https://www.amputeecoalition.org/easyread/inmotion/may_jun_06/congenital_part3†ez.pdf
- Bray JJ (1970) Prosthetics†Orthotics Education Program: Prosthetic principles, upper extremity amputations: fabrication and fitting principles. Los Angeles: Prosthetics†Orthotics Education Program, Division of Orthopedic Surgery, University of California, Los Angeles.
- Biddiss EA, Chau TT (2007) Upper limb prosthesis use and abandonment: A survey of the last 25 years. Prosthet Orthot Int 31: 236-257.
- https://professionals.ottobockexport.com/cps/rde/xchg/ottobock_export_en/hs.xsl/232.html
- Vasluian E, de Jong IG, Janssen WG, Poelma MJ, van Wijk I, et al. (2013) Opinions of youngsters with congenital below†elbow deficiency, and those of their parents and professionals concerning prosthetic use and rehabilitation treatment 8: e67101.
- Wagner L, Bagley A, James M (2007) Reasons for Prosthetic Rejection by Children with Unilateral Congenital Transverse Forearm Total Deficiency. American Academy of Orthotists and Prosthetists 19: 51†54.
- Colombo G, Filippi S, Rizzi C, Rotini F (2010) A new design paradigm for the development of custom†fit soft sockets for lower limb Prosthetics. Computers Industry: Soft Products Dev 61: 513â€ÂÂ523.
- https://www.gizmag.com/open†bionics†superhero†Prosthetics†disney/39181/
- https://www.theguardian.com/artanddesign/architectureâ€ÂÂdesignâ€ÂÂblog/2015/jul/22/lego†prosthetic†arm†that†kidscan†hack†themselves
- Petrick IJ, Simpson TW (2013) 3D printing disrupts manufacturing: how economies of one create new rules of competition. Res Tech Manag 56: 12-16.
- Ullman D (2010) The Mechanical Design Process (4th Edn) McGraw†Hill New York.
- Advancing Minorities Interest in Engineering (2015). AMIE: Plant the Seeds of Greatness: Investing in our Future with Historically Black College & Universities [Brochure]. MVLE Inc.
- https://enablingthe future.org/which-design/
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences