Difficult Airway Management in Recurrent Respiratory Papillomatosis Patient during CO2 Laser Surgery
Peña-de-Buen N*, Araujo-Vázquez M, Gil-Marín F, Gracia-Roche A, Toro-Núñez M and Martínez-Nuez S
Anesthesiology, Reanimation and Pain Therapy Department, Hospital Universitario Miguel Servet. Zaragoza, Spain
- Corresponding Author:
- Peña-de-Buen Natalia
Anesthesiology, Reanimation and Pain Therapy Department
Hospital Universitario Miguel Servet, Zaragoza, Spain
E-mail: nataliapdb@hotmail.es
Received date: August 19, 2017; Accepted date: August 28, 2017; Published date: September 07, 2017
Citation: Peña-de-Buen N, Araujo-Vázquez M, Gil-Marín F, Gracia-Roche A, Toro- Núñez M, et al. (2017) Difficult Airway Management in Recurrent Respiratory Papillomatosis Patient during CO2 Laser Surgery. Res J Ear Nose Throat. Vol. 1 No. 1:1
Abstract
Title: Difficult Airway Management in Recurrent Respiratory Papillomatosis Patient during CO2 Laser Surgery: A Case Report. Background: Recurrent respiratory papillomatosis is a condition that can quickly compromise a previously asymptomatic airway with risk of obstruction.
Case report: Laser CO2 surgery on a respiratory recurrent papillomatosis patient which posed a challenge in airway management. Conclusion: This case highlights a group of patients which would have a difficult airway. Careful planning is essential before intubation attempts and, to be successful, it is imperative to plan effective management.
Keywords: Recurrent respiratory papillomatosis; CO2 laser surgery; Difficult airway
Abbreviations: ASA: American Society of Anesthesiologists; DA: Difficult Airway; ENT: Ear-Nose-Throat; ET: Endotracheal Tube; RRP: Respiratory Recurrent Papillomatosis
Keywords
Recurrent respiratory papillomatosis; CO2 laser surgery; Difficult airway
Abbreviations
ASA: American Society of Anesthesiologists; DA: Difficult Airway; ENT: Ear-Nose-Throat; ET: Endotracheal Tube; RRP: Respiratory Recurrent Papillomatosis
Introduction
Recurrent Respiratory Papillomatosis (RRP) is the most prevalent condition involving benign laryngeal growths [1] and the World Health Organization (WHO) considers this infection to be an epidemic of high relevance to public health [2]. RRP is a chronic condition characterized by benign, wart-like growths in the upper airway caused by human papillomavirus infection [3,4]. These warts show a strong predilection for the larynx, including vocal chords [4].
RRP follows an unpredictable course with significant impact on quality of life, associated with morbidity and possibility of oropharyngeal carcinoma development [2-4]. Moreover, rapid growth of papilloma can quickly compromise a previously asymptomatic airway with risk of obstruction [5,6]. This presents a challenge for both the Ear-Nose-Throat (ENT) surgeon and the anesthesiologist due to its recurring nature, possibility of progression to malignancy and Difficult Airway (DA) management.
We describe a case of DA management in a patient diagnosed with RRP affecting his vocal chords.
Case Report
We present the case of a 107 kg 55 years old male patient, with a Body Mass Index (BMI) of 34.96. He has been diagnosed of RRP. He was scheduled to be surgically intervened after being treated on several occasions with intralesional cidofovir without positive outcome. No adverse events were reported intraoperatively or postoperatively in those interventions.
The patient consulted about dysphonia of several months duration. The ENT surgery team decided treatment with CO2 laser surgery. As medical background, 5 intralesional injections of cidofovir were performed on his RRP with no adverse effects reported. He did not take any regular medical treatment and had no history of drug allergies. Analytical, radiological and electrocardiographic findings were within normal range. As predictors of DA, obesity and RRP were found.
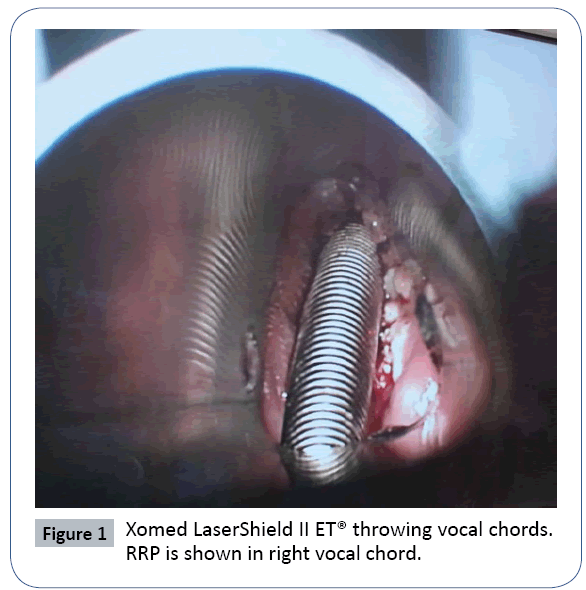
The day of the procedure, premedication with midazolam 0.03 mg/ kg was administered. In the operating room, non-invasive blood pressure, electrocardiogram, pulsioximetry, bispectral index (BIS) and Train of Four (TOF) were monitored. Preoxygenation with face mask was performed for 10 min. Anesthesia induction was carried out with intravenous administration of 200 μg of fentanyl, 3 mg/kg propofol and rocuronium as muscle relaxant at 0.6 mg/kg. In preparation for the event of a DA, we made sure appropriate devices were at our disposal, including a 6 size Xomed LaserShield II Endotracheal Tube (ET) (Xomed, Inc., Jacksonville, FL)® suitable for laser surgery. Direct laryngoscopy revealed an exophytic growth on the right vocal chord, which, despite adequate muscle relaxation, made impossible the progression of the ET. We took the decision to use a Frova Intubating Introducer (Cook Medical, Brisbane, Australia)® and a 5 size reinforced ET to overpass the vocal chords and secure the airway. As CO2 laser surgery cannot be performed without the appropriate ET, we decided to replace the reinforced ET for a 5.5 size Xomed LaserShield II ET®over a Cook Airway exchange catheter (Cook Medical Incorporated, Bloomington, IN, USA)®. We needed to use Magill forceps to guide the ET through the patient’s stenosis. The double cuff was filled with saline and adequate ventilation was confirmed. We maintained the anesthetic depth with total intravenous anaesthesia during the airway management process, using 6 mg/kg/h propofol and 0.1 μg/kg/min remifentanil.
Presenting normal ventilatory and circulatory parameters, we decided to proceed with the surgical procedure. On the image captured, the correct placement of the Xomed LaserShield II ET® was verified and the exophytic growth on the right vocal chord was shown (Figure 1). This one hindered the tracheal tube advancement.
As adjunct drugs, we administered corticoids (8 mg of dexamethasone), 40 mg of omeprazole, 1 g of acetaminophen and 50 mg of dexketoprofen. Adequate muscle relaxation registered on TOF made repeated muscle relaxant administration unnecessary.
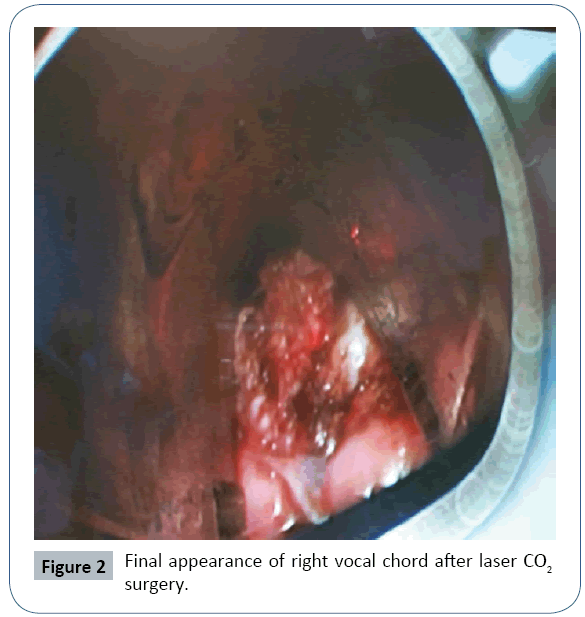
After finishing the procedure (Figure 2), extubation was performed in the operating room with adequate parameters: BIS>85, 4 responses on TOF, adequate spontaneous ventilation and good reaction to verbal orders.
No adverse events were observed in the immediate postoperative period and there was not reported recurrence or progression to malignancy with evidence of cure.
Discussion
DA is one of the well-known life-threatening events associated with general anesthesia. It usually happens during induction, while attempting to ventilate or inserting the ET and deteriorating respiratory compromise may appear [7,8].
A DA is defined by the American Society of Anesthesiologists (ASA) as the clinical situation in which a conventionally trained anesthesiologist experiences difficulty with face mask ventilation of the upper airway, difficulty with tracheal intubation or both [9]. In the Practice Guidelines published by the ASA, the DA represents a complex interaction between patient factors, clinical setting, and the skills of the practitioner [9]. In ENT surgery, airway difficulty is a particularly relevant matter due to its high incidence. A study made by Ayuso et al. found that in ENT surgery, difficult tracheal intubation ranges goes from 8 to 10% and the incidence rises to 28% when the patient presents a tumor of the airway. [10].
In the operating room, the ENT surgeon and the anesthesiologist have very different and oftentimes apparently conflicting needs with regards to the airway. For ENT surgeons, the critical issue is to obtain the widest and least impeded view of the larynx possible [11]. They also require that the larynx be completely still during more delicate surgical movements and yet they may wish to see the larynx spontaneously moving at other times [11].
Anesthesiologists need complete control of the airway, including controlled ventilation, as well as the capacity to continuously monitor the patient’s physiological responses [11].
RRP is one of the ENT pathologies which can be involved in making a DA. This disease has a chronic unpredictable course and presents airway obstruction risk [3,5,6]. Various treatments are employed to deal with RRP, and recently new therapeutic devices such as intralesional cidofovir or bevacizumab have been introduced [3,5,12,13]. Intralesional cidofovir administration is widely used now and complete remission of the disease with reduction in the risk of relapse has been observed in a high percentage of cases [3,5,13]. However, in our case, cidofovir administration failed in producing satisfying results and it was decided therefore to use CO2 laser on the warts as a therapeutic alternative.
CO2 laser microsurgery is based on lesion resection to maintain airway patency and improve voice quality [5,14]. Although outcomes have been favorable, it has several drawbacks, such as the need for general anesthesia and enough experience of the surgeon in laser handling to avoid injury of unaffected areas or explosion when there is contact with anesthetic gases [14]. Furthermore, it is necessary to use tracheal tubes designed for laser surgery, cuff filling with saline and 0.3-0.4% fraction of inspired oxygen ventilation [15-17].
Regarding the airway, our patient did not have any background of difficult tracheal intubation in previous anesthetic procedures, and the only DA predictor he had was obesity. However, RRP was described as a difficult tracheal intubation predictor and therefore DA equipment was prepared with anticipation.
As it is indicated by the 2013 ASA Practice Guideline, adequate preparation in the event of possible DA is necessary [9]. This basic preparation includes availability of equipment for management, informing the patient with a known or suspected DA, assigning an individual to provide assistance when a DA is encountered, pre-anesthetic pre-oxygenation by mask and administration of supplemental oxygen throughout the process of DA management [9].
In our case the patient was initially preoxygenated using face mask. After anesthetic induction and achievement of apnea, manual ventilation with face mask did not pose any difficulty, so it was performed an intubation with Macintosh laryngoscope. Grade II Cormack-Lehane was visualized, and also an exophytic tumor on the right vocal chord which caused glottic stenosis and difficulty the advancement of the ET chosen. According to the lack of difficulties in ventilation with face mask, the DA situation did not classify as an emergency [9]. The ASA DA algorithm notes that when initial intubation attempts are unsuccessful and face mask ventilation is adequate, the next step are alternative approaches to intubation [9]. For this reason, a Frova Intubating Introducer was used as an alternative method to pass through the vocal chords and to place, in a successfully way, a smaller size ET over it.
Later, a Cook Airway Exchange Catheter® was used to place the Xomed Lasershield II ET® (needed to allow the utilization of CO2 laser), ensuring an adequate airway control. A temporary airway may have been achieved with an airway exchange catheter, as it was done correctly in our clinical case. Such devices have been described as an alternative to maintain the airway patency in patients with laryngeal papillomatosis in the elective and emergency setting [18].
Several articles have described similar DA situations in RRP patients as the one that our work group presents. The Royal National Throat Nose and Ear Hospital from London showcased in their article the subglottic jet technique in 352 patients treated with microlaryngoscopy, 89 of whom had DA [11]. Authors note that for the laryngologist this technique allows for a minimally impeded airway and reduces movement of the larynx considerably [11]. Moreover, for the anesthesiologist, it is more secure than supraglottic jet ventilation [11].
Other authors such as George et al. in 2015, described the use of fiberoptic intubation, which can allow successful passage in cases where the glottic opening is narrowed [19]. As in their case, other methods like jet ventilation could be potentially hazardous [19]. Other techniques, like formal tracheostomy, should be avoided if possible in these patients, as it may predispose to distal dissemination of papillomata previously confined to the larynx and a consequent worsening of long term prognosis [7].
Conclusion
RRP poses a challenge for both the ENT surgeon and the anesthesiologist. It is a prevalent disease with high rate of relapse and malignancy risk, which needs to be surgically operated in many cases. This case highlights a group of patients which would be difficult to intubate, due to subglottic stenosis or airway edema. Careful planning is essential before intubation attempts and, to be successful, it is imperative to plan effective management keeping good communication and flexibility in decision-making [19].
Acknowledgement
The support of Anesthesiology, Reanimation and Pain Therapy Department and ENT Department (Hospital Universitario Miguel Servet) has been vital for the realization of this project.
Funding
No fundings were used to support the work.
Competing and Conflicting Interests
There are no competing or conflicting interests.
References
- Soto-Posada MI, Tamez-Velarde M, Domínguez-Sosa FR (2014) Recurrent respiratory papillomatosis, results of the treatment with CO2 laser in a referente center experience of six years. An Orl Mex 59: 92-101.
- Gama Longubuco CE, Barroso HL, Sampaio F, Petillo CR, Silva N, et al (2014) Dysphonia as a sign of HPV laryngeal infection: A case report. BMC Res Notes 7: 898.
- Fusconi M, Grasso M, Greco A, Gallo A, Campo F, et al. (2014) Recurrent respiratory papillomatosis by HPV: Review of the literature and update on the use of cidofovir. Acta Otorhinolaryngol Ital 34: 375- 381.
- Benedict PA, Ruiz R, Yoo M, Verma A, Ahmed OH, et al. (2017) Laryngeal distribution of recurrent respiratory papillomatosis in a previously untreated cohort. Laryngoscope.
- Recurrent respiratory papillomatosis by HPV: Review of the literature and update on the use of cidofovir
- Sidle DM, Haines GK (2002) 3rd, Altman KW. Bilateral vocal process papillomas: Report of a case. Ear Nose Throat Journal 81:790-791.
- Carroll CD, Saunders NC (2002) Respiratory papillomatosis: A rare cause of collapse in a young adult presenting to the emergency department. Emerg Med J 19: 362-365.
- Workeneh SA, Gebregzi AH, Denu ZA (2017) Magnitude and predisposing factors of difficult airway during induction of general anaesthesia. Anesthesiol Res Pract 2017: 1-6.
- Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, et al (2013) American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway. An update report by the american society of anesthesiologists task force on management of the difficult airway. Anesthesiology 118: 251-270.
- Ayuso MA, Sala X, Luis M, Carbó JM (2003) Predicting difficult orotracheal intubation in pharyngo-laryngeal disease: Preliminary results of a composite index. Can J Anaesth 50: 81-85.
- Rubin JS, Patel A, Lennox P. Subglottic (2005) Jet ventilation for suspension microlaryngoscopy. J Voice 19: 146-150.
- Zur KB, Fox E. Bevacizumab (2017) chemotherapy for management of pulmonary and laryngotracheal papillomatosis in a child. Laryngoscope 127: 1538-1542.
- Brunetto B, Zelada U (2007) Use of cidofovir in recurrent respiratory papillomatosis. Rev Bibliográfica Rev Otorrinolaringol Cir Cabeza Cuello 67: 153-156.
- Gutierrez C, Monerris E, Duran MD, Sancho M, Gras JR (2016) Papillomas and laryngeal papillomatosis. Treatment with CO2 laser surgery. Our experience over 15 years. Acta Otorrinolaringol. Esp. 61: 442-427.
- Wolf GL, Simpson JI (1987) Flammability of endotracheal tubes in oxygen and nitrous oxide enriched atmosphere. Anesthesiology 67: 236-239.
- Ossoff RH (1989) Laser safety in otolaryngology head and neck surgery: Anesthetic an educational considerations for laryngeal surgery. Laryngoscop 99: 1-26.
- Llamas I, Wolfschoon A, Rodriguez E (2007) Incendio de un tubo endotraqueal durante traqueostomia. Rev colomb Anestesiol 35: 75-77.
- Hulme GJ, Blues CM (1999) Acromegaly and papillomatosis: Difficult intubation and use of the airway exchange catheter. Anaesthesia 54: 787-789.
- George J, Kader JA, Arumugam S, Murphy A (2015) Successful intubation of a difficult airway due to a large obstructive vocal cord polyp augmented by the delivery of a transtracheal injection of local anaesthetic. BMJ Case Rep 1.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences