Spinal Cord Occupation Ratio (Scor) and its Application in the Diagnosis of Cervical Spinal Cord Compression in Mucopolysaccharidoses
Julia Almeida*
Department of Department of Medicine, University of Salamanca, Salamanca, Brazil
- *Corresponding Author:
- Julia Almeida
Department of Department of Medicine, University of Salamanca, Salamanca, Brazil
Tel: 5521999780171
E-mail: julia.almeida@unirio.br
Received Date: December 10, 2021; Accepted Date: December 24, 2021; Published Date: December 31, 2021
Citation: Almeida J (2021) Spinal Cord Occupation Ratio (Scor) and its Application in the Diagnosis of Cervical Spinal Cord Compression in Mucopolysaccharidoses. J Mol Genet Med Vol:5 No:1.
Abstract
Introduction
Mucopolysaccharidoses (MPS) can lead to cervical Spinal Cord Compression (SCC). Diagnostic scores for SCC in MPS use the obliteration of the passage of cerebrospinal fluid in the anterior and posterior spinal cord in the sagittal section of Magnetic Resonance Imaging (MRI). The Spinal Cord Occupation Ratio (SCOR) published, by Nouri et al (2018), establishes the spinal cord filling index for the spinal cord, identifying disproportionate spinal cord occupation in the canal. When evaluating congenital canal stenosis, the risk of spinal cord injury has been considered increased when the SCOR is ≥ 70% in the median sagittal plane or ≥ 80% in the axial plane. Although these values have not been validated for MPS populations, they could be useful.
Objective
To verify the SCOR in MPS patients with diagnosis of cervical SCC comparing the SCOR with other markers proposed in the existing MPS SCC scores, such as the extent of gliosis, clinical impact and the SCC assessment as represented by the obliteration of CSF flow.
Methods
We reviewed imaging tests of the cervical spine from MPS patients with previously confirmed SCC, using the SCOR measure in the median sagittal plane, evaluation of the presence and extent of spinal gliosis on MRI, evaluation of the clinical impact using a clinical score and evaluation of the images for the obliteration of Cerebral Spinal Fluid (CSF) flow.
Results
Thirty-one MRI of 24 different patients were included. The average SCOR was 87.1%. This was lower (81.6%) in patients without gliosis, when compared to those with focal (90.5%) and extensive (97%) gliosis. The only patient with gliosis associated with a lacunar lesion, resulting from an acute compressive injury, had a 68% SCOR, due to the atrophic spinal cord injury. As expected, SCOR was higher in patients with total or partial CSF obliteration, but one among the 3 patients without CSF flow obliteration, with a 76% SCOR, had already developed focal gliosis and mild clinical abnormalities. Patients with more extensive gliosis had higher clinical scores. Four patients had more than one imaging scan evaluated. SCOR upward trend showed an annual average increase of 3.8%.
Discussion and conclusions
The use of SCOR allows the diagnosis of cervical spinal canal stenosis in an objective way. It is possible that the cut-off values used by Nouri et al in patients with congenital stenosis could be useful to diagnose cervical stenosis in MPS patients, preceding the finding of CSF flow obstruction, presence of gliosis or clinical abnormalities. Furthermore, the use of SCOR may assist in the longitudinal evaluation of disease progression. Better follow-up and timely diagnosis allows for scheduling of surgery at the best clinical moment, minimizing complications.
Keywords
Mucopolysaccharidoses; Glycosaminoglycans; Lysosomal; Platyspondyly; Ligament laxity
Introduction
Mucopolysaccharidoses (MPS) constitute a heterogeneous group of Lysosomal Storage Diseases (LSD), characterized by the dysfunction of one of the enzymes involved in the degradation pathways of glycosaminoglycans (GAG) [1].
Spine disease is especially common in MPS types I-Hurler, IVA, and VI. Few studies have attempted to estimate the incidence of CMC in the MPS subtypes, with incidences ranging from 16 to 75% depending on subtype and treatment modality [2-8]. Spinal involvement is complex and can be extensive. Platyspondyly occurs progressively and with increased load on the vertebrae, whose mineralization process is impaired by the deposition of GAGs, leading to low bone density and progressive deformities [9]. Involvement of the meninges and supporting ligaments are associated with changes in bone and cartilage and, in MPS type IVA, ligament laxity, leading to spinal cord stenosis and compression [10-11].
Even minimal spinal canal stenosis can lead to acute compressions and serious injuries, usually due to exaggerated or abrupt cervical extension and flexion movements (such as the one needed for difficult orotracheal intubation) [12].However, more commonly, accumulated minor injuries from routine movement of head and neck result in axonal injury, demyelination, gliosis and atrophy. Neurological changes resulting from these insults are often irreversible [12-15].
Diagnostic criteria for cervical spinal canal stenosis exist for congenital forms. An absolute antero-posterior diameter of the cervical spinal canal is considered normal when greater than 12-13 mm in adults or when the Torg-Pavlov ratio (ratio between the antero-posterior diameters of the vertebral body and its adjacent vertebral canal) is greater than 0.80. However, the absolute diameter criterion does not apply adequately to patients with MPS, whose vertebral bodies are frequently dysplastic and whose spinal canal diameters are narrower, not exceeding 11 mm in adults, even in the absence of stenosis. The Torg-Pavlov ratio, additionally, having been developed for measurement in plain x-ray films, neither takes into account the soft tissue components inside the canal, like the GAG deposits, nor considers spine diameter in the evaluation [16].
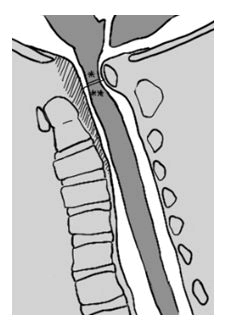
The spinal cord occupation ratio (SCOR), first published by Nouri et al, establishes the spinal canal filling index by the spinal cord (as illustrated in Figure 3), in order to identify a disproportionate occupation of the canal. It was found that, for congenital canal stenoses, the risk of spinal cord injury is increased when the SCOR is ≥ 70% in the median sagittal cut or ≥ 80% in the axial as seen in MRI [17]. Although these values are not validated for MPS populations, the comparison of SCOR of the same patient in different clinical situations can be informative, since it quantifies these findings.
SCC scores in MPS use the obliteration of the passage of CSF in the anterior and posterior columns in the sagittal section of MRI as the earliest radiological indication of canal stenosis [18,19].The measurement of SCOR can help quantify these values. A SCOR of 100% is equivalent to a complete obliteration of the CSF, anterior and posterior to the spinal cord, however, even patients without CSF flow obstruction could already have irreversible spinal injury.
Recent studies show that patients diagnosed and undergoing SCC surgical correction before the appearance of important clinical symptoms have a better long-term prognosis [4]. Therefore, there is a need for better imaging criteria for the diagnosis of SCC in MPS, which do not depend on the existence of severe compressions associated with gliosis and neurological injury.
Materials and Methods
A retrospective longitudinal study was carried out using 31 MRI scans from 24 MPS patients followed at the National Institute of Women, Children and Adolescents´ Health Fernandes Figueira, a tertiary hospital in Rio de Janeiro, Brazil. Patients with cervical SCC suspected or confirmed in imaging exams who had not yet undergone decompressive cervical surgery were included.
The collected patient data included age at diagnosis, age at neurological evaluation and at each cervical spine MRI scan performed and at last follow-up, sex, MPS type and subtype, and use of enzyme replacement therapy or stem cell transplant.
Patients’ scans were subdivided in 4 groups, according to the amount of spinal cord lesion. Group 0 (G0)=no gliosis, group 1 (G1)=focal gliosis, that is, limited <50% the spinal level, group 2 (G2)=extensive gliosis involving more than 50% of the spinal level, and group 3 (G3)=gliosis associated with lacunar lesion (signal similar to CSF in T1 and T2 weighted scans, suggesting sequelar lesion).
Author JVA measured anterior-posterior width measures on mid-sagittal imaging of the spinal canal (that is, the width containing both spinal cord and CSF) and the spinal cord using MRI scans. Measures of each of these widths, in each of the 7 spinal levels, were obtained, twice, and a mean value calculated. SCOR was then calculated, and the highest value in each imaging exam was considered for the purpose of evaluating CSCC, as the point of narrower stenosis.
Additionally, gliosis cranial-caudal extension was measured in the number of spinal levels affected, and the degree of CSF flow obstruction was quantified as “2” when both anterior and posterior CSF columns were obliterated, “1” when only one was obstructed and “0” when there was CSF flow, both anteriorly and posteriorly, in the whole of the cervical spinal cord.
The clinical score used in our hospital, which uses the routine complete neurological exam and converts it into a 0 to 11 score of severity, 0 being the asymptomatic patient, measured clinical severity of patients. Such score considered the presence of pyramidal signs (increased deep-tendon reflexes, decreased strength and the presence of Babinski, Chaddock, Tromner or Hoffman signs), sensitivity abnormalities, bulbar function and sphincter involvement. (Figure 1)
Final measurements obtained were analyzed using means and medians. Data referring to the four subgroups, G0, G1, G2 e G3, was compared using means and confidence intervals (IC95%). When possible, the ANOVA test for independent measures was used for statistical analysis.
Results
Twenty-four patients with MPS types I (n=3), II (n=5), IVA (n=6) or VI (n=10) and SCC were evaluated. Four patients (numbers 1, 12, 19 and 21) had more than one MRI scan, totaling 31 exams evaluated Table 1.
| Age (years) | MPS type | Gliosis subgroup (G0, G1, G2, G3) | Gliosis cranial-caudal extension | Clinical score (0-11) | SCOR (%) | Number of CSF columns obstructed (0-2) | |
|---|---|---|---|---|---|---|---|
| Patient 1 | 7.3 | I | G0 | 0 | NA | 72 | 0 |
| 9.8 | I | G0 | 0 | 2 | 87 | 1 | |
| 11.7 | I | G1 | 1 | 3 | 84 | 1 | |
| 13.7 | I | G2 | 4 | 3 | 100 | 2 | |
| Patient 2 | 0.4 | I | G0 | 0 | 1 | 73 | 1 |
| Patient 3 | 13.9 | I | G1 | 1 | 7 | 100 | 2 |
| Patient 4 | 40.9 | II | G1 | 1 | 1 | 100 | 2 |
| Patient 5 | 16.0 | II | G0 | 0 | 0 | 85 | 1 |
| Patient 6 | 25.2 | II | G1 | 1 | 1 | 89 | 1 |
| Patient 7 | 12.6 | II | G0 | 0 | NA | 78 | 0 |
| Patient 8 | 5.5 | II | G0 | 0 | NA | 75 | 1 |
| Patient 9 | 10.6 | IVA | G1 | 2 | 5 | 81 | 1 |
| Patient 10 | 9.8 | IVA | G3 | 3 | 11 | 68 | 0 |
| Patient 11 | 9.9 | IVA | G1 | 1 | 4 | 86 | NA |
| Patient 12 | 3.9 | IVA | G0 | 0 | NA | 82 | 0 |
| 12.0 | IVA | G0 | 0 | NA | 84 | 1 | |
| 13.4 | IVA | G0 | 0 | NA | 85 | 1 | |
| Patient 13 | 12.9 | IVA | G2 | 2 | 2 | 85 | 1 |
| Patient 14 | 13.2 | IVA | G2 | 2 | NA | 100 | 2 |
| Patient 15 | 2.5 | VI | G0 | 0 | 3 | 73 | 1 |
| Patient 16 | 3.1 | VI | G1 | 1 | 1 | 76 | 0 |
| Patient 17 | 3.4 | VI | G1 | 1 | 0 | 81 | 1 |
| Patient 18 | 5.9 | VI | G2 | 5 | 7 | 100 | 2 |
| Patient 19 | 6.4 | VI | G0 | 0 | 0 | 83 | 1 |
| 9.2 | VI | G1 | 1 | 2 | 89 | 1 | |
| Patient 20 | 10.3 | VI | G1 | 2 | 0 | 100 | 2 |
| Patient 21 | 9.6 | VI | G0 | 0 | 1 | 93 | 1 |
| 10.4 | VI | G1 | 2 | 1 | 100 | 2 | |
| Patient 22 | 1.4 | VI | G2 | 2 | 2 | 100 | 2 |
| Patient 23 | 13.0 | VI | G1 | 2 | 8 | 100 | 2 |
| Patient 24 | 3.9 | VI | G0 | 0 | 0 | 91 | 1 |
| MEAN | 10.4 | 1.1 | 2.6 | 87.1 | 1.1 | ||
| MEDIAN | 9.9 | 1.0 | 1.5 | 85.5 | 1.0 |
CSF=cerebrospinal fluid; G0=no gliosis; G1=focal gliosis, that is, limited <50% the spinal level; G2=extensive gliosis involving more than 50% of the spinal level; G3=gliosis associated with lacunar lesion (signal similar to CSF in T1 and T2 weighted scans, suggesting sequelar lesion); NA=not available; SCOR=spinal cord occupation ratio.
Table 1: Characteristics of patients and scans evaluated.
CSF=cerebrospinal fluid; G0=no gliosis; G1=focal gliosis, that is, limited <50% the spinal level; G2=extensive gliosis involving more than 50% of the spinal level; G3=gliosis associated with lacunar lesion (signal similar to CSF in T1 and T2 weighted scans, suggesting sequelar lesion); NA=not available; SCOR=spinal cord occupation ratio.
Divided according to gliosis extension, six scans were included in G0, 10 in G1, 5 in G2 and a single one in G3.
The average SCOR was 87.1%. This average was lower (81.6%) in patients without gliosis (G0), compared to patients with focal (G1, SCOR 90.5%) and extensive (G2, SCOR 97.0%). The only patient with gliosis associated with a lacuna, resulting from an acute compressive injury, had a 68% SCOR. This low SCOR was in accordance with the atrophic nature of the spinal cord injury, which leads to a much narrower spinal cord, despite the canal stenosis. The difference between groups G0, G1 and G2 was statistically significant (Table 2).
Mean clinical scores were lower in groups with less extensive gliosis (G0=1.3; G1=2.4) and higher in those with extensive lesions (G2=3.5; G3=11), with a gradient effect. Because not all patients had neurological evaluations done at the time of MRI scan, the number of scans with paired clinical scores was reduced and did not allow for a subsequent statistical analysis between G2 and G3. No statistically significant difference was observed between groups G0 e G1. (Table 2)
As should be expected, patients with extensive gliosis in a single spinal level (G2) had a mean cranial-caudal involvement significantly more extensive than those with focal gliosis in a single spinal level (G1), as seen in Table 2.
| G0 | G1 | G2 | G3 | p-value | |
|---|---|---|---|---|---|
| N patients | 6 | 10 | 5 | 1 | |
| N scans | 13 | 12 | 6 | 1 | |
| SCOR (%) | |||||
| N | 13 | 12 | 5 | 1 | |
| Mean | 81,6 | 90,5 | 97,0 | 68,0 | <0.005* |
| CI95% | 72–93 | 76–100 | 85–100 | n/a | |
| Clinical score (0-11) | |||||
| N | 6 | 12 | 4 | 1 | |
| Mean | 0,7 | 2,8 | 3,5 | 11,0 | 0.087 † |
| CI95% | 0–2 | 0–7 | 2–7 | n/a | |
| Gliosis cranial-caudal extension (levels involved) | |||||
| N | 6 | 10 | 5 | 1 | |
| Mean | 0 | 1,3 | 3,0 | 3,0 | < 0.005 ± |
| CI95% | n/a | 1–2 | 2–5 | n/a | |
| Number of CSF columns obstructed (0-2) | |||||
| N | 13 | 11 | 5 | 1 | |
| Mean | 0,9 | 1,4 | 1,8 | 0 | < 0.05* |
| CI95% | 0–2 | 0–2 | 1–2 | n/a |
* P-value obtained in the comparison between groups G0, G1 and G2. Number of patients in G3 did not allow for statistical analysis. † P-value obtained in the comparison between groups G0 and G1. Number of patients in G2 and G3 did not allow for statistical analysis. ± p- value obtained in the comparison between groups G1 and G2. Number of patients in G3 did not allow for statistical analysis. CSF=cerebrospinal fluid; G0=no gliosis; G1=focal gliosis, that is, limited <50% the spinal level; G2=extensive gliosis involving more than 50% of the spinal level; G3=gliosis associated with lacunar lesion (signal similar to CSF in T1 and T2 weighted scans, suggesting sequelar lesion); N/A=not applicable; SCOR=Spinal Cord Occupation Ratio.
Table 2: Comparison between groups according to SCOR, clinical score, gliosis cranial-caudal extension and CSF columns obstruction.
| Score | Clinical finding |
|---|---|
| Strength * | |
| 0 | 5/5 |
| 1 | 4/5 |
| 2 | 3/5 |
| 3 | 2/5 |
| 4 | 1/5 or 0/5 |
| Deep tendon reflexes | |
| 0 | Normal or reduced |
| 1 | Increased |
| 2 | Exalted |
| Babinski, Chaddock, Tromner or Hoffman signs | |
| 0 | Absent |
| 1 | Present |
| Sensitivy examination | |
| 0 | Normal |
| 1 | Altered, in any modality |
| 2 | Abolished, in any modality |
| Bulbar signs or sphincter involvement | |
| 0 | Absent |
| 1 | Either one present |
| 2 | Both present |
| Other causes or possible explanations for the abnormal findings have been excluded, leaving spinal cord compression as the most likely cause | |
*Using the Medical Research Council (MRC) scale
Table 3: Clinical score used in the evaluation of spinal cord compression.
Clinical scores were lower in the groups with SCOR in the 70 to 79 range and 80 to 89 range (1.7 and 1.4 points on average, respectively) than in the group with SCOR in the 90 to 100 range (average of 3.0 points) , with no statistically significant difference between groups. Further comparisons of clinical scores between groups with SCOR in the 70 to 85 range and in the 86 to 100 ranges also did not show any significant difference, as well as the comparison of SCORs of groups with different clinical scores.
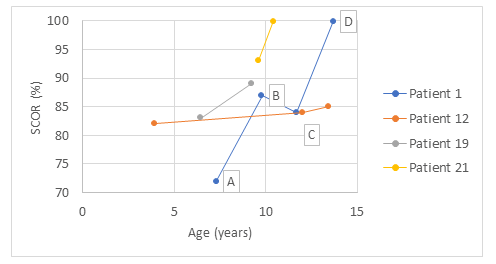
Four patients, with MPS types I (1), IVA (1) and VI (2), had serial imaging exams over the years, prior to being referred to decompressive surgery. In these cases, it was possible to evaluate the temporal evolution of stenosis with serial SCOR measurements. The calculation of the SCOR upward trend showed a linear increase of 3.9%, 0.3%, 2.1% and 8.8% per year, with an annual average increase of 3.8% (Figure 2).
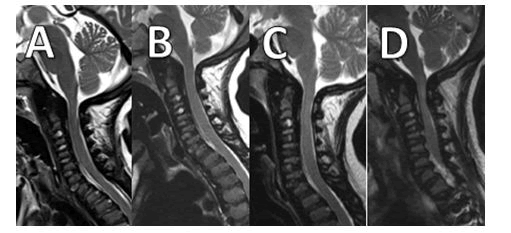
The figure illustrates 4 T2-weighted mid-sagittal magnetic resonance imaging scans of the cervical spine of Patient 1 in diferente ages (A-D), as shown above on the graphic.
The apparent reduction in the SCOR value found between the 2nd and 3rd measurements of Patient 1 can be attributed to small variations resulting from images taken with a greater or lesser degree of cervical extension, as has been demonstrated in other studies [20,21].
Among patients with non-sequelar spinal cord abnormalities (groups G0, G1 and G2), the ones who did not have any obliteration of CSF flow had lower SCOR values (76.7%) than those with partial (83.6%) or complete (100%) obliteration. Only 3 exams out of 29 evaluated regarding CSF flow had no obliteration (10%), anteriorly or posteriorly. This small number limited statistical analysis. It is noteworthy that in one of these three patients (Patient 16), with MPS VI and SCOR of 76%, despite sustained CSF flow, there was focal gliosis (G1) and altered neurological examination (clinical score=1). This patient had been previously submitted to an urgent ventriculo-peritoneal shunt placement, performed after a difficult orotracheal intubation (nasofibroscopy was not available), in which case a traumatic cervical hyperextension could justify the presence of gliosis at the craniocervical junction, as seen in cases described in the literature [22,23].
Discussion
The cranio-cervical junction (CCJ) is the portion most frequently involved in patients with MPS related SCC. This occurs not only due to the characteristic changes of multiple dysostosis in these patients, but also due to the differentiated anatomy and the range of movement of the first two cervical vertebrae. The formation of a dysplastic, hypoplastic and delayed ossification process makes it malleable and flexible. The constant trauma caused by the usual movement of the atlantoaxial joint leads to microfractures, fractures, subluxation or dislocation. The latter reduces the antero-posterior diameter of the spinal canal even more severely [10,15].
The thickening of the cruciate ligament, posterior to the odontoid, of the yellow ligament, anteriorly to the posterior vertebral arches, and of the meninges, which surround the medulla, occurs secondary to the deposition of GAGs in the tissues (exemplified by the hatched area of Figure 3).
The spinal cord occupation ratio is calculated between the width of the spinal cord (*) and the width of the spinal canal comprised of the total width the cord has available for dynamic movement inside the canal (**) in the same level of the spine. In the above illustration, soft tissue thickening (meninges and support ligaments) is represented by the hatched área, and determines a narrowing of the spinal canal, without a narrowing of the bony.
This thickening is frequent and common in the cervical spinal cord, especially in the CCJ, and may even involve the region adjacent to the foramen magnum, so that not only is the cervical spine at risk of injury, but also the lower part of the brainstem.
These factors add up so that the cervical spinal canal of MPS patients has reduced amplitude, without necessarily occurring a bony stenosis of the canal. The use of SCOR to assess the reduction of the spinal canal in relation to the thickness of the cervical spinal cord allows an objective measurement of this stenosis.
In this study, the use of this measure in MPS patients showed a correlation between the increase in SCOR and a higher frequency of focal and extensive gliosis, a data compatible with clinical observation and the scientific literature, where findings of narrower stenoses are associated with more severe spinal lesions. Likewise, the presence of extensive gliosis (G2) at one spinal level is associated with injury extending to adjacent levels.
SCOR increased progressively with age in the 4 patients in whom this longitudinal analysis was possible. This data is compatible with the progressive nature of MPS. Additional studies of the rate of progression of the stenosis can aid in monitoring these patients, helping perhaps to decide the best moment for surgical intervention.
Patients with no gliosis (G0) or with focal gliosis (G1) showed no significant difference in relation to the clinical involvement assessed according to the clinical score used. Broomfield et al also observed that patients with focal gliosis did not present significant differences in relation to clinical manifestations when compared to those without gliosis (using their own clinical parameters), in contrast to patients with extensive gliosis (G2) who had worse neurological involvement. The severity of stenosis, assessed according to increasing values of SCOR, showed no association with the severity of the clinical involvement, suggesting that clinical abnormalities are probably due more to the consequences of the stenosis (spinal cord injury with gliosis) than to the degree of stenosis itself.
Although it was not possible to carry out statistical analysis comparing the groups without obliteration of the CSF flow with the others (partial and complete obliteration), one of the patients with adequate CSF flow had clinical alteration and gliosis. Some authors argue that microtrauma mechanisms allow spinal cord injuries to occur even in the absence of stenosis. However, this was not the case of this patient, whose 76% SCOR would already represent, according to the criteria of Nouri et al, a higher risk of spinal cord injury. This highlights the possibility that using CSF flow obstruction as a solo imaging criterion for SCC diagnosis might lead to false-negative results and late diagnosis.
All patients with at least 1 CSF obliterated column (anterior or posterior) had SCOR ≥ 70%. Although this data may represent a selection bias in patients whose diagnosis of SCC was established due to the presence of this criterion, it is possible that this data also indicates that the use of SCOR may result in a better diagnostic yield.
Conclusion
Our study was a retrospective one, using scans of patients already diagnosed with SCC, and hence there are limitations to the conclusions we’re able to draw. While this study does not aim to propose the isolated measurement of SCOR in the mid-sagittal section ≥ 70% as an isolated criterion for surgical indication in MPS patients, this measure seems to allow an objective, and perhaps earlier, diagnosis of cervical spinal canal stenosis than other methods currently available. Nouri et al found that a mid-sagittal section ≥ 70% measure is associated with greater risk of spinal damage in congenital stenosis, and it would be interesting to have this cut-off point validated for MPS populations perhaps in a future study. All but one of them (The one with atrophic lesion, G3) had mid-sagittal section SCOR ≥ 70%, with clinical scores being lower in patients with lower SCOR values. This might suggests that the 70% cut-off point could be used for the MPS populations are well.
Although sensitivity analysis was not in the scope of this study, we believe that the SCOR measurement may offer less diagnostic losses than the isolated use of CSF assessment, as recommended in the proposed scores for the diagnosis of SCC in MPS types IV and VI [18,19].Importantly, it has been observed that patients who underwent surgical decompression while still clinically asymptomatic enjoyed a better surgical outcome [4]. In that case, the usage of tools that depend on the appearance of clinical symptoms for the diagnostic of SCC might be delaying the referral for a timely intervention.
Surgical decompression, when indicated, should always be performed on a scheduled basis and with a team trained in the management of MPS patients and the potential complications involved. A timely diagnosis helps in such scheduling and preparedness.
Furthermore, future studies may help to determine whether longitudinal monitoring of the rate of increase in SCOR can provide clinically relevant data, as an indirect measure of the increase in the thickness of ligaments and meninges secondary to the progressive deposition of GAGs and a direct measure of that stenosis. This could contribute with additional information to schedule visits and monitor neurological changes (clinical or neurophysiological) in accordance to the estimated speed of disease progression, and the perceived need of a more or less urgent scheduling of surgical approach. As new treatments for these diseases become available, tools capable of evaluating disease progression speed might become invaluable.
References
- JonesS, Wijburg F (2016) Mucopolysaccharidoses, Oligosaccharidoses and Sialic Acid Disorders In:Saudubray J-M, Baumgartner MR, Walter J, editors. Inborn Metabolic Diseases. 6th ed. Berlin: Springer Berlin Heidelberg 25:577–590
- Eisengart JB, Rudser KD, Xue Y, Orchard P, Miller W, et al. (2018) Long-term outcomes of systemic therapies for Hurler syndrome: an international multicenter comparison. Genet Med 20:1423–1429
- Harmatz P, Mengel KE, Giugliani R, Valayannopoulos V, Lin SP, et al. (2013) The Morquio A Clinical Assessment Program: Baseline results illustrating progressive, multisystemic clinical impairments in Morquio A subjects. Mol Genet Metab 109:54–61
- Broomfield A, Zuberi K, Mercer J, Moss G, Finnegan N, et al. ( 2018) Outcomes from 18 years of cervical spine surgery in MPS IVA: a single centre’s experience. Child’s Nerv Syst 34:1705–1716
- Montaño A, Tomatsu S, Gottesman G, Smith M, Orii T (2007) International Morquio A registry: clinical manifestation and natural course of Morquio A disease. J Inherit Metab Dis 30:165–174
- Solanki GA, Sun PP, Martin KW, Hendriksz CJ, Lampe C, et al. (2016) Cervical cord compression in mucopolysaccharidosis VI (MPS VI): Findings from the MPS VI Clinical Surveillance Program (CSP). Mol Genet Metab 118:310–318
- Holt JB, Poe MD, Escolar ML (2011) Natural progression of neurological disease in mucopolysaccharidosis type II. Pediatrics 127:642-754
- Manara R, Priante E, Grimaldi M, Santoro L, Astarita L, et al. (2011) Brain and spine MRI features of Hunter disease: Frequency, natural evolution and response to therapy. J Inherit Metab Dis 34:763–780
- BulutE,PektasE,SivriHS,BilginerB,UmarogluMM,etal.(2018)Evaluationofspinalinvolvementinchildrenwithmucopolysaccharidosis VI: The role of MRI. Br J Radiol 91:1–9
- Ransford AO, Crockard HA, Stevens JM, Modaghegh S (1996) Occipito-atlanto-axial fusion in Morquio-Brailsford syndrome. A ten-year experience. J Bone Joint Surg Br 78:307–313
- Peck SH, Casal ML, Malhotra NR, Ficicioglu C, Smith LJ (2016) Pathogenesis and treatment of spine disease in the mucopolysaccharidoses. Mol Genet Metab 118:232–243
- Tsuchiya M, Terai H, Mizutani K, Funai Y, Tanaka K, et al. (2019) General Anesthesia Management for Adult Mucopolysaccharidosis Patients Undergoing Major Spine Surgery. Med Princ Pract 42:435-644
- Leone A, Rigante D, Amato DZ, Casale R, Pedone L, et al. (2015) Spinal involvement in mucopolysaccharidoses: a review. Child’s Nerv Syst 31:203–212
- Crockard HA, Heilman AE, Stevens JM (1993) Progressive myelopathy secondary to odontoid fractures: clinical, radiological, and surgical features. J Neurosurg 78:579–586
- Crockard HA, Stevens JM (1995) Craniovertebral junction anomalies in inherited disorders: Part of the syndrome or caused by the disorder? Eur J Pediatr 154:504–512
- Solanki GA, Lo WB, Hendriksz CJ (2013) MRI morphometric characterisation of the paediatric cervical spine and spinal cord in children with MPS IVA (Morquio-Brailsford syndrome). J Inherit Metab Dis 36:329-337
- Nouri A, Montejo J, Sun X, Virojanapa J, Kolb LE, et al. (2017) Cervical Cord-Canal Mismatch: A New Method for Identifying Predisposition to Spinal Cord Injury. Vol. 108, World Neurosurgery. Elsevier Inc 7:112–132
- Möllmann C, Lampe CG, Müller-Forell W, Scarpa M, Harmatz P, et al. (2013) Development of a Scoring System to Evaluate the Severity of Craniocervical Spinal Cord Compression in Patients with Mucopolysaccharidosis IVA (Morquio A Syndrome). JIMD Rep 11:65–73
- Lampe C, Lampe C, Schwarz M, Müller-Forell W, Harmatz P,et al. (2013) Craniocervical decompression in patients with mucopolysaccharidosis VI: Development of a scoring system to determine indication and outcome of surgery. J Inherit Metab Dis 36:1005–1013
- Jha SC, Miyazaki M, Tsumura H (2018 ) Kinetic change of spinal cord compression on flexion-extension magnetic resonance imaging in cervical spine. Clin Neurol Neurosurg 174:86–91
- Mackenzie WG, Dhawale AA, Demczko MM, Ditro C, Rogers KJ, et al. (2013) Flexion-Extension Cervical Spine MRI in Children With Skeletal Dysplasia: Is It Safe and Effective? J Pediatr Orthop 8:33-91
- Lipson SJ (1977) Dysplasia of the odontoid process in Morquio’s syndrome causing quadriparesis. J Bone Joint Surg Am 59:340–344
- Turker RJ, Slack C, Regan Q (1995) Thoracic paraplegia after lumbar spinal surgery. J Spinal Disord 8:195–200
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences