Tuberculosis in HIV/AIDS Patients
Matilda Gjergji1*, Jul Bushati2, Arjan Harxhi1, Hasan Hafizi2 and Pellumb Pipero1
1Department of Infectious Diseases, University Hospital Center “Mother Teresa”, Tirana, Albania
2Department of Pneumology, University Hospital “Shefqet Ndroqi”, Tirana, Albania
- Corresponding Author:
- Matilda Gjergji
Department of Infectious Diseases
University Hospital Center “Mother Teresa”
Rruga e Dibrës 372, Tirana 1000, Albania Tirana
Tel: +355 4 234 9209
E-mail: gjergjid2000@yahoo.com
Received date: August 21, 2017; Accepted date: August 29, 2017; Published date: Spetember 05, 2017
Citation: Gjergji M, Bushati J, Harxhi A, Hafizi H, Pipero P (2017) Tuberculosis in HIV/AIDS Patients. Adv Tech Clin Microbiol. Vol. 1 No. 3:16.
Abstract
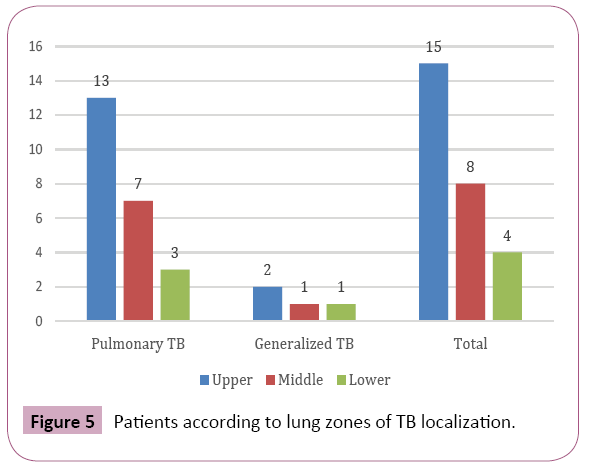
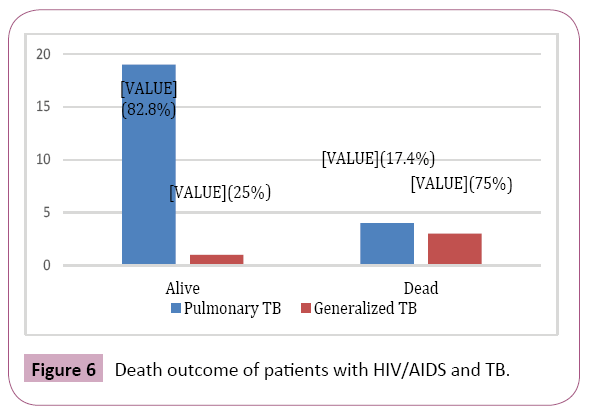
Background: In Albania the incidence of people with both TB and HIV is small; however, it is a category that should not be neglected. Objective: The main aim of the study is to assess the characteristics of TB in the HIV/AIDS patients. Methods: During 2004-2015 years are studied 77 HIV/AIDS patients with pulmonary complications from which in all resulted 27 (32.2%) cases of TB, 23 (85.2%) cases as pulmonary tuberculosis and 4 (14.2%) cases as generalized tuberculosis. Results: The average age of the subjects with pulmonary TB and generalized TB was respectively 48.1 ± 9.8 and 47.8 ± 10.2 years, males –22 (95.7%) and 2(50%), smokers – 21 (91.3%) and 4 (100%), urban residents 16 (69.6%) and 3 (75%), unemployed – 9 (39.1%) and 1 (25%). Period of knowing HIV infection was respectively 6.2 ± 2.2 and 4 ± 2.2 years, period of ART treatment - 5.3 ± 2.8 and 2.9 ± 3. According to the count of CD4 cellules, 6 (26.1%) patients with pulmonary TB resulted with 200-999 cells/ml, 8 (34.8%) - with 100-199 cells/ml and 9(39.1%) <100 cells/ml and all generalized TB patients with <100 cells/ml. Clinical manifestation of pulmonary TB only were: cough – 73.9%, expectoration- 43.5%, dyspnoea – 34.8%, chest pain – 26.1%, haemoptysis – 26,1%, weight loss – 65.2%, fatigue – 87%, fever – 78.3%, anorexia- 78.3%; chest radiograph showing evidence of adenopathy in 5 (21.7%) cases and with CT in 7 (30.4%) cases. Lesions localised on the right lung in 5 (21.7%) cases, on the left- 8 (34.8%), and bilateral –10 (43.5%). Upper zone localization was in 13 (56.5%) cases, middle zone – 7 (30.4%) and lower zone–3 (13%). During the study died 4 (17.4%) of patients with pulmonary TB, 3 patients with 100-199 CD4 cells/ml and one patient with <100 CD4 cells/ml and 3 (75%) of patients with generalized TB all with <100 CD4 cells/ml. Conclusion: TB is a common respiratory complication with high mortality rate in HIV/AIDS patients. The level of CD4+ count is predictive factor for clinical manifestation and prognosis.
Keywords
HIV/AIDS; CD4+; Pulmonary TB; Generalized TB; ART; Mortality
Abbreviations
AIDS: Acquired Immune Deficiency Syndrome; ART: Antiretroviral Therapy; HIV: Human Immunodeficiency Virus; LTBI: Latent TB Infection; TB: Tuberculosis
Introduction
HIV infection has a profound impact on the global tuberculosis (TB) problem. Due to its ability to destroy the immune system, HIV has emerged as the most significant risk factor for progression of dormant TB infection to clinical disease [1-4].
Progression from TB infection to TB disease is accelereted from different factors that reduced eficacity of body defence, like malnutrition, Diabetes, HIV immune deficencies, and treated patientes for a long time with immunosuppressors and corticosteroids therapy. The impact that HIV has on the pathogenesis of TB is clear. From above factors HIV infection plays the main role in increasing probbability of developing from infection to TB disease, and raise the risk of reactivation of the tuberculosis (post primary TB). It is one of the most important risk factors associated with an increased risk of latent TB infection (LTBI) progressing to active TB disease. HIV-infected people have an annual risk of 5% to 15% of developing active TB once infected [5]. TB is the most common opportunistic infection in people living with HIV worldwide. TB also occurs earlier in the course of HIV infection than many other opportunistic infections.
When someone has both HIV and TB each disease speeds up the progress of the other. In addition to HIV infection speeding up the progression from latent to active TB, TB bacteria also accelerate the progress of HIV infection [6].
The risk of progressing from latent to active TB is estimated to be between 12 and 20 times greater in people living with HIV than among those without HIV infection [7]. Overall it is considered that the lifetime risk for HIV negative people of progressing from latent to active TB is about 5-10%, whereas for HIV positive people this same figure is the annual risk [8,9].
In 2015 there were an estimated 10.4 million new cases of active TB worldwide. Globally 11% of the incident TB cases in 2015 are estimated to have been among people living with HIV [10].
It is also the most common cause of death in HIV-positive adults living in developing countries, despite being a preventable and treatable disease [11]. Around one third of the deaths in the AIDS subjects came from tuberculosis. Approximately 12-15 million people around the world are co-infected with HIV and TB. Tuberculosis can lead to 15% deaths in AIDS patients worldwide [12-15].
The risk of death in co-infected individuals is also twice that of HIV infected individuals without TB, even when CD4 cell count and antiretroviral therapy are taken into account [8,16,17].
By the world literature TB is second cause of the deaths in HIV positive patients. HIV positive patients have 30 times more risk, to have tuberculosis, than HIV negative. TB is the cause for 40% of deaths in AIDS patients in Africa and Asia [18]. Also TB is the largest single cause of death in the setting of AIDS [11], accounting for about 26% of AIDS-related deaths [15], 99% of which occur in developing countries [19].
In 2015 400,000 people who had both TB and HIV are estimated to have died, in addition to the 1.4 million people who died from TB alone [10]. Those people who have HIV and TB co-infection when they die are internationally reported as having died of HIV infection [20].
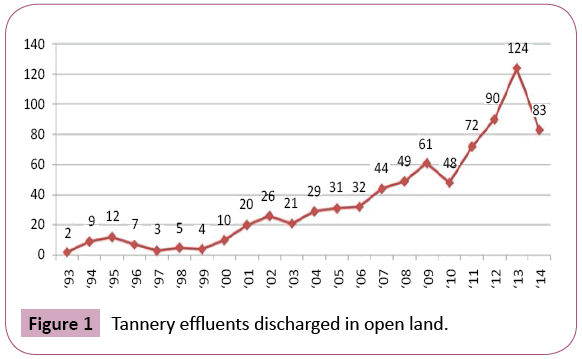
The annual number of new HIV diagnoses in Albania, 1993-2014 [21] are presented in Figure 1.
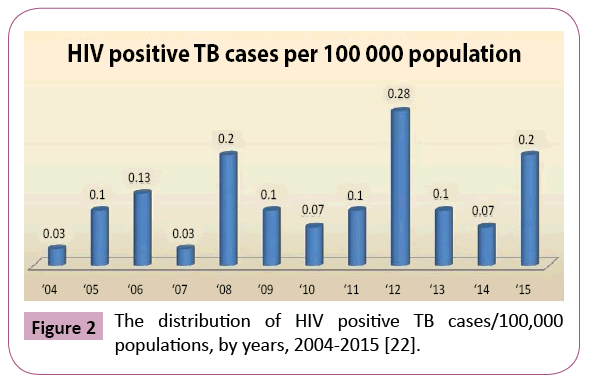
In Albania the number of people with both TB and HIV is small, from January 2004 to December 2015, approximately 5.6 % of the 751 HIV positive people in Albania are co-infected with TB (from 751 HIV positive cases, 42 cases have TB and HIV coinfection) (Figure 2), however, it is a category that should not be neglected [22].
More than 60% of tuberculosis cases in HIV patients are pulmonary disease. Clinical manifestation depend from the HIV disease stage. In early stage when the celluary immunity is quasy perserved, pulmonary tuberculosis resembles with postprimary TB in adults, with cavernes and infiltrates in the superior lobes of the lungs.Tuberculine test are usually positive, also positive in sputum smear microscopy. In HIV advanced disease with damaged cellular immunity, TB presentation is non-specific: fever, weight loss, fatigue, with or without cough.
Patients with low CD4+ count, may have extrapulmonary disease in bone narrow, lymphatic nodes, CNS, liver ect. HIV positive people with pulmonary TB may have the classic symptoms of TB, but many people with both TB and HIV infection have few symptoms of TB or even less specific ones. In addition, up to a fifth of people with both pulmonary TB and HIV have normal chest X-rays. HIV positive people with TB may indeed frequently have so called “sub clinical” TB, which often is not recognized as TB and subsequently there are delays in both TB diagnosis and TB treatment. HIV infected people are also more likely than people who are not infected with HIV to have extra pulmonary TB. Forty to eighty percent of HIV infected people with TB have extra pulmonary disease, compared with 10-20% of people without HIV [23].
Starting with the issues above it is important knowing the situation of tuberculosis in HIV/AIDS patients in our country. We tried to have a comprehensive insight about the occurrence of pulmonary manifestations in HIV/AIDS patients, and especially coexistence with TB. Design study is to answer questions concerning sociocultural factors in patients living with HIV/AIDS and TB, clinical characteristics, impact of several factors and behavioral in the course of the disease, predictive role of CD4 count.
Materials and Methods
This was a retrospective observational cohort study. It was conducted at the Outpatient service for HIV/AIDS, part of Infectious Department, University Hospital Center, “Mother Teresa”, Tirana, Albania. From January 2004 to December 2015 among 77 adult HIV/AIDS patients with pulmonary complications, there were 27 cases of TB, from them 23(85.2%) cases as pulmonary tuberculosis and 4 (14.2%) cases as generalized tuberculosis. The diagnosis of tuberculosis was based on clinical symptomatology, radiological and/or microbiological evidence of tubercular infection or with histology confirmation.
Based on a protocol, demographic data, clinical-radiological characteristics, and CD4 count were collected. CD4 count was determined by flow cytometry. The CD4 count were obtained at clinical presentation. They were used to assess the magnitude of injury to the host immune system.
The main outcome variable was TB diagnosis. CD4 count, age, gender, smoking habits, residing in urban/rural areas, period of knowing HIV infection, clinical manifestation, chest radiograph presentation, death were the main independent variables.
The study was approved by the ethics committee of Medical University of Tirana, Albania.
Data Analysis
All data collected was dropped in the Microsoft Excel program, from which they were exported to Statistical Package for Social Sciences (SPSS) 20.0 and Medstat, with which statistical data analysis was performed. For all categoric variables (nominal, including binary/dichotomous and ordinal), the absolute numbers and percentages were calculated. For all numeric variables, where data were subject to normal distribution, arithmetic averages ± standard deviations were computed. Differences between discrete group variables was carried out using Hi-square test. Data was compiled by simple and composite tables as well as graphs. Significant values of p ≤ 0.05 were considered.
Results
In the serie of 77 HIV/AIDS patients with pulmonary complications, tuberculosis has been diagnosed in 27 (32.2%) patients, 23 (27.4%) –pulmonary TB and 4 (4.8%) generalized TB. According to all 27 TB patients, with pulmonary TB were 23 (85.2%) and with generalized TB - 4 (14.8%). PCP was concomitant in 3 patient and COPD in one patients with HIV/AIDS and pulmonary TB.
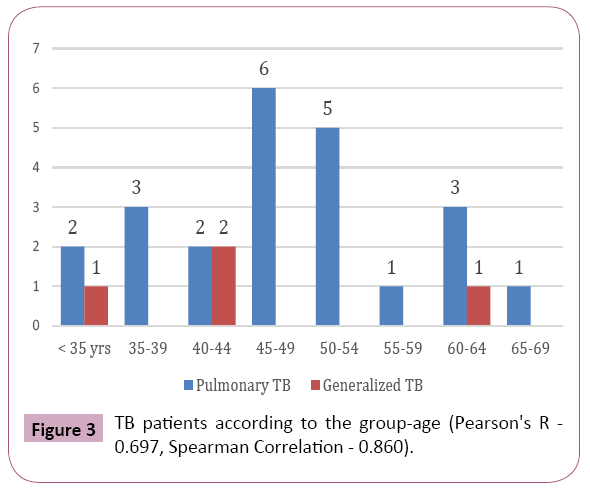
The average age of the subjects with pulmonary TB and generalized TB was respectively 48.1 ± 9.8 (32 to 67 years) and 47.8 ± 10.2 (42-63 years) years (Figure 3), males – 22 (95.7%) and 2 (50%) (Pearson Chi-Square Asymptotic Significance (2-sided) 0.007), smokers – 21 (91.3%) and 4 (100%) (Pearson's R 0.558, Spearman Correlation 0.558), urban residents 16 (69.6%) and 3 (75%), low educations – 11 (47.8%) and 4(100%), unemployed – 9(39.1%) and 1(25%),workers - 6 (26.1%) and 2 (50%).
For pulmonary TB and generalized TB, respectively, time of knowing HIV infection was 6.2 ± 2.2 (2 to 10 years) and 4 ± 2.2 (1 to 6 years) years, the average period treated with antiretroviral therapy - 5.3 ± 2.8 (1 to 10 years) and 2.9 ± 3 (0.2 to 6 years).
The pulmonary TB patients have been known living with HIV <3 years in 2 (8.7%) cases, 3-5 years in 7 (30.4%), 6-8 years in 9 (39.1%) and 9-12 years in 5 (21.7%) cases. The period of treatment with antiretroviral therapy in the pulmonary TB cases were ≤ 1 year in 2 (8.7%) cases, 2-4 years in 8 (34.8%) cases, 5-7 years in 7 (30.4%) cases and 8-10 years in 6 (26.1%) cases.
The generalized TB patients have been known living with HIV <3 years in 1 (25%) cases, 3-5 years in 2 (50%) and 6-8 years in 1 (25%). The period of treatment with antiretroviral therapy in the pulmonary TB cases were ≤ 1 year in 2 (50%) cases and 5-7 years in 2 (50%) cases.
CD4 counts in pulmonary TB patients resulted 200-299 cells/ml in 6 (26.1%) patients, 100-199 cells/ml in 8 (34.8%) patients and in 9 (39.1%) patients in level <100 cells/ml, while in all patients with generalized TB was <100 cells/ml. (Pearson's R 0.571, Spearman Correlation 0.602).
Clinically, pulmonary tuberculosis has acute onset in 9 (39.1%) patients, sub-acute in 12 (52.2%) patients, and chronic in 2 (8.7%) patients. In Table 1 are presented clinical manifestations and frequencies in relation to the all 77 patients with pulmonary complications, 23 cases with pulmonary TB and 4 cases with generalized TB.
| Symptoms | All pulmonary cases | Pulmonary TB | Generalized TB |
|---|---|---|---|
| Cough | 61 (79.2%) | 17 (73.9%) | 4 (100%) |
| Sputum | 31 (40.3%) | 10 (43.5%) | 2 (50%) |
| Dyspnea at rest | 26 (33.8%) | 8 (34.8%) | 2 (50%) |
| Dyspnea on exertion | 29 (37.7%) | 6 (26.1%) | 2 (50%) |
| Chest pain | 24 (31.2%) | 6 (26.1%) | 1 (25%) |
| Hemoptysis | 22 (28.6%) | 6 (26.1%) | 1 (25%) |
| Weight loss | 50 (64.9%) | 15 (65.2%) | 3 (75%) |
| Weakness | 62 (80.5) | 20 (87%) | 2 (50%) |
| Fever | 51 (66.2%) | 18 (78.3%) | 3 (75%) |
| Anorexia | 49 (63.6%) | 18 (78.3%) | 1 (25%) |
| Osteoarticular pain | 3 (3.9%) | 1 (4.3%) | - |
| Sweating | 3 (3.9%) | 3 (13%) | - |
| Headache | 1 (1.3%) | - | 1 (25%) |
| Diarrhea | 2 (2.6%) | 1 (4.3%) | - |
Table 1: Respiratory symptoms among HIV/AIDS patients with pulmonary manifestations.
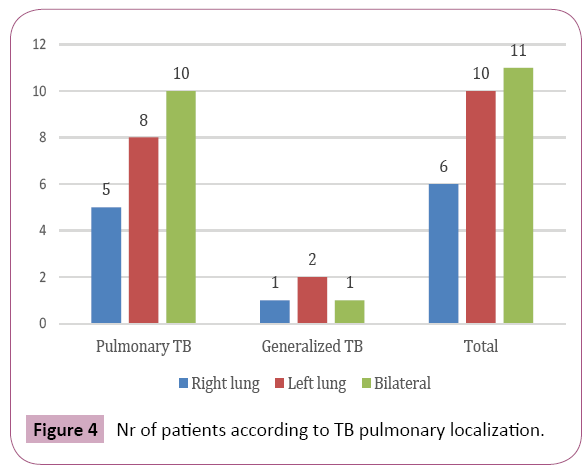
Pulmonary TB lesions are localised on the right lung in 5 (21.7%) cases, on the left - 8 (34.8%), and bilateral –10 (43.5%); generalized TB – 1 (25%) case on the right, 2 (50%) on the left and 1 (25%) bilateral; from all cases - 6 (22.2%) case on the right, 10 (37%) on the left and 11 (40.8%) bilateral (Figure 4). Pulmonary Tb lesions are localized in upper zones in 13 (56.5%) cases, middle zone – 7(30.4%) and lower zone – 3(13%): generalized TB - in upper zones in 2 (50%) cases, middle zone – 1 (25%), and lower zone – 1 (25 %); from all cases - in upper zones in 15 (55.6%) cases, middle zone – 8 (29.6%) and lower zone – 4 (14.8%) (Figure 5). More common was seen bilateral pulmonary lesions (Figure 4). Of the 27 patients, 12 (44.4%) presented with atypical patterns, with parenchymal opacities at middle and lower zones. Chest radiograph showing evidence of adenopathy in 5 (21.7%) cases, while with CT in 7 (30.4%) cases.
Of all patients with HIV/AIDS and TB were reported 7 (26%) deaths (Figure 6): 4 (17.4%) of pulmonary TB and 3 (75%) of generalized TB. Deaths in the patients of pulmonary TB were grouped in level of CD4<199 cells/ml, while in generalized TB in CD4<100 cells/ ml. (Pearson Chi-Square 5.888, Asymptotic Significance (2-sided) 0.015).
Discussion
While TB and HIV co-infection remains a major public health problem in many parts of the world, the number is still lower in Albania [24]. When someone has both HIV and TB each disease speeds up the progress of the other [25]. TB is the most common opportunistic infection in people living with HIV worldwide [26]. TB also occurs earlier in the course of HIV infection than many other opportunistic infections [27].
With regard to the gender structure, TB - HIV patients have been predominated in males - 88.8%, comparewith 50-69% in males TB in HIV seronegative [25,26]. This is in accordance with another study in Albania [22], where 88% of TB and HIV patients were males. In Albania, more men than women are diagnosed with HIV and TB and die from it like in most of the world. This gender ratio is reported almost the same from decades in our country, suspecting under-diagnosis in women. It may be supposed that women with tuberculosis are not declared for a lot of sociocultural causes or various issue related with access in healthcare system and health services [22,27-29].
Therefore, notwithstanding the biological explanations, there are strong arguments in favor of a link between female undernotification rates in the context of specific cultural factors which play an important role in developing and transitional societies [30]. Similar situation may well apply in transitional Albania. However, not all researchers have found such a gender discrepancy [31,32].
The average age of the subjects with pulmonary TB was 48.1 ± 9.8 (32 to 67 years), with most affected 45-54 years (47.8%). In other studies the most affected age was 36-45 years old (35%) [22], under 33-40 years were at a higher risk for TB [32], 38-47 years and 28-37 years age groups (both 40%) [33] and 25-44 years [34] that may reflect behavioral differences in terms of exposure and various socio-economic factors [35].
HIV/AIDS with pulmonary TB and generalized TB, respectively, were smokers in 21 (91.3%) and 4 (100%) patients, this probably, among others, with the negative impact of tobacco related to the progression of both diseases. Although both smoking and HIV infection may be associated through their common associations with poverty and high-risk behavior, tobacco smoking appears to be an independent and important risk factor for contracting HIV [36,37]. Other studies have demonstrated rate of progression of HIV infection to AIDS in smokers [38,39], but this association has not been observed in all studies [40,41]. Smoking further raises the risk of contracting TB in HIV-positive persons [42]. HIV infected smokers also have higher respiratory symptoms and risk of mortality, when compared to non-smokers [43].
Many patients in our study had low educations, and unemployed. Education level is a risk factor for active TB among HIV/AIDS persons [44,45]. More than 70% of the patients with tuberculosis in our country had 0-8 years of education, a level which is significantly higher than in the overall Albanian population of the same age-group [46]. With regard to the structure of occupations, TB-HIV patients have been predominated in the unemployed and workers group, because of poor social economic factors and lack of heath care adherence.
The clinical presentation of pulmonary TB can vary widely in both immunocompetent and immunocompromised hosts. In general, the presentation in HIV-infected patients is similar to that seen in HIV-uninfected patients. Symptoms usually are present for weeks to months, and an acute onset of fever and cough is more suggestive of a non-mycobacterial pulmonary process. This is in accordance with our results of sub-acute onset of TB in most cases. In HIV-infected patients, clinical manifestations of pulmonary TB reflect different levels of immunosuppression. Earlier in the course of HIV disease, TB is more likely to present as classic reactivation-type disease, whereas patients with advanced immunosuppression are more likely to present with findings consistent with primary TB.
According to the respiratory symptoms we could not find significant difference in the patient with pulmonary complication vs. tuberculosis. Assessments of respiratory symptoms in HIV subject can be very difficult for many reasons. Respiratory symptoms are common in HIV patients, but may come from a wide spectrum of diseases. The spectrum of lung diseases in HIV-infected patients includes those linked to HIV and those not related to HIV.
Of the 27 patients, 12 (44.4%) presented with atypical patterns, with parenchymal opacities at middle and lower zones. Chest radiograph showing evidence of adenopathy in 5 (21.7%) cases, while with CT in 7 (30.4%) cases. CT scan, resulted a useful tool for assessing patients with intrathoracic adenopathy, especially in the suspicious of adenopathy in radiographic examination.
The chest radiograph is important examination of diagnosis for pulmonary TB. In tuberculosis patients with relatively intact immune system, the radiographic findings are similar to those met with in non-HIV population [47]. In patients with severe immunodeficiency, there are atypical manifestations like diffuse or lower lobe bilateral reticulo-nodular infiltrates [48]. Upper-lobe infiltrates and cavities are the typical findings in reactivation TB, whereas intrathoracic lymphadenopathy and lower-lobe disease are seen in primary TB. In HIV-infected persons with higher CD4 counts (>200 cells/ml), the radiographic pattern tends to be one of reactivation disease with upper-lobe infiltrates with or without cavities [49]. In HIV-infected persons who have a greater degree of immunosuppression (CD4<200 cells/ml), a pattern of primary disease with intrathoracic lymphadenopathy and lower-lobe infiltrates is seen. As chest radiographs may appear normal in up to 21% of those with culture-positive TB and CD4 of <50 cells/ml [50] a high index of suspicion must be maintained in evaluating an HIV-infected patient with symptoms suggestive of TB [51,52].
Every opportunistic infections and neoplastic disease have the specific clinical and radiographical presentations. However, there may be considerable variations and overlapping in these presentations. There is not a standard constellation signs, symptoms and imagery features for diagnosis of Tuberculosis in HIV patients. Therefore, when it is possible, it is preferable to have a definitive microbiological diagnosis or pathological diagnosis.
Several studies have used the patients' CD4 cell counts to assess immune suppression and found that a lower CD4 cell count was associated with a higher risk of TB infection [32,53- 57]. These studies are consistent with our findings where CD4 counts in pulmonary TB patients resulted 200-299 cells/ml in 6 (26.1%) patients, 100-199 cells/ml in 8 (34.8%) patients and in 9 (39.1%) patients in level <100 cells/ml, while in all patients with generalized TB was <100 cells/ml. (Pearson's R 0.571, Spearman Correlation 0.602) The depletion of CD4 cells, which is a main feature of AIDS, is certainly an important contributor to the increased risk of reactivation of latent TB and susceptibility to new M. tuberculosis infection. From the data of the study, results a strong correlation between CD4 count cells and TB severity, being the lowest in generalised forms, associated with high deaths rates (75% cases). The CD4 determine the immunosuppression degree in HIV positive patients. There is an inverse relationship between CD4 count and immunosuppression degree. Some of the relevant studies have concluded that CD4 is a strong predictor of the HIV disease progress and patients survival [58].
Of all patients with HIV/AIDS and TB were reported 7 (26%) deaths: 4 (17.4%) of pulmonary TB and 3 (75%) of generalized TB. Deaths in the patients of pulmonary TB were grouped in level of CD4<199 cells/ml, while in generalized TB in CD4<100 cells/ ml. (Pearson Chi-Square 5.888, Asymptotic Significance (2-sided) 0.015). We conclude, according with the literature data, that the CD4 cell count is a strong predictor of the risk of death in HIV patients with pulmonary complications [59]. In another study in our country the specific weight of mortality was 45.2% [22]. Death tuberculosis rates in HIV patients are reduced in 32% since 2004 year [60,61]. Patients with HIV and tuberculosis in Eastern Europe have a risk of death nearly four-times higher than that in patients from Western Europe and Latin America. This increased mortality rate is associated with modifiable risk factors such as lack of drug susceptibility testing and suboptimal initial antituberculosis treatment in settings with a high prevalence of drug resistance. Urgent action is needed to improve tuberculosis care for patients living with HIV in Eastern Europe [62].
Conclusion
TB is a common respiratory complication with high mortality rate in HIV/AIDS patients. The level of CD4+ count is predictive factor for severity of clinical manifestation and prognosis. Co-infection TB-HIV is more prevalent in males, smokers, low educations and unemployed. TB is often presented with atypical radiological patterns.
Acknowledgement
The authors wish to thank all subjects who participated in this study for their help in collecting the data and care health for patients living with HIV/AIDS.
Conflict of Interest
No competing financial interests exist.
References
- Selwyn PA, Hartel D, Lewis VA (1989) A prospective study of the risk of tuberculosis among intravenous drug users with human immunodeficiency virus infection. N Engl J Med 320: 545–550.
- Kochi A (1991) The global tuberculosis situation and the new control strategy of WHO. Tubercle 72: 1-6.
- Narain JP, Raviglione MC, Kochi A (1992) HIV-associated tuberculosis in developing countries: Epidemiology and strategies for prevention. Tubercle Lung Dis 73: 311-321.
- San KE, Muhamad M, Pulmonary (2001) Tuberculosis in HIV Infection: The relationship of the radiographic appearance to CD4 T-lymphocytes count. Malays J Med Sci 8: 34-40.
- Rieder HL (1999) CHAPTER 3, Tuberculosis, infection with the human immunodeficiency virus (HIV), In: Epidemiologic basis of tuberculosis control, p: 69.
- Mayer K (2010) Synergistic pandemics: Confronting the global HIV and tuberculosis epidemics. Clin Infect Dis 50.
- Luetkemeyer A (2013) Tuberculosis and HIV, HIV in site knowledge base chapter.
- Miller R (2001) AIDS and the lung. Ne ABC OF AIDS, Fifth Edition. Edited by MICHAEL W ADLER, BMJ Publishing Group, pp: 30-37.
- Implementing the WHO Stop TB strategy: A handbook for national tuberculosis control programmes. Geneva, World Health Organization, p: 67.
- Global Tuberculosis Control (2016) WHO, Geneva.
- Corbett EL, Watt CJ, Walker N, Maher D, Williams BG, et al. (2003) The growing burden of tuberculosis: Global trends and interactions with the HIV epidemic. Arch Intern Med 163: 1009-1021.
- (2001) Mycobacterial and nonbacterial pulmonary complications in hospitalized patients with HIV: A prospective cohort study. BMC Pulm Med 1.
- USPHS/IDSA Prevention of Opportunistic Infections Working Group (1995) USPHS/IDSA guidelines for the prevention of opportunistic infections in persons infected with HIV: Disease specific recommendations. Clin Infect Dis 21: S32-S43.
- Grau I, Pallares R, Tubau F, Schulze MH, Llopis F, et al. (2005) Epidemiologic changes in bacteraemia pneumococcal disease in patients with human immunodeficiency virus in the era of highly active antiretroviral therapy. Arch Intern Med 165: 1533-1540.
- Getahun H, Gunneberg C, Granich R, Nunn P (2010) HIV infection-associated tuberculosis: The epidemiology and the response. Clin Infect Dis 50: S201-S207.
- (2003) Treating TB and HIV – Healthlink Worldwide (2003).
- Suchindran S (2009) Is HIV infection a risk factor for multi-drug resistant tuberculosis? A systematic review. PLoS ONE 4: e5561.
- Global Tuberculosis Report (2013).
- Collins KR, Quinones-Mateu ME, Toossi Z, Arts EJ (2002) Impact of tuberculosis on HIV-1 replication, diversity and disease progression. AIDS Rev 4: 165-176.
- International Classification of Diseases (ICD) (2010) WHO, Geneva.
- The Global Fund (2015) To fight AIDS, tuberculosis and malaria, TB and HIV, concept note. Investing for impact against tuberculosis and HIV. Single TB and HIV Concept Note Albania.
- Balla F, Drevishi M, Bani R, Balla E, Bino S (2016) HIV/TB mortality in Albania during the years 2004-2015, Proceedings of Academics Era International Conference, Zurich, Switzerland.
- Sterling T (2010) HIV infection-related tuberculosis: Clinical manifestations and treatment. Clin Infect Dis 50: S 223-230.
- World Health Organization (2006) Guidelines for the programmatic management of drug-resistant tuberculosis.
- Kurti V, Hafizi H, Kurti B, Marku F, Mema D (2014) Distribution of tuberculosis cases in Albania during 2012-2013.Management in health, pp: 16-18.
- (2015-2019) National Tb Strategy Albania.
- (2017) Albania marks World TB Day, promotes TB care delivery.
- Pitchenik AE, Rubinson HA (1985) The radiographic appearance of tuberculosis in patients with the acquired immune deficiency syndrome(AIDS) and pre-AIDS. Am Rev Respir Dis 131: 393-396.
- Surveillance report. Tuberculosis surveillance and monitoring in Europe (2013) European Centre for Diseases Prevention and Control. WHO. Regional Office for Europe. (World Health Organization. Global tuberculosis control annual reports from 1997 to 2008. Geneva, Switzerland: WHO.
- World Health Organization. Global Tuberculosis Report (2012) Geneva: World Health Organization.
- Johansson E, Long NH, Diwan VK, Winkvist A (2000) Gender and tuberculosis control: Perspectives on health seeking behavior among men and women in Vietnam. Health Pol 52: 33-51.
- Lawn SD (2005) Tuberculosis and HIV co-infection. Medicine 33: 112-113.
- Erhabor O, Jeremiah ZA, Adias TC, Okere CE (2010) The prevalence of human immunodeficiency virus infection among TB patients in Port Harcourt Nigeria.
- van der Werf MJ, Ködmön C, Zucs PH, Hollo V, Amato-Gauci AJ, et al. (2016) Tuberculosis and HIV co-infection in Europe: Looking at one reality from two angles. AIDS 30: 2845-2853.
- Sudre P (1996) Risk factors for tuberculosis among HIV-infected patients in Switzerland. Eur Respir J 9: 279-283.
- Chao A, Bulterys M, Musanganire F, Habimana P, Nawrocki P, et al. (1994) Risk factors associated with prevalent HIV-1 infection among pregnant women in Rwanda. National University of Rwanda-Johns Hopkins University AIDS Research Team. Int J Epidemiol 23: 371-380.
- Penkower L, Dew MA, Kingsley L, Becker JT, Satz P, et al. (1991) Behavioral, health and psychosocial factors and risk for HIV infection among sexually active homosexual men: The Multicenter AIDS Cohort Study. Am J Public Health 81: 194-196.
- Nieman RB, Fleming J, Coker RJ, Harris JR, Mitchell DM (1993) The effect of cigarette smoking on the development of AIDS in HIV-1-seropositive individuals. AIDS 7: 705-710.
- Feldman JG, Minkoff H, Schneider MF, Gange SJ, Cohen M, et al. (2006) Association of cigarette smoking with HIV prognosis among women in the HAART era: A report from the women’s interagency HIV study. Am J Public Health 96: 1060-1065.
- Craib KJ, Schechter MT, Montaner JS, Le TN, Sestak P, et al. (1992) The effect of cigarette smoking on lymphocyte subsets and progression to AIDS in a cohort of homosexual men. Clin Invest Med 15: 301-308.
- Webber MP, Schoenbaum EE, Gourevitch MN, Buono D, Klein RS (1999) A prospective study of HIV disease progression in female and male drug users. AIDS 13: 257-262.
- Miguez-Burbano MJ, Burbano X, Ashkin D, Pitchenik A, Allan R, et al. (2003) Impact of tobacco use on the development of opportunistic respiratory infections in HIV seropositive patients on antiretroviral therapy. Addict Biol 8: 39-43.
- Crothers K, Griffith TA, McGinnis KA, Rodriguez-Barradas MC, Leaf DA, et al. (2005) The impact of cigarette smoking on mortality, quality of life and comorbid illness among HIV-positive veterans. J Gen Intern Med 20: 1142-1145.
- Mohammed T (2011) Risk factors of active tuberculosis in people living with HIV/AIDS in South-West Ethiopia: A case control study. Ethiop J Health Sci 21.
- Hussain H, Akhtar S, Nanan D (2003) Prevalence of and risk factors associated with Mycobacterium tuberculosis infection in prisoners, North West Frontier Province, Pakistan. Int J Epidemiol 32: 794-799.
- Burazeri G, Kark JD (2011) Hostility and acute coronary syndrome in a transitional post-communist Muslim country: A population-based study in Tirana, Albania. Eur J Public Health 21: 469-476.
- Theuer CP, Hopewell PC, Elias D (1990) Human immunodeficiency virus infection in tuberculosis patients. J Infect Dis 162: 8.
- Raviglione MC, Narain JP, Kochi A (1992) HIV- associated tuberculosis in developing countries: Clinical features, diagnosis and treatment. Bull World Health Org 70: 515.
- Post FA, Wood R, Pillay GP (1995) Pulmonary tuberculosis in HIV infection: Radiographic appearance is related to CD4+ T-lymphocyte count. Tubercle Lung Dis 76: 518-521.
- Chamie G, Luetkemeyer A, Walusimbi-Nanteza M (2010) Significant variation in presentation of pulmonary tuberculosis across a high resolution of CD4 strata. Int J Tuberc Lung Dis 14: 1295-1302.
- Greenberg SD, Frager D, Suster B (1994) Active pulmonary tuberculosis in patients with AIDS: Spectrum of radiographic findings (including a normal appearance). Radiology 193: 115-119.
- Long R, Maycher B, Scalcini M (1991) The chest roentgenogram in pulmonary tuberculosis patients seropositive for immunodeficiency virus type-1. Chest 99: 123-127.
- Catherine FH, Mutevedzi PC, Lessells RJ, Cooke GS, Tanser FC, et al. (2010) The tuberculosis challenge in a rural South African HIV programme. BMC Infect Dis 10: 23.
- Kruk A (2011) Tuberculosis among HIV-positive patients across Europe: Changes over time and risk factors. AIDS, Epidemiol Soc 25: 1505-1513.
- Taarnhøj GA (2011) Incidence, risk factors and mortality of tuberculosis in Danish HIV patients 1995-2007. BMC Pulm Med 11: 26.
- Wood R, Maartens G, Lombard CJ (2000) Risk factors for developing tuberculosis in HIV-1-infected adults from communities with a low or very high incidence of tuberculosis. J AIDS 23: 75-80.
- Colebunders R (2006) Tuberculosis immune reconstitution inflammatory syndrome in countries with limited resources. Int J Tuberc Lung Dis 10: 946-953.
- Egger M, May M, Chêne G (2002) Prognosis of HIV-1-infected patients starting highly active antiretroviral therapy: A collaborative analysis of prospective studies. Lancet 360: 119-129.
- Panel on Antiretroviral Guidelines for Adults and Adolescents (2008) Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents. Department of Health and Human Services.
- Global HIV statistics (2016) Fact sheet, November.
- TB/HIV facts (2015).
- Podlekareva DN, Efsen AMW, Schultze A, Post FA, Skrahina AM, et al. (2016) TB: HIV study group in EuroCoord. Tuberculosis-related mortality in people living with HIV in Europe and Latin America: An international cohort study. Lancet HIV 3: e120-e131.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences