A Survey of Assessment Anxiety, Depression, and Visual Dependence in Neurologic and Geriatric Physical Therapy Practices
Klatt BN1*, Sparto PJ1, Hoppes CW2, Brandfass K3 and Whitney SL1
1Department of Physical Therapy, University of Pittsburgh, USA
2Doctoral Program in Physical Therapy, Army-Baylor University, USA
3Doctoral in Physical Therapy, University of Pittsburgh Medical Center - Centers for Rehab Services, USA
- *Corresponding Author:
- Klatt BN
Department of Physical Therapy
University of Pittsburgh, Pittsburgh, PA, USA
Tel: 412-596-3950
E-mail: bnk12@pitt.edu
Received Date: March 19, 2021; Accepted Date: April 01, 2021; Published Date: April 07, 2021
Citation: Brooke NK, Patrick JS, Carrie WH, Kathleen B, Susan LW (2021) A Survey of Assessment of Anxiety, Depression, and Visual Dependence in Neurologic and Geriatric Physical Therapy Practices. J Physiother Res Vol.5 No.3:16.
Abstract
Background: Anxiety, depression, and visual dependence (ADVD) affect functional outcomes in people with neurologic diagnoses and older adults. The purpose of this project was to determine if physical therapists evaluate ADVD consistently in neurologic/geriatric physical therapy and if treatment strategies are standardized across providers. The hypothesis was that ADVD are not consistently assessed and that treatment strategies are not standardized.
Methods and Findings: Ninety-five physical therapists identified as primarily treating people with neurologic diagnoses were invited to complete an electronic survey about the assessment of ADVD. Clinical practice setting, typical caseload, experience, and degrees/certifications were recorded for each participant. Survey completion rate was 40% (n=38). Approximately 18% of the therapists “always” assess for anxiety (32% “most of time”; 8% “half the time”; 32% “sometimes”; and 10% “never”). Depression assessment was similar, and visual dependence was reported to be assessed slightly more than anxiety and depression. Qualitative evaluation revealed that physical therapists use varying assessment methods and intervention strategies for ADVD. There were significant positive associations between clinical practice setting and the assessment of visual dependence (χ2 (2, N=45) = 15.67, p < 0.001, with more physical therapists assessing visual dependence in the outpatient setting. Positive associations were also found between visual dependence assessment and the physical therapist being a board certified neurologic clinical specialist (χ2 (1, N=45) = 7.16, p= 0.007) or having a Doctorate of Physical Therapy (χ2 (1, N=45) = 7.19, p= 0.007). A major limitation of this study was that the surveyed physical therapists were all within the same geographical location.
Conclusion: Our results indicate that physical therapists are not consistently assessing for ADVD and the treatment strategies are not standardized, even when ADVD is evaluated. Additional education is warranted to improve care.
Keywords
Anxiety; Depression
Abbreviations
ADVD: Anxiety, Depression, and Visual Dependence; NCS: Neurologic Clinical Specialty (From the American Board of Physical Therapy Specialties); SVV: Subjective Visual Vertical
Introduction
Anxiety and depression are common in the United States, with the National Institutes of Mental Health estimating that 18.1% of adults experience anxiety and 6.7% experience depression within a year. The Anxiety and Depression Association of America reports that more than $42 billion are spent per year on healthcare costs secondary to anxiety disorders with more than $22 billion of the yearly costs related to utilization of repeated health care services. Anxiety and depression are common amongst people with neurologic diagnoses and older adults, and they also they have associations with worse functional outcomes [1,2]. Treatment strategies for anxiety and depression can be implemented into physical therapist practice, and referral for pharmacologic management and/or referral for multidisciplinary health services can optimize overall health outcomes and quality of life for people with anxiety and depression [3,4].
Anxiety is typically assessed using self-report measures but not all of the instruments are appropriate for older adults [5]. A 2012 systematic review identified a total of 91 different anxiety measures and based on their psychometric properties, determined that 5 instruments, the Beck Anxiety Inventory, Penn State Worry Questionnaire, Geriatric Mental Status Examination, Worry Scale, and Geriatric Anxiety Inventory were appropriate to use to assess anxiety in older adults [6]. The use of questionnaires, such as the Patient Health Questionnaire-2 (PHQ-2), the Patient Health Questionnaire-9 (PHQ-9), and the Geriatric Depression Scale (GDS-15) were also recommended to identify depression in physical therapist practice [7].
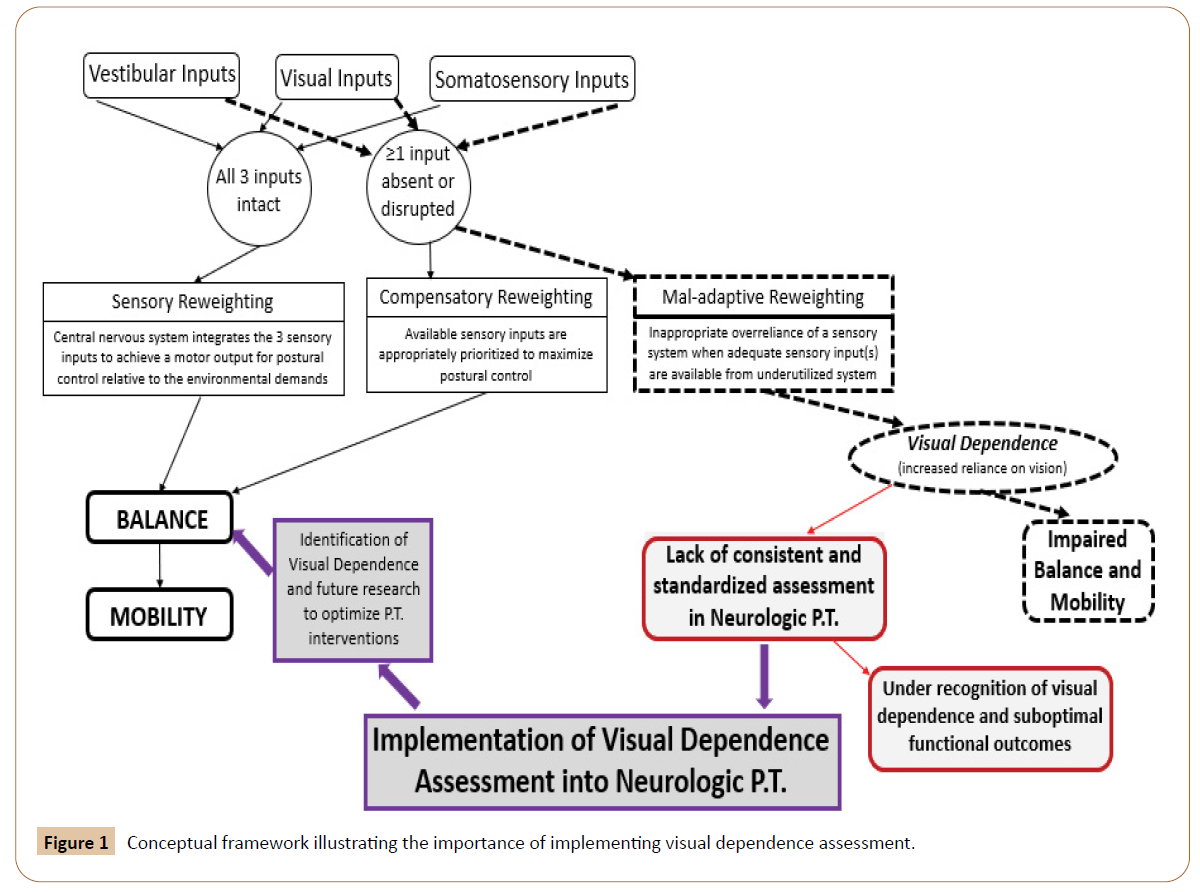
Visual dependence, which is a mal-adaptive sensory reweighting where increased reliance is placed on visual inputs compared to vestibular or somatosensory inputs for balance, has also been linked to worse outcomes and poorer prognosis for people with balance impairments of multiple etiologist [8-11]. There is a lack of consistent and standardized visual dependence assessment in neurologic/geriatric physical therapy which leads to an underrecognition of visual dependence (Figure 1). Identification of visual dependence may assist in optimal physical therapy outcomes [12,13].
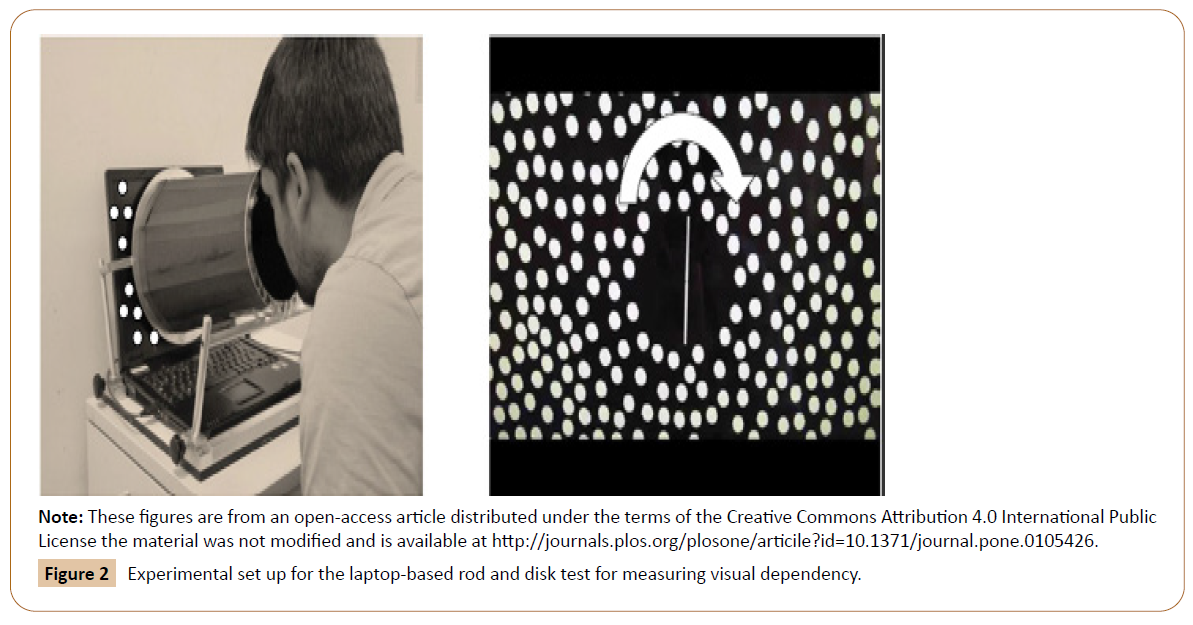
One way to assess visual dependence is with computerized dynamic post urography [14], but very few clinics have access these devices due to time, space, and cost. Clinicians often use the modified clinical test of sensory interaction and balance to assess the impact of sensory inputs on postural control [15]. Others have used computerized subjective visual vertical (SVV) rod and disk testing [16,17]. The computerized SVV rod and disk test assesses the ability of the patient to align a rod vertically with a blank field or align the rod vertically with the presence of roll motion (disk) in the background moving either clockwise or counter clock wise.
The rod and disk test yields quantifiable measurements of the patient's perception of vertical in dynamic visual environments, as measured by the degree of tilt from earth-vertical after the patient positions an illuminated rod using a keypad. This test can be completed in a laboratory setting where the rod and dots are illuminated in a full field array in an otherwise dark room [18]. For clinical application of the SVV rod and disk test, the patient places their head inside of a bucket to block peripheral cues, and the rod and moving dots are visualized on a laptop inside the bucket (Figure 2) [19].
Anxiety, depression, and/or visual dependence (ADVD) are not only prevalent with persons with balance and vestibular disorders [20,21] but are commonly seen in persons with head trauma including concussion [22,23], stroke [24], multiple sclerosis [25], and in older adults [26]. Depression and anxiety have been associated with decreased cognitive performance, impaired sleep, additional medical illness, increased mortality, and decreased quality of life [27-30]. Screening for anxiety and depression by physical therapists can lead to appropriate interventions that could reduce symptoms of anxiety and depression [31].
The purpose of this study was to determine if physical therapists screen for ADVD consistently in neurologic/geriatric physical therapy clinics and if treatment strategies are standardized across providers.
Research Methodology
Physical therapists identified within the University of Pittsburgh Medical Centre, Centres for Rehab Services who treat individuals with geriatric or neurologic diagnoses were invited to complete a survey with the objective to quantify ADVD knowledge and behaviour regarding ADVD assessment and treatment. The Institutional Review Board at the University of Pittsburgh approved the study protocol. Ninety-five physical therapists were sent an electronic survey about the assessment of ADVD using Qualtrics software (Qualtrics, LLC, and Seattle, WA). Physical therapists who worked in acute care, acute inpatient rehabilitation, outpatient, and skilled nursing facilities were included. The physical therapists were given one month to complete the survey with a reminder sent two weeks following the initial invitation. The survey is included as an Appendix. In addition to obtaining information about clinical practice setting, degree earned, years of experience, and attainment of clinical specialty, the survey asked the physical therapists if they assessed ADVD and if so, how they assessed each. If they responded that they did not assess ADVD, they were prompted to answer reasons for not assessing the particular factor and what, if any, barriers they faced in their clinical practice related to assessing ADVD.
Using IBM SPSS Statistics 22 (IBM Corporation, Armonk, NY), Descriptive statistics and frequency tables were used for quantitative analysis of the data. Chi-squared tests of independence were used to determine associations between individual therapist characteristics (practice setting, degree earned, and specialty) and the frequency of assessment of anxiety, depression, and visual dependence. For the chi-squared tests, the five responses for the frequency of assessment of each of the three factors (anxiety, depression, and visual dependence) were dichotomized to represent assessment occurring “most of the time or more” and “half of the time or less”. Qualitative analysis included the identification of thematic responses which were in the open-ended questions related to how the identification of ADVD impacts physical therapy plan of care.
Results
The number of physical therapists identified in each practice setting and the number of those completing the entire survey are provided in Table 1. Forty-nine physical therapists initiated the survey, but there was a drop in the number of responders as the survey progressed. Forty-six physical therapists answered the start of the visual dependence questions (question #6) with 4 more dropouts during subsequent visual dependence questions. At the start of the questions related to anxiety and depression (question #13), there were 38 responders and there were no additional dropouts for the remainder of the survey.
| Variables | Number of physical therapists identified within setting | Number of physical therapists who initiated the survey (%) | Number of physical therapists who completed the survey (%) |
|---|---|---|---|
| Acute Care | 25 | 11 (44%) | 8 (32%) |
| Acute Rehab | 26 | 13 (50%) | 11 (42%) |
| Outpatient | 35 | 24 (69%) | 18 (51%) |
| Skilled Nursing | 9 | 1 (11%) | 1 (11%) |
| Total | 95 | 49 | 38 |
Table 1: Number of physical therapists identified in each clinical setting and the number that initiated/completed the survey.
A 40% survey completion rate was obtained (38 physical therapists completed the entire survey), with 23% of the respondents practicing in the acute care setting, 26% in acute inpatient rehabilitation, 49% in outpatient, and 2% in skilled nursing facilities. The respondents’ experience practicing in the physical therapy settings ranged from: 1-5 years (36% of respondents); 6-10 years (22%); 11-15 years (12%); 16-20 years (10%); greater than 20 years (20%). Twenty-six percent of the physical therapists had a Master of Physical Therapy degree and 74% a Doctorate of Physical Therapy degree. Thirty eight percent had an American Board of Physical Therapy Specialties Neurologic Clinical Specialty (NCS) and 5% had a Geriatric Clinical Specialty. The “Vestibular Rehabilitation: A Competency-Based Course” at Emory University was completed by 24% of the sample. All of the participating physical therapists (38/38) report treating older adults in their clinical practice.
The primary aim of this study was to determine whether or not physical therapists are assessing anxiety, depression, and visual dependency in their clinical practice and the data related to this aim is provided in Table 2.
| In your clinical practice, do you assess for: | |||
|---|---|---|---|
| Variables | Anxiety? (n=38) | Depression? (n=38) | Visual Dependence? (n=46) |
| Always | 18% | 24% | 30% |
| Most of the time | 32% | 26% | 39% |
| About half the time | 8% | 8% | 11% |
| Sometimes | 32% | 29% | 17% |
| Never | 10% | 13% | 2% |
Table 2: Physical therapist responses to whether or not they assess for anxiety, depression, and/or visual dependency in clinical practice (bold line illustrates dichotomy used in statistical analysis).
Visual dependence
A significant association was noted between clinical practice setting and the assessment of visual dependence (χ2 (2, N=45) = 15.67, p < .001). Assessment of visual dependence was performed by 95% of the outpatient physical therapists, 54% of the acute rehab physical therapists, and 30% of the acute care physical therapists. Positive associations between visual dependence assessment and the physical therapist having an NCS (94% v. 55% for not having an NCS, χ2 (1, N=45) = 7.16, p= .007) or having a Doctorate of Physical Therapy degree (79% vs. 36% not having a Doctorate of Physical Therapy degree, χ2 (1, N=45) = 7.19, p = .007) were noted. For 43% (18/42) of the physical therapists’, specific diagnoses guide the decision to assess for visual dependency while 55% (23/42) of the physical therapists’ report that the clinical presentation of the patient drives the decision to assess visual dependence.
The physical therapists were asked “which methods are capable of assessing visual dependence” and the responses are recorded in Table 3. When asked “which methods do you use clinically to assess visual dependence”, none of the physical therapists’ reported use of the computerized SVV rod and disk test (optimal method), 24 reported the use of the modified clinical test of sensory interaction and balance, and 3 reported the use of computerized dynamic post urography. There were 37 respondents that reported methods that do not assess visual dependence.
| Variables | Number of Physical Therapists that believe this test was capable of assessing visual dependency (%) (n=42) | Number of Physical Therapists that report using this test to assess visual dependency in clinical practice (%) (n=42) |
|---|---|---|
| Static visual acuity | 9 (21%) | 4 (10%) |
| Dynamic visual acuity | 11 (26%) | 3 (7%) |
| Oculomotor examination (pursuits, saccades, gaze holding) | 16 (38%) | 9 (21%) |
| Vestibulo-ocular reflex cancellation | 2 (5%) | 1 (2%) |
| Depth perception | 11 (26%) | 1 (2%) |
| Romberg | 26 (62%) | 15 (36%) |
| Modified clinical test of sensory interaction and balance | 35 (83%) | 24 (69%) |
| Computerized dynamic posturography | 24 (57%) | 3 (7%) |
| Subjective visual vertical bucket test | 8 (19%) | 1 (2%) |
| Computerized subjective visual vertical (rod & frame) | 6 (14%) | 0 |
| Computerized subjective visual vertical (rod & disk) | 7 (17%) | 0 |
| Rotational chair | 2 (5%) | 0 |
| Other responses | 1 (2%): “Visual scanning” 1 (2%): “Walking with head turns” 1 (2%): “Increased visual reliance during function” |
Table 3: Responses recorded by the physical therapists when asked which methods can assess visual dependence.
The physical therapists were asked about barriers in clinical practice that make using a specific visual dependence method impractical. The specific barriers identified include the functional ability of the patient, the prioritization on functional tasks, lack of equipment, lack of time, lack of training, and cognitive deficits of the patient.
When asked how their treatment strategies differed for patients identified to have visual dependence, the responses varied and, in some instances, contradicted a colleagues’ response. A discrepancy was observed amongst the responses with some physical therapists feeling balance activities should be completed with eyes closed and/or in low lighting, while others believe treating in bright setting and encouraging use of visual cues is the ideal strategy for treating visual dependence. Approximately 44% of the physical therapists reported that the focus of treatment should be on prioritizing teaching the patient compensatory strategies such as using an assistive device or walking near a wall for support, while 50% felt treatment should focus on working on reweighting sensory input utilization to promote functional recovery. One physical therapist reported that they focus on strengthening or weight shifting. Additionally, education to increase safety awareness was reported.
Anxiety and Depression
There was not an association was observed between clinical practice setting and the assessment of anxiety (χ2 (2, N=37) = 1.45, p = 0.48), or depression (χ2 (2, N=37) = 4.07, p = 0.13). Similarly, education was not associated with the assessment of anxiety or depression.
A variety of assessment methods and utilization of different clinical decisions to determine when to assess for anxiety and depression. The physical therapists reported that their decision of whether to assess for anxiety and depression was determined by: patient diagnoses (38% of physical therapists’ report this as a factor); medications prescribed (29%); symptom/behaviour presentation (79%, with wide range of description); and lack of improvement with rehabilitation efforts (38%). The specific method used to assess for anxiety and depression varied amongst the physical therapists with reported methods including self-report questionnaires, verbal interview/patient history, and information gathered from the intake form/chart review.
When asked how anxiety and depression are assessed in clinical practice, a wide range of responses were noted. In the 37 participating physical therapists, 79% relied on the qualitative examination to assess anxiety and depression. The electronic medical record is used by 84% and a patient history/intake form is used by 51%. Only 9% report the use of a validated questionnaire to identify anxiety and/or depression. The questionnaires reported to be used for anxiety were the Situational Characteristics Questionnaire (SitQ) [32], Dizziness Handicap Inventory (DHI) [33], the Hospital Anxiety and Depression Scale [34], and Beck Anxiety Inventory (BAI) [35]. Those reported to be used for depression were the Hospital Anxiety and Depression Scale [34] and Beck Depression Inventory (BDI) [36]. Other methods reported to be used for both anxiety and depression included gross assessment/observation, vitals, behavioural health consult, and neuropsychology evaluation.
Physical therapists report a wide range of responses for how the identification of anxiety and/or depression impacts their treatment strategies used. Twenty-eight percent of the responses focused on altering verbal communication with the patient (slowing down, different tone of voice, selectively providing feedback, increased feedback, engaging the patient with personal interests/beliefs/values, building rapport, extra time to provide rationale, calm and reassuring, acknowledge feelings and discuss their impact on participation, alleviate fears and build confidence). Emphasizing patient cantered goals and implementing personally meaningful activities were reported as a focus by 11% of the physical therapists. Reports of adding psychologically informed physical therapy, cognitive behavioural therapy techniques, relaxation training, meditation techniques, mindfulness, stress management, pacing, and breathing techniques to their treatment were noted in 33% of the responses. Behaviour modifications (walking program, sleep schedule) and treatment in a low stimulating environment was also reported. Increased attention to symptom management during patient education was reported by 33% of physical therapists as a strategy modification. Referral to other services (neuropsychology, primary care physician, psychiatrist, psychotherapy, a counsellor, or physician for medication) was reported as part of the multidisciplinary team approach for these patients was reported as a strategy used by 56% of the physical therapists who identify that a patient has anxiety and/or depression.
Discussion
Our results indicate that physical therapists do not consistently assess for ADVD. Only 18% of the physical therapists reported that they always assess for anxiety, 24% always assess for depression, and 30% always assess for visual dependence. Ten percent of the physical therapists never assess anxiety, 13% never assess depression, and 2% never assess visual dependence. The high percentage of the other responses (“most of the time”, “about half the time”, and “sometimes”) indicate the variability in the frequency that ADVD is assessed during the episode of care.
Despite some physical therapist’s impression that they can intuitively identify when a patient is anxious and/or depressed, research shows that validated outcome assessments should be utilized rather than physical therapist judgment alone [37]. One example of an appropriate tool for people with physical health problems is the Hospital Anxiety and Depression Scale [34], which is reliable and valid for detecting and measuring the severity of anxiety and depression [34]. One study surveying 416 physical therapists identified limited clinician knowledge, lack of follow-up resources, and clinicians’ beliefs that the information of presence of depression would not impact the plan of care and/ or outcomes as some of the barriers to screening for depression in clinical practice.
Most research studies use computerized SVV rod and disk testing to assess visual dependence, but based on our survey, this is not being done in clinical practice (0/42 physical therapists who responded to questions related to how visual dependence is assessed, reported use of this method in their clinical practice and only 7/42 had knowledge that this method can assess visual dependence). Rod and disk testing can be performed using a clinic laptop [12]. Additionally, some clinicians use the Situational Characteristics Questionnaire to screen for the need to assess visual dependence.
While many of the responses for how the physical therapist alters their treatment for people with ADVD identified appropriate strategies, there were some conflicting reports and the lack of standardization of intervention strategies was apparent. This lack of standardization and treatment variability does not promote best practice and/or optimal functional outcomes for older adults. Standardization of the examination and interventions for ADVD could decrease variability in physical therapy practice patterns. The standardization would facilitate research, as consistently delivered treatment paradigms addressing ADVD could be compared across patient groups and/or settings.
Limitations of this study include surveying physical therapists in the same geographical location. The software allowed the physical therapist to partially complete the survey and we noted that of the 49 physical therapists who initiated the survey, 38 completed it in its entirety. Factors that may have affected the response rate include time or additional burden; however, this survey was estimated to take less than 10 minutes to complete. Future research should investigate the impact of using standardized assessment methods for ADVD and determining if there are better patient outcomes.
Conclusion
While it is expected that older adults undergoing physical therapy interventions will make functional improvements, there are a subset of complex patients who do not achieve expected outcomes following rehabilitation. This results in chronic impairments that limit activity and participation, thereby increasing disability and healthcare utilization. These complex patients may have common (and treatable) features including the presence of anxiety, depression, and/or visual dependence (ADVD) that are not being identified and are not being treated in clinical practice. This study investigated the knowledge and clinical practice patterns related to assessment and treatment of ADVD and found that these three features are not being assessed consistently or in a standardized way across practice settings. Some physical therapists lack adequate knowledge regarding ADVD, indicating a need for education and training to optimize care.
Acknowledgement
Thank you to the University of Pittsburgh Medical Center - Centers for Rehab Services Neurologic Physical Therapists for their participation, and to the American Physical Therapy Association Academy of Neurologic Physical Therapy for Knowledge Translation mentorship.
Funding
Dr. Klatt was supported by an NIH Training in Auditory and Vestibular Neuroscience Grant (#T32-DC011499) during the completion of this trial.
Competing Interests
The authors report no conflict of interest. The views expressed are those of the authors and do not necessarily reflect the official policy or position of the Department of the Army, Department of Defence, or the U.S. Government.
References
- Balaban CD, Thayer JF (2001) Neurological bases for balance-anxiety links. J Anxiety Disord 15: 53-79.
- Baldacci F (2015) Migraine features in migraineurs with and without anxiety-depression symptoms: A hospital-based study. Clin Neurol Neurosurg 132: 74-78.
- Dissanayaka NNW (2017) Cognitive Behavior Therapy for Anxiety in Parkinson's Disease: Outcomes for Patients and Caregivers. Clin Gerontol 40: 159-171.
- SK W, Alyna T, John AH, Sean AH, Megan EV, et al. (2016) Group cognitive behavioural therapy for stroke survivors with depression and their carers. Top Stroke Rehabil 23: 358-65.
- Dennis RE, Boddington SJA, Funnell NJ (2007) Self-report measures of anxiety: Are they suitable for older adults?. Aging Ment Health 11: 668-677.
- Therrien Z, Hunsley J (2012) Assessment of anxiety in older adults: A systematic review of commonly used measures. Aging Ment Health 16: 1-16.
- Vieira ER, Brown E, Raue P (2014) Depression in older adults: Screening and referral. J Geriatr Phys Ther 37: 24-30.
- Crevits L (2007) False perception of visual verticality in multiple sclerosis. Eur J Neurol 14: 228-232.
- Cousins S (2014) Visual dependency and dizziness after vestibular neuritis. PloS one 9: e105426.
- Bronstein AM (1996) Visually and posturally mediated tilt illusion in Parkinson's disease and in labyrinthine defective subjects. Neurology 47: 651-656.
- Slaboda JC (2009) Visual field dependence influences balance in patients with stroke. Med Biol Soc 2009:1147-1150.
- Pavlou M (2010) The Use of optokinetic stimulation in vestibular rehabilitation. J Neurol Phys Ther 34: 105-110.
- Pavlou M (2011) The effect of repeated visual motion stimuli on visual dependence and postural control in normal subjects. Gait & Posture 33: 113-118.
- Redfern MS, Furman JM (1994) Postural sway of patients with vestibular disorders during optic flow. J Vestib Res 4: 221-230.
- Shumway-Cook A, Horak FB (1986) Assessing the influence of sensory interaction on balance. Phys Ther 66: 1548-1550.
- Dichgans J (1972) Moving visual scenes influence the apparent direction of gravity. Science 178: 1217-1219.
- yardley L, Pollak K, Gresty MA, Guerraz M, Rudge P, et al., (2001) Visual vertigo: Symptom assessment, spatial orientation and postural control. Brain 124: 1646-1656.
- Clark DB (1994) Panic in otolaryngology patients presenting with dizziness or hearing loss. Am J Psychiatry 151: 1223-1225.
- Moldover JE, Goldberg KB, Prout MF (2004) Depression after traumatic brain injury: A review of evidence for clinical heterogeneity. Neuropsychol Rev 14: 143-154.
- Moore EL, Terryberry-Spohr L, Hope DA (2006) Mild traumatic brain injury and anxiety sequelae: a review of the literature. Brain Inj 20: 117-132.
- Wright F (2017) Factors associated with poststroke anxiety: A systematic review and meta-analysis. Stroke Res Treat 2017: 2124743.
- Simpson S (2016) Anxiety, depression and fatigue at 5-year review following CNS demyelination. Acta Neurol Scand 134: 403-413.
- King-Kallimanis B, Gum AM, Kohn R (2009) Comorbidity of depressive and anxiety disorders for older Americans in the national comorbidity survey-replication. Am J Geriatr Psychiatry 17: 782-792.
- Salthouse TA (2012) How general are the effects of trait anxiety and depressive symptoms on cognitive functioning?. Emotion 12: 1075-1084.
- Norbury R, Evans S (2018) Time to think: Subjective sleep quality, trait anxiety and university start time. Psychiatry Res 271: 214-219.
- Medina AB (2014) Update of sleep alterations in depression. Sleep Sci 7: 165-169.
- Brenes GA (2007) Anxiety, depression, and quality of life in primary care patients. J Clin Psychiatry 9: 437-443.
- Titov N (2016) Treating anxiety and depression in older adults: A randomised controlled trial comparing guided v. self-guided internet-delivered cognitive-behavioural therapy. B J Psych Open 2: 50-58.
- Romas RT, Jacob RG, Lilienfeld SO (1997) Space and motion discomfort in Brazilian versus American patients with anxiety disorders. J Anxiety Disord 11: 131-139.
- Jacobson GP, Newman CW (1990) The development of the Dizziness Handicap Inventory. Arch Otolaryngol Head Neck Surg 116: 424-427.
- Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67: 361-370.
- Beck AT (1988) An inventory for measuring clinical anxiety: Psychometric properties. J Consult Clin Psychol 56: 893-897.
- Beck AT (1961) An inventory for measuring depression. Arch Gen Psychiatry 4: 561-571.
- Haggman S, Maher CG, Refshauge KM (2004) Screening for Symptoms of Depression by Physical Therapists Managing Low Back Pain. Physical Therapy 84: 1157.
- Bjelland I (2002) The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 52: 69-77.
- Fay P (2017) Depression screening by physical therapists: Practices, beliefs, barriers. J Back Musculoskelet Rehabil 30: 1221-1229.
- Pavlou M (2004) Simulator based rehabilitation in refractory dizziness. J Neurol 251: 983-995.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences