Vitamin D Metabolism and Bone Loss After Bariatric Surgery
Endocrinology Research Center Moscow, Russia
- Corresponding Author:
- Natalya Mazurina
Endocrinology Research Center Moscow, Russia
Tel: +7499-612-7740
E-mail: natalyamazurina@mail.ru
Received Date: September 28, 2017; Accepted Date: October 18, 2017; Published Date: October 25, 2017
Citation: Mazurina N. (2017) Vitamin D Metabolism and Bone Loss after Bariatric Surgery. J Metab. Vol. 1 No.1: 1.
Copyright: © 2017 Mazurina N. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Obesity surgery is a highly effective treatment for morbidly obese patients. Despite effective weight reduction, the impact of bariatric surgery on bone is a major concern. Mechanisms of the deleterious effect include calcium and vitamin D malabsorption with secondary hyperparathyroidism (SHPT), deficiency in other nutrients and alterations in gut-derived hormones. Sleeve gastrectomy (SG) and Roux-en-Y gastric bypass (RYGB) are the most frequently performed bariatric procedures in the past few years. RYGB and SG have comparable effects in terms of energy and food restriction and subsequent risk of micronutrient and protein deficiencies in the long-term follow-up period. Most of the publications report bone mineral density (BMD) loss after bariatric surgery. It is interesting that hip bone loss is more significant than spine BMD loss. Clinical Practice Guidelines recommend calcium and vitamin D supplementation postoperatively after malabsorbtive obesity surgical procedures with dose adjustment by a qualified medical professional based on serum markers. Oral doses of vitamin D may need to be as high as 50000 IU 1 to 3 times weekly or daily. Vitamin D loading and ongoing vitamin D, calcium, and BMI-adjusted protein supplementation in combination with physical exercise may decelerate the loss of BMD after bariatric surgery.
Obesity surgery is a highly effective treatment for morbidly obese patients. Despite effective weight reduction, the impact of bariatric surgery on bone is a major concern. Mechanisms of the deleterious effect include calcium and vitamin D malabsorption with secondary hyperparathyroidism (SHPT), deficiency in other nutrients and alterations in gut-derived hormones. Sleeve gastrectomy (SG) and Roux-en-Y gastric bypass (RYGB) are the most frequently performed bariatric procedures in the past few years. RYGB and SG have comparable effects in terms of energy and food restriction and subsequent risk of micronutrient and protein deficiencies in the long-term follow-up period. Most of the publications report bone mineral density (BMD) loss after bariatric surgery. It is interesting that hip bone loss is more significant than spine BMD loss. Clinical Practice Guidelines recommend calcium and vitamin D supplementation postoperatively after malabsorbtive obesity surgical procedures with dose adjustment by a qualified medical professional based on serum markers. Oral doses of vitamin D may need to be as high as 50000 IU 1 to 3 times weekly or daily. Vitamin D loading and ongoing vitamin D, calcium, and BMI-adjusted protein supplementation in combination with physical exercise may decelerate the loss of BMD after bariatric surgery.
Keywords
Bariatric Surgery follow-up; Vitamin D; Secondary Hyperparathyroidism; Calcium Supplementation; Bone Mineral Density
Introduction
Obesity surgery is a highly effective treatment for morbidly obese patients. Accumulating evidence suggests that bariatric surgery improves survival among patients with severe obesity [1-6].
Beneficial short-term effects on common comorbidities are well known [7-11], but a growing data pool from long-term follow-up reveals increasing evidence of potentially severe nutritional and pharmacological consequences [12-15]. Complications are the results of postoperative changes in intake, absorption and bioavailability of micro and macronutrients.
Despite effective weight reduction, the impact of bariatric surgery on bone is a major concern [16-18]. Mechanisms of the deleterious effect include calcium and vitamin D malabsorption with secondary hyperparathyroidism (SHPT), deficiency in other nutrients and alterations in gut-derived hormones. Clinical guidelines to prevent bone loss and fractures after bariatric surgery are not appropriate and pharmacological supplementation should be worked out.
Obesity and calcium metabolism
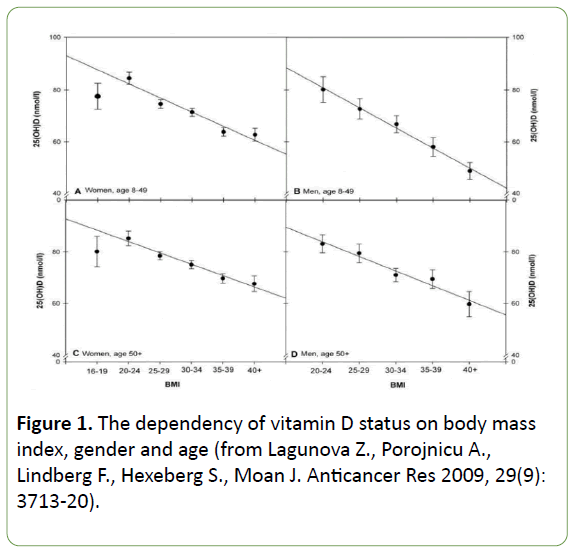
The first point is calcium metabolism in obesity, because it is very important for understanding the problem. Several population studies found the dependency between BMI and vitamin D status [19-22]. A significant inverse correlation exists between serum 25(OH)D level and body mass index (BMI). We can see the same pattern in males and in females, in younger persons and in persons after 50 (Figure 1).
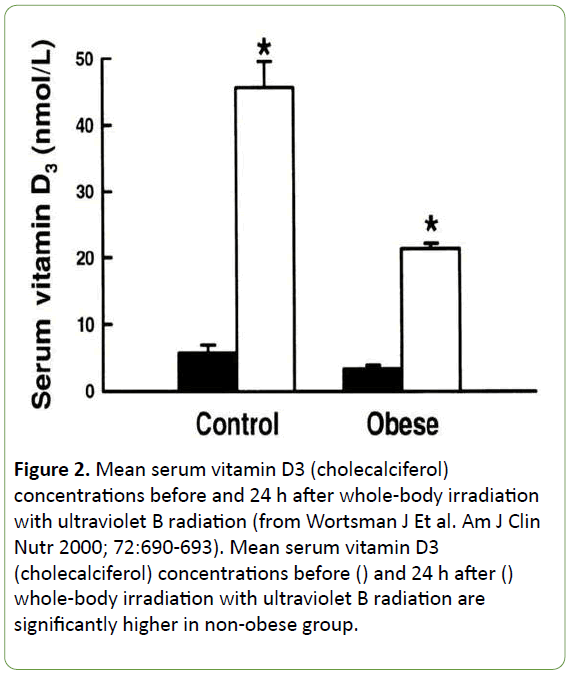
Why does this correlation exist? It can be easily explained. Cholecalciferol and ergocalciferol are fat soluble substances and after oral intake or after exposure to solar ultraviolet (UV) radiation they are diffused in a fat tissue. The study by Worthman J. and his colleagues (23) illustrates the difference in serum vitamin D concentrations after UV irradiation and oral intake in obese patients and in normal weight controls (Figure 2).
Figure 2: Mean serum vitamin D3 (cholecalciferol) concentrations before and 24 h after whole-body irradiation with ultraviolet B radiation (from Wortsman J Et al. Am J Clin Nutr 2000; 72:690-693). Mean serum vitamin D3 (cholecalciferol) concentrations before () and 24 h after () whole-body irradiation with ultraviolet B radiation are significantly higher in non-obese group.
SHPT is a compensation of chronic hypocalcemia and chronic vitamin D deficiency. This pathophysiological mechanism plays an important role in obesity, especially in morbidly obese patients seeking for bariatric surgery. Up to 60- 90% of patients with BMI ≥ 40 kg/m2 have vitamin D deficiency [23,24]. A significant inverse correlation was found between BMI and serum parathyroid hormone (PTH) level. The frequency of SHPT in morbidly obese patients is 25% - 50% [25-29]. So, we must realize that before bariatric surgery, a majority of patients have vitamin D depletion and SHPT.
Until recently, obesity was believed to be protective against osteoporotic fractures. Nevertheless, if we have a look at modifiable osteoporosis risk factors we will see that the most significant risk factors are typical for obesity. Obese patients have vitamin D deficiency, low physical activity and sex steroid deficiency.
However, traumatology departments report a surprisingly high proportion of obese postmenopausal women attending the clinic with fractures. Subsequently, multiple studies have demonstrated the importance of obesity in the epidemiology of fractures. Obese women are at increased risk of fracture in ankle, leg, humerus, and vertebral column and at lower risk of wrist, hip and pelvis fracture when compared to non-obese women [30].
In men, it has been reported that multiple rib fractures are associated with obesity [30]. Furthermore, falls appear to play an important role in the pathogenesis of fractures in obese subjects. Regarding hip fracture and major fractures, the FRAX algorithm has proven to be a useful predictor in obese individuals. So, obesity is not considered to be protective against fractures anymore.
Nutrient deficiency after bariatric surgery
The next point is nutrient deficiency after bariatric surgery. Vitamin D is mostly absorbed in duodenum and small intestine after emulsification with bile salts. Approximately 80% of calcium are absorbed in duodenum and proximal small bowel (vitamin D dependent active transport), about 20% are absorbed in the distal small intestine by passive diffusion.
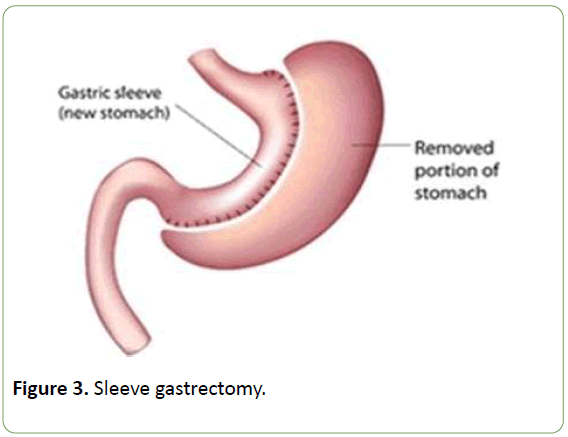
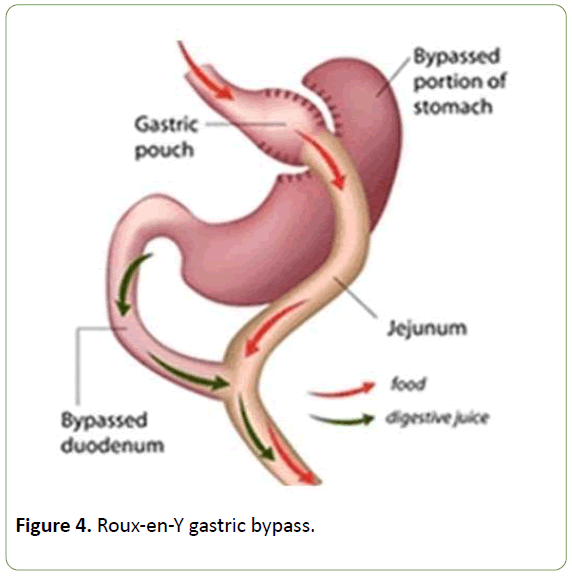
Sleeve gastrectomy (SG) (Figure 3) and Roux-en-Y gastric bypass (RYGB) (Figure 4) are the most frequently performed bariatric procedures in the past few years [31,32]. SG is a restrictive operation and it does not change physiological food transition. Duodenum - the main location of calcium and vitamin D absorption is not bypassed after gastric sleeve.
Because of RYGB duodenum is bypassed and nutritional deficiencies after RYGB are well known and were reported by multiple retrospective studies [32,33]. The most frequent specific deficiencies after RYGBP are vitamin В12 and ferrum (10-50%), folic acid (40-45%), calcium and vitamin D (60-80%) [33]. It is obviously that calcium and vitamin D depletion have the first place in this list.
Hypothetically, we may not expect significant nutritional deficiencies after restrictive operations. However, clinical practice demonstrates us that nutrient deficiencies after restrictive surgery do exist [34-38]. Most of the studies that assessed SG versus RYGB found no significant difference in nutritional consequences.
RYGB and SG have comparable effects in terms of energy and food restriction and subsequent risk of micronutrient and protein deficiencies in the first year post bariatric surgery [34]. Such results advocate for a cautious monitoring of protein intake after RYGB and SG and a systematic multivitamin and mineral supplementation in the first year after SG.
During a mean follow up period of 4 years post RYGB or SG, patients were identified with several micronutrient deficiencies, including vitamin D, folate, and vitamin B12 [36]. SG may have a more favorable effect on the metabolism of vitamin B12 compared with RYGB, being associated with less malabsorption.
Peterly and his group (2017) also found no difference in vitamin deficiencies between the SG and RYGB [38]. Their data are particularly reliable because they achieved 97% follow–up rate. In their study both groups had a rather high rate of deficiencies despite regular vitamin supplementation in all patients. The very high follow-up rate (97%) with regular laboratory investigations may explain the high prevalence. No severe malnutrition was observed. These results demonstrate the need for life-long vitamin supplementation and monitoring of deficiencies following LSG and LRYGB.
BMD after bariatric surgery
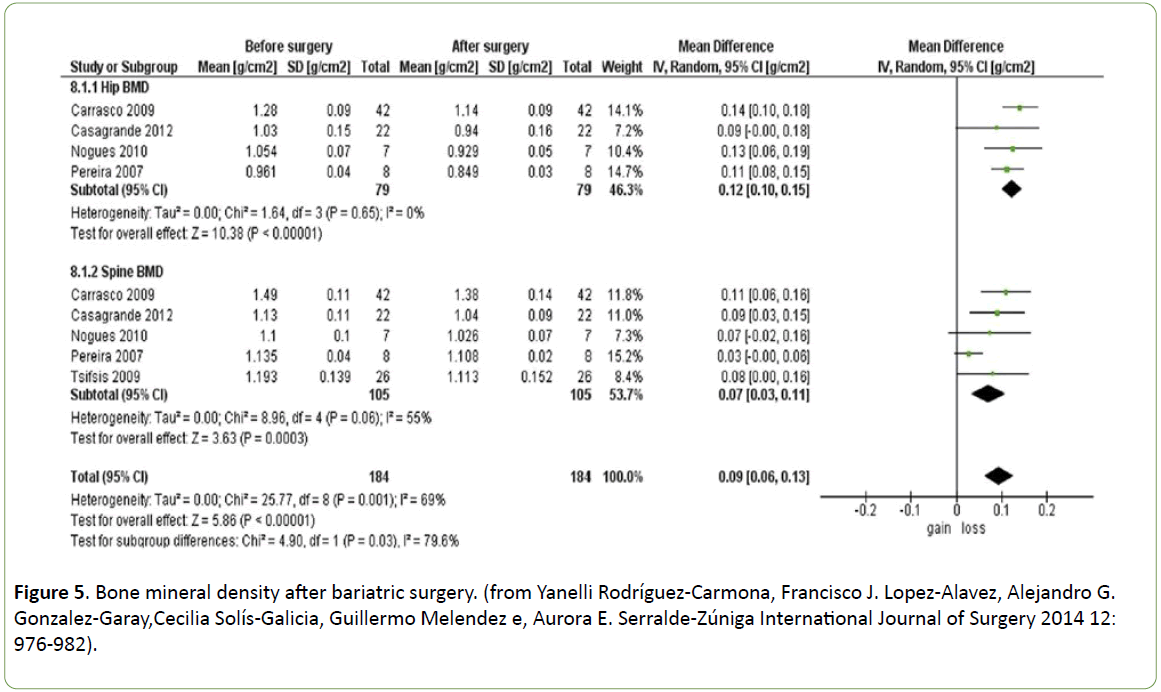
So, what is about bone mineral density (BMD) after Bariatric Surgery? While searching PubMed Database I have found the only one systematic review [16]. In Most of the publications included in the review (Figure 5), the type of surgery was RYGB, in two studies – SG. However, we can see that all the surveys report BMD loss.
The decline of hip bone density after GB was revealed in some prospective studies [17,18]. It is interesting that hip bone loss was more significant than spine BMD loss.
SG tends to be the most popular bariatric procedure and studies concerning BMD changes after SG are very important. Two longitudinal studies found significant declines in bone density at axial sites, with average DXA-measured femoral bone loss (range −5.2 to −8.3%) exceeding average spine bone loss (range −1.2% to −4.6%) within the first year after SG [39,40].
In contrast, in third study Ruiz-Tovar et al. [41] found significant increases in spine BMD over 2 years (+7.9%). The reason for the discrepant results at the lumbar spine are unclear, although the last study had remarkable improvements in vitamin D deficiency (prevalence of 95% preoperatively to 2% postoperatively) as compared with most other studies that have documented either stability or worsening of vitamin D deficiency and secondary hyperparathyroidism after bariatric surgery.
Treatment and prophylactic
In addition, the last point of is treatment and prophylactic of calcium metabolism impairment and BMD loss after bariatric surgery.
Cases of osteomalacia after BS are being reported regularly since 1985. If you search for “ostemalacia and bariatric surgery”, you can find over 25 papers. If the patient has no appropriate monitoring and treatment secondary hyperparathyroidism, vitamin D deficiency, severe osteoporosis and osteomalacia due to malabsorption may occur.
Clinical Practice Guidelines recommend calcium and vitamin D supplementation postoperatively after malabsorbtive obesity surgical procedures with dose adjustment by a qualified medical professional based on serum markers [12]. Oral doses of vitamin D may need to be as high as 50000 IU 1 to 3 times weekly or daily [32].
At the same time, we know from the results of the follow-up studies that vitamin D dosages between 1000 and 5000 IU daily are insufficient to maintain serum 25(OH)D optimal concentration (>30 ng/ml). Moreover, even vitamin D supplementation regimen with 50000 IU weekly plus a daily dose is not always sufficient to achieve 25(OH)D normal range [42]. To work out the optimal supplementation regimen is a great need!
There are some recommendations that should be discussed when we speculate about the treatment and prophylactic of calcium metabolism impairment in bariatric patients:
• Morbidly obese patients need vitamin D loading before surgery in accordance with actual Clinical Guidelines for evaluation, treatment and prevention of vitamin D deficiency.
• In the early postoperative period (7-10 days after surgery), patients should start taking 1500-1800 mg calcium and 800 IU vitamin D daily.
• After 3 months vitamin D dose adjustment based on serum markers (25(OH)D, calcium, phosphorus,) is required.
• PTH level measurement 6 months after surgery is necessary.
• Monitoring of PTH and 25(OH)D levels should be accompanied by monitoring of calcium
• All bariatric patients should have DXA for bone density assessment 24 month postoperatively. Appropriate treatment for osteoporosis (T-2.5) should be provided.
• Vitamin D supplementation is individual up to 50000 IU daily (daily/ daily + bolus dose 1-3 times a week).
• Optimization of calcium and vitamin D supplementation is the first step for SHPT correction. Alfacalcidol can be added to ergocalciferol therapy to normalize PTH level.
Conclusion
Although the benefits of bariatric surgery are well established, the potential for adverse effects on skeletal integrity remains an important concern.
Vitamin D loading and ongoing vitamin D, calcium, and BMIadjusted protein supplementation in combination with physical exercise decelerates the loss of BMD after bariatric surgery.
References
- Pontiroli AEW, Morabito A (2011) Long-term prevention of mortality in morbid obesity through bariatric surgery. A systematic review and meta-analysis of trials performed with gastric banding and gastric bypass. Ann Surg 253: 484-487.
- Buchwald H, Rudser KD, Williams SE, Michalek VN, Vagasky J, et al. (2010) Overall mortality, incremental life expectancy, and cause of death at 25 years in the program on the surgical control of the hyperlipidemias. Ann Surg 251: 1034-1040.
- Padwal R, Klarenbach S, Wiebe N, Birch D, Karmali S,et al. (2011) Bariatric surgery: a systematic review and network meta-analysis of randomized trials. Obes Rev 12: 602-621.
- Garb J, Welch G, Zagarins S, Kuhn J, Romanelli J (2009) Bariatric surgery for the treatment of morbid obesity: a meta-analysis of weight loss outcomes for laparoscopic adjustable gastric banding and laparoscopic gastric bypass. Obes Surg 19: 1447-1455.
- Valezi AC, Mali Junior J, de Menezes MA (2010) Weight loss outcome after silastic ring Roux-en-Y gastric by-pass: 8 years of follow-up. Obes Surg 20: 1491-1495.
- Toouli J, Kow L, Ramos AC, Aigner F, Pattyn P, et al. (2009) International multicenter study of safety and effectiveness of Swedish Adjustable Gastric Band in 1-, 3-, and 5-year follow-up cohorts. Surg Obes Relat Dis 5: 598-609.
- Buchwald H, Estok R, Fahrbach K, Banel D, Jensen MD, et al. (2009) Weight and type 2 diabetes after bariatric surgery: systemic review and meta-analysis. Am J Med 122: 248-256.
- Hofso D, Nordstrand N, Johnson LK, Karlsen TI, Hager H, et al. (2010) Obesity-related cardiovascular risk factors after weight loss: a clinical trial comparing gastric bypass surgery and intensive lifestyle intervention. Eur J Endocrinol 163: 735-745.
- Schauer PR, Kashyap S, Wolski K, Brethauer SA, Kirwan JP, et al. (2012) Bariatric Surgery versus Intensive Medical Therapy in Obese Patients with Diabetes. N Engl J Med 366: 1567-1576.
- Mingrone G, Panunzi S, De Gaetano A, Guidone C, Iaconelli A, et al. (2012) Bariatric Surgery versus Conventional Medical Therapy for Type 2 Diabetes. N Engl J Med 366: 1577-1585.
- Hofso D, Jenssen T, Bollerslev J, Ueland T, Godang K, et al. (2010) Beta cell function after weight loss: a clinical trial comparing gastric bypass surgery and intensive lifestyle intervention. Eur J Endocrinol 164: 231-238.
- Heber D, Greenway F L, Kaplan L M, Livingston E, Salvador J, et al. (2010) Endocrine and Nutritional Management of the Post-Bariatric Surgery Patient: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 95: 4823-4843.
- Brolin R, Leung M (1999) Survey of vitamin and mineral supplementation after gastric bypass and biliopancreatic diversion for morbid obesity. Obes Surg 9: 150-154.
- Skroubis G, Sakellapoulos G, Pouggouras K,Mead N, Nikiforidis G, et al. (2002) Comparison of nutritional deficiencies after Roux-en-Y gastric bypass and after biliopancreatic diversion with Roux-en-Y gastric bypass. Obes Surg 12: 551-558.
- Gasteyger C, Suter M, Gaillard RC, Giusti V (2008) Nutritional deficiencies after Roux-en-Y gastric bypass for morbid obesity often cannot be prevented by standard multivitamin supplementation. Am J Clin Nutr 87: 1128-1133.
- Rodríguez-Carmona Y, Lopez-Alavez F, Gonzalez-Garay A, Solís-Galicia C, Meléndez G, et al. (2014) Bone mineral density after bariatric surgery. A systematic review. International Journal of Surgery 12: 976-982.
- Fleischer J, Stein EM, Bessler M, Della Badia M, Restuccia N, et al. (2008)The Decline in Hip Bone Density after Gastric Bypass Surgery Is Associated with Extent of Weight Loss. J Clin Endocrinol Metab 93(10): 3735-3740.
- Yu E, Bouxsein ML, Putman MS, Monis EL, Roy AE, et al. (2015) Two-Year Changes in Bone Density After Roux-en-Y Gastric Bypass Surgery. J Clin Endocrinol Metab 100(4): 1452-1459.
- Lagunova Z, Porojnicu A, Lindberg F, Hexeberg S, Moan J, et al. (2009) The dependency of vitamin D status on body mass index, gender, age and season. Anticancer Res 29(9): 3713-3720.
- Arunabh S, Pollak S, Yeh J, Aloia JF (2003) Body fat content and 25-hydroxyvitamin D levels in healthy women. J Clin Endocrinol Metab 88: 157-161.
- Hypponen E, Power C (2006) Vitamin D status and glucose homeostasis in the 1958 British Birth Cohort. Diabetes Care 29(10): 2244-2246.
- McGill A, Stewart J, Lithander F, Strick C, Poppitt S (2008) Relationships of low serum vitamin D3 with anthropometry and markers of metabolic syndrome and diabetes in overweight and obesity. Nutrition Journal 7(4): 52.
- Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF (2000) Decreased bioavaillability of vitamin D in obesity. Am J Clin Nutr 72: 690-693.
- Carlin A, Rao D, Meslemani A, Genaw J, Parikh N, et al. (2006) Prevalence of vitamin D depletion among morbidly obese patients sеeking gastric bypass surgery. Surg Obes Relat Dis 2: 98-103.
- Sanchez-Hernandez J, Ybarra J, Gich I, Leiva AD, Rius X, et al. (2005) Effects of bariatric surgery on vitamin D status and secondary hyperparathyroidism: a prospective study. Obes Surg 15: 1389-1395.
- Snijder MB, van Dam RM, Visser M, Deeg DJ, Dekker JM, et al. (2005) Adiposity in relation to vitamin D status and parathyroid hormone levels: a population-based study in older men and women. J Clin Endocrinol Metab 90: 4119-4123.
- Hamoui N, Kim K, Anthone G, Crookes PF (2003) The significance of elevated levels of parathyroid hormone in patients with morbid obesity before and after bariatric surgery. Arch Surg 138: 891-897.
- Kamycheva E, Sundsfjord J, Jorde R (2004) Serum parathyroid hormone level is associated with body mass index. The 5th Tromso study. Eur J Endocrinol 151: 167-172.
- Hultin H, Edfeldt K, Sundbom M, Hellman P (2010)Left-Shifted Relation between Calcium and Parathyroid Hormone in Obesity.J Clin Endocrin Metab95(8): 3973-3981.
- Premaor M, Comim F, Compston J (2014) Obesity and Fractures.Arq Bras Endocrinol Metab 58(5).
- Fried M, Yumuk V, Oppert JM, Scopinaro N, Torres AJ, et al. (2013) Interdisciplinary European Guidelines on Metabolic and Bariatric Surgery. Obes Facts l6: 449-468.
- Mechanick JI, Youdim A, Jones DB, Garvey WT, Hurley DL, et al. (2013) Clinical Practice Guidelines for the Perioperative Nutritional, Metabolic, and Nonsurgical Support of the Bariatric Surgery Patient—2013 Update: Cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity (Silver Spring) 1(27).
- Gasteyger C, Suter H, Gaillard R, Giusti V (2008) Nutritional deficiencies after Roux-en-Y gastric bypass for morbid obesity often cannot be prevented by standart multivitamin supplementation. Am J Clin Nutr 87: 1128-1133.
- Verger E, Aron-Wisnewsky J, Dao M, Kayser BD, Oppert JM, et al. (2016) Micronutrient and Protein Deficiencies After Gastric Bypass and Sleeve Gastrectomy: a 1-year Follow-up. Obes Surg 26(4): 785-796.
- van Rutte PWJ, Aarts EO, Smulders JF, Nienhuijs SW (2014) Nutrient deficiencies before and after sleeve gastrectomy. Obes Surg 24(10): 1639-1646.
- Alexandrou A, Armeni E, Kouskouni E, Tsoka E, Diamantis T, et al. (2014)Cross-sectional long-term micronutrient deficiencies after sleeve gastrectomy versus Roux-en-Y gastric bypass: a pilot study.Surg Obes Relat Dis 10(2): 262-268.
- Moizé V, Ibarzabal A, Sanchez Dalmau B, Flores L, Andreu A, et al. (2012) Nystagmus: an uncommon neurological manifestation of thiamine deficiency as a serious complication of sleeve gastrectomy.Nutr Clin Pract 27(6): 788-792.
- Peterli R, Wolnerhanssen B, Vetter D, Nett P, Gass M, et al. (2017) Laparoscopic Sleeve Gastrectomy Versus Roux-Y-Gastric Bypass for Morbid Obesity—3-Year Outcomes of the Prospective Randomized Swiss Multicenter Bypass or Sleeve Study (SM-BOSS). Ann Surg 265: 466-473.
- Adamczyk P, Bužga M, Holéczy P, Švagera Z, Zonča P, et al.(2015)Body Size, Bone Mineral Density, and Body Composition in Obese Women After Laparoscopic Sleeve Gastrectomy: A 1-Year Longitudinal Study. Horm Metab Res47(12):873-879.
- Nogues X, Goday A, Peña MJ, Benaiges D, de Ramón M, et al. (2010)Bone mass loss after sleeve gastrectomy: a prospective comparative study with gastric bypass. Cir Esp 88(2):103-109.
- Ruiz-Tovar J, Oller I, Priego P, Arroyo A, Calero A, et al. (2013) Short- and mid-term changes in bone mineral density after laparoscopic sleeve gastrectomy.Obes Surg 23(7):861-866.
- Peterson L, Zeng X, Caufield-Noll CP, Schweitzer MA, Magnuson TH, et al. (2016) Vitamin D status and supplementation before and after bariatric surgery: a comprehensive literature review. Surg Obes Relat Dis 12(3): 693-702.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences