ISSN : 2348-9502
American Journal of Ethnomedicine
The Magic of Herbal Curcumin Therapy in Recurrent Oral Lichen Planus
S.G.T Dental College Gurgaon, Haryana, India
Abstract
Oral lichen planus is a cell-mediated immune condition. It is one of the most common dermatological disease present in the oral cavity. It is mostly found in middle aged and elderly Indian population with a prevalence rate of 2.6%. The purpose of this article is to highlight a case of oral lichen planus affecting a 22- year-old male without concomitant cutaneous lesions who had been treated earlier with topical steroid but repeated recurrence of the lesion made us to shift the treatment from steroid to herbal curcumin which yielded positive results.
Keywords
Oral lichen planus, Curcumin, Herbal therapy.
INTRODUCTION
Oral lichen planus (OLP) is a chronic inflammatory condition characterized by mucosal lesions of varying appearance and severity [3]. It has a global prevalence of about 0.5% to 2%, with prevalence rate of 2.6% in the Indian population [2]. It occurs more commonly in females with ratio of approximately 2:1 [3,4]. It tends to be more persistent and more resistant to treatment [5].
The clinical presentation of OLP ranges from mild painless white keratotic lesions to painful erosions and ulcerations. Oral lichen planus is classified into reticular, erosive, atrophic, and bullous types [6]. The reticular form is the most common type and presents as papules and plaques with interlacing white keratotic lines (Wickham striae) with an erythematous border. The striae are typically located bilaterally on the buccal mucosa, mucobuccal fold, gingiva, and less commonly, the tongue, palate, and lips. The reticular type has been reported to occur significantly more often in men compared to women and is usually asymptomatic [7]. Erosive, atrophic, or bullous type lesions cause burning sensation and pain [8].
The treatment of oral lichen planus is corticosteroids which are widely used and the dosage depends on the severity of the lesion. The frequent use and misuse of currently used therapeutic agents has led to the evolution of resistant strains of common pathogens as well as increased incidence of adverse effects associated with their usage. So the search for the alternative medicinal treatment is still going on. Medicinal plants have been used as a traditional treatment agent for numerous human diseases in many parts of world. In rural areas of developing countries, they continue to be used as the primary source of medicine. About 80% of people in developing countries use traditional medicines for their health care.
CASE REPORT
A 22-year-old male presented with a chief complaint of burning sensation on chewing food on both right and left side of buccal mucosa. The patient reported aggravation of the discomfort and sensitivity in the buccal mucosa on consumption of spicy food and drinks. Local deposits were inconsistent with the corresponding lesion. No cutaneous lesions were visible.
The patient’s past dental, and family histories were found to be not significant. The patient was fit and healthy and was not taking any medication. He was a nonsmoker but had a habit of gutkha chewing with a frequency of 2-3 packets of gutkha per day since 2 years.
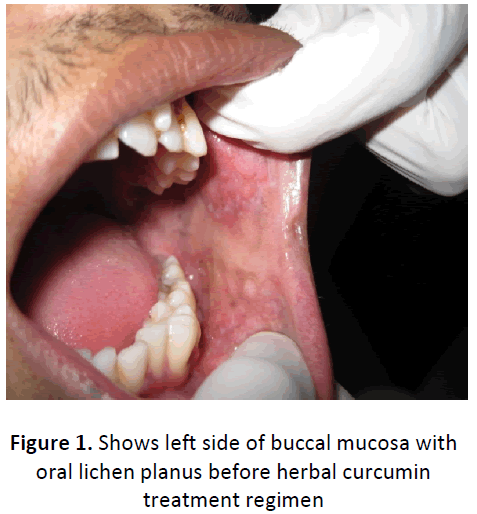
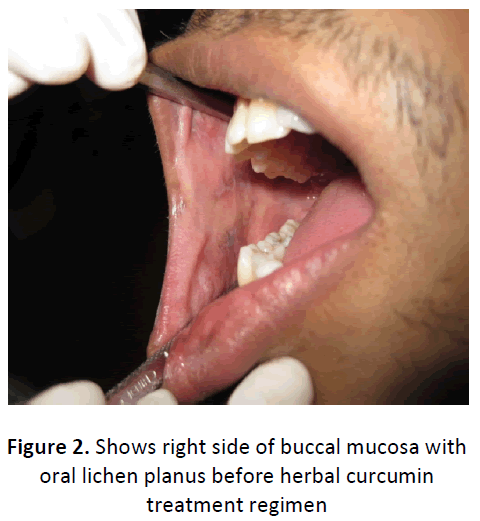
The built and appearance of patient was normal and there was no clinical evidence of lymphadenopathy. On Intra oral examination, no cutaneous lesions were evident other than the interlacing white keratotic lines (known as Wickham’s striae) with an erythematous border. White radiating striae were present on left buccal mucosa in retro commissural area extending from 23-26 region. Similarly, the White radiating striae were present on right buccal mucosa extending from 14-17 region (Figure 1, 2). The striae were non scrappable and did not disappear on stretching. Generalized mild to moderate plaque accumulation and extrinsic stains were present. There were no signs of ulceration.
Routine hematological investigations were done. An incisional biopsy of the lower left posterior buccal mucosa on histopathological examination showed hyperparakeratosis of stratified squamous epithelium and basal cell degeneration. A dense band-like lymphocytic infiltration was found at the epithelial-connective tissue interface and there were areas of atrophic epithelium with saw-tooth rete ridges.
Based on the clinical and histopathological findings, the final diagnosis of reticular oral lichen planus was made.
Treatment was started with a topical steroid kenacort 0.1%. The patient was instructed to apply a thin layer of ointment directly on the lesion three times a day (after meals and at bedtime), and not to take anything orally for one hour after its application, following which he had to rinse with Chlorhexidine (0.2%) mouthwash for a period of one week. Patient was also advised to completely quit the habit of gutkha chewing and to avoid spicy food, along with a healthy diet, rich in fresh fruits and vegetables. He was educated and motivated regarding a proper plaque control regimen. He was kept on follow up and after a week, dose was tapered. The topical steroid was withdrawal after 2 weeks. On evaluation after 2 weeks there was no lesion. At the end of 3 weeks, the patient again reported with similar symptoms of burning sensation on eating spicy food. On examination, there was a presence of white patch on the same area, with Wickham striae, confirming the reoccurrence of the lesion. Hence, the Patient was again started with the same topical steroid kenacort with same dosage for one week and then the dose was tapered for next one week. The patient was recalled after one month of the withdrawal of the topical steroid treatment it was noticed that the lesion reoccur at the same area. So, alternative herbal curcumin therapy was planned to prevent the reoccurrence of the lesion as curcumin is being used in treating oral submucous fibrosis and leukoplakia.
Treatment was started again and aimed primarily at reducing the symptoms of the patient. The therapeutic regimen for the first 4 weeks included herbal medication with systemic administration of curcumin capsules. It is administered with a two divided dosage of 500 mg given twice daily for a period of 4 weeks. The patient was recalled every week to evaluate the response of curcumin on routine follow up.
The patient was advised to completely quit the habit of gutkha chewing and to avoid spicy food, along with a healthy diet rich in fresh fruit and vegetables. The patient was educated and motivated regarding a proper plaque control regimen, which included tooth brushing twice daily with a soft brush and toothpaste. The patient was counseled about the benefits of curcumin and told that many patients responded to curcumin at varying doses of its usage for treating ehite lesions.
On using curcumin at the 1st week recall visit, the patient reported slight decrease in the size of lesion with no symptoms of discomfort to curcumin. At the 2nd week recall visit, further improvement was seen in the regression of lesion. Oral hygiene instructions were reinforced. During the end of 3rd week follow up, the patient was asked to taper the dose with once a day 500 mg curcumin capsule for 2 weeks. After 5th week, patient again came to the department for routine follow up. There were no symptoms of discomfort and no clinical sign of the lesion. No side effect was reported after one month of continuous usage of curcumin. After one month, the dose was further taper to 250mg of curcumin for the next two weeks. Then local application of curcumin paste was started for one month. The treatment was withdrawal and patient was kept on follow up for 3 months. On subsequent follow up for 3 months on both the sides of buccal mucosa no evidence of lesion was seen (Figure 3, 4) and patient didn’t show any sign of discomfort.
DISCUSSION
Lichen planus was first described in the literature by Eramus Wilson in 1869 [9]. The exact etiology of oral lichen planus is not well understood. However, oral lichen planus occurrence is related to a T-cell mediated immune response. Activation of the inflammatory mediator nuclear factor kappa B [10] and the inhibition of the transforming growth factor control pathway may result in hyper-proliferation of keratinocytes, thereby causing the white lesions in oral lichen planus [11]. No known cure exists for oral lichen planus. Treatment modalities in oral lichen planus are still empirical. In general, asymptomatic reticular and plaque form doesn’t warrant any pharmacological intervention. There is no single recommended therapy but Corticosteroids remain the mainstay of oral lichen planus therapy because of their activity in dampening cell-mediated immune activity, and they can be administered topically, intralesionally, or systemically. Topical corticosteroids (in order of decreasing potency) such as 0.05% betamethasone valerate gel, 0.05% fluocinonide gel, and 0.1% triamcinolone acetonide can be used along with Capsule Lycostar contains a combination of lycopene, vitamin E, and retinoids which reduces the hyperkeratosis of oral mucosa. But they have a disadvantage that prolong use of topical steroids for a period of greater than two weeks continuous use may results in mucosal atrophy and secondary candidiasis, and may increase the potential of systemic absorption [12].
Regardless of clinical type, lesions of oral lichen planus undergo periods of exacerbation and quiescence [12]. Reported that the relapse was seen on discontinuation of steroid therapy. The present case, initially did observe relapse of oral lichen planus to corticosteroid therapy. Hence the authors planned to start and observe the response of the patient to curcumin. Though very little scientific information is present on the benefit of using curcumin, the authors planned to observe the response of the patient.
In this case report, a patient with reticular oral lichen planus was treated with both topical steroids followed by herbal curcumin therapy. Curcumin is a polyphenol derived from curcuma longa plant, commonly known as turmeric. The components of turmeric are named curcuminoids, which include mainly curcumin (diferuloyl methane), demethoxycurcumin, and bisdemethoxy-curcumin. It has been used extensively in ayurvedic medicine for centuries, as it is nontoxic and has variety of therapeutic properties including antioxidant, analgesic, antiinflammatory, antiseptic activity and anticarcinogenic activity. The anti-carcinogenic effects of curcumin are due to direct antioxidant and free radical scavenging effects and their ability to indirectly increase glutathione levels, thereby aiding in hepatic detoxification of mutagens and carcinogens. Curcumin has been shown to suppress transformation, proliferation, and metastasis of tumors. These effects are mediated through its regulation of various transcription factors, growth factors, inflammatory cytokines, protein kinases, and other enzymes. It also inhibits proliferation of cancer cells by arresting them in various phases of the cell cycle and by inducing Apoptosis [13]. Research over the last few decades has shown that curcumin is a potent anti-inflammatory agent with strong therapeutic potential against a variety of cancers.
In this case, we found that the oral lichen planus responded well to curcumin. As the dose was initially started at 1gm for 2 weeks, and then tapered to 500 mg for next 2 weeks. Further it was tapered to 250 mg for 2 weeks and followed by 1 month of local application. The follow up after 3 month on last use of curcumin observed significant benefit, with no change in the appearance of normal mucousa. The recurrence of the lesion was absent in this case when the alternative herbal curcumin was chosen as a choice of treatment. Also, curcumin has advantage over the corticosteroids as steroids can cause mucosal atrophy and candidiasis if used repeatedly. Its continuous usage makes the body resistant and there are chances of recurrence of lesion.
CONCLUSION
The curcumin is found to be an effective treatment in oral lichen planus even in the cases where topical steroids have been used and recurrence was seen. It was found to be a good herbal alternative to steroids. Further investigations and clinical trials have been going on curcumin use in various pre cancerous lesions and conditions.
REFERENCES
- Setterfield JF, Black MM, Challacombe SJ. The management of oral lichen planus. Clin Exp Dermatol. 2000; 25:176-182.
- Murti PR, Daftary DK, Bhonsle RB, et al. Malignant potential of oral lichen planus: observations in 722 patients from India. J Oral Pathol. 1986; 15(2):71-77.
- Vincent SD, Fotos PG, Baker KA, Williams TP. Oral lichen planus: the clinical, and therapeutic features of 100 cases. Oral Surg Oral Med Oral Pathol. 1990; 70(2):165- 171.
- Scully C, Beyli M, Ferreiro MC, et al. Update on oral lichen planus: etiopathogenesis and management. Crit Rev Oral Biol Med. 1998; 9(1):86-122.
- Mollaoglu N. Oral lichen planus: a review. Brit J Oral Maxillofacial Surg 2000; 38(4):370-7.
- Laiejendecker R, Van Joost T, Tank B, Oranje AP, Neumann AP. Oral lichen planus in childhood. Pediatr Dematol 2005; 22:299-304.
- Greenberg MS, Glick M, eds. Burket’s Oral Medicine. 10th ed. Hamilton: BC Decker Inc. 2003:89-95.
- Edwards, Kelsch R: Oral Lichen Planus: Clinical Presentation and Management: J Can Dent Assoc 2002; 68(8):494-9.
- Scully C, El-com M: Lichen planus: Review and update on pathogenesis. Journal of oral pathology 1985; 14:431-58.
- Santoro A, Majorana A, Bardellini E, Festa S, Sapelli P, Facchetti F. NF- KappaB expression in oral and cutaneous lichen planus. J Pathol 2003; 201:466-72.
- Kartsaidis A, Schreurs O, Axell T, Helgeland K, Schenck K. Inhibition of transforming growth factor- beta/smad signaling pathway in the epithelium of oral lichen. J Invest Dermatol 2003; 121:1283- 90.
- Usatine R.P, Tinitigan M. Diagnosis and Treatment of Lichen Planus. Am Fam Physician 2011; 84(1):53-60.
- Jurenka JS. Anti-inflammatory Properties of Curcumin, a Major Constituent of Curcuma longa: A Review of Preclinical and Clinical Research. Altern Med Rev 2009; 14(2):141- 153.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences