The Branching Pattern and Intraneural Distribution of the Musculocutaneous Nerve
Yehia Elgammal, Andrey Frolov, Yun Tan and John R. Martin*
Center for Anatomical Science and Education, Department of Surgery, Saint Louis University School of Medicine, 1402 S. Grand Blvd., Schwitalla Hall M-306, St. Louis, Missouri, 63104, USA
- *Corresponding Author:
- John R. Martin
Center for Anatomical Science and Education,
Department of Surgery,
Saint Louis University School of Medicine,
1402 S. Grand Blvd, Schwitalla Hall M-306, St. Louis, Missouri, 63104,
USA
Tel: 314-977-8037
E-mail: john.martin@health.slu.edu
Received: August 06, 2021; Accepted: August 20, 2021; Published: August 27, 2021
Citation: Elgammal Y, Frolov A, Tan Y, Martin JR (2021) The Branching Pattern and Intraneural Distribution of the Musculocutaneous Nerve. J Anat Sci Res vol.4: 002.
Abstract
Objective: The purpose of this study was to gain additional insights into the musculocutaneous nerve (MCN) branching pattern and its intraneural distribution that should improve the outcome of surgical treatments of elbow flexor spasticity (EFS) and MCN injury.
Methods: The study was performed on 20 human cadaveric arms. The distance from the coracoid process to the exit points of the MCN motor branches was measured and expressed as a percentage of the arm length. The intraneural distribution of each fasciculus was identified at proximal, middle, and distal levels following blunt intraneural dissection from the respective branch termination to the lateral cord.
Results: The MCN branches to the coracobrachialis, biceps, and brachialis muscles arise respectively at approximately 17%, 45%, and 60% of the distance between the coracoid process and the medial epicondyle. Intraneural dissection revealed that sensory fascicles occupied the medial segment of the MCN at the proximal level and the lateral segment at the distal level. In contrast, motor fascicles occupied the anterolateral, lateral, and posterior segments of the MCN at the proximal level and the medial segment at the distal level.
Conclusion: Based on the current data, the lateral half of the proximal and middle levels and the medial half of the distal level of the MCN would be the preferred sites for motor nerve transfer thereby improving chances for positive outcomes of the surgical techniques for EFS and MCN injury treatments.
Keywords
Conclusion: Based on the current data, the lateral half of the proximal and middle levels and the medial half of the distal level of the MCN would be the preferred sites for motor nerve transfer thereby improving chances for positive outcomes of the surgical techniques for EFS and MCN injury treatments.
Introduction
Effective treatments for EFS and MCN injury require a thorough knowledge of the MCN anatomy. EFS is the most common manifestation of upper limb spasticity and is mediated by contracture of the biceps brachii and brachialis muscles, which are supplied by the MCN [1]. Microsurgical selective neurectomy, formerly termed hyponeurotization, has proven to be an effective surgical technique [2]. This procedure entails dissection of the MCN motor branches at their entrance into the muscle and resection of a portion of the terminal branches. It is currently recommended that a partial neurectomy must include the sectioning of 50–80% of all branches to a targeted muscle for it to be effective [3]. Therefore, the correct knowledge of the branching pattern and the number of secondary and terminal motor branches of the MCN are required for proper planning and execution of selective neurectomy.
Injuries to the MCN, either due to direct trauma to the nerve or the upper roots of the brachial plexus, result in upper limb flexor paralysis [4]. The function of a damaged MCN can be restored by neurotization or nerve transfer, which involves suturing a grafted nerve, commonly an intercostal nerve, to the distal end of the MCN or one of its motor branches [5]. Nerve grafting is an alternative treatment option where an autologous nerve, typically the sural nerve, connects the trunks of the plexus to the MCN [6]. Success of the aforementioned surgical techniques depends on accurate fascicular matching by connecting related fascicles proximally and distally. The intraneural distribution of the MCN, a detailed mapping of the fascicles inside the nerve at different levels, could improve the results of MCN grafting or neurotization by anastomosing the correct fascicles and precluding axonal misrouting.
Previous studies have primarily focused on determining the number of primary motor trunks as well as the characterization of their exit points from the MCN rather than the number of terminal branches of each motor nerve [7,8]. However, the intraneural distribution of the MCN has not been adequately addressed. Given the importance of a thorough knowledge of the MCN anatomy in successful surgical treatment of EFS and MCN injury, the current study was aimed to gain additional insights into the MCN branching pattern focusing primarily on its relation to the coracobrachialis, biceps brachii and brachialis muscles. The other important aspect of the study was addressing in depth the MCN intraneural distribution.
Materials and Methods
The study was performed on 20 arms (12 left and 8 right) procured from 15 human cadavers (4 males and 11 females). The cadavers were received through Saint Louis University (SLU) School of Medicine Gift Body Program from individuals who had given their written informed consent. The arms were cut from the midpoint of the clavicle to include the scapula and the shoulder joint. Nineteen arms were preserved with a mixture of ethylene glycol and isopropyl alcohol and one arm was un-embalmed. In each specimen, the arm length was measured from the coracoid process to the medial epicondyle. The MCN was exposed through an incision along the deltopectoral groove extended along the medial side of the arm to the cubital fossa. The pectoralis major and minor were cut and reflected.
Dissections were performed from proximal to distal using a 3.5 x loupe magnification. The origin of the MCN from the lateral cord was identified and the nerve was followed distally through the coracobrachialis until its termination as the lateral cutaneous nerve of the forearm. Branches of the MCN to the coracobrachialis, biceps and brachialis were identified and the number of primary, secondary, and terminal branches to each muscle were recorded. The distance from the coracoid process to the exit point of the first motor branch of the MCN to each muscle was then measured and expressed as a percentage of the distance from the coracoid process to the medial epicondyle to account for a variation in the arm’s length.
To assess the MCN intraneural distribution, each branch was followed proximally using intraneural dissection, excising the outer nerve sheath and dissecting the nerve branch proximally, until the origin of the MCN was reached. Photographs were taken using a Canon EOS Digital Rebel XT camera and diagrams of the branching pattern of all the specimens were constructed. The relative positions of the fascicles were plotted on cross section diagrams of the MCN. For descriptive purposes, the cross-section diagram was divided into 8 equal segments: anterior, posterior, lateral, medial, anterolateral, anteromedial, posterolateral and posteromedial. The intraneural distribution of the MCN was described at three levels: proximally, at its origin from the lateral cord, in the middle, after the emergence of the branch to coracobrachialis, and distally after the emergence of the branches to biceps muscle.
Results
The arm length of the specimens studied averaged 29.7+2.64 cm, and ranged from 26 to 36 cm. In 19 specimens (95%) the MCN pierced through the coracobrachialis muscle (CBM) and then descended between the biceps and brachialis muscles. It then travelled distally along the lateral border of the biceps brachii as the lateral cutaneous nerve of the forearm (LCNF). The average distance from the coracoid process to the emergence of the first motor branches of the MCN and the percent of the specimens that have one, two or three motor trunks to each muscle are shown in Table 1.
| Muscle | Average distance from coracoid process to exit of first motor branch | Number of motor trunks and % of specimens | Notes | |||
|---|---|---|---|---|---|---|
| Measurement (cm) | % of arm length | One | Two | Three | ||
| CBM | 4.94+1.67§ | 16.72+6.25 | 40% | 35% | 5% | -CBM was supplied solely by two branches from the lateral cord in one specimen (5%), and in another specimen (5%), the MCN did not perforate the CBM and no branches were observed arising from the primary trunk. - CBM was supplied by an additional branch from the lateral cord in 6 specimens (30%), and from the median nerve in one (5%). |
| BB | 13.20+2.35 | 44.4+7.06 | 17 (85%) | 3 (15%)* | 0% | - An average of 3.3 secondary and 5.5 terminal branches supplied the biceps. |
| BR | 17.52+1.85 | 59.1+6.1 | 100% | 0% | 0% | - An average of 2.6 secondary and 3.8 terminal branches supplied the brachialis. |
*In two specimens, the proximal branch innervated the short head and the distal branch innervated the long head of the biceps brachii muscle. The average distance between them was 2.5 cm. In the remaining specimen, one branch bifurcated into two secondary branches to individually innervate both heads of the biceps, and an additional branch innervated the common belly. CBM= coracobrachialis muscle, BB= Biceps brachii muscle, BR= Brachialis muscle. §Values are mean ± SD.
Table 1: Technical error for the measured parameters of femur using bones and radiographs parameters.
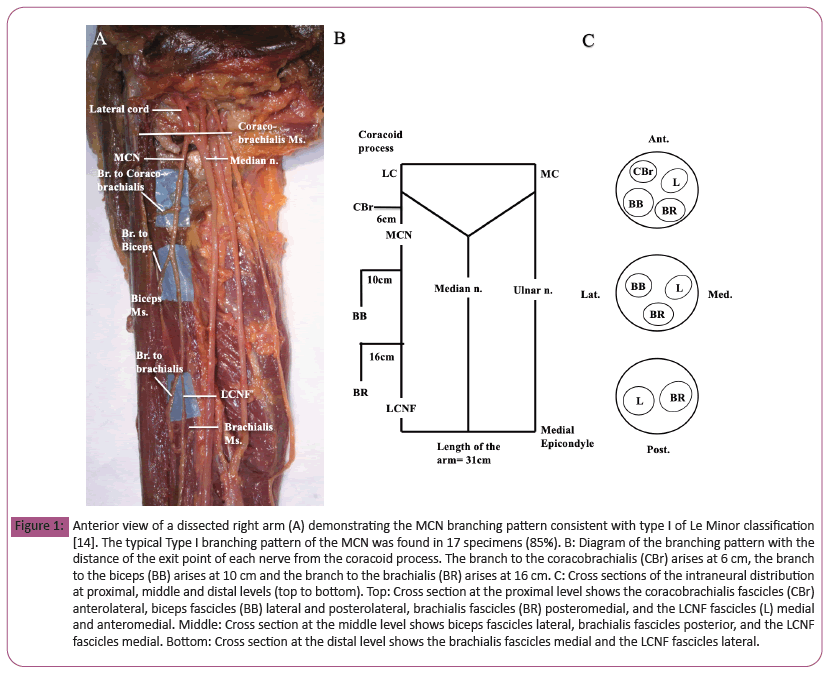
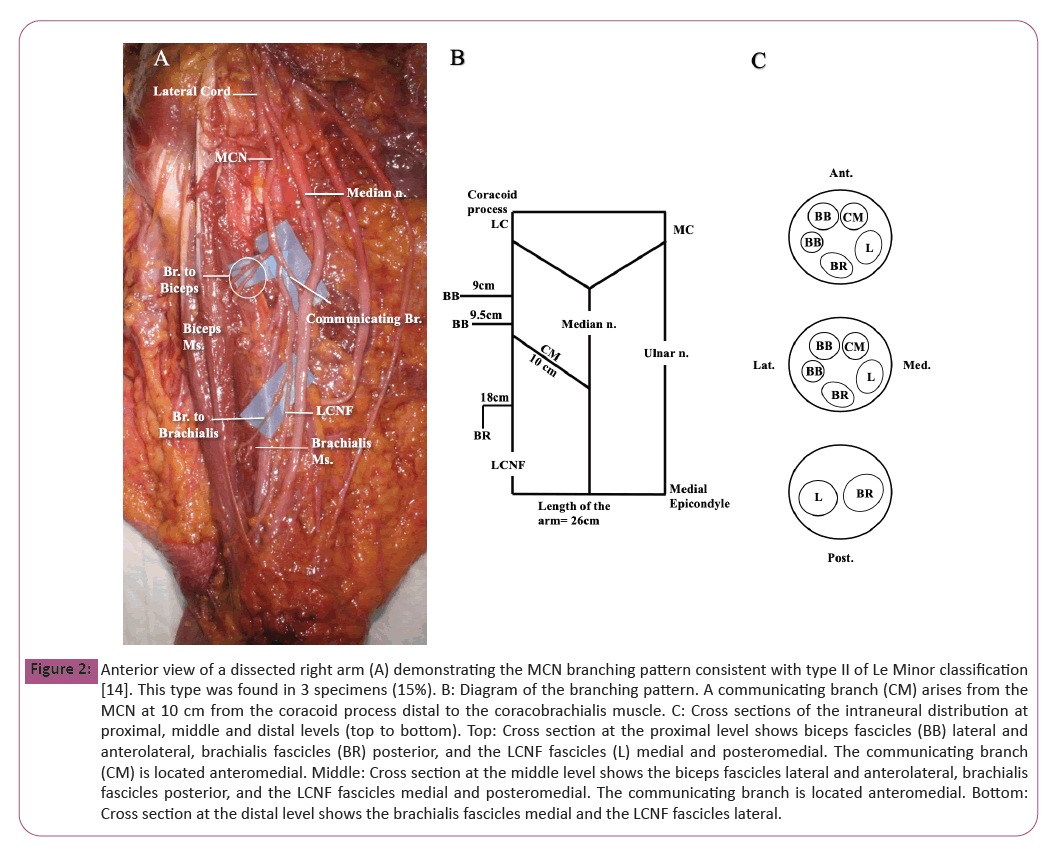
A communicating branch between the MCN and median nerve (MN) was found in 3 specimens (15%). The communicating branch was located distal to the point of entry into the CBM and at an average distance of 11.6 cm from the coracoid process (39% of the arm length). In the majority of specimens, the coracobrachialis fascicles were located in the anterior and anterolateral segments at the proximal level; the biceps fascicles were located mainly in the lateral and posterolateral segments at the proximal and middle levels; the brachialis fascicles were located mainly in the posterior and posteromedial segments at the proximal and middle levels, and the LCNF fascicles were located mainly in the medial and anteromedial segments at the proximal and middle levels of the MCN. Distally, after the MCN gives off the branches to the biceps brachii muscle, the brachialis fascicles were located in the medial and posteromedial segments and the LCNF fascicles were located in the lateral and posterolateral segments. The fascicular distribution of the MCN at each level is demonstrated in Table 2 as well as the (Figures 1 and 2).
| Location Level | Anterior | Antero- lateral |
Lateral | Postero- lateral |
Posterior | Postero- medial |
Medial | Anetro- medial |
|---|---|---|---|---|---|---|---|---|
| Proximal | CBM*35% BB 20% |
CBM*40% | BB 45% BR 10% |
BB 35% BR 5% |
BR 40% | BR 45% LCNF 5% |
LCNF 70% | CBM* 5% LCNF 25% |
| Middle | BB 20% LCNF 20% |
BB 10% | BB 35% | BB 35% BR 15% |
BR 40% | BR 45% LCNF 20% |
LCNF 20% | LCNF 40% |
| Distal | - | LCNF 5% | LCNF 80% | LCNF 15% | - | BR 5% | BR 95% | - |
*CBM fascicles were not found in the MCN in 20% of specimens. CBM=coracobrachialis muscle, BB=Biceps brachii muscle, BR=Brachialis muscle.
Table 2: Percentage of fascicular distribution of the MCN motor and sensory branches at the proximal, middle, and distal levels.
Figure 1: Anterior view of a dissected right arm (A) demonstrating the MCN branching pattern consistent with type I of Le Minor classification [14]. The typical Type I branching pattern of the MCN was found in 17 specimens (85%). B: Diagram of the branching pattern with the distance of the exit point of each nerve from the coracoid process. The branch to the coracobrachialis (CBr) arises at 6 cm, the branch to the biceps (BB) arises at 10 cm and the branch to the brachialis (BR) arises at 16 cm. C: Cross sections of the intraneural distribution at proximal, middle and distal levels (top to bottom). Top: Cross section at the proximal level shows the coracobrachialis fascicles (CBr) anterolateral, biceps fascicles (BB) lateral and posterolateral, brachialis fascicles (BR) posteromedial, and the LCNF fascicles (L) medial and anteromedial. Middle: Cross section at the middle level shows biceps fascicles lateral, brachialis fascicles posterior, and the LCNF fascicles medial. Bottom: Cross section at the distal level shows the brachialis fascicles medial and the LCNF fascicles lateral.
Figure 2: Anterior view of a dissected right arm (A) demonstrating the MCN branching pattern consistent with type II of Le Minor classification [14]. This type was found in 3 specimens (15%). B: Diagram of the branching pattern. A communicating branch (CM) arises from the MCN at 10 cm from the coracoid process distal to the coracobrachialis muscle. C: Cross sections of the intraneural distribution at proximal, middle and distal levels (top to bottom). Top: Cross section at the proximal level shows biceps fascicles (BB) lateral and anterolateral, brachialis fascicles (BR) posterior, and the LCNF fascicles (L) medial and posteromedial. The communicating branch (CM) is located anteromedial. Middle: Cross section at the middle level shows the biceps fascicles lateral and anterolateral, brachialis fascicles posterior, and the LCNF fascicles medial and posteromedial. The communicating branch is located anteromedial. Bottom: Cross section at the distal level shows the brachialis fascicles medial and the LCNF fascicles lateral.
Discussion
In its classical description, the MCN pierces the CBM to descend along the biceps and brachialis muscles, and then continues along the forearm as the LCNF. In the current study, one specimen (5%) was identified where the MCN did not pass through the CBM but rather was located medial to it. Similar cases of the MCN not penetrating the CBM have been previously reported with an incidence ranging from 6 to 17% [9-11]. The MCN is usually the sole nerve supply to CBM, but it has been reported previously that a branch from the lateral cord, lateral root of the MN or MN may supply the CBM [11-14]. In the current study, it was found in one specimen (5%) that the CBM was supplied solely by two branches from the lateral cord. Additionally, in 6 specimens (30%), the CBM was supplied by the MCN and an additional branch from the lateral cord.
In previous studies, different reference points were used to determine the location of the motor branches to the elbow flexor muscles, which makes comparison of the respective data difficult [7,8]. In the present study, the point of origin of each nerve was measured from the coracoid process and was expressed as a percentage of the arm length measured between the coracoid process and the medial epicondyle. The results of the current study are, in general, in agreement with the MCN branching patterns described in [7] where the similar measurement method was used. Therefore, the most proximal motor branch to the coracobrachialis, and biceps muscles emerged from the MCN at an average of 4.94+1.67 cm (16.72%+6.2 of arm length) and 13.2+2.35 cm (44.4%+7.06 of arm length) from the coracoid process, respectively. The brachialis was exclusively supplied by a single branch arising from the MCN that emerged at an average distance of 17.52+1.85 cm from the coracoid process (59.1%+6.1 of arm length). Hence, based on these data, it is recommended that in the EFS related surgical procedures, an incision between 17% and 60% of the arm length would be necessary to fully expose the MCN branches.
The terminal branching pattern of each motor nerve to the biceps and brachialis muscles has not been adequately addressed in the literature despite such knowledge is important for surgeons performing selective partial neurectomy for EFS treatment [15].
There is a common agreement in the field that a partial neurectomy must include the sectioning of 50–80% of all branches to a targeted muscle for it to be effective [3]. Only one study [15] reported an average number of terminal branches of 7.9 and 6.5 dedicated to the biceps and the brachialis muscles, respectively. In the present study, the number of terminal branches to the biceps brachii and brachialis muscles were found to be significantly lower with an average of 3.3 secondary and 5.5 terminal branches supplying the biceps and an average of 2.6 secondary and 3.8 terminal branches supplying the brachialis. One possible explanation for this discrepancy is the previously mentioned study might have included the number of the secondary branches in addition to the terminal branches.
Variations in the MCN anatomy have been reported in several publications [14,16-19]. For instance, in the report from Le Minor [14], the MCN variations were divided into five types. Using that approach in the present study, type I, the most typical branching pattern, was found in 17 specimens (85%). Type II, representing one communicating branch between the MCN and MN, was found in 3 specimens (15%) arising at an average distance of 11.6 cm from the coracoid process (39% of arm length) and distal to the point of entry into the CBM. Types III, IV, and V were not found in the current study. The communicating branches were reported to be present in 8% to 53.6% of specimens and have been grouped into various categories [16,19-26]. Based on Venieratos classification [19], all of the communicating branches in the present study were classified as type II, where the communicating branch was distal to the point of MCN entry into the CBM. Also, all the communicating branches were directed from the MCN proximally to the MN distally, which is consistent with the findings of Guttenberg and Ingolotti [16].
There is also a paucity of the data in the literature describing the MCN intraneural distribution [27-29]. One such report [27] examined the MCN topography by using histochemical staining where it was found that the fascicles of the branches to the biceps, brachialis, and LCNF were constantly located from lateral to medial at proximal and distal levels. In the present study, to better ascertain the MCN intraneural distribution, each branch was followed proximally using intraneural dissection until the origin of the MCN was reached to identify the relative position of the fascicular groups at three different levels: proximal, middle, and distal. It was concluded thereafter that the lateral half of the MCN proximally, and the medial half of the MCN distally, would be the preferred sites for any motor nerve transfer. Such a conclusion could be viewed as the most accurate because it was based on the largest number of specimens studied so far. Using such knowledge to modify the existing surgical techniques of the MCN neurotization with a mixed nerve, such as the intercostal nerve, may improve the respective outcome.
Conclusion
The MCN branches to the coracobrachialis, biceps, and brachialis muscles arise respectively at a distance from the coracoid process that respectively corresponds to approximately 17%, 45%, and 60% of the distance between the coracoid process and the medial epicondyle. Additionally, using twenty specimens, we have confirmed that while the sensory fascicles are located laterally and the brachialis fascicles are located medially at the distal level, the sensory fascicles are located medially and the fascicles to the coracobrachialis, biceps, and brachialis are located laterally at the proximal level. Based on the data obtained, the lateral half of the proximal and middle levels and the medial half of the distal level of MCN are the preferred sites for any motor nerve transfer. The reported findings could be important for the development of more efficient microsurgical procedures for EFS treatment as well as for MCN neurotization.
Declarations
Not applicable
Funding
This study was supported by the Center for Anatomical Science and Education, SLU School of Medicine.
Conflict of Interests
None declared.
Data Availability
The datasets and materials used and/or analyzed during the current study are presented in the main paper and additional files.
Acknowledgements
We gratefully acknowledge Michael Ackermann, Vickie Grapperhaus, and John Luther for preparing and providing the cadaver specimens that were used in this study.
Disclosure
These data were presented in part at the Annual Experimental Biology Meeting (FASEB J. (2020), 34: Suppl.1, Abstract 04481).
References
- Purohit AK, Raju BS, Kumar KS, Mallikarjun KD (1998) Selective musculocutaneous fasciculotomy for spastic elbow in cerebral palsy: a preliminary study. Acta Neurochir (Wien) 140(5): 473-478.
- Brunelli G, Brunelli F (1983) Partial selective denervation in spastic palsies (hyponeurotization). Microsurgery 4(4): 221-224.
- Sindou MP, Simon F, Mertens P, Decq P (2007) Selective peripheral neurotomy (SPN) for spasticity in childhood. Childs Nerv Syst 23(9): 957-970.
- Desai S, Varacallo M (2019) Anatomy, Shoulder and upper limb, arm nerves – statpearls. Treasure Island (FL).
- Narakas AO, Hentz VR (1988) Neurotization in brachial plexus injuries. Indication and results. Clin Orthop Relat Res (237): 43-56.
- Millesi H (1988) Brachial plexus injuries. Nerve grafting. Clin Orthop Relat Res (237): 36-42.
- Lee JH, Kim HW, Im S, An X, Lee MS, et al. (2010) Localization of motor entry points and terminal intramuscular nerve endings of the musculocutaneous nerve to biceps and brachialis muscles. Surg Radiol Anat 32(3): 213-220.
- Vicente PD, Calvet PF, Burgaya AC, Perez ML (2005) Innervation of biceps brachii and brachialis: Anatomical and surgical approach. Clin Anat 18(3): 186-194.
- Gumusalan Y, Yazar F, Ozan H (1998) Variant innervation of the coracobrachialis muscle and unusual course of the musculocutaneous nerve in man. Kaibogaku Zasshi 73(3): 269-272.
- Koizumi M (1989) [A morphological study on the coracobrachialis muscle]. Kaibogaku Zasshi 64(1) :18–35.
- Nakatani T, Tanaka S, Mizukami S (1997) Absence of the musculocutaneous nerve with innervation of coracobrachialis, biceps brachii, brachialis and the lateral border of the forearm by branches from the lateral cord of the brachial plexus. J Anat 191 ( Pt 3): 459-460.
- Beheiry E (2004) Anatomical variations of the median nerve distribution and communication in the arm. Folia Morphol (Warsz) 63(3): 313-318.
- Gumusburun E, Adiguzel E (2000) A variation of the brachial plexus characterized by the absence of the musculocutaneous nerve: a case report. Surg Radiol Anat 22(1): 63-65.
- Le Minor, JM (1990) [A rare variation of the median and musculocutaneous nerves in man]. Arch Anat Histol Embryol 73: 33-42.
- Cambon-Binder A, Leclercq C (2015) Anatomical study of the musculocutaneous nerve branching pattern: application for selective neurectomy in the treatment of elbow flexors spasticity. Surg Radiol Anat 37(4): 341-348.
- Guerri-Guttenberg RA, Ingolotti M (2009). Classifying musculocutaneous nerve variations. Clin Anat 22(6): 671-683.
- Hayashi M, Shionoya K, Hayashi S, Hatayama N, Kawata S, et al. (2017) A novel classification of musculocutaneous nerve variations: The relationship between the communicating branch and transposed innervation of the brachial flexors to the median nerve. Ann Anat 209: 45-50.
- Sirico F, Castaldo C, Baioccato V, Marino V, Zappia M, et al. (2019) Prevalence of musculocutaneous nerve variations: Systematic review and meta-analysis. Clin Anat 32(2): 183-195.
- Venieratos D, Anagnostopoulou S (1998) Classification of communications between the musculocutaneous and median nerves. Clin Anat 11(5): 327-331.
- Chitra R (2007). Various types of intercommunications between musculocutaneous and median nerves. An analytical study. Ann Indian Acad Neurol 10(2):100–104.
- Choi D, Rodriguez-Niedenfuhr M, Vazquez T, Parkin I, Sanudo JR (2002) Patterns of connections between the musculocutaneous and median nerves in the axilla and arm. Clin Anat 15(1): 11-17.
- Eglseder WA, Goldman M (1997) Anatomic variations of the musculocutaneous nerve in the arm. Am J Orthop (Belle Mead NJ) 26(11): 777-780.
- Krishnamurthy, A, Nayak SR, Venkatraya Prabhu L, Hegde RP, Surendran S, et al. (2007) The branching pattern and communications of the musculocutaneous nerve. J Hand Surg Eur 32(5): 560-562.
- Kwolczak-McGrath A, Kolesnik A, Ciszek B (2008) Anatomy of branches of the musculocutaneous nerve to the biceps and brachialis in human fetuses. Clin Anat 21(2): 142-146.
- Prasada Rao PV, Chaudhary SC (2000) Communication of the musculocutaneous nerve with the median nerve. East Afr Med J 77(9): 498-503.
- Uysal II, Karabulut AK, Buyukmumcu M, Unver Dogan N, Salbacak A (2009) The course and variations of the branches of the musculocutaneous nerve in human fetuses. Clin Anat 22(3): 337-345.
- Chiarapattanakom P, Leechavengvongs S, Witoonchart K, Uerpairojkit C, Thuvasethakul P (1998) Anatomy and internal topography of the musculocutaneous nerve: the nerves to the biceps and brachialis muscle. J Hand Surg Am 23(2): 250-255.
- Sunderland S, Marshall RD, Swaney WE (1959) The intraneural topography of the circumflex, musculocutaneous and obturator nerves. Brain 82(1): 116-129.
- Macchi V, Tiengo C, Porzionato A, Parenti A, Stecco C, et al. (2007) Musculocutaneous nerve: histotopographic study and clinical implications. Clin Anat 20(4): 400-406.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences