Oral Health in Children Suffering from Pyelonephritis and Nephrotic Syndrome
Department of Pediatric Dentistry, Faculty of Dental Medicine, Medical University-Varna, Varna, Bulgaria
- Corresponding Author:
- Angelova ST
Department of Pediatric Dentistry
Faculty of Dental Medicine
Medical University-Varna, Varna, Bulgaria
Tel: +359888147562
E-mail: dsirma_angelova@abv.bg
Received Date: October 15, 2017; Accepted Date: October 16, 2017; Published Date: November 24, 2017
Citation: Angelova ST. Oral Health in Children Suffering from Pyelonephritis and Nephrotic Syndrome. J Health Hyg. Vol.1 No.1:06
Copyright: © 2017 Angelova ST. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Bacterial infections of urinary tract are among most widely distributed infectious diseases in childhood. The onset and progression of the systemic disorders of pyelonephritis and nephrotic syndrome are related with the necessity of frequent hospitalization of children. There is a risk for children to get in stress in their attempts to cope with medicines’ programs, as well as with considerable restrictions of the alimentary regime. This can result in negligence concerning the significance of preventive cares for oral health, leading to its drastic deterioration.
Objectives: The purpose of this study is to evaluate the oral hygiene status and gingival condition of children suffering from pyelonephritis and nephrotic syndrome in relation to some clinical and environmental caries risk assessment factors.
Methods: By the means of the documentary method of personally addressed inquiry we obtain essential data regarding the common health status and the variety of cares provided for the oral and dental health of children. Based on the clinical method of PLI Silness-Lȍe record, we evaluate the degree of plaque accumulation upon teeth surfaces in its capacity of a considerable marker of initiation and progression of tooth decay process. By implementation of the gingival index GI Lȍe-Silness we ascertain or disprove a state of gingival inflammation.
Results: Among the predominant portion of children with established nephrotic syndrome GI fluctuates in range of values equivalent to moderate degree of gingivitis.
Conclusion: The prevailing portion of children with nephrotic syndrome is characterized with poor oral hygiene and moderate to severe degree of gingival inflammation.
Keywords
Renal disorders; Oral hygiene; Dental plaque; Gingival inflammation; Dental prophylactic cares
Introduction
Bacterial infections of urinary tract are among most widely distributed infectious diseases in childhood [1]. These are determined as inflammatory processes with impact upon tissues localized between the urethra and kidney parenchyma, with the definite symptom of bacteriuria. Urinary tract infections can occur in different ages, including the breastfeeding period and early childhood, often as a consequence of urine reflux [2,3]. Nephrotic syndrome characterizes with a complex of symptoms of proteinuria, hypo-proteinaemia, hypo-albuminaemia, hyperlipoproteinaemia, with increased concentration of cholesterol and triglycerides. The disease affects children predominantly between 1 and 6 years of age. A significant para-clinical indicator is the reduction of serum concentration of calcium, at the expense of protein-associated calcium [4]. The onset and progression of the systemic disorders of pyelonephritis and nephrotic syndrome are related with the necessity of frequent hospitalization of children. Efforts of doctors, parents and patients are concentrated on overcoming the somatic problem. The protocol of proper therapy of nephrotic syndrome and pyelonephritis includes: specific dietary regime with limitation of proteins-enriched foods and predominant consumption of fruits and carbohydrates; application of antibiotics, mainly of the group of aminoglycosides- Amicacin, Gentamycin; cephalosporines of second and third generation- Claforan, Rocephin, Fortum, semi-synthetic penicillines- Piperacillin. To reinforce the anti-inflammatory efficiency of antibiotics, these are combined with anti-pyretic medicines and non-steroid antiinflammatory drugs. In conditions of established nephrotic syndrome, in 90% of patients in child’s age there is an urgent necessity of corticosteroids’ administration [1-5]. Scientific literature ascertains the destructive impact of prolonged usage of these medicines upon hard teeth tissues, mainly enamel [6-8]. Disturbances of the processes of enamel organic matrix formation and mineralization can serve as predisposing factors for increased rate of caries activity of dentition of children frequently treated with antibiotics and immune-suppressive remedies. Investigations of the adverse effects of Amoxicillin establish that its application in the period of early childhood can cause disturbance of mineralization of enamel of permanent teeth. The dose-dependent impact of Amoxicillin upon ameloblasts reflects negatively their function, accentually during mineralization and maturation, related to quantity and/or quality hypo-mineralization defects [8,9]. Other authors identify infectious diseases and exposure of children to various environmental toxins as etiological factors for occurrence of demarcation zones of disturbed opacity upon enamel surface, which is often associated with enamel hypoplasia. Diffusive regions of disturbed transparency and smoothness correlate with application of antibiotics of the group of penicillines in conditions of significant duration and frequency of intake[10].
The enhanced risk of tooth decay among patients treated with glucocorticoids can be manifested as a consequence of their common health status, as well as of physical and psychological effects of applied pharmacotherapy. Research performed in clinical conditions verifies that in patients in immune-deficiency state are diagnosed definite findings of rampant caries and periodontal disorders. The slow rate of progression of asymptomatic periodontitis is associated with explicit destruction of the root surfaces of affected teeth [7]. In the context of some studies, parallel to the intensity of intake of antibiotics and corticosteroids, infectious and autoimmune diseases are also characterized with considerable dynamics of body temperature curves. Frequent episodes of sub-febrile and febrile state can reflect upon complex processes of formation of hard teeth tissues. Disturbance of balanced and coordinated build-up of specific architectonics of apatite crystals makes enamel vulnerable to multiple caries-provoking factors into oral cavity [9]. There is a risk for children to get in stress in their attempts to cope with medicines’ programs, as well as with considerable restrictions of the alimentary regime. This can result in negligence concerning the significance of preventive cares for oral health, leading to its drastic deterioration.
Tooth decay is a multifactorial, behavior-related bacterial disease. In a large number of countries caries is considered to be one of the most significant health problems among the population of child’s age [11]. Plenty of predisposing factors can provide an effect of stimulation and intensive progression of tooth decay. Among these predictors with its explicit role is the poor oral hygiene. The unsatisfactory level of oral hygiene round a tooth affected by caries induces a cumulative effect of gingival inflammation. Infected primary teeth are associated with a potential risk of disturbance of the structure and development of their permanent followers [12]. Models of caries risk assessment consist of combinations of indicators, including biological inductors, protective factors, clinical findings [13-15]. Researches accentuate on some essential factors: specifics of nutrition, frequency and consistency of consumed carbohydrates; exposure to endogenous and exogenous forms of fluorides with preventive effect; host’s susceptibility to cariesprovoking microorganisms; representatives of oral microbiota; social-economic traits; cultural markers; behavioral patterns [16]. The categorization of a high level of tooth decay risk can be determined on the base of a single clinical finding, namely moderate or great amount of dental plaque deposited especially upon frontal teeth surfaces, involving marginal gingiva [17]. Low level of caries risk associates with no zones of visible plaque and no symptoms of gingival inflammation. Moderate risk determination corresponds with the diagnosis of gingivitis [18]. Some researchers, including participants in the National Initiative for improvement of oral health, organized by professionals of various scopes of medicine and dental medicine under the aegis of the American Academy of Pediatrics, accentuate upon the clinical significance and practical value of a simplified protocol for caries risk assessment. Into the context of this protocol are designated some considerable indicators of tooth decay risk, namely: carious lesions active at the moment of dental examination; treated carious lesions; registration of fillings on teeth and teeth surfaces; caries upon the root surface of the tooth; application of products for endogenous and exogenous fluoride prophylaxis; alimentary regime; frequency of carbohydrates’ nutrition; oral-hygiene procedures; tests for verification of the microbial titter of Streptococcus mutans and Lactobacillus; tests for record of salivary flow[6,19-21].
The aim of the study is to evaluate the oral hygiene status and gingival condition of children suffering from pyelonephritis and nephrotic syndrome in relation to some caries risk assessment factors.
Study Design
Material
The representatives of the current investigation are 116 children suffering from renal disorders. With the diagnosis of pyelonephritis are 92 of all the subjects. Among them predominate girls- 71.74% and the ratio of boys consists of 28.26%. A total number of 24 of the participants in the study are with the established diagnosis of nephrotic syndrome. The ratio of girls amounts to 54.17% and the rest 45.83% are boys.
Methods
By the means of the documentary method of personally addressed inquiry we obtain essential data regarding the common health status and the variety of cares provided for the oral and dental health of children, namely: specifics of nutrition habits; individually and professionally conducted oral hygiene procedures; application of endogenous and exogenous forms of fluorides’ prophylaxis. Based on the clinical method of PLI Silness-Lȍe record, we evaluate the degree of plaque accumulation upon teeth surfaces in its capacity of a considerable marker of initiation and progression of tooth decay process. By implementation of the gingival index GI Lȍe-Silness we ascertain or disprove a state of gingival inflammation.
Study Results
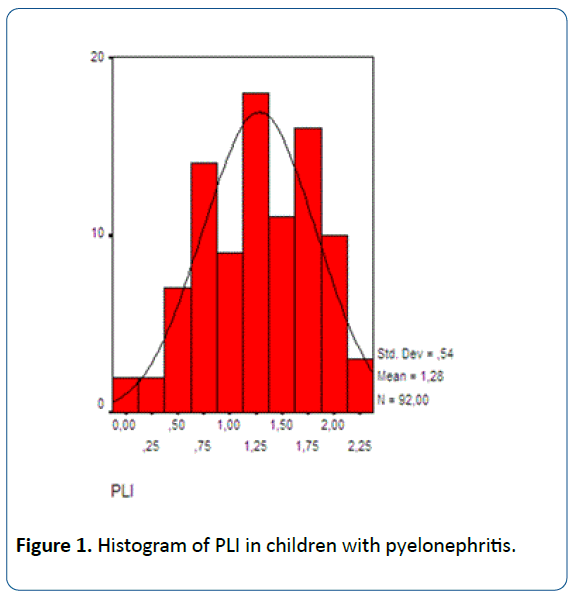
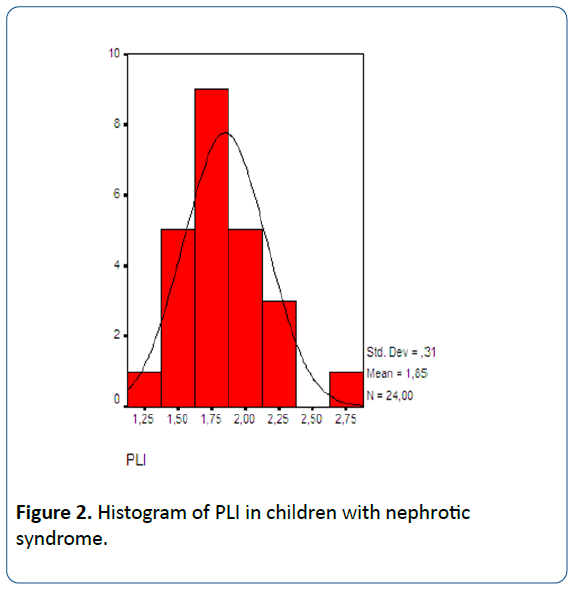
The histogram of PLI in patients with pyelonephritis demonstrates that in 1.1% of these (in 1 of a total number of 92 patients) the value of PLI equals to 0. This result is interpreted as perfect oral hygiene status. Also in 1.1% of all the representatives of this examined group, namely in 1 patient is registered a maximum value of PLI=2.36. The last value associates with poor oral hygiene condition. In the predominant portion of children with pyelonephritis the index of PLI varies in the interval between 1.00 and 1.77, equivalent to good towards satisfactory oral hygiene level. The histogram of PLI concerning children with the diagnosis of nephrotic syndrome illustrates that in 4.2% of these (in 1 of a total number of 24 patients) is recorded the lowest value of PLI=1.32. The maximum value of PLI=2.68 also concerns 4.2% of the representatives of this group. In the prevailing portion of children suffering from nephrotic syndrome, namely 37.5% of them, the indicator of PLI fluctuates between 1.82 and 2.00. (Figures 1 and 2) [22].
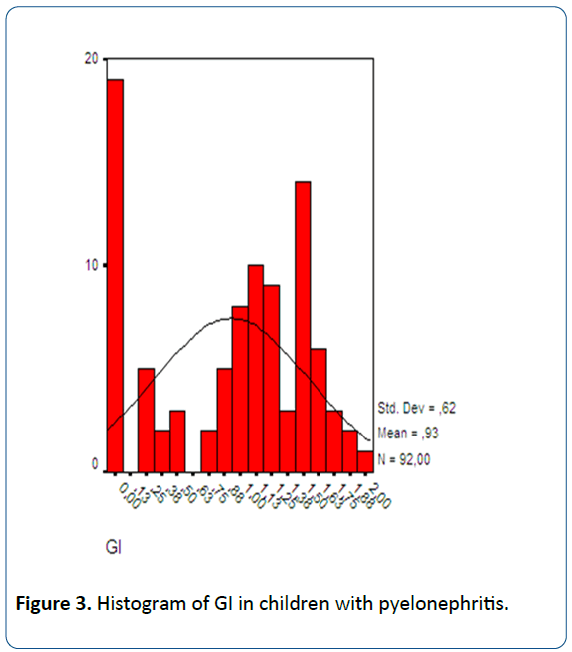
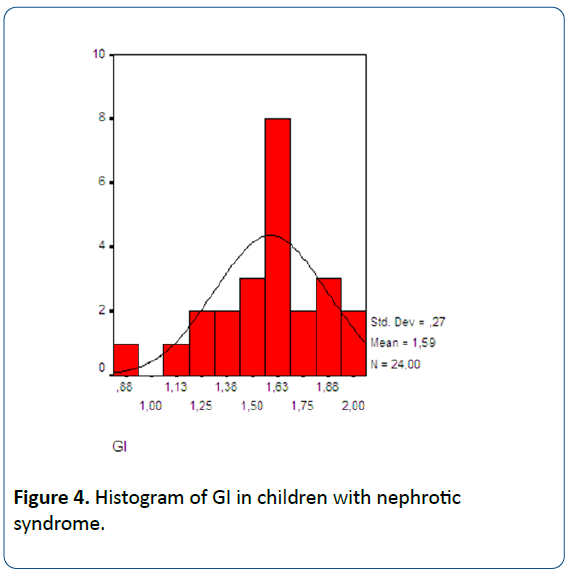
According to the histogram of GI of children with the diagnosis of pyelonephritis, for 20.7% of them (19 of the total number of 92 participants) is ascertained the minimal value of GI=0.00, interpreted as lack of gingival inflammation. In 1.1% of children included into this group of investigation (in 1 child suffering from pyelonephritis) is established the maximum value of GI=2.00. Among the predominant portion of the examined participants in this group the index of GI varies in the range between 0.99 and 2.00, corresponding to a moderate degree of gingival inflammation. The value of GI=0.91 concerns only 1 out of a total number of 24 patients with diagnosed nephrotic syndrome. Also in 4.2% of the representatives of the group is recorded the maximum value of GI=2.05. This result is interpreted as a state of moderate with a tendency to severe inflammation of gingival tissues. Among the predominant portion of 37.5% of children with established nephrotic syndrome GI fluctuates in the range between 1.64 and 1.77, equivalent to moderate degree of gingivitis (Figures 3 and 4) [22].
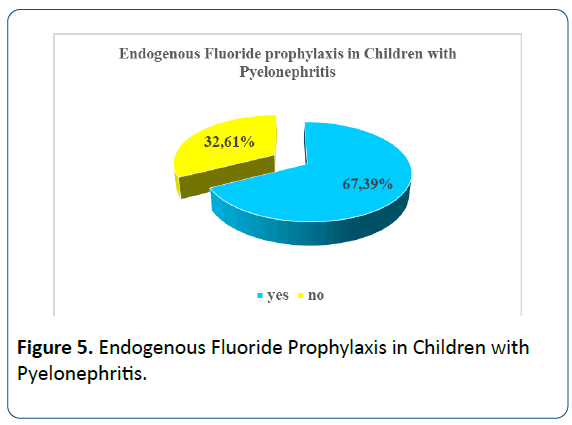
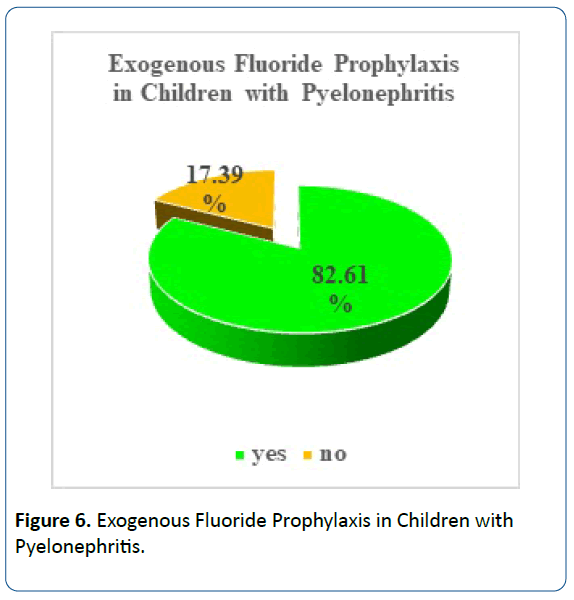
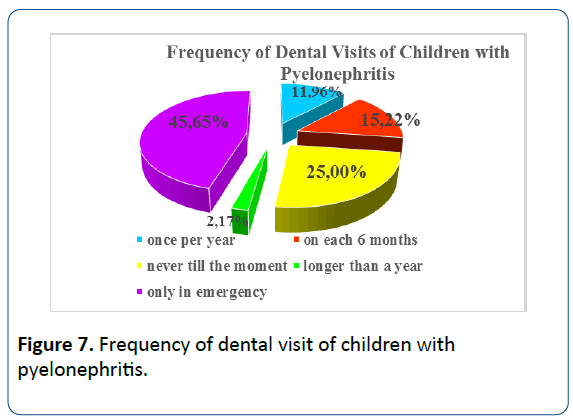
Application of endogenous fluoride prophylaxis is registered among 67.39% of all the children with the diagnosis of pyelonephritis included into the investigation. Implementation of exogenous fluoride prophylaxis concerns 82.6% of the participants suffering from pyelonephritis. (Figures 5 and 6) [22]. Approximately 1/3 of these patients (32.61%) perform regular individual oral hygiene procedures twice per day. Almost equivalent, namely 28.26% is the portion of children involved in this group who are characterized with a lack of oral hygiene habits on individual level. More than one half (51.09%) of the patients with pyelonephritis consume sugar-containing foods and drinks incessantly. Among ¼ of the children of this group is recorded lack of dental visits. About ½ (45.65%) of the representatives of the group seek for dental services only in emergency. Only 15.22% of children included in the group perform prophylactic check-ups twice per year (Figure 7) [22].
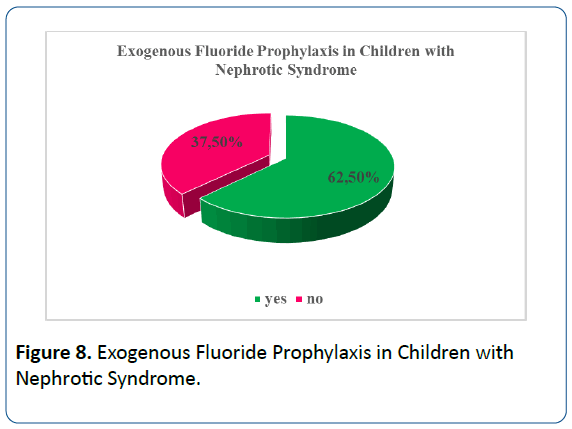
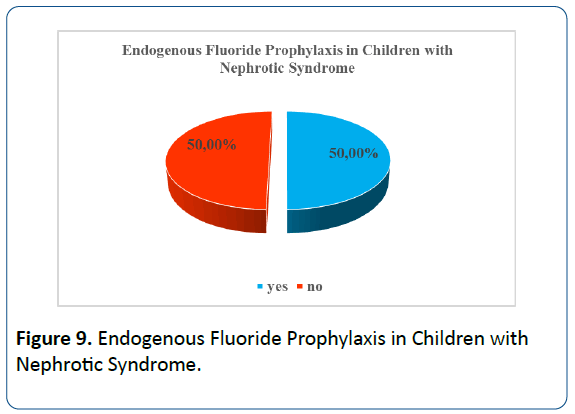
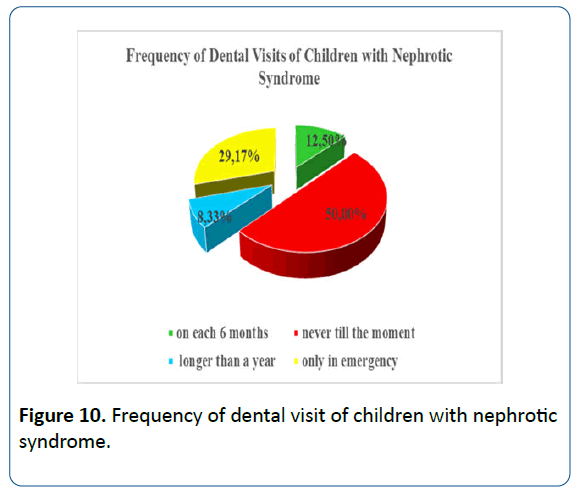
Among ½ of the children suffering from nephrotic syndrome is performed endogenous fluoride prophylaxis. Equal is the portion of participants of this group without application, respectively no effect of fluorides during the stages of initial mineralization and pre-eruptive mineralization of hard teeth structures. Regarding 62.50% of children with the diagnosis of nephrotic syndrome we establish application of exogenous fluoride prophylaxis (Figures 8 and 9)[22]. More than 1/3 of the patients with diagnosed nephrotic syndrome (regarding participants equal to 37.50% of all the representatives of the group) demonstrate regular oral hygiene habits, with tooth-brushing procedures conducted twice per day. Lack of individual oral hygiene cares is recorded among 29.17% of all the children of this group. Uncontrolled sugar foods and drinks consumption concerns ¾ of all the patients with nephrotic syndrome. We ascertain that ½ of the children included in that group never visited dentist before. A portion of 29.17% of these children visit dentist only in emergency. Only 12.50% of participants in the study suffering from nephrotic syndrome perform regular prophylactic dental check-ups on each 6 months (Figure 10) [22].
Discussion
Based on investigations performed among participants younger than 6 years of age is established that children with diagnosed caries lesions need 3.5 times greater volume of treatment procedures (newly done restorations, separation in the zone of a-proximal contacts, extraction) on primary teeth in the period between 7 and 12 years, in comparison with children of the same age without registered tooth decay [23-25]. Attitude of parents towards oral health of their children conceptually associates with cultural and social-economic indicators. Some people ignore the importance of dental cares, particularly for primary dentition, because of lack of basic health-related knowledge, language and communication barriers or other environmental traits [26-28]. Among the products characterized with strong protective potential against tooth decay are endogenous and topical fluorides, appropriate for application respectively during the period of pre-eruptive and post-eruptive mineralization. Tooth-brushing with fluoride-containing tooth pastes influences in a mechanical and chemical way the dynamics of qualitative and quantitative traits of dental plaque. The explicit effect of caries reduction concerns primary, as well as permanent teeth [29,30]. Researchers accentuate on the urgent necessity of performance of training programs with the active participation of general practitioners and pediatricians in order to be educated to provide adequate complex cares for the oral health of their patients, seeking collaboration with dental medicine colleagues for optimization of quality and duration of life of children suffering from renal diseases in different periods of childhood [31-34]. Procedures of caries risk assessment applied in dental practice serve as determinants of individual susceptibility to oral-dental diseases, and as prerequisites for organization and performance of preventive cares. Individuallycomposed and oriented, as well as target group implemented primary prophylaxis aim to exclude the incidence of oral health disorders on personal, group and population level. Researchers and practitioners take into consideration the range of therapeutic effects upon clinically manifested diseases and efficiency of treatment procedures applied in accordance with prerogatives of preventive and restorative dental medicine, avoiding complications of any kind [16].
Conclusion
In the frames of our study we can conclude that both of the indices of PLI and GI are characterized with higher values in the group of children suffering from nephrotic syndrome. The predominant portion of the representatives of this investigated group is characterized with poor oral hygiene and moderate to severe degree of gingival inflammation. Regarding some environmental caries risk assessment factors, namely: application of endogenous fluoride prophylaxis, implementation of exogenous fluoride prophylaxis, frequency of individual oral hygiene procedures, frequency of sugar-containing foods and drinks consumption and frequency of dental visits, we establish definitely higher risk of caries among children with the diagnosis of nephrotic syndrome, in comparison with these suffering from pyelonephritis.
References
- Palazzi DL, Campell JR (2011) Acute cystitis in children older than two years and adolescents.
- Bliznakova D (2010) Pediatrics for Dental Medicine Students. 227-272.
- Herold, Gerd. Internal Medicine. Ch. II. Sofia, MI, “Sharov”, 2011, 182-233.
- Meyrier A (2016) Acute kidney injury (acute renal failure) in minimal change disease and other forms of nephrotic syndrome.
- Ivanov, Ivan (2005) Internal diseases. Comments or one practical approach for their diagnostics and treatment. Sofia-Moskva, Pensoft 221-296.
- Blue Ch, Isringhausen K, Dils E (2011) Raising Oral Health Awareness among Nephrology Nurses. The Journal of Dental Hygiene 85: 151-157.
- Lăcătuşu S, Ghiorghe A (2004) Clinical aspects of the evolution of dental caries and periodontal disease in patients treated with corticosteroids. Rev Med ChirSoc Med Nat Iasi 108: 899-902.
- MihalaşE, Matricala L, Chelmuş A, Gheţu N, Petcu A, et al.( 2016) The Role of Chronic Exposure to Amoxicillin/Clavulanic Acid on the Developmental Enamel Defects in Mice. ToxicolPathol 44: 61-70.
- Beentjes VE, Weerheijm KL, Groen HJ (2002 ) Factors involved in the aetiology of molar-incisor hypomineralisation (MIH). Eur J Paediatr Dent 3: 9-13.
- Arrow P (2009) Risk factors in the occurrence of enamel defects of the first permanent molars among schoolchildren in Western Australia. Community Dent Oral Epidemiol 37: 405-15.
- Do LG (2012)Distribution of caries in children: Variations between and within populations. J Dent Res 91: 536–543.
- Stenlund H, Mejare I, Kallestal C (2002) Caries rates related to approximal caries at ages 11-13: a 10-year follow-up study in Sweden. J Dent Res 81: 455-458.
- Alaluusua S, Malmivirta R (1994) Early plaque accumulation- A sign for caries risk in young children. Community Dent Oral Epidemiol 22: 273-276.
- Roeters J, Burgesdijk R, Truin GJ, van 't Hof M (1995) Dental caries and its determinants in 2- to 5-year old children. ASDC J Dent Child 62: 401-408.
- Russell MW, Hajishengallis G, Childers NK, Michalek SM (1999) Secretory immunity in defence against cariogenic mutans streptococci. Caries Res 33: 4-15.
- Zero D, Fontana M, Lennon AM (2001) Clinical applications and outcomes of using indicators of risk in caries management. J Dent Educ 65: 1126-32.
- Vanobbergen J, Martens L, Lessaffre E, Bogaerts K, Declerck D (2001)The value of a baseline caries risk assessment model in the primary dentition for the prediction of caries increment in the permanent dentition. Caries Res 35: 442-450.
- Ramos-Gomez FJ, Crystal YO, Waing M, Crall JJ, Featherstone JDB (2010) Pediatric Dental Care: Prevention and Management Protocols Based on Caries Risk Assessment. J Calif Dent Assoc 38: 746–761.
- Lewis CW , Boulter S, Keels MA , Krol DM, Mouradian WE, et al.( 2009) Oral health and pediatricians: results of a national survey. AcadPediatr, 9: 457-461.
- Ramos-GomezFJ, Crystal YO, Domejean S, Featherstone JD (2012) Minimal intervention dentistry: Part 3. Paediatric dental care- prevention and management protocols using caries risk assessment for infants and young children. British Dental Journal 213: 501-508.
- Ramos-Gomez FJ, Crystal YO, Ng MW, Crall JJ , Featherstone JDB , et al. ( 2010) Pediatric dental care: prevention and management protocols based on caries risk assessment. J Calif Dent Assoc 38: 746-761.
- Angelova ST (2017) Assessment and Prevention of Caries Risk in Children Suffering from Some Renal Disorders, dissertation, 117-121, 127-134.
- Low W, Tan S, Schwartz S (1999) The effect of severe caries on the quality of life in young children. Pediatr Dent 21: 325-326.
- PittsNB (2004) Are we ready to move from operative to non-operative/preventive treatment of dental caries in clinical practice.Caries Res 38: 294-304.
- RatnayakeN, Ekanayake L (2005) Prevalence and impact of oral pain in 8-year-old children in Sri Lanka. Int J Paediatr Dent 15: 105-112.
- AdairPM, Pine CM, Burnside G, Nicoll AD, Gillett A, et al. (2004)Familial and cultural perceptions and beliefs of oral hygiene and dietary practices among ethnically and socio-economically diverse groups. Community Dent Health 21: 102-111.
- Ng MW (2003) Multicultural influences on child-rearing practices: implications for today’s pediatric dentist. Pediatric Dent 25: 19-22.
- Skeie MS, Espelid I, Riordan PJ, Klock KS(2008) Caries increment in children aged 3-5 years in relation to parents’ dental attitudes: Oslo, Norway 2002 to 2004.Community Dent Oral Epidemiol 36: 441-450.
- Carl JJ (2005) Development and integration of oral health services for pre-school-age children. Pediatr 27: 323-330.
- Tsang P, Qi F, Shi W (2006)Medical approach to dental caries: Fight the disease, not the lesion. Pediatr Dent 28: 188-198.
- Caspary G, Krol DM, Boulter S, Keels MA, Romano-Clarke G, et al. (2008) Perceptions of oral health training and attitudes toward performing oral health screening among graduating pediatric residents. Pediatrics 122: e465-e471.
- Ditto MR, Jones JE, Sanders B, Weddell JA, Jackson R ,et al.( 2010) Pediatrician’s role in children’s oral health: an Indiana survey. ClinPediatr (Phila) 49: 12-19.
- Douglas AB, Douglass JM, Krol DM (2009) Educating pediatricians and family physicians in children’s oral health. AcadPediatr 9: 452-456.
- Freed GL, Dunham KM, Switalski KE , Jones MD Jr, McGuinness GA, et al. (2009) Recently trained general pediatricians: perspectives on residency training and scope of practice. Pediatrics 123: 38-43.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences