Wearable Sensors for Vestibular Rehabilitation: A Pilot Study
Martini, DN1,2,4*, Pettigrew, NC1,2,3, Wilhelm, JL1,2, Parrington L1,2, and King, LA1
1Department of Neurology, Oregon Health & Science University, Portland, OR, USA
2Veterans Affairs Portland Healthcare System, Portland, OR, USA
3Center for Regenerative Medicine, Oregon Health & Science University, Portland, OR, USA
4Department of Kinesiology, University of Massachusetts Amherst, USA
- *Corresponding Author:
- Dr. Douglas N. Martini
Department of Kinesiology
University of Massachusetts
Amherst, USA
Tel: 413-545-7834
E-mail: dmartini@umass.edu
Received Date: March 25, 2021; Accepted Date: July 12, 2021; Published Date: July 19, 2021
Citation: Douglas NMW, Natalie CP, Jennifer LW, Lucy P, Laurie AK (2021) Wearable Sensors for Vestibular Rehabilitation: A Pilot Study. J Physiother Res Vol.5 No.8:31.
Abstract
Background: Vestibular rehabilitation is used to treat dizziness and balance disorders with varying degrees of success. One limitation in current clinical vestibular rehabilitation practice is that head and trunk movement lack objective quantification. Wearable inertial measurement units (IMUs) provide objective measures, which could help determine dosing factors and improve vestibular rehabilitation efficacy. The purpose of this study was to explore IMU- quantified values for cervical and trunk range of motion (ROM) and peak angular velocity during four common vestibular rehabilitation exercises and to determine the consistency of participant performance between visits.
Methods: Eighteen participants (28.7 (5.1) years, 9 female) completed two, 30-second trials of four common vestibular rehabilitation exercises (gaze stabilization, visual motion sensitivity, static balance with head turns, and walking with head turns) on two separate days (11.1 (7.6) days between). Two IMUs, forehead and sternum, quantified cervical and trunk ROM and peak angular velocity in the transverse and sagittal planes. Intraclass correlation models were used to assess the between visit reliability of participants’ exercise performance.
Results: Mean cervical ROM ranged from 64.2-175.9° (transverse) and 43.9- 106.5° (sagittal) across the four exercises, mean trunk ranged from 1.33-169.2° (transverse) and 2.8-83.9° (sagittal). Mean cervical peak angular velocity ranged from 223.8-387.4°/s (transverse) and 170.4-256.8°/s (sagittal) across the four exercises, mean trunk ranged from 6.1-211.1°/s (transverse) and 15.2-140.2°/s (sagittal). Participant performance consistency ranged from moderate to excellent (ICC [3, 2] 0.57-0.93) for ROM and peak angular velocity.
Conclusion: These results suggest that clinicians could use IMUs to objectively quantify patient performance and progress, but reliability may be exercise specific.
Keywords
IMU; Intraclass correlation; Peak angular velocity; ROM
Introduction
Balance impairments are common, with over 33 million adults in the United States reporting dizziness or balance problems per year and roughly 13% of neurological patients in emergency departments complaining of dizziness [1,2]. More than 29% of adults over 60 years old reported dizziness to their clinician, which can lead to twice the risk of falls in that age group [3,4]. Further, half of people who fall due to dizziness are likely to become recurrent fallers [5]. Unfortunately, dizziness and falls are related to disability and decreased quality of life [6-8]. Dizziness, falls and imbalance are common across populations, even in young people. Up to 81% of people with mild traumatic brain injury (mTBI) report dizziness immediately following injury, while about 18% continue to complain about dizziness up to three months following injury [9-11]. Dizziness also occurs in diseases of the nervous system, with 59% of people with Multiple Sclerosis complaining of dizziness [12]. Over 40% of people with vestibular-related dizziness are unable to work, and 19% are home restricted [13].
Vestibular rehabilitation is a common approach to reduce dizziness and balance impairments across populations whereby patients are instructed to perform exercises that involve very specific head movements and balance exercises to promote better gaze stability and postural control [9,14-17]. There are some overarching guiding principles for optimizing the efficacy of vestibular rehabilitation that relate to approach, customization and timing. Generally speaking, vestibular rehabilitation should be active, started early, customized and progressive [18].
Dosing factors, such as movement and range of head movements, are important aspects that may impact outcomes, but less is known about these practices [19,20]. A clinical practice guideline for vestibular hypofunction reported that there is very little evidence available for dosing recommendations and stated that researchers should ‘examine the impact of frequency, intensity, time, and type of exercises on rehabilitation outcomes’ [20]. However, though the intensity (e.g. velocity of head movement) dose factor is likely a critical aspect of vestibular rehabilitation, it is not well defined or easily measured. Head movement to transient stimuli can exceed 150°/s, which exceeds vestibular ocular reflex (VOR) compensation abilities observed in patients with neuritis [21-23]. Studies have shown that vestibular rehabilitation training for gaze stabilization performed at slower head movement velocities (i.e. <150°/s) does not improve VOR responses that are required for daily activity [21,22] VOR gain relies on the ratio between head and eye velocities, resulting in retinal slip, which induces the error signal responsible for VOR adaptation. Importantly, retinal slip cannot be achieved without enough head velocity.
Secondarily, range of motion (ROM) plays a role in vestibular rehabilitation intensity, but like velocity, measuring ROM during vestibular rehabilitation exercises is subjective for current vestibular rehabilitation techniques. Using objective assessments, such as wearable sensors, could increase the ability to characterize velocity and ROM during vestibular rehabilitation, thereby helping to establish dosing guidelines.
Inertial Measurement Units (IMUs) are used to measure multiple aspects of balance and gait, and have been shown to be valid across populations with balance impairments [24-26] further, advances in algorithms permit use for unconventional sensor placement locations, including on the head and trunk [27]. Recently published data has established IMUs as valid tools for characterizing head and trunk movement, such as those used during common vestibular rehabilitation exercises [27,28]. Theoretically, both clinicians and patients could benefit from objective characterization of patient performance and progress across the rehabilitation timeline.
One important component for adding objective quantification of head velocity and ROM would be normative values to help set rehabilitation goals. There is limited published normative data for vestibular rehabilitation exercises. The exceptions are for the seated gaze stabilization exercise with angular velocity as the outcome variable. These normative angular velocities ranged from 129-287°/s, and represent a range of populations (e.g. young adult, older adult, and athletes) [29-35]. Given that vestibular rehabilitation requires increasingly difficult conditions (e.g. seated to standing, standing to walking, etc.), it is important to explore ROM and angular velocities across the common vestibular rehabilitation exercises that incorporate head movement.
The purpose of this study was to implement IMUs as a preliminary step to establishing normative values for cervical and trunk ROM and velocity in four commonly used vestibular rehabilitation exercises: gaze stabilization, visual motion sensitivity, static balance with head turns, and walking with head turns. The second purpose was to investigate the consistency of healthy participant performance of vestibular rehabilitation exercises across time using intraclass correlations. We hypothesize that healthy adults would have good (intraclass correlation coefficient >0.75) consistent head velocity and ROM, given the same instructions on separate days. Establsihing consistency of vestibular rehabilitation exercise performance will help interpret abberant patient findings.
Research Methodology
Participants
A convenience sample of 20 healthy control subjects were recruited. Inclusion criteria consisted of participants being between 20-40 years old and the ability to complete two testing sessions within 30 days. Exclusion criteria consisted of participants: 1) having musculoskeletal, neurological, or sensory deficits that could cause balance dysfunction 2) reporting neck pain or 3) being pregnant. This study was approved by the Oregon Health & Science University Institutional Review Board. Signed informed consent was obtained from all participants prior to participation.
Procedure
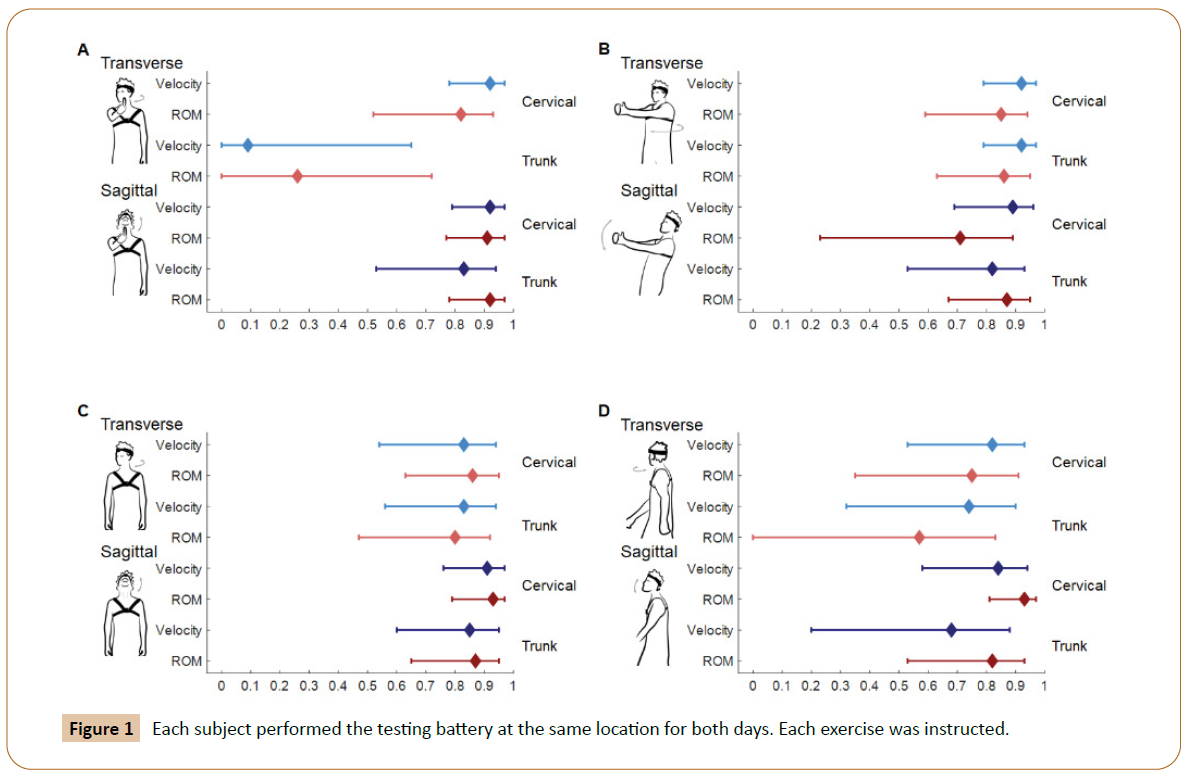
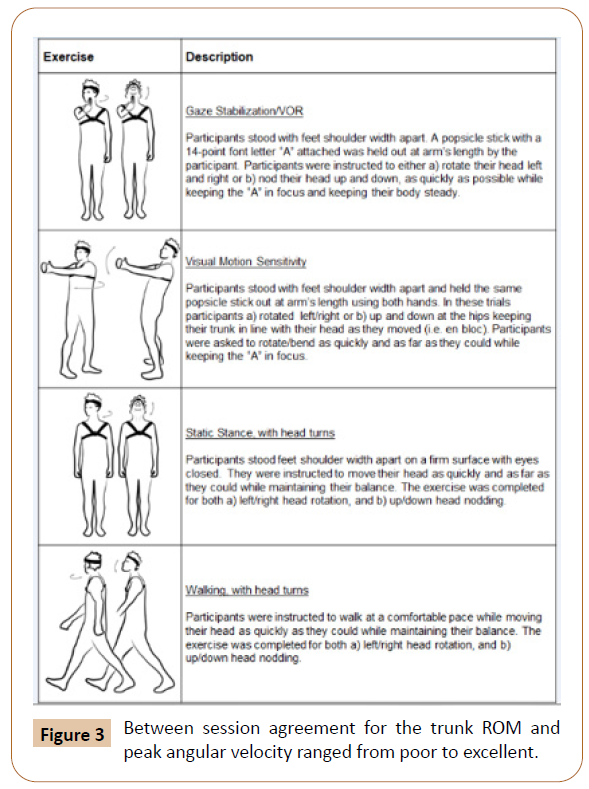
Subjects were evaluated using a vestibular exercise testing battery on two separate days (mean [SD] time between testing=11.1 [7.6] days). The testing battery included four common vestibular exercises, which were performed in the transverse plane (left/ right rotations) and the sagittal plane (up/down motions): 1) Gaze stabilization/VOR; 2) Visual motion sensitivity (VMS); 3) Static balance with head turns; and 4) Walking with head turns. These four exercises are well established as common vestibular rehabilitation exercises and they incorporate varying levels of difficulty. Unlike the previous literature reporting normative data for seated gaze stabilization, the four exercises were measured using standard, progressively difficult levels of exercises to include standing and walking conditions. Two trials were completed per exercise resulting in 16 trials per session (4 exercises, 2 planes of movements and 2 trials each). Each trial lasted for 30 seconds. Further information on each of the exercises is represented in Figure 1. Testing was performed outside of a controlled laboratory environment and included clinical offices and clinic spaces. Each subject performed the testing battery at the same location for both days. Each exercise was instructed (Figure 1) and demonstrated by the same physical therapist for both testing sessions. If a trial was performed incorrectly, the trial was stopped, and the participant was reinstructed to ensure the exercise was done correctly. The instructions and any subsequent corrections followed previously reported guidelines. Participants were provided the opportunity to take a short break as needed throughout the testing session.
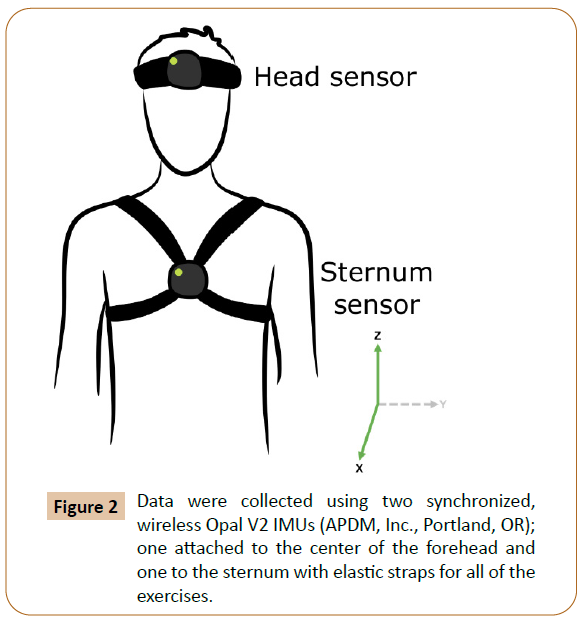
Data were collected using two synchronized, wireless Opal V2 IMUs (APDM, Inc., Portland, OR); one attached to the center of the forehead and one to the sternum with elastic straps for all of the exercises Figure 2. Data were processed using Moveo Software (APDM Inc., Portland, OR). The joint axes are determined by a combination of the sensor placement and calibration pose. Segment orientation is determined through sensor fusion with the accelerometer providing a tilt reference, the magnetometer providing a heading reference, and the gyroscope providing measurements on how the orientation changes with time. Joint angles are then determined by the relative orientation between adjacent segments. Cervical and trunk ROM, and peak angular velocity in both the sagittal and transverse planes were measured for each vestibular rehabilitation exercise condition.
Statistical Methods
The variables of interest were the ROM and the peak angular velocity of the head and trunk. As a preliminary step to establishing normative values for objective quantification of vestibular rehabilitation exercises we calculated the mean, standard deviation, and minimum and maximum values for each of the ROM and angular velocity outcome variables. To examine how consistently people performed between sessions, a twoway mixed effects ICC (3,2) model assessed absolute agreement of the means between session one and two. This ICC (3,2) model was selected based on previously reported guidelines.38 ICCs were interpreted as poor (<0.50), moderate (0.50-0.75), good (0.75-0.90), or excellent (>0.90) reliability based on established thresholds.39 In addition to the ICCs, we calculated the mean differences between sessions, with the 95% confidence intervals for the mean differences. Alpha was set a priori to p<0.05, and 95% confidence intervals have been included to aid the interpretation of the reader. Statistical analyses were run in IBM SPSS version 25.
Results
Of the 20 participants, data from 18 participants were analyzed. Two people were excluded due to technical issues relating to movement during a 3 second pre-trial calibration. The 18 participants that were analyzed were 28.7(5.1) years old and nine were female.
ROM and peak angular velocity values
Means, standard deviations, and the minimum and maximum values for the ROM and peak angular velocity for both segments (cervical and trunk) and each exercise are provided in Table 1.
| Gaze Stabilization | Visual Motion Sensitivity | Balance | Gait | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Transverse | Sagittal | Transverse | Sagittal | Transverse | Sagittal | Transverse | Sagittal | |||
| Range of Motion (°) | Cervical | Mean | 64.2 -17.47 |
43.93 -17.79 |
175.94 -29.96 |
106.47 -21.96 |
115.61 -23.13 |
68.04 -26.47 |
117.65 -23.74 |
68.91 -20.24 |
| Min-Max | 40.40-102.49 | 18.01-85.85 | 119.29-217.97 | 62.57-142.06 | 70.70-150.87 | 24.86-114.28 | 66.79-160.89 | 38.05-107.99 | ||
| Trunk | Mean | 1.33 -1.21 |
2.77 -1.63 |
169.15 -28.44 |
83.94 -35.29 |
4.04 -3.84 |
5.45 -2.99 |
19.13 -11.51 |
9.1 -2.22 |
|
| Min-Max | 0.49- 5.52 |
0.72- 6.74 |
113.78-218.19 | 14.59-133.14 | 1.04- 15.59 |
1.66- 11.79 |
7.97- 51.95 |
5.43- 13.86 |
||
| Peak Angular Velocity (°/s) | Cervical | Mean | 257.75 -81.74 |
189.56 -60.02 |
223.75 -62.05 |
170.37 -56.76 |
387.43 -102.54 |
238.8 -73.11 |
382.83 -76.82 |
256.81 -64.93 |
| Min-Max | 153.56-438.75 | 89.97-311.15 | 130.48-371.03 | 86.54-330.03 | 172.56-585.18 | 91.71-365.56 | 199.32-498.38 | 118.91-368.97 | ||
| Trunk | Mean | 6.09 -3.48 |
15.21 -6.82 |
211.09 -56.15 |
140.19 -66.68 |
14.43 -8.98 |
26.2 -15.06 |
61.37 -16.58 |
58.77 -13.43 |
|
| Min-Max | 2.97- 18.52 |
5.33- 29.32 |
123.34-327.59 | 46.79-292.20 | 4.53- 40.11 |
7.34- 59.95 |
35.53-95.48 | 35.58-87.20 | ||
Table 1: The means are presented as mean (standard deviation). The Min-Max provide the minimum and maximum values recorded during any one trial, at either time point.
Consistency of participant performance
Between session agreement (ICC) ranged from good and excellent for cervical ROM and peak angular velocity, with the lowest agreement occurring for cervical ROM during the VMS task in the transverse plane. Between session agreement for the trunk ROM and peak angular velocity ranged from poor to excellent (Figure 3). The mean differences and 95% confidence intervals are in Table 2.
Figure 3: Between session agreement for the trunk ROM and peak angular velocity ranged from poor to excellent.
| Variables | Gaze Stabilization | Visual Motion Sensitivity | Balance | Gait | |||||
|---|---|---|---|---|---|---|---|---|---|
| Transverse | Sagittal | Transverse | Sagittal | Transverse | Sagittal | Transverse | Sagittal | ||
| Range of Motion (°) | Cervical | -4.93 | -0.8 | -2.6 | -3.4 | 4.2 | 6.3 | -5.7 | 2.6 |
| (-11.6-1.8) | (-5.8-4.3) | (-13.6-8.3) | (-13.7-6.9) | (-3.8-12.2) | (-0.04-12.6) | (-16.1-4.7) | (-2.6-7.9) | ||
| Trunk | 0.4 | 0.1 | 0.1 | 8.4 | 1.4 | 0.3 | -6 | -0.7 | |
| (-0.5-1.2) | (-0.3-0. 6) | (-9.7-10.0) | (-3.0-19.8) | (-0.1-2.9) | (-0.7-1.3) | (-12.5-0.4) | (-1.5-0.1) | ||
| Peak Angular Velocity (°/s) | Cervical | -5.9 | -7.9 | -9 | -15.6 | 12.3 | 16.2 | 9.6 | 19.8 |
| (-28.6-16.8) | (-24.1-8.2) | (-26.2-8.2) | (-32.6-1.4) | (-27.2-51.8) | (-3.6-36.0) | (-19.9-39.2) | (-2.7-42.3) | ||
| Trunk | 1.51 | 0.1 | -8.1 | 13.7 | 2.3 | -0.5 | -7.4 | -4.4 | |
| (-1.0-4.0) | (-2.5-2.7) | (-23.5-7.2) | (-11.7-39.0) | (-0.9-5.6) | (-5.9-5.0) | (-14.2 - -0.5) | (-10.9-2.0) | ||
Table 2: The mean differences and 95% confidence intervals.
Discussion
This pilot study set out to implement IMUs during four common vestibular rehabilitation exercises as 1) the first attempt to quantify standing and walking vestibular rehabilitation exercise conditions, a preliminary step to establishing normative values for cervical and trunk ROM and velocity in these four commonly used exercises and 2) to determine how consistently healthy people perform these four common exercises. Healthy adults have faster angular velocities and more ROM during the standing and walking exercises than previous reports during the seated exercise conditions. Our results suggest that healthy adults perform vestibular rehabilitation exercises similarly over time, both in terms of peak angular velocity and ROM of the head and trunk. Further, IMU measurements during vestibular rehabilitation could be useful for setting targeted goals and tracking improvements during vestibular rehabilitation both in the clinic and at home.
We report IMU quantification of performance data across four common vestibular rehabilitation exercises during quiet standing and gait, which expands on the limited normative data available for the seated gaze stabilization exercise [29-35]. In general, the values for cervical velocity during quiet standing gaze stabilization we report are higher than published values for transverse and sagittal plane velocities during seated gaze stabilization. In the civilian population, the average maximum transverse velocity ranged from 129°/s to 169°/s, for those over 60 years old and under, respectively. These values are lower than those observed in athlete populations, which report between 134°/s to 287°/s. Other attempts at providing seated normative transverse velocities implemented metronome-based pacing (50 beats/min), which is equivalent to approximately 133°/s.33 In a younger, between 20 and 49 years old, healthy population, seated normative values for sagittal plane gaze stabilization was faster, averaging 190°/s . Regardless of movement plane, results suggest that age and skill (athlete versus non-athlete) are underlying factors in seated cervical velocity during gaze stabilization. The values reported herein may be higher due to the standing position of the task, allowing for some sternal movement, increasing the velocity of cervical movement. Importantly, more complex conditions of vestibular rehabilitation (e.g. walking with head turns) have not had relevant outcome values reported to date. In order to establish complete normative data, future investigations should quantify angular velocity and ROM in larger groups, across the vestibular rehabilitation exercise difficulty levels.
Peak angular velocity was consistently reliable across vestibular rehabilitation exercises, with only three of 16 velocity measures exhibiting 95% CIs that extend into poor reliability (ICC < 0.50). In fact, 64% (n=7 of 11) of the lowest velocity reliability (ICC 95% CI lower bound < 0.75) was observed in trunk angular velocity. ROM had five of 16 ICCs categorized as poor, three of which were specific to the trunk [36-40] found excellent (ICC=0.98) subject performance consistency between days, but they limited cervical ROM to 60° left and right (total of 120° of movement) with visual end point goals for rotation, while we implemented no limitations on ROM. Further, there was no description of the time between or the number of subjects in the investigation. The average cervical ROM observed in the results herein, regardless of vestibular rehabilitation exercise, was greater than 60°. While several subjects had a maximum cervical ROM over 200°, this excessive range is explained by additional movement from the trunk. This compensatory strategy may have played a critical role in the poorer repeatability scores for the sternal transverse ROMs observed.
Though IMUs have been used for gait and balance characterization across a multitude of clinical populations, less work has measured head and trunk movements during complex activities requiring vestibular influence on balance and gait [41-47] Across the seven studies that quantified a vestibular rehabilitation exercise (only cervical velocity during seated gaze stabilization), three used optical tracking equipment, three used accelerometer and/or IMU technology and one used a clinician’s visual inspection of patient matching their head movement with the beat of a metronome. The results herein, quantification of trunk movement had lower validity than cervical movement. Combined, the results of these studies provide support for IMU implementation in vestibular rehabilitation-based exercises. The results herein expand on these previous reports.
Potential advantages to adding IMUs during vestibular rehabilitation exercises include improved dosage and performance quality. As discussed, cervical angular rotation required for improved VOR needs to be at least 150°/s, though some populations may require increased velocities that are lifestyle specific. For instance, vestibular rehabilitation cervical velocity training might require increased velocity thresholds (e.g. > 150°/s) for athletes than non-athletes, while decreased cervical velocity thresholds (e.g. ≤ 150°/s) might be sufficient for older adult populations. Clinical trials aimed to determine the effects of these dosing factors on the efficacy of vestibular rehabilitation are necessary to further improve vestibular rehabilitation outcomes in specific populations. For quality exercise form, the trunk should remain still for vestibular rehabilitation exercises, thereby isolating head movement. Aside from the VMS exercise where there is exaggerated trunk movement and the trunk and head move together, extra trunk motion may be a sign of compensation (adding to cervical velocity and ROM via the trunk) for inability to achieve 150°/s. Though, specific to the standing VMS condition, the trunk and cervical ROM and velocities should be tightly synced for correct performance. IMU information can provide added detail about the individual segment ROM and velocity, detailing intersegmental coordination. Data from the trunk would provide clinicians additional information regarding patient performance and strategy.
Across rehabilitation, most of the exercise occurs in the home. IMUs may be useful in providing objective information on both quality and quantity (e.g. dosing) of vestibular rehabilitation exercise performance at home. Patients often avoid exacerbating symptoms, thus limiting their ROM and velocity while performing vestibular rehabilitation without supervision. Based on our results, IMUs characterize and log information on performance, which may improve vestibular rehabilitation exercise performance as well as adherence at home. It is known that home exercises are not as effective as supervised exercises performed in the clinic, in part because of reduced compliance [48,49] Previous studies have found patient compliance, specific to vestibular rehabilitation home exercise program, is one of the main barriers [50-52] A systematic review of strategies used in vestibular rehabilitation home exercise program adherence found strong evidence for a combination of a written summary of exercises and a maintenance log of home exercise program, including symptomology [53] Others found a combination of specific adherence strategies such as information and self-monitoring improved compliance and adherence. The use of IMUs may add another objective tool to improve compliance. Additionally, the physical therapist could remotely access the data, which would allow for regular monitoring of patient progress.
The IMUs used for this study had no previously established algorithms to characterize vestibular rehabilitation, thus, we worked with the company (APDM Inc.) to develop algorithms for objectively measuring vestibular rehabilitation exercises. Development of the inertial system was iterative and utilized a user-centered design to process feedback, reports, and measures.
Throughout this process, two main changes were made to improve the reliability of the system and quality of the measures and to enhance its usability. The first were changes to provide a more informative error message in trials where there were no head turns or missing sensor data from the gyroscope. These did not result in any change in whether results were produced or not, simply a more helpful error message that would benefit both clinician and patient. The other changes included 1) relaxing the thresholds for still period detection (initially these were set based on foot sensor data for gait analysis and were updated based on what is reasonable to expect during a still period for the upper body sensor locations); 2) disabling turn detection for standing trials, since the transverse condition was sometimes being detected as a series of many gait turns and excluded from analysis; 3) correcting sensor labels that were mislabeled during sensor configuration.
Limitations. There are inherent limitations to this study. Although we enrolled 20 participants, we only had data for both trials across all conditions and both days for 18 participants. This pilot dataset is comprised of a relatively small dataset. Additionally, the small (N=18) cohort that participated were young, so the data may not be applicable to all age groups. Future studies should assess ROM and peak angular velocity normative performance across ages, vestibular populations, and in larger cohorts. Although not a direct limitation of this study, it should be acknowledged that using IMUs in the clinic is in the early stages so access and usability may still be a limitation for implementation.
Conclusion
Implementing IMUs to characterize cervical and trunk movement during vestibular rehabilitation exercises shows promise for providing reliable and objective information on exercise performance. Using IMUs during vestibular rehabilitation exercises has the potential improve rehabilitation efficacy in the clinic and at home. Specifically, the utilization of IMUs in the clinic could help verify that the patients are doing the correct exercise, at the correct speed, frequency and intensity. In the future, IMUs could be instrumental for individualized patient care through characterization of rehabilitation performance and aid in a physical therapist’s exercise prescription, including examination of compliance.
Acknowledgements
This study was supported by the Assistant Secretary of Defense for Health Affairs under the Award Number W81XWH-17-1-0424 and by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Award Number UL1TR002369. All interpretations and opinions are those of the author and are not necessarily endorsed by the Department of Defense or National Institutes of Health. The authors would like to thank Ms. Lindsey Lee for her significant time and effort in this project.
References
- Ward BK, Agrawal Y, Hoffman HJ, John PC, Charles CD (2013) Prevalence and Impact of Bilateral Vestibular Hypofunction: Results From the 2008 US National Health Interview Survey. JAMA Otolaryngol Head Neck Surg 139: 803-810.
- Brandt T, Dieterich M (2017) The dizzy patient: Don't forget disorders of the central vestibular system. Nat Rev Neurol 13: 352-362.
- O'Loughlin JL, Robitaille Y, Boivin JF, Suissa S (1993) Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol 137: 342-354.
- Sloane P, Blazer D, George LK (1989) Dizziness in a community elderly population. J Am Geriatr Soc 37: 101-108.
- Stalenhoef PA, Crebolder HF, Knottnerus JA, Frans Gem, Van DH (1997) Incidence, risk factors and consequences of falls among elderly subjects living in the community: a criteria-based analysis. Eur J Public Health 7: 328-334.
- Agrawal Y, Carey JP, Della Santina CC (2009) Disorders of Balance and Vestibular Function in US Adults: Data From the National Health and Nutrition Examination Survey, 2001-2004. Arch Intern Med 169: 938-944.
- Yardley L, Owen N, Nazareth I, Luxon L (1998) Prevalence and presentation of dizziness in a general practice community sample of working age people. Br J Gen Pract 48: 1131-1135.
- Jacobson GP, Newman CW (1990) The development of the dizziness handicap inventory. Arch Otolaryng Head Neck Surg 116: 424-427.
- Alsalaheen BA, Mucha A, Morris LO (2010) Vestibular rehabilitation for dizziness and balance disorders after concussion. J Neurol Phys Ther 34: 87-93.
- Dischinger PC, Ryb GE, Kufera JA (2009) Early predictors of postconcussive syndrome in a population of trauma patients with mild traumatic brain injury. J Trauma Acute Care Surg 66: 289-297.
- Lannsjö M, Geijerstam J-La, Johansson U (2009) Prevalence and structure of symptoms at 3 months after mild traumatic brain injury in a national cohort. Brain Injury 23: 213-219.
- Rae-Grant AD, Eckert NJ, Bartz S (1999) Sensory symptoms of multiple sclerosis: a hidden reservoir of morbidity. Mult Scler 5: 179-183.
- Neuhauser HK, Radtke A, Von Brevern M, Franziska L, Maria F, et al. (2008) Burden of dizziness and vertigo in the community. Arch Intern Med 168: 2118-2124.
- Gizzi M (1995) The efficacy of vestibular rehabilitation for patients with head trauma. J Head Trauma Rehabil 10: 60-77.
- Herdman SJ (1990) Treatment of benign paroxysmal positional vertigo. Physical therapy 70: 381- 388.
- Hoffer ME, Gottshall KR, Moore R, Ben JB, Derin W (2004) Characterizing and treating dizziness after mild head trauma. Otol Neurotol 25: 135-138.
- Gurr BM, Nick (2001) Psychological consequences of vertigo and the effectiveness of vestibular rehabilitation for brain injury patients. Brain Injury 15: 387-400.
- Lacour M, Bernard-Demanze L (2015) Interaction between vestibular compensation mechanisms and vestibular rehabilitation therapy: 10 recommendations for optimal functional recovery. Front Neurol 5: 285.
- Hall CD, Herdman SJ, Whitney SL, Stephen PC, Richard AC, et al. (2016) Vestibular Rehabilitation for Peripheral Vestibular Hypofunction: An Evidence-Based Clinical Practice Guideline: From the American Physical Therapy Association Neurology Section. J Neurol Phys Ther 40: 124-155.
- Murray DA, Meldrum D, Lennon O (2017) Can vestibular rehabilitation exercises help patients with concussion? A systematic review of efficacy, prescription and progression patterns. Br J Sports Med 51: 442-451.
- Rinaudo CN, Schubert MC, Figtree WV, Christopher JT, Americo AM (2019) Human vestibulo-ocular reflex adaptation is frequency selective. J Neurophysiol 122: 984-993.
- Roller RA, Hall CD (2018) A speed-based approach to vestibular rehabilitation for peripheral vestibular hypofunction: A retrospective chart review. J Vestib Res 28: 349-357.
- Halmagyi GM, Curthoys IS (1988) A clinical sign of canal paresis. Arch. Neurol 45: 737-739.
- Freeman DL, Gera G, Horak FB (2001) The Instrumented Test of Sensory Integration for Balance: A Validation Study. J Geriatr Phys Ther 2018; 41: 77.
- Ghislieri M, Gastaldi L, Pastorelli S (2019) Wearable Inertial Sensors to Assess Standing Balance: A Systematic Review. Sensors 19: 4075.
- Morris R, Stuart S, McBarron G (2019) Validity of Mobility Lab (version 2) for gait assessment in young adults, older adults and Parkinson’s disease. Physiol Meas 40: 095003.
- Parrington L, Jehu DA, Fino PC, Sean P, Mahmoud El G, et al. (2018) Validation of an inertial sensor algorithm to quantify head and trunk movement in healthy young adults and individuals with mild traumatic brain injury. Sensors 18: 4501.
- Paul SS, Walther RG, Beseris EA (2017) Feasibility and Validity of Discriminating Yaw Plane Head- on-Trunk Motion Using Inertial Wearable Sensors. IEEE Trans Neural Syst Rehabilitation Eng 25: 2347-2354.
- Gottshall KR, Hoffer ME (2010) Tracking recovery of vestibular function in individuals with blast- induced head trauma using vestibular-visual-cognitive interaction tests. J Neurol Phys Ther 34: 94-97.
- Honaker JA, Criter RE, Patterson JN (2015) Gaze stabilization test asymmetry score as an indicator of previous concussion in a cohort of collegiate football players. Clin J Sport Med 25: 361-366.
- Honaker JA, Shepard NT (2010) Age effect on the gaze stabilization test. J Vestib Res Equilib Orientat 20: 357-362.
- Massingale S, Alexander A, Gerkin R (2019) Gaze stability in the elite athlete: A normative observational study. J Vestib Res 1-8.
- Mucha A, Collins MW, Elbin R (2014) A brief vestibular/ocular motor screening (VOMS) assessment to evaluate concussions: preliminary findings. Am J Sports Med 42: 2479-2486.
- Schneiders AG, Sullivan SJ, Rathbone EJ (2010) Visual acuity in young elite motorsport athletes: A preliminary report. Phys Ther Sport 11: 47-49.
- Ward BK, Mohammad MT, Whitney SL, Marchetti GF, Joseph MF (2010) The reliability, stability, and concurrent validity of a test of gaze stabilization. J Vestib Res 20: 363-372.
- Balaban CD, Hoffer ME, Gottshall KR (2012) Top-down approach to vestibular compensation: translational lessons from vestibular rehabilitation. Brain research 1482: 101-111.
- Alsalaheen BA, Whitney SL, Mucha A, Laura O M, Joseph MF, et al. (2013) Exercise prescription patterns in patients treated with vestibular rehabilitation after concussion. Physiother Res Int 18: 100-108.
- Koo TK and Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15: 155-163.
- Portney L, Watkins M (2009) Foundations of clinical research: applications to practice (3rdedn) Pearson Prentice Hall. Upper Saddle River, New Jersey.
- Jheng Y-C, Yu C-H, Chen P-Y (2019) Establishment of vestibular function multimodality platform. J Chin Med Assoc 82: 328-334.
- Mancini M, Carlson-Kuhta P, Zampieri C (2012) Postural sway as a marker of progression in Parkinson's disease: a pilot longitudinal study. Gait Posture 36: 471-476.
- Mancini M, Horak FB, Zampieri C, Patricia CK, John GN, et al. (2011) Trunk accelerometry reveals postural instability in untreated Parkinson's disease. Parkinsonism Relat Disord 17: 557-562.
- Mancini M, Salarian A, Carlson-Kuhta P (2012) ISway: A sensitive, valid and reliable measure of postural control. J Neuroeng Rehabil 9: 59.
- Spain R, George RS, Salarian A (2012) Body-worn motion sensors detect balance and gait deficits in people with multiple sclerosis who have normal walking speed. Gait & posture 35: 573-578.
- Mancini M, Chiari L, Holmstrom L (2016) Gait & Posture Validity and reliability of an IMU-based method to detect APAs prior to gait initiation.
- Mancini M, Chiari L, Holmstrom L (2016) Validity and reliability of an IMU-based method to detect APAs prior to gait initiation. Gait & posture 43: 125-131.
- Loyd BJ, Saviers-Steiger J, Fangman A (2020) Turning Toward Monitoring of Gaze Stability Exercises: The Utility of Wearable Sensors. J Neurol Phys Ther 44: 261-267.
- Galey JL, Eagle SR, Blaney NA (2020) Effect of Patient Compliance With Treatment Recommendations on Clinical Outcomes in Chronic mTBI: A TEAM-TBI Study. Military Medicine.
- Kao C-L, Chen L-K, Chern C-M (2010) Rehabilitation outcome in home-based versus supervised exercise programs for chronically dizzy patients. Arch Gerontol Geriatr 2010; 51: 264- 267.
- Ricci NA, Aratani MC, Caovilla HH (2015) Challenges in conducting a randomized clinical trial of older people with chronic dizziness: before, during and after vestibular rehabilitation. Contemp Clin Trials 40: 26-34.
- Yardley L, Kirby S (2006) Evaluation of booklet-based self-management of symptoms in Meniere disease: a randomized controlled trial. Psychosom Med 68: 762-769.
- Geraghty AW, Kirby S, Essery R (2014) Internet-based vestibular rehabilitation for adults aged 50 years and over: a protocol for a randomised controlled trial. BMJ open 4: e005871.
- Gaikwad SB, Mukherjee T, Shah PV (2016) Home exercise program adherence strategies in vestibular rehabilitation: A systematic review. Phys Ther Rehabil Sci 5: 53-62.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences