Fragility Hip Fracture in the under 60s: A Qualitative Study of Recovery Experiences and the Implications for Nursing
Gillian Janes1*, Laura Serrant2 and Magi Sque3
1Yorkshire and Humber Patient Safety Translational Research Centre, Bradford Royal Infirmary, Bradford, UK
2Department of Health and Wellbeing, Sheffield Hallam University, Sheffield, UK
3Department of Clinical Practice and Innovation, The Royal Wolverhampton NHS Trust, Faculty of Education, Health and Wellbeing, University of Wolverhampton, Wolverhampton, UK
- *Corresponding Author:
- Gillian Janes
Yorkshire and Humber Patient Safety Translational Research Centre
Bradford Royal Infirmary
Bradford, UK
E-mail: g.janes@live.co.uk
Received Date: July 7, 2018; Accepted Date: September 5, 2018; Published Date: September 11, 2018
Citation: Janes G, Serrant L, Sque M (2018) Fragility Hip Fracture in the under 60s: A Qualitative Study of Recovery Experiences and the Implications for Nursing. J trauma Orth Nurs 2:3.
Abstract
Background: Hip fracture is a common, serious, complex injury and an important cause of morbidity, mortality and rising healthcare costs. Incidence and impact in the under 60s has been under researched. The aim of this study was therefore to explore the recovery experiences of young adults with an isolated hip fracture following a minor fall to inform future care delivery.
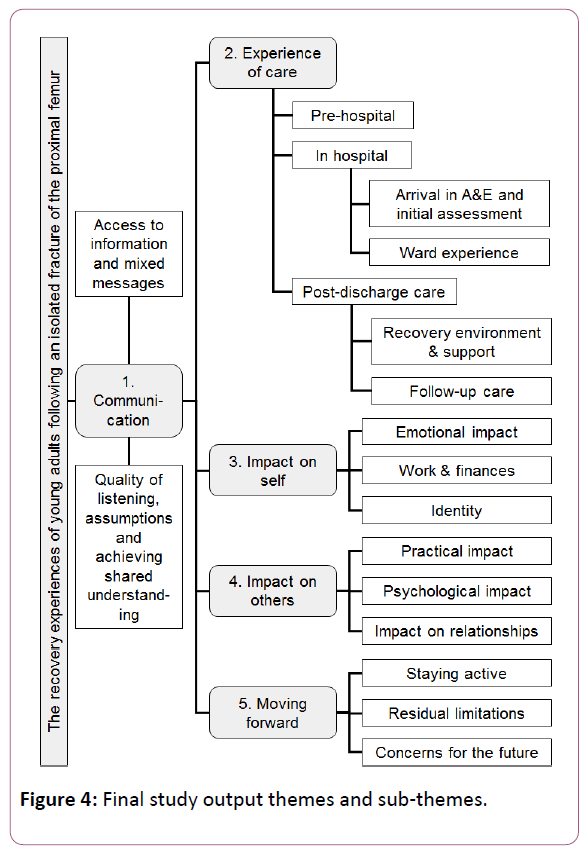
Methods and Findings: The Silences Framework was used to guide a critical interpretivist study. Thirty in-depth, minimally structured, story-telling interviews were conducted with participants between one and 10 years post injury. One cross-cutting theme, ‘Communication’ and four main themes: ‘Experience of care’, ’Impact on self’, ‘Impact on others’ and ‘Moving forward’ were identified. The findings indicated multi-faceted, often long term, physical, social and psychological impact on participants, their family and wider social networks. This included Post Traumatic Stress Disorder type symptoms and impact on work, finances and relationships. Inadequacies in the current care pathway and limited relevance of the commonly used patient reported hip fracture outcome measures used for young adults were also identified.
Conclusion: The dominant discourse on fragility hip fracture almost exclusively focuses on the elderly and short-term outcomes. This was the first study investigating the long-term impact of fragility hip fracture in young adults from their perspective and the first application of a new research framework in an acute care setting. It found the needs of younger hip fracture patients are not adequately recognised or addressed. Increased awareness and improvements in healthcare provision are needed to minimise the long-term personal and societal impact of fragility fracture in the under 60s.
Keywords
Fragility hip fracture; Under 60s; Silences; Recovery experiences; Orthopaedic nursing; Marginalisation; Falls
Introduction
Hip fracture is common, threatens functional status and leaves patients vulnerable [1-3]. It requires a complex recovery journey [4], multidisciplinary treatment and often extended hospital stay [5,6]. As an important cause of morbidity and mortality worldwide [7], hip fracture is one of the biggest challenges [8] and most significant healthcare burdens [9] of the 21st century. Associated with a dramatic increase in healthcare consumption [10] and cost to the UK alone of approximately £2billion annually [11], it’s impact on healthcare costs, individuals and society is considerable.
Hip fracture includes all fractures of the proximal femur [12]. This is a serious injury [13], often a sudden, traumatic event [3] that poses a threat to life and: ‘…a catastrophic sentinel event causing major secondary prevention implications’. [14].
‘Fragility fractures’ result from low-energy injury such as a fall from standing height [15,16]. These predominantly occur in later life, average age 83 years [17]. United Kingdom guidance [11] addresses all ages, however the National Hip Fracture Database (for England, Wales, Northern Ireland and the Channel Islands), the largest prospective register in the world [6] only records hip fractures in people aged 60 plus. This scope reflects the major public health threat these fractures present for older people [14] and that hip fractures in the under 60s result from high impact injury and predisposing health conditions [18]. The comprehensiveness of hip fracture recording in younger people varies considerably between nations. Norway mirrors England, only recording the 60s and over [19] whilst Scotland includes everyone aged 50 and over at injury [6] and The Australia and New Zealand Hip Fracture Registry includes all patients aged 40 and over [20]. The UK has one of the highest hip fracture rates in Europe [21]. A relatively rare injury in young adults, it has potentially devastating effects on patients and their families [22-24] and increases healthcare usage [6,9]. These individuals are of working age therefore the potential social and economic implications of this injury in this group are profound [25].
The significance of hip fracture in young people may be underestimated [26]. Public health trends such as osteoporosis, which increases fracture risk in younger individuals and is reaching epidemic proportions worldwide [27], means incidence at an earlier age may rise considerably. Hip fracture is one of the most devastating complications of osteoporosis [28] at population and individual level [29]. The result is more activity addressing osteoporotic related fractures [21] and calls for increased acute orthopaedic care capacity and review of hip fracture care models [9].
Background
The large body of knowledge regarding the causes, treatment and clinical outcomes of hip fracture following minor trauma predominantly focuses on the elderly. A review of the literature [30] however indicates little is known of patient experience and even less about the outcomes and experiences of adults under 60 years of age. Their relatively small numbers, short hospital stay, younger age, fewer co-morbidities, and low rate of surgical complications mean this sub-group of the fragility hip fracture population fall outside the widely accepted societal and professional norms for this injury and are inadvertently marginalised as a result. Yet, the potential social and economic implications of hip fracture for younger adults with personal and social responsibilities are marked [25]. The aim of this study was therefore to explore the recovery experiences of young adults who had sustained an isolated hip fracture following a minor fall to inform nursing practice and enhance long-term patient outcomes.
Methods
A new research framework, The Silences Framework [31], guided an interpretive, criticalist approach. This was appropriate to ‘give voice’ to participants [32] and enable healthcare improvement through change and advocacy [33] by recognising the contextual nature of knowledge and inquiry [34].
Ethical considerations
Research Ethics Committee approval was obtained from the relevant academic and health care organisations. All participants provided written consent, including the use of verbatim quotations. The study design addressed issues concerning safety, maintaining anonymity and potential distress.
Sample/participants
Participants were recruited using a postal invitation, from a purposive cohort sample [35] of 343 individuals in one English region who met the inclusion criteria outlined in Table 1 and identified from a prospectively collected, high quality [36] dataset based on the European Standardised Audit of Hip Fractures in Europe (SAHFE) process [37]. The study recruited to target at the first attempt, achieving a response rate of 21% (n-71). Of these 71 responses, 31 were subsequently uncontactable, one served as a pilot interview and one individual did not attend for interview. Data collection continued until saturation was achieved [38] resulting in a study group of 30 participants.
| Inclusion criteria | Exclusion criteria |
|---|---|
| Age 18-60 years at time of fall | Age under 18 years or over 60 years at time of injury |
| Between 9 months and 10 years since fall | <9 months or >10 years since fall |
| Surgical repair of isolated fracture of the proximal femur (hip) | Planned hip arthroplasty (hip replacement) for chronic conditions e.g. osteoarthritis |
| Isolated hip fracture following low velocity fall | No fall e.g. stress fracture, pathological (malignancy) fracture |
| High velocity trauma or multiple injuries | |
| Taking Bisphosphonate medication indicating previously diagnosed osteoporosis | |
| No contact address on record |
Table 1: Inclusion/exclusion criteria.
Data collection
A minimally structured interview guide was designed and used. A pilot interview enabled the researcher to hone interviewing skills, develop a field-note format and practice verbal summarising for in-interview member checking. One to one interviews were conducted by telephone or on private NHS premises as selected by participants. Twenty-eight interviews lasted 90-155 minutes and two 50-60 minutes. All were digitally recorded and transcribed verbatim with identifying information removed. Participants were debriefed by the researcher concerning their interview content and experience. This included signposting to further support if necessary.
Data analysis
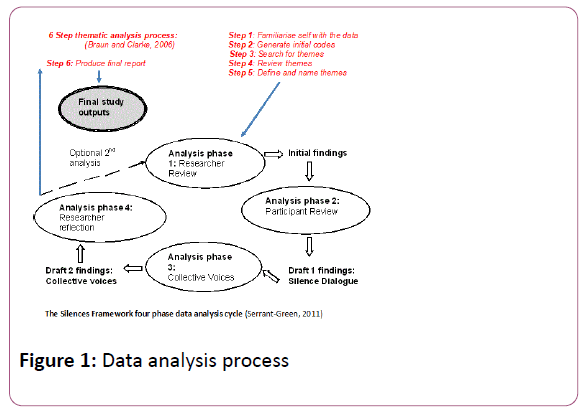
The researcher completed inductive, data driven thematic analysis [39] within the four-phase cyclical analysis of The Silences Framework [31]. Figure 1 illustrates this process. The data was analysed using Nvivo 10 to arrive at initial findings (phase 1) which were reviewed by 13 study participants and revised to arrive at draft 1 findings (phase 2). The phase 3 analysis, ‘collective voices’ process aims to include:
‘…the social networks of participants and others whose cultural, social or professional situation may impact on the research question’ [31]. Thirteen volunteers, from social groups featuring in the participant stories as having impacted on their experience of recovery, reviewed the draft 1 findings to arrive at the draft 2 findings. These included healthcare staff and carers with experience of caring for hip fracture patients, accessed using established research and public involvement processes in the host organisation and local ambulance service. Further researcher reflection on these draft 2 findings resulted in the final study outputs.
Rigour
The trustworthiness framework [40] was used to ensure study quality. Three member-checking processes i.e. periodic verbal in-interview summaries, participant review of initial findings and final study outputs plus ‘collective voices’ review of draft 1 findings enhanced credibility. Deviant cases in the data were also actively sought and analysed [41] and a data sample was independently coded by an experienced colleague followed by theme comparison. Maintaining an audit trail and making all documents and decision making processes available enhanced dependability. The researcher undertook all interviews and most of the transcribing to ensure consistency. Transcribing guidance was provided for contract transcribers and the researcher checked all transcripts for accuracy. Thick description enhanced transferability and description of research processes and decision making enhanced confirmability.
This study was undertaken by a nurse academic with past personal experience of this injury but no experience of orthopaedic nursing or the study site. Addressing positionality and researcher identity required reflexivity throughout the planning and execution of the research to ensure a trustworthy and honest account [42] with personal assumptions recognised and made explicit [43].
Findings
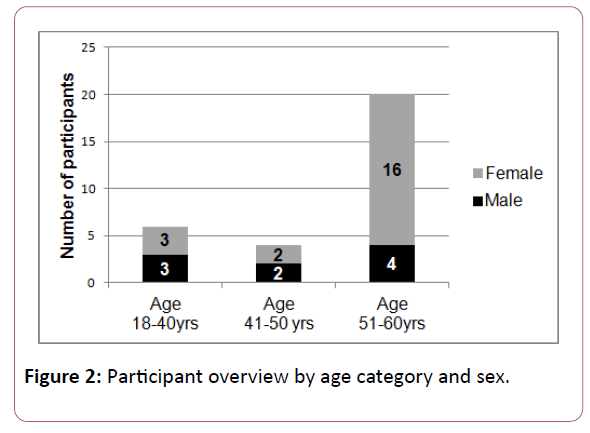
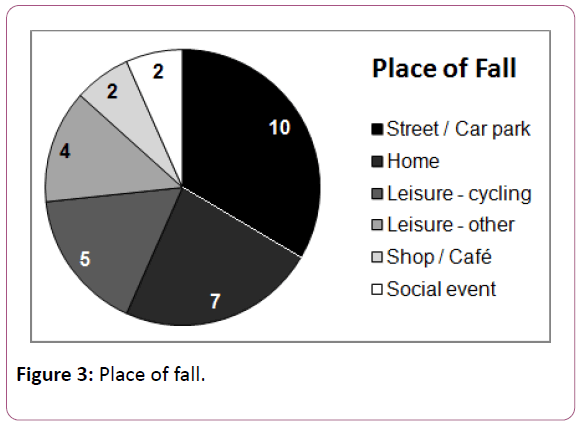
Participant characteristics are presented in Table 2 with key information summarised in Table 2 and Figures 2 and 3.
| Participant ID | Sex | Age at injury (years) | Time since injury (years) | S | AI | LA | D’s | Occupation | Pre-fall health conditions | Site of fall | Conditions found post injury | Conditions developed since injury | Type of surgery |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 02. RB (117) | F | 51-60 | 5-9 years | N | WRL | N | N | Hosuewife-husband | None | outside | Osteoporosis | Parkinsons Disease | Not known |
| 03. SF (10) | F | 51-60 | 1-4 years | Y | WRL | Y | N | Education manager | prem menopause | from step-kitchen surface -wheelchair | Osteopenia | Polymyalgia Rheumatica Temporal Arteritis | Screws\IM nail |
| 04. SJP (16) | F | 51-60 | 10 years | N | WRL | N | N | Radiographer | Ulcerative Colitis | café/shop | None | None | THR |
| 05. GT (339) | F | 29-40 | 1-4years | N | ORL | N | N | Nursery Nurse | None | at home | None | None | THR - multiple |
| 06. PAS (114) | F | 51-60 | 5-9 years | N | ORL | N | N | Office Worker | Thyroidectomy | at home | None | CVA | Pins |
| 07. JFS (25) | F | 41-50 | 5-9 years | N | WRL | Y | C | Community Midwife | None | outside | CKD/bipolar | None | Screws\IM nail |
| 08. FmC (171) | F | 51-60 | 1-4 years | N | WRL | Y | N | Nursery Nurse | None | inside venue | Osteoporosis | None | THR |
| 09. PW (244) | M | 29-40 | 1-4 years | Y | ORL | Y | N | Chef | None | outside | B12 deficiency | Embolisation | THR |
| 10. JD (331) | F | 51-60 | 1-4 years | N | WRL | N | N | Office Worker | None | outside | Osteoporosis | None | THR |
| 11. GB (11) | M | 51-60 | 1-4 years | N | WRL | N | N | Retired | Knee problem - RA as a child | outside | None | None | DHS |
| 12. PB (305) | M | 51-60 | 1-4 years | N | WRL | N | N | Factory worker | 2 previous sports related fractures | cycling | None | None | Screws\IM nail |
| 13. AEA (20) | F | 51-60 | 10 years | Ex | WRL | Y | N | Warden | None | at home | Osteoporosis | None | Screws\IM nail |
| 14. LSS (178) | F | 29-40 | 5-9 years | N | WRL | Y | N | Physiotherapist | None | outside | Osteopenia | None | DHS |
| 15. VJJ (83) | F | 51-60 | 5-9 years | N | WRL | Y | N | Office Worker | None | at home | Osteoporosis | None | Multiple |
| 16. DH (335) | F | 51-60 | 1-4 years | Ex | Teetotal | N | C | Pharmacy Worker | Possible bone density issues | outside | Osteopenia | None | Repair - type unknown |
| 17. JP (307) | M | 51-60 | 1-4 years | N | WRL | N | P | Airline Pilot | None | cycling | None | None | DHS |
| 18. DM (115) | F | 51-60 | 5-9 years | N | WRL | Y | N | Office Worker | None | outside | Osteopenia | None | Screws\IM nail |
| 19. MES (150) | F | 51-60 | 5-9 years | N | WRL | N | N | Office Worker | None | outside | None | None | Pins |
| 20. HEW (237) | F | 51-60 | 1-4 years | Ex | WRL | N | N | Office Worker | Osteopenia | outside | Osteopenia | None | Screws\IM nail |
| 21. MS (313) | M | 51-60 | 1-4 years | N | WRL | N | NK | Self-employed | None | cycling | None | None | Screws\IM nail |
| 22. PS (148) | F | 51-60 | 5-9 years | Ex | WRL | N | N | Office Worker | None | wheelchair | Osteoporosis | None | Plate |
| 23. AVS (289) | F | 29-40 | 1-4 years | Ex | Teetotal | N | N | Housewife-husband | Denerative neuro disorder | From step - kitchen surface - wheelchair | None | None | Screws\IM nail |
| 24. PST (322) | M | 41-50 | 1-4 years | N | WRL | N | C | Retired police- insurance investigator | None | cycling | None | None | Pins |
| 25. RP (167) | F | 51-60 | 5-9 years | N | WRL | Y | N | Retail Supervisor | None | outside | None | None | Part replacement |
| 26. MW (63) | F | 51-60 | 5-9 years | N | WRL | Y | Pets | Housewife-husband | Multiple | outside | Osteoporosis | None | THR |
| 27. ST (7) | M | 41-50 | 10 years | N | WRL | N | C | Self-employed | None | skating | None | None | Pins |
| 28. PBW (72) | M | 29-40 | 5-9 years | N | WRL | N | N | Science labs | None | cycling | None | None | Pins |
| 29. GA (84) | M | 29-40 | 5-9 years | Ex | ORL | N | C | Phramaceutical company | None | running | None | None | DHS |
| 30. JH (69) | M | 29-40 | 5-9 years | Ex | WRL | N | N | Disability | Osteogenesis Imperfecta | outside | None | None | Pins |
| 31. LL (241) | F | 41-50 | 1-4 years | Y | WRL | Y | P | Unemployed | Cerebral Palsy | café/shop | None | None | Multiple |
Abbreviations: S-Smoker, AI-Alcohol Intake, LA-Lives alone, D’s-Dependents, WRL-alcohol within recommended limits, ORL-alcohol outside recommended limits, Ex-exsmoker, THR-Total Hip Replacement, DHS-Dynamic Hip Screw, CVA-Cardiovascular Accident, Outside-public thoroughfare, CKD-Chronic Kidney Disease, IM nail- Intramedullary nail, RA-Rheumatoid Arthritis, N-NO, Y-Yes, C-Children, P-Parents, NK-Not known.
Table 2: Participant characteristics.
Participants were almost all employed, often had dependent children and/or elderly relatives and one third lived alone. Three participants required multiple operations and seven hip replacement and almost half of the group reported diagnosis of previously undiagnosed conditions such as osteopenia or osteoporosis as a result of the injury. Figure 4 details the themes and sub-themes.
Theme 1: Communication
This pervaded many aspects of participant’s recovery experiences.
Subtheme 1: Access to information and mixed messages: Receiving clear, accurate information, staff continuity and participants knowing who to ask for support was crucial. However poor communication and lack of information, including the need for urgent surgery, often added to participant distress.
Drawing on previous healthcare experience or professional knowledge helped participants’ understanding and reduced anxiety. This was not possible for all participants however and conflicting information left some fearful, with little confidence in their care.
Subtheme 2: Achieving shared understanding: Staff assumptions based on accepted fragility hip fracture norms often led to poor listening, and disbelief that minor trauma had caused severe injury:
‘…they couldn’t understand how I’d managed to break it…bear in mind I was only 54 and there was a lot of people in their 70s and 80s.
Lack of shared understanding and unfamiliarity with care processes underpinned many of the poor experiences described. This included staff assumptions regarding the absence of pain when in fact the participant did not understand how to use the self-administered analgesia on offer (Table 3).
| Time since injury | Number of participants |
|---|---|
| 1-4 yrs | 14 |
| 5-9 yrs | 13 |
| 10 yrs | 3 |
Table 3: Time since injury.
Theme 2: Experience of care
This ranged from ‘excellent’ to ‘appalling’ which encompassed pre-hospital, in-hospital and post discharge settings. The quality of care experience often varied between participants and at different points in the same story or patient journey.
Subtheme 1: Pre-hospital care: Whilst some participants were incapacitated and as a result received urgent medical care as is the norm for traumatic hip fracture, others responded differently. This resulted in delayed help seeking, unconventional routes to treatment and delayed diagnosis of up to six weeks, even after medical assessment. Participant responses post injury included driving themselves to hospital and continuing manual work before eventually seeking help, having underestimated injury severity or a reluctance to be off work and unable to meet family responsibilities. Many participants described being told they didn’t present ‘like a fractured hip’ (SJP) although for some this was unsurprising, which reflects current social norms regarding hip fracture:
‘…I don’t fit the classic demographic for that kind of injury…so it might not be the first port of call for diagnosis…people that are under 50…’ (GA).
Subtheme 2: In-hospital care: Hospital experiences varied greatly from being ‘well looked after’ (JD) to: ‘…quite horrendous… lack of care really…lack of humanity’ (RP).
Participants identified a lack of clear pathways for younger patients and staff assumptions based on accepted norms for fragility hip fracture. These included incorrect accusations regarding alcohol abuse.
Hospital stay varied from 24 hours to three months but was mostly seven days. Participants often felt out of place among much older people with the same injury but were all highly motivated to recover to pre-injury fitness. Participants found the extended period of reduced physical capability difficult as all were independent and mostly very active pre-injury. Hospital staff expected more of younger patients who perceived difficulties accessing adaptive equipment as ‘reverse ageism’:
‘I had to ask for a lot of stuff…whereas…when you hit a certain age and things get triggered…because…its more prevalent…you get targets…or pathways set up…you don’t fit… the pathway…cos you’ve got a neck of femur… in your 30s…’ (LS)
Primarily as a result of assumptions regarding the recovery needs-or lack of-of younger patients.
Subtheme 3: post-discharge care: Six to 12 week recovery was common but sometimes stretched to 18 months. The restricted weight-bearing commonly required for younger patients with this injury predominantly determined where participants recuperated but staff often overestimated the support available: ‘…I live on my own…there’s just a presumption that…you’re gonna have somebody at home that can care for you…’ (LS).
Often participants felt isolated, unprepared and struggled with everyday activities post discharge despite creative adaptation. Access to loan equipment varied, many borrowed or bought their own having been ‘fobbed off’ (RP).
Physiotherapy was variable. Some individuals had none:
‘…I asked about physiotherapy…said I…can’t do my job the way I am…he just dismissed it…said you’re a motivated man you won’t need it… I understand it’s all the cutbacks…but…there wasn’t no plan…you just go do it kind of thing…’ (MS). Others experienced rationing of resources so sourced and funded themselves. Most participants were pursing physical recovery goals over five years post-injury.
Bone density assessment was common, often triggered by the participant’s youth, but normal results surprised staff who expected abnormalities. One 33-year-old participant was initially refused assessment on age grounds then had screening she described as designed for the elderly and of little relevance to her situation. She was ultimately diagnosed with the bone density of an 80-year-old:
‘…there’s a gap…pre-menopausal…you’re a bit younger you don’t fit the criteria…we’ll wait until after your menopause…by then…you might be osteoporotic and then we’ll worry about it…’ (LS).
Follow up varied. Some participants felt abandoned:
‘…you’re on your own…no support really…you have to sort issues…two different systems…once you’re discharged from hospital they’ve done with ya…you’re in no-man’s land…’ (RP) or noted limited staff knowledge of this injury in younger people.
Theme 3: Impact on self
Subtheme 1: Emotional impact: Shock was very common. The experience challenged cyclist participants’ perception of themselves as very fit and used to falling without serious injury. Sustaining serious harm at low speed or from a minor fall was hard to rationalise for all participants and intensified its impact especially for individuals previously told fracture was unlikely given their clinical presentation or age. Unexpected news of urgent surgery and extended rehabilitation or subsequent permanent disability, further intensified the trauma. Sense-making was important in terms of helping participants come to terms with the injury: ‘…made me think…if I’d been in pain…like most people…that have a replacement hip…are…they’re really… pleased…cos it’s a new lease of life…to me it was the other way round…I was perfectly alright and I’d got to have one…’ (JD) and prompted one to challenge her own association of hip fracture with old age.
By far the commonest impact on self identified by participants was fear. Some participants described this as a psychological scar in addition to the physical scar left by the injury. Fear of falling was very common:
‘…for two years I became very very depressed…it has changed my life…I was quite an active person and now I have to think about everything…I have this fear of falling over…and that’s sad’ (MES).
Most participants remained very cautious walking, especially in bad weather, on poorly lit or uneven surfaces. Footwear was a big issue, particularly but not exclusively for females who wore: ‘…sensible, awful shoes…’ (SJP) post injury except for occasional, short trips when they risked: ‘…car to bar…’ (DM) or ‘dress’ shoes.
Avoidance was a frequently used strategy for dealing with fear. These included trying to ignore pain and not seeking help for ongoing symptoms; either because of fear of further surgery or poor care previously. Some participants travelled significant distances to avoid returning to the accident site. However, common risk management or avoidance strategies such as only undertaking ‘must do’ journeys, were not possible due to work and other commitments.
As time progressed a small number of participants had come to see the fall as a: ‘…blessing in disguise…’(GT) offering the chance to re-evaluate personal relationships and change workaholic or otherwise unhealthy lifestyles but this was uncommon.
Subtheme 2: Work and finances: Often the first period of extended sick leave, all participants pursued a quick return to mitigate lost income and regain the self-worth, normality and social interaction work offered. Returning was difficult however and some participants described feeling like a bag of nerves, having to start all over again. Those able to work from home during recovery maintained their work identity but still worried about returning. Staged return was common although many people still experienced difficulties years later:
‘…I was still in such a lot of pain…I struggled…even now, sometimes it’s so hard…I just keep going because I need my wages…know I’m not as capable as everybody else…like I let the side down…feel like I’ve aged fifteen years…’ (DH).
Sick pay or competitors who caretaker-ed businesses for self-employed participants who would otherwise have gone bankrupt were crucial: ‘…it could have been a whole lot worse… you’ve got the mortgage…food and what have you…without that money…’ (PB).
Participants had never previously considered potential inability to work, therefore some re-structured finances to protect their capacity to support themselves or dependents.
Subtheme 3: Identity: Enduring altered self-concept was common. The injury prompted a new perspective and stimulated early retirement. Positive new identities emerged as some participants became advocates for others or organisers of their own care, feeling let down by a lack of rehabilitation support: All were highly motivated to prevent physical dependence, enable return to previous activities and avoid disability yet friends and family expected quicker recovery:
‘…”so and so’s in their 70s…had a hip replacement and they’re doing better than you”…that’s the last thing you want…is being told that…’ (LS)
This reflects the perhaps understandable but potentially inappropriate application of accepted social norms for hip fracture recovery to this younger client group, which participants reported as having a detrimental emotional impact as they actively pursued recovery and the return to independence this represented.
Mourning pre-injury self was common:
‘…it’s…like a loss of your femininity having to wear awful, sensible, flat shoes…’ (SJP).
Yet participants wanted to be perceived as normal, often still actively hiding limited mobility several years post injury. This active concealment of enduring limitations may further reinforce the invisibility of the impact of hip fracture in this younger group and their long-term recovery needs.
Theme 4: Impact on others
Wide-ranging, long-term impact on family members, co-workers and friends was identified.
Subtheme 1: Practical impact: Providing practical help during extended periods of reduced mobility affected relatives, resulting in substantial disruption as they juggled caring with other responsibilities:
‘…stayed at my parents’…for eight months in my bedroom because I couldn’t negotiate the stairs…have not seen my house since I did this…very near a whole year now…my husband comes to visit…he works long hours…and he wouldn’t be around…my husband will take me to Morrisons…and to the pub…there’s no way my mother could do that…’ (GT).
Subtheme 2: Psychological impact: Often in the context of relatives fearing another fall, participants vigorously pursued independence:
‘…she [daughter] never knew I was having baths…she used to phone…to make sure I was ok…if she’d known…she used to worry about me going up and down the stairs…’ (MES).
Such psychological impact also extended to children and grandchildren indicating widespread psychological impact within participants’ personal and wider social networks as a result of the injury.
Subtheme 3: Impact on relationships: Some were enhanced, for example by time off work enabling the development of a more balanced work perspective and richer personal relationships. Others were disrupted however, often due to differing expectations of recovery based on common social norms associated with hip fracture. This led to examples of lost friendship and social networks as well as conflict within close personal relationships. Perceived risk of further falls caused relationship difficulties. Resuming cycling for example was often a contentious issue within close relationships for those injured in this way: The injury was also a catalyst for major life decisions by members of participants’ networks however: ‘…its brought home to her how easy it is…how it can change your life…so she decided…she would take her retirement while she was…fit and able…it shook her… she thought if I’d have broke my neck doing that [climbing walls]…that was understandable…but not… walking through a bus station…’ (MES).
This indicates participants’ injury experiences also challenged those around them to re-evaluate their own identities and expectations of their future.
Theme 5: Moving forward
Subtheme 1: Staying active: All participants identified resuming regular exercise as important. However, they risk assessed activities post injury and either avoided participating or adapted them. They recounted no longer daring to go out alone for fear of falling but were often unable to voice such feelings with others:
‘…its very difficult to explain to anybody…what happens to me…I become very vulnerable…but I couldn’t say to anybody I am absolutely terrified, petrified…’ (MES).
Finding time for exercise was difficult, particularly following return to work, due to fatigue from residual pain and reduced physical stamina. This commonly persisted for years.
Subtheme 2: Residual limitations: The few participants reporting little pain and near normal function within two years of injury also described physical symptoms and strategies for accommodating the injury. This indicates potential residual impact they did not define as such. Most of these individuals had fallen during regular sporting activities such as cycling and used these to support recovery. Their stories also focused more on physical than psychological or social impact.
The limited effectiveness of current patient reported outcome measures for use with younger hip fracture patients was often highlighted however:
‘…the scale…its quite simplistic…yes I can put my shoes and socks on and yes I can walk…but when you’re in your 30s three miles doesn’t seem a lot…because it’s measuring the hip…it doesn’t pick up on the problems you’re getting elsewhere…its all the other impacts that it has on you…’ (LS).
This is not surprising as such measures were designed for a different patient group ie. post hip replacement for degenerative conditions rather than traumatic injury. However, enduring pain, stiffness and limping were very commonly reported by participants. A range of coping strategies were described, with many participants avoiding prescribed analgesia preferring to use non-pharmaceutical relief or over the counter analgesia. This autonomous, self-care further reduces the visibility of young hip fracture patient recovery needs as measured by NHS usage and the wider social discourse.
Subtheme 3: Concerns for the future: Despite a positive outlook many participants faced an unforeseen, more difficult future often linked to altered self-concept post injury. They focused on maintaining long term independence and maximising bone health. Most were anticipating further, sometimes multiple, operations. Those with hip replacement particularly were aware that the effective life of the prosthesis may be shortened by the higher activity levels arising from their younger age. They were also concerned about the greater risks associated with the multiple revision surgeries that would be necessary as a result of their relative youth although this was mixed with optimism that future technological advances could mitigate these. An uncertain future however created fears regarding inability to continue a chosen career and worry about maintaining physical or financial independence and ability to support a growing family. This resulted in actions such as:
‘…getting myself into a position where I’ve got support systems…financial outgoings are minimal…I’ve got something to fall back on...’ (SF).
Maintaining bone health particularly concerned the many participants, for whom compromised bone density was discovered. The challenges of balancing weight-bearing exercise to promote healthy bone with persistent pain and other mobility limitations, was a key finding. Participants reported trying to balance positive focus and conscious action with putting such concerns to the back of their mind to enable day-to-day life.
Discussion
These findings predominantly challenge accepted notions that fragility hip fracture recovery in young people is unproblematic, possibly because they offer the first, long term, patient perspective on this topic.
Participants’ experiences reflect their ‘difference’ to what they and others expected. This concerns professional and social norms regarding fragility hip fracture as an injury of old age, caused by high velocity injury or co-morbidities and lifestyle factors such as alcohol abuse. This study does not fully support these, but rather reflects previous evidence [26,44] that the impact of fragility hip fracture in young people has been significantly underestimated. This study also supports previous research that normal bone density can provide false reassurance and should therefore be supplemented by other measures to provide valid assessment [15,45].
The long-term physical, psychological and sociological sequelae affecting the person injured and substantial impact on participants’ social networks and family carers this study found, challenge common perceptions that young hip fracture patients recover quickly, supported by active social networks. These ‘collateral consequences’, which extend beyond the physical to financial and other psychosocial impact, supports previous research with ex-offenders [46]. Furthermore, the limited effectiveness of commonly used patient reported hip fracture outcome measures this study identified indicates further work is needed.
Hip fracture patients are not a homogenous group [47], which may explain the varied experiences reported. Pain severity [48,49] and post injury function and quality of life [50] vary by surgical procedure. Similarly, younger people’s experience of internal fixation following sudden, traumatic injury from a minor fall will likely differ from that of elders following planned hip replacement. Inadequacies identified in the hip fracture care pathway, because participants did not fit professional norms for this injury, support previous findings [28] that care pathways do not always live up to expectations.
Excepting some cyclists, this study strongly supports previous research identifying fear of falling, loss of confidence and Post Traumatic Stress Disorder in the elderly post hip fracture. This study uncovered two further silences: hidden, compromised physiology in participants who were otherwise fit and well; and a gap in road accident reporting regarding cyclists. Both may exacerbate the under-recognition of fragility hip fracture in the under 60s. In addition, participants’ relatively short hospital stay, largely self-supported rehabilitation and concealment of ongoing physical and psychological sequelae may further reduce the visibility of their needs.
Involving only one English region limits transferability and including members from additional social network groups such as retail staff and participants’ spouses/partners in the Collective Voices process could have provided additional perspectives. Lack of method triangulation was mitigated by member-checking, a transparent audit trail and structured approach to data analysis, seeking out negative cases and researcher reflexivity, to ensure the study’s trustworthiness overall [40]. The Silences Framework [31] was found to be wholly appropriate for guiding this study although some lessons were learned from its first application in an acute care/rehabilitation setting. These and some suggested revision of the framework are discussed in detail elsewhere [51].
Conclusion
These findings challenge the dominant discourse concerning fragility fracture. The considerable burden of fragility hip fracture in the elderly explains its prominence and short-term outcomes focus. This study however, indicates these do not reflect the recovery experiences or needs of younger patients despite the changing aetiology of fragility hip fracture and projected increase in the under 60s. Further research is required to test transferability to a larger population and develop more appropriate patient reported outcome measures for this client group. Furthermore, economic evaluation of fragility hip fracture in the under 60s is needed along with evaluation of the impact on families and wider social networks, including their ability to provide care.
Reviewing the appropriateness of the hip fracture care pathway for young patients who do not fit widely accepted norms for this injury is also warranted. Similarly extending national hip fracture databases to ensure universal inclusion of the under 60s in all countries would reduce the invisibility and current marginalisation of this sub-set of the fragility hip fracture population and better inform future nursing practice and policy.
Meanwhile, nurses must adopt an holistic, individualised approach to caring for younger hip fracture patients. Nurses must also be cognisant of the limited relevance of standard patient reported outcome measures for this younger population and listen more actively to patients to prevent making inaccurate assumptions concerning for example the injury causation, recovery and support needs of younger hip fracture patients fuelled by the prevailing professional and social norms regarding this injury.
Declarations
Authors acknowledge the support of study participants who willingly gave their time and experiences in participating in the study. Authors acknowledge and thank Ms Louise Donnison for providing a patient perspective throughout the design and delivery of the study. Further acknowledge Mr Ben Ollivere and Nottingham University Hospitals NHS Trust for providing clinical advice and supporting study recruitment and data collection. Extend thanks to Teesside University for providing study time for the first author. All the authors read and approved the final manuscript and there are no conflicts of interest and research work is non-funded.
References
- Morse JM, Brien OB (1995) Preserving self: from victim to patient, to disabled person. J of Adv Nurs 21: 886-896.
- Olsson LE, Nystrom AEM, Karlsson J, Ekman I (2007) Admitted with a hip fracture: patient perceptions of rehabilitation. J Adv Nurs 16: 853-859.
- Proctor R, Wade R, Woodward Y, Pendleton N, Baldwin R, et al. (2008) The impact of psychological factors in recovery following surgery for hip fracture. Disabil and Rehabil 30: 716-722.
- Currie CT, Hutchinson JD (2005) Audit, guidelines and standards: Clinical governance for hip fracture care in Scotland. Disabil and Rehabil 27: 1099-1105.
- Visschedijk J, Achterberg W, Van Balen R, Hertogh C (2010) Fear of falling after hip fracture: A systematic review of measurement instruments, prevalence, interventions and related factors. J Am Geriatr Soc 58: 1739-1748.
- Gunasekera N, Boulton C, Morris C, Moran C (2010) Hip fracture audit: the Nottingham experience. Osteoporos Int 21: S647-653.
- Santamaria N, Houghton L, Kimmel L, Graham A (2003) Clinical pathways for fractured neck of femur: a cohort study of health related quality of life, patient satisfaction and clinical outcome. Aust J Adv Nurs 20: 24- 29.
- Parsons N, Griffin XL, Achten J, Costa ML (2014) Outcome assessment after hip fracture: is EQ-5D the answer? Bone Joint Res 3: 69-75.
- Holt G, Smith R, Duncan K, Hutchison JD, Reid D (2009) Changes in population demographics and the future incidence of hip fracture. Injury 40: 722- 726.
- Leigheb F, Vanhaecht K, Sermeus W, Lodewijckx C, Deneckere Set al. (2013) The effect of care pathways for hip fractures: a systematic overview of secondary studies. Eur J Orthop Surg Traumatol 23: 737- 745.
- NICE Clinical guidelines (2011) The Management of Hip Fracture in Adults (CG124). Crown, London, UK.
- Archibald G (2003) Patients’ experiences of hip fracture. J Adv Nurs 44: 385-392.
- Balen VR, Bot EM, Steyerberg EW, Cools HJM, Habbema JD (2003) Quality of life after hip fracture: A comparison of four health status measures in 208 patients. Disabil Rehabil 25: 507-519.
- Partridge M, Marsh D (2007) A UK national hip fracture database. J Orthop Nurs 11: 122- 123.
- Oetgen ME, Miki RA, Smart LR, Lindskog DM (2009) Evaluation of bone mineral density and metabolic abnormalities associated with low-energy hip fractures. Curr Orthop Pract 20: 674-668.
- Chesser TJS, Handley R, Swift C (2011) New NICE guideline to improve outcomes for hip fracture patients. Injury 42: 727- 729.
- HQIP (2014) National Hip Fracture Database: Anaesthesia Sprint Audit of Practice (ASAP) report 2014. Royal College of Physicians, London.
- Plant F (2010) Personal Communication Project Co-ordinator, NHFD . National Hip Fracture Database for England, Wales, NI and the Channel Islands.
- Gjertsen JE, Engesaeter LB, Furnes O, Havelin LI, Steindal K (2008) The Norwegian Hip Fracture Register: : experiences after the first 2 years and 15,576 reported operations. Acta Orthop 79: 583-593.
- Australia and New Zealand Hip Fracture Registry (2012) Towards a National Hip Fracture Registry Issue 1 Jan 2012 Australia: Australia and New Zealand Hip Fracture Registry. Available from https://www.anzona.net/documents/2012_jan_newsletter%20.pdf
- Osteoporosis in the UK at Breaking Point (2010) A report on the current management of postmenopausal women with osteoporosis in the UK. The Patients Association.
- Young Y, Resnick B (2009) Don’t worry, be positive: improving functional recovery 1 year after hip fracture. Rehabil Nurs 34: 110-117.
- Vilardo L, Shah M (2011) Chronic pain after hip and knee replacement. Techniques in Regional Anaesthesia and Pain Manag 15: 110-115.
- Schiller C, Franke T, Belle J, Gould SJ, Sale J (2015) Words of wisdom - patient perspectives to guide recovery for older adults after hip fracture: a qualitative study. Patient Prefer Adherence 12: 57-63.
- Holt G, Smith R, Duncan K, Hutchison JD, Gregori A (2008) Epidemiology and outcome after hip fracture in the under 65s – evidence from the Scottish hip fracture audit. Injury 39: 1175-1181.
- Boden SD, Labropoulos P, Saunders R (1990) Hip fractures in young patients: is this early osteoporosis? Calcif Tissue Int 46: 65-72.
- WHO (2003) The burden of musculoskeletal conditions at the start of the new millennium. Report of a WHO Scientific Group. World Health Organisation, Geneva.
- Vanhaecht K, Semeus W, Peers J, Lodewijckx C, Deneckere S (2012) The impact of care pathways for patients with proximal femur fracture: rationale and design of a cluster-randomized controlled trial. BMC Health Serv Res 12: 124-131.
- Cumming RG, Nevitt MC, Cummings SR (1997) Epidemiology of hip fractures. Epidemiologic Reviews 19: 224-257.
- Janes G, Serrant L, Sque M (2018) Silent slips, trips and broken hips in the under 60s: A review of the literature. Int J Orthop Trauma Nurs 30: 23-30.
- Green SL (2011) The Sound of 'Silence': A Framework for researching sensitive issues or marginalised perspectives in health. J Res Nurs 16: 347-360.
- Pownall E (2004) Using a patient narrative to influence orthopaedic nursing care in fractured hips. J Orthop Nurs 8: 151-159.
- Denzin NK, Lincoln YS (1994) Handbook of Qualitative Research. Sage, London.
- Lincoln YS, Lynham SA, Guba EG (2011) Paradigmatic controversies, contradictions, and emerging influences, revisited. In: Denzin NK, Lincoln YS (eds.) The SAGE handbook of qualitative research. Sage, London.
- Connelly L, Yoder L (2000) Improving qualitative proposals: Common problem areas. Clin Nurse Spec 14: 69-74.
- Moppett IK, Parker M, Griffiths R, Bowers T, White SM (2012) Nottingham hip fracture score: longitudinal and multi-case assessment. Br J of Anaesth 109: 546-550.
- Parker MJ, Currie CT, Mountain JA, Thorngren KG (1998) Standardised audit of hip fracture in Europe (SAHFE). Hip Int 8: 10-15.
- Huberman AM, Miles MB (2002) The qualitative researcher’s companion. Sage, London.
- Braun V, Clarke V (2006) Using thematic analysis in psychology. Qual Res Psychol 3: 77-101.
- Lincoln YS, Guba EG (1985) Naturalistic Inquiry. Sage, California.
- Green J, Thorogood N (2014) Qualitative Methods for Health Research (3rd edn). Sage, London.
- Pelias RJ (2011) In: Denzin NK and Lincoln YS (eds.) Writing into Position: Strategies for composition and Evaluation (4th edn.) The SAGE Handbook of Qualitative Research Sage, London, pp: 659-668.
- Asselin ME (2003) Insider research: issues to consider when doing qualitative research in your own setting. J Nurses Staff Dev 19: 99-103.
- Karantana A, Boulton C, Bouliotis C, Shu SSK, Scammell BE, et al. (2011) Epidemiology and outcome of fracture of the hip in women aged 65yrs and under: A cohort study. J Bone Joint Surg 93: 658- 664.
- Aspray TJ (2013) New horizons in fracture risk assessment. Age and Ageing 42: 548-554.
- Thomas T, Hebenton B (2013) Dilemmas and consequences of prior criminal record: a criminological perspective from England and Wales. Crim Justice Stud 26: 228-243.
- Eastwood EA, Magaziner J, Wang J, Silberzweig SB, Hannan EL, et al. (2002) Patients with hip fracture: subgroups and their outcomes. J Am Geriatr Soc 50: 1240-1249.
- Foss NB, Kristensen MT, Palm H, Kehlet H (2009) Postoperative pain after hip fracture is procedure specific. Br J Anaesth 102: 111-116.
- Kondo A, Sada K, Ito Y, Yamaguchi C, Horii N, et al. (2014) Difficulties in life after hip fracture and expected hospital supports for patients and their families. Int J of Orthop Trauma Nurs 18: 191-204.
- Coughlin TA, Janes G, Nightingale J, Moran CG, Forward D, et al. (2016) Outcomes in young hip fracture patients. Orthopaedic Trauma Association Annual Meeting. Maryland, USA.
- Janes G, Serrant L, Sque M (2018) Screaming Silences: lessons from the application of a new research framework. Nurse Res (ahead of print).
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences