ISSN : 2393-8854
Global Journal of Research and Review
Scrub typhus: A mini review of the diagnostic challenges
Azlina Binti Ibrahim*
Department of Medicine, Bentong Hospital,Pahang, Malaysia
- *Corresponding Author:
- Ibrahim BA
Department of Medicine,
Bentong Hospital,
Pahang,
Malaysia;
E-mail: azlina1984@yahoo.com
Received Date: January 25, 2021; Accepted Date: February 08, 2021;Published Date: February 15, 2021
Citation: Ibrahim AB (2021) Scrub Typhus: A Mini Review of the Diagnostic Challenges. Glob J Res Rev Vol.8 No.S1: 001.
Abstract
Scrub typhus is a zoonotic disease caused by Orientia tsutsugamushi and is transmitted to humans by a vector of the Trombiculidae family. An estimated one million new infections of typhus scrub occur every year, and more than one billion people around the world are at risk. The disease most commonly distributed in the Asia Pacific regions including Malaysia. Scrub typhus has been a neglected infectious disease for a long time hence many aspects of the disease including the diagnosis are still uncertain. It affects people of every age, including children. Humans are accidental hosts of the zoonotic disease. Patients with scrub typhus often develop non-specific symptoms that may mimic other zoonotic diseases. The clinical similarities between scrub typhus and other zoonotic diseases, the absence of pathognomonic eschars in some patients and the absence of diagnostic tests in some health care facilities pose a major challenge for the clinician. Effective and appropriate care should be initiated in a timely manner, as delay in treatment of scrub typhus can result in serious multiorgan failure with a case-fatality rate of up to 70%.
Keywords
Scrub typhus; Neglected infectious disease; Diagnostic challenges
Introduction
Scrub typhus is an acute febrile illness caused by Orientia Tsutsugamushi commonly occur in zoonosis endemic in the Asia Pacific region. It is also called as tsutsugamushi disease or rural typhus [1]. The disease is transmitted by the bites of infected Leptotrombidium mites also known as chiggers [2]. Although the majority of scrub typhus is known to be more common in rural areas, there are reported cases of acute infection and serological evidence of infection in metropolitan cities [3]. Patients commonly had flu-like symptoms such as fever, headache, abdominal pain, and myalgia lasting approximately one week. Scrub typhus is an important differential diagnosis in patients with acute febrile illness in South East Asia. The lack of diagnostic test for scrub typhus particularly in rural hospital impose a major challenge for clinicians. Clinicians must have a high index suspicion of scrub typhus, especially for patients who live or travel to the endemic region. Failure to diagnose scrub typhus results in delayed treatment and the patient will end up with serious complications such as multiorgan failure, disseminated intravascular coagulopathy and even death. Early diagnosis and appropriate management of scrub typhus is crucial.
In a paper entitled 'A Case of Successful Treatment of Septic Shock Secondary to Scrub Typhus,' we described the case of a young man in a district hospital with unexplained fever and septic shock who was successfully treated with scrub typhus on the basis of clinical history, recreation exposure and presence of eschar.
Scrub typhus is commonly distributed in the Tsutsugamushi triangle. This includes a very large area bounded by Japan in the east, through China, the Philippines, tropical Australia in the south and west through India and Pakistan [4]. The scrub typhus vector is present in most countries of the South East Asia region and is endemic in certain geographical regions of those countries [4]. The incubation period for scrub typhus is between six and twenty-one days [5]. Human infection is initiated by bite of infected larval, also known as chigger. Endothelial cells are one of the primary cellular targets for Orientia tsutsugamushi during systemic infection [4]. The multiplication of the organism at the site of inoculation results in vascular injury involving organs such as the kidney, liver, brain, skin, meninges and lungs. Patients develop rickettsemia within a few days and vascular injury in organs results in diffuse intravascular coagulation (DIC) with platelet consumption, vascular leakage, pulmonary edema, shock, hepatic dysfunction and meningoencephalitis.
The most common clinical features of scrub typhus are fever with chills, headache, back pain, myalgia, profuse sweating, vomiting, and enlarged lymph nodes [5]. These symptoms may mimic other zoonotic diseases such as dengue fever, leptospirosis, malaria, salmonella typhi and other rickettsial disease. The severity of infection can range from mild symptoms and signs to multiorgan failure [6]. Clinical similarities between scrub typhus and other zoonotic diseases result in a major challenge for clinicians to diagnose scrub typhus. It is crucial for clinicians to be able to diagnose typhus scrub on the basis of clinical judgment, as delays in therapy are associated with a higher risk of complications [7].
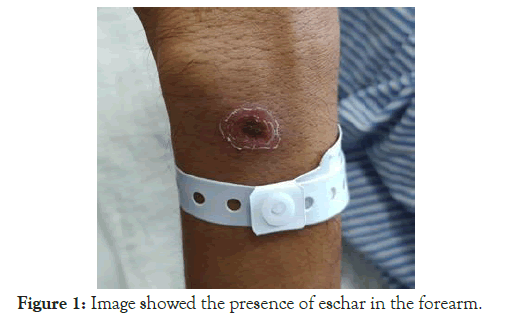
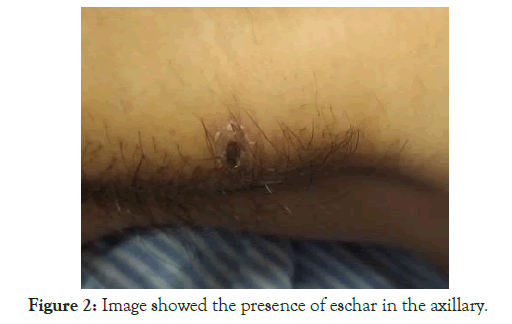
Eschar is a valuable clue to the diagnosis of scrub typhus, although the overall prevalence of eschar varies in between 20%-87% [8]. It begins as a papule at the site of chigger feeding and then ulcerates and form a black crust like a necrotic lesion (Figure 1 and Figure 2). The border of an eschar may be erythematous. The size of the eschar range is between 5 mm-20 mm and is commonly seen in the covered areas of the body such as axilla, groin, inguinal, chest, lower back including buttocks [9]. Retrospective analysis showed that there was a significant difference in the distribution of eschars between males and females with some unusual sites of the eschar including the cheek, ear lobe and dorsum of the feet [10]. Eschar resolves in 3-4 weeks but may occasionally cause scarring or hyperpigmentation [11]. Most patients did not notice the lesion as the vector bite is painless, although it may sometimes be pruritic. Therefore, given the location of the eschar in the covered area and the nature of the bite that is painless, it is often missed during routine physical examination. A thorough examination is needed to improve the detection of eschar, leading to an improvement in the diagnosis of scrub typhus in the clinical setting. An eschar may not be observed in each confirmed case, therefore the history of travel to or reside in an endemic area is also an important indication of favouring the diagnosis of scrub typhus [2].
At present, no laboratory test is diagnostically reliable in the early phase of typhus scrub. The disease is diagnosed at an early presentation on the basis of clinical signs and symptoms, laboratory features and epidemiological evidence. Patients with scrub typhus may develop thrombocytopenia, elevated liver enzymes, bilirubin and creatinine. Most patients have normal white cell counts but leukopenia or leukocytosis is not uncommon. Laboratory findings are relatively non-specific. There are four ways to detect the presence of O, tsutsugamushi infections, including serology, biopsy, culture and polymerase chain reactions. The lack of these diagnostic tests in district hospitals, however, has raised another challenge for clinicians. There are few serological tests currently available for use. Clinician must be aware of the limitations of these tests. Weil Felix OX-K agglutination is the oldest test that is easy to perform and inexpensive, but lacks specificity and sensitivity. It is therefore no longer recommended for use [12]. The current reference standard test is the indirect fluorescent antibody test and the indirect immunoperoxidase test [13]. The indirect fluorescent antibody test is more sensitive and results can be achieved within a few hours, but the test is expensive and requires training [14]. Indirect fluorescent antibody test uses anti-human fluorescent antibody to detect specific antibodies to scrub typhus antigen from the patient serum while indirect immunoperoxidase test uses peroxidase instead of fluorescein in the same manner. The serologic diagnosis of acute infection among patients living in endemic area must be differentiated from background immunity against scrub typhus. Therefore, the definitive diagnosis of acute scrub typhus infection with an indirect fluorescent antibody assay is based on at least fourfold increase in titer in paired samples taken at least 14 days apart [14]. Other serological tests that have also been developed for the diagnosis of scrub typhus include the enzyme-linked immunosorbent assay and the passive hemagglutination assay. Another diagnostic test for scrub typhus is an eschar biopsy that may show histological changes such as focal areas of cutaneous necrosis surrounded by an area of intense vasculitis, with perivascular lymphocyte and macrophage collections. Other diagnostic tests include culture of the organism and polymerase chain reaction, but are only available in specialized centers that have access to the laboratory facilities [15].
Conclusion
Scrub typhus is a neglected zoonotic disease that causes lifethreatening illness. It is an important cause of acute febrile disease in the Asia-Pacific region. The non-specific clinical characteristics and absence of eschar present a major challenge for the clinician. The lack of a diagnostic test in the early phases of scrub typhus has raised concerns about misdiagnosis of scrub typhus. The main management challenge is to deliver specific therapy in a timely and effective manner, as delays in treatment result in major complications. Clinicians must be able to recognize typhus scrub on the basis of symptoms, clinical signs, laboratory features with epidemiological clues. Rapid and accurate diagnosis of scrub typhus is needed especially in endemic settings to prevent complications and death.
References
- Chakraborty S, Sarma N (2017) Scrub typhus: An emerging threat. Indian J Dermatol 62: 478-485
- Xu G, Walker DH, Jupiter D, Melby PC, Arcari CM (2017) A review of the global epidemiology of scrub typhus. PLoS Negl Trop Dis 11: e0006062.
- Wei Y, Huang Y, Luo L, Xiao X, Liu L, et al. (2014) Rapid increase of scrub typhus: An epidemiology and spatial-temporal cluster analysis in Guangzhou City, Southern China, 2006-2012. PloS One 9: e101976.
- Kumar D, Raina DJ, Gupta S, Angurana A (2010) Epidemiology of scrub typhus. JK Science 12: 60-62.
- Devine J (2003) A review of scrub typhus management in 2000-2001 and implications for soldiers. Journal of Rural Remote Environmental Health 2: 14-20.
- Settle EB, Pinkerton H, Corbett A (1945) A pathologic study of tsutsugamushi disease (scrub typhus) with notes on clinicopathologic correlation. Journal of Laboratory and Clinical Medicine 30: 639-661.
- Trung NV, Hoi LT, Dien VM, Huong DT, Hoa TM, et al. (2019) Clinical manifestations and molecular diagnosis of scrub typhus and murine typhus, Vietnam, 2015-2017. Emerg Infect Dis 25: 633-641.
- Ogawa M, Hagiwara T, Kishimoto T, Shiga S, Yoshida Y, et al. (2002) Scrub typhus in Japan: Epidemiology and clinical features of cases reported in 1998. Am J Trop Med Hyg 67: 162-165.
- Sundriyal D, Kumar N, Chandrasekharan A, Sharma B (2013) Eschar: An important clue to diagnosis. BMJ Case Rep 2013: bcr2013010105.
- Kundavaram AP, Jonathan AJ, Nathaniel SD, Varghese GM (2013) Eschar in scrub typhus: A valuable clue to the diagnosis. J Postgrad Med 59: 177-178.
- Saini R, Pui JC, Burgin S (2004) Rickettsialpox: Report of three cases and a review. J Am Acad Dermatol 51: S137-142.
- Kelly DJ, Wong PW, Gan E, Lewis Jr GE (1988) Comparative evaluation of the indirect immunoperoxidase test for the serodiagnosis of rickettsial disease. Am J Trop Med Hyg 38: 400-406.
- Koh GCKW, Maude RJ, Paris DH, Newton PN, Blacksell SD (2010) Diagnosis of scrub typhus. Am J Trop Med Hyg 82: 368-370.
- Blacksell SD, Bryant NJ, Paris DH, Doust JA, Sakoda Y, et al. (2007) Scrub typhus serologic testing with the indirect immunofluorescence method as a diagnostic gold standard: A lack of consensus leads to a lot of confusion. Clin Infect Dis 44: 391-401.
- Kim DM, Yun NR, Yang TY, Lee JH, Yang JT, et al. (2006) Usefulness of nested PCR for the diagnosis of scrub typhus in clinical practice: A prospective study. The American journal of tropical medicine and hygiene 75: 542-545.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences