Retrospective Analysis of Histopathological and Microbiological Correlation of Autopsy Series
Tanushri Mukherjee*, Soma Mukherjee, Nalin Singh and Anshuman Singh
Department of Pathology, Command Hospital, Chandigarh, India
- *Corresponding Author:
- Tanushri Mukherjee
Oncopathologist
Associate Professor
Department of Pathology
Command Hospital, Chandigarh, India
Tel: +91 8697989701
E-mail: tanujamukherjee@yahoo.com
Received Date: March 06, 2017; Accepted Date: March 29, 2017; Published Date: April 07, 2017
Citation: Mukherjee T, Mukherjee S, Singh N, et al. Retrospective Analysis of Histopathological and Microbiological Correlation of Autopsy Series. J Clin Med Ther. 2017, 2:2.
Copyright: © 2017 Mukherjee T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: In this retrospective observational study, we reviewed macroscopic postmortem examinations of surgical Intensive Care Unit (ICU) patients who died from suspected sepsis or septic shock.
Methods: All 125 Patients who were admitted in the ICU and subsequently died and cause of death labeled as sepsis/septic shock. Clinical data and postmortem findings were documented in all patients.
Results: The study included postmortem results which included gross, histopathology and microbiology. The main causes of death as reported in the patient history were sepsis with multiple organ dysfunction syndrome (70%) and cardiorespiratory failure (30%). Pathologies were detected in the lungs in 18 cases, kidneys/urinary tract 05 cases, gastrointestinal tract 02 cases, cardiovascular system 09 cases, liver 20 cases, spleen 01 case, central nervous system 30 cases, and pancreas 08 cases and in 32 cases multiple organ pathology was seen like lung, brain, liver. The autopsy and microbiological examination revealed confirmatory growth and septic focus in 40 (32%) cases only. The microbiological isolates were obtained from CSF, heart blood, ascitic fluid, pleural and pericardial fluid and tracheal aspirates. Most common isolate was Klebsiella in 25 cases.
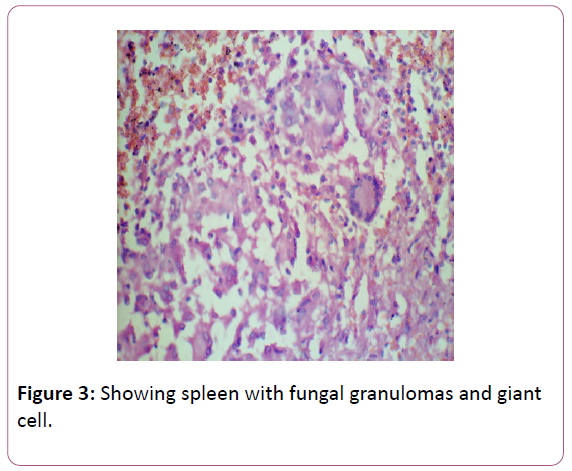
Conclusion: Relevant postmortem findings explaining death in surgical ICU patients who died because of sepsis/ septic shock were a continuous septic focus in approximately 40%, primary CNS pathology 37.5% cardiac pathologies in 7.2%. The most frequently affected organs were the brain, liver, lungs. Multiple organ system was also involved in 32 cases and disseminated fungal infection was the cause of death in 2 cases.
Keywords
Histopathology; Hemorrhagic infiltrations; Encephalitis; Pathology
Introduction
This retrospective observational study reviews the macroscopic, histological and microbiological findings in postmortem examinations of 125 patients who died in ICU clinically labeled as sepsis or septic shock.
Methods
125 patients during their ICU stay who subsequently died from suspected sepsis/septic shock. The clinical records of all patients were checked and the results of the microbiological specimens of each patient were retrieved to confirm infection. The postmortem examination was done in indicated cases after proper consent was performed in patients as follows: A vertical incision from suprasternal notch to the symphysis was used to expose internal organs. The organs were removed in four blocks: 1) Heart and lungs, 2) Liver and gastrointestinal tract, 3) Urogenital system, 4) Brain. Afterwards, all organs were systematically examined for macroscopic pathologies and tissue samples were taken for histological analyses and samples from CSF, pleural fluid, ascitic fluid, and peritoneal fluid; pus and heart blood were subjected to culture and microbiological examination.
The following variables of all study patients were extracted from the clinical charts as gender, age, disease status, and source of infection, the pathogen type cultured, presence of sepsis or septic shock; the number of failing organs, presence of acute respiratory distress syndrome. Autopsy reports of all study patients were searched for pathologies of the following organ systems: cardiovascular system, lungs, liver, kidneys and urinary tract, gastrointestinal tract, spleen, pancreas, and central nervous system. Pathologies of other organ systems were recorded separately.
Postmortem findings of each organ system were entered. The weight of each organ was measured. Heart was seen whether enlarged or not and further seen for any diffuse or localized red-blue (yellow-tan at later stages) lesions of the myocardium with or without occlusion of the supplying coronary artery, dilatation of the right or left ventricular chamber, reddened and granular pericardium optionally accompanied by pericardial effusion, fluid collection in the pericardial cavity and any friable, bulky or destructive vegetation’s on cardiac valves containing fibrin, inflammatory cells, and pathogens on histology were studied. Lungs for any frothy, blood-tinged fluid. Consolidated lung areas (increased in volume) with patchy infiltrations rendering pus on sectioning, Fluid collection in one or both pleural cavities (blood, hematothorax; pus, pleural empyema). Reddened, edematous mucosa of substantial parts of the tracheobronchial tree; optionally accompanied by serous or mucous secretion. Partial or total occlusion of a pulmonary artery is due to a venous thrombus. Consolidated lung areas; with hemorrhagic infiltrations. Reddened, edematous pleura optionally accompanied by a fibrinous exudate, raised, red-blue (red-brown at later stages), wedge-shaped areas extending to the lung periphery optionally accompanied by fibrinous pleuritis. Consolidated (dark blue-red) lung areas reduced in volume.
Liver was examined whether yellow, greasy and readily fractured with increased weight (2000 g). Diffuse, patchy and pale alterations localized in the central region of the liver lobules, purulent inflammation of the extra/intrahepatic bile ducts with or without necrotic infiltration of portal fields. Enlarged or tense gallbladder with bright-red to green-black patchy discoloration and optionally fibrin-layered serosa or suppurative exudate.
Diffuse or localized bowel alterations with dilatation, edema and wall thickening (optionally intraluminal gas) with or without occlusion of the supplying mesenteric artery. Edematous gastric mucosa; with vascular congestion, but maintained mucosal barrier Intraluminal blood originating from lesions of the gastrointestinal tract. Erosions of the gastric or duodenal mucosa are equal to or greater than 0.5 cm in diameter. Continuous localized or diffuse inflammation of the peritoneum with suppurative or fibrinous exudate. Diffuse or localized bowel alterations with congestive edema, wall thickening, dusky to purple-red discoloration and hemorrhagic lesions with or without luminal blood.
Serous fluid collection in the abdominal cavity. Pale and wedge-shaped areas of the spleen; optionally accompanied by fibrin coverage of the splenic capsule. Enlarged and soft spleen with deliquescent splenic parenchyma on incision. Diffuse or localized, pale or reddish areas of the pancreatic parenchyma. Blue-black hemorrhagic areas interspersed with foci of yellow-white, chalky fat necrosis.
Kidney for any diffuse enlargement with or without specific parenchymal pathology. Sharply demarcated, pale (yellow-white at later stages) areas containing hemorrhagic foci with or without occlusion of the supplying renal artery. Grayish-white discoloration of pyelum and ureter optionally accompanied by patchy inflammation or necrosis of the renal parenchyma. Reddened, edematous mucosa of the urinary bladder optionally accompanied by a suppurative exudate.
Postmortem findings of the central nervous system studied like brain edema, ischemia, intracerebral hemorrhage, encephalitis. Swollen brain with flattened gyri, narrowed sulci and compressed ventricular cavities, any tentorial or foraminal brain herniation. Diffuse or localized, pale and swollen (gelatinous or liquefied at later stages) areas of the brain without occlusion of the supplying cerebral artery.
Statistical Analysis
The SPSS software program (SPSS 12.0.1.; SPSS, Chicago, IL) was used for statistical analysis. Descriptive statistical methods were applied to evaluate the frequency of pathologies of single organ systems. In order to compare the frequency of organ pathologies between groups, Fisher’s exact test was used, as appropriate. P values 0.05 were considered as indicating statistical significance. Data are given as mean values SD, if not otherwise indicated.
Results
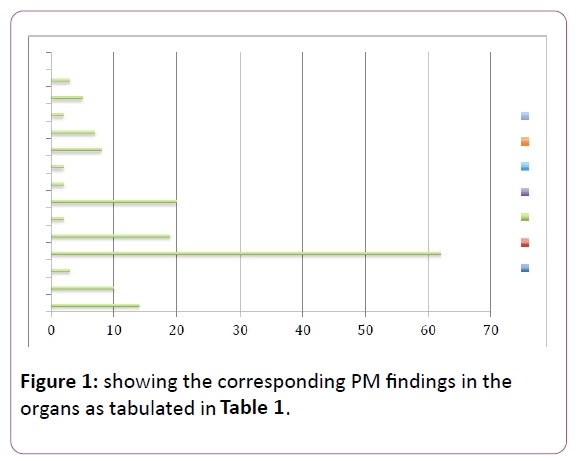
Post mortem examination was done in the 125 patients of which all were male except one female patient who died of metastatic breast cancer. The age range was in between 26-47 yrs. of age. Primary CNS pathology: 37.5% cardiac pathologies in 7.2%. The most frequently affected organs were the brain, liver, lungs. Multiple organ system was also involved in 32 cases and disseminated fungal infection was the cause of death in 2 cases, malignancy was the cause of death in 08 cases (Figure 1).
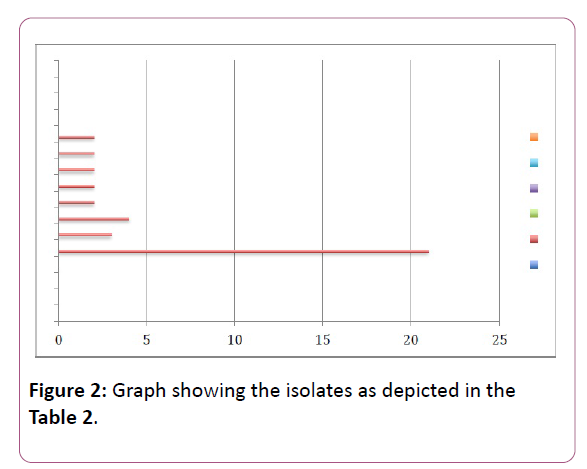
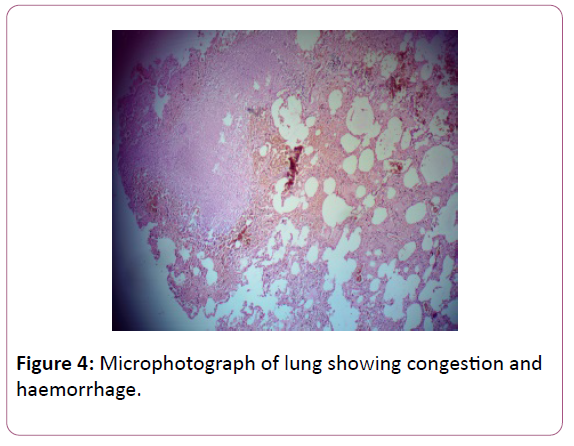
The brain edema was observed in nearly 62 patients 49.6% of patients. Fifty of these patients were admitted to the ICU because of a primary CNS pathology. The results of the postmortem summarized in form of Table 1. Brain hemorrhage was seen in 14 patients, infarct in 10 cases, abscess in 03 cases, edema 62 cases, lung congestion and pneumonia 19 cases, lung abscess in 02 cases, liver cirrhosis in 20 cases, 02 cases acute tubular necrosis histologically, pancreatitis in 08 cases, coronary artery disease in 07 cases, cardiomyopathies 02 cases, malignancies in 08 cases. Septic focus found in approximately 40% of the postmortem samples. The culture grew Klebsiella in 23 cases, Acinetobacter in 03 cases, Escherichia coli in 04 cases, streptococci in 02 cases, 02 cases in Pseudomonas, Burkholdria in 02 cases, Enterococci in 02 cases and candida in 02 (Table 2). The most common isolate is Klebsiella (52%) (Figures 2-4).
| Brain PM changes | Lung | Liver | Kidney | GI tract | Heart | Neoplasms | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Haemorrhage | Infarct | abscess | edema | Congestion and pneumonia | abscess | Cirrhosis | acute tubular necrosis | Ischemia | Pancreatitis | CAD | Cardiomyopathy | Lymphoma | Carcinoma |
| 14 | 10 | 3 | 62 | 19 | 2 | 20 | 2 | 2 | 8 | 7 | 2 | 5 | 3 |
Table 1: Postmortem organ changes in the autopsy findings (n=125).
| Isolate | No of cases |
|---|---|
| Klebsiella | 21 |
| Acinetobacter | 3 |
| Escherichia coli | 4 |
| Streptococci | 2 |
| Enterobacter | 2 |
| Burkholderia | 2 |
| Candida | 2 |
| Pseudomonas | 2 |
Table 2: Showing the microbiological isolate from the autopsy cases.
Discussion
To evaluate sepsis the main features are the gross pathology, the microscopic pathology (histopathology and cytopathology), and identification and quantification of infectious agents [1-5]. Sepsis-related myocardial dysfunction includes reduced left and right ejection fractions and elevated heart rate and evidence of apoptotic damage to cardiac myofibrils and myocarditis with enlargement of capillary endothelial cells as part of the generalised endothelial, upregulation phenomenon. Given the generally old age of patients admitted to ICU with sepsis, many will have coronary artery disease, with or without previous myocardial infarction, at autopsy [6-23].
In our patient population, most continuous septic foci detected were located in the lungs, CSF, peritoneal cavity and heart in only 40% of the cases. Of all organ pathologies, the most relevant for patient mortality seems to have been pathology of the cerebral nervous system and brain and cardiovascular pathology, since uncontrollable shock was the clinical cause of death in 25% of the study population and almost all patients had shock [21-26]. Patients who died of septic shock showed more such apoptosis in the amygdala and medullary autonomic nuclei than those dying of non-septic shock and sudden extra-cranial trauma which was seen in our patients dying due to nonsepsis causes and in whom there were no microbiologic growth.
Conclusion
The main clinical and postmortem causes of death in critically ill patients in ICU who were labeled as sepsis were brain pathology, refractory multiple organ dysfunction syndrome and uncontrollable cardiovascular failure. Relevant postmortem findings explaining these results were a septic focus in only 40% of cases. The most frequently affected organs were the brain, liver, cardiopulmonary system. Autopsy examination of the organs and histology helps to arrive at the final cause of death.
References
- Morris JA, Harrison LM, Partridge SM (2006) Postmortem bacteriology: a revaluation. J Clin Pathol 59:9.
- Dellinger P, Carlet JM, Masur H, Gerlach H, Calandra T, et al. (2004) Surviving sepsis campaign guidelines for management of severe sepsis and septic shock. Crit Care Med 32: 858-878.
- Roosen J, Frans E, Wilmer A, Knockaert DC, Bobbaers H (2000) Comparison of premortem clinical diagnoses in critically ill patients and subsequent autopsy findings. Mayo Clin Proc 75:562-567.
- Goldman L, Sayson R, Robbins S, Cohn LH, Bettman M, et al. (1983) The value of the autopsy in three medical eras. N Engl J Med 308:1000-1005.
- Combes A, Mokhtari M, Couvelard A, Trouillet JL, Baudot J, et al. (2004) Clinical and autopsy diagnoses in the intensive care unit: a prospective study. Arch Intern Med164:389-392.
- Perkins GD, McAuley DF, Davies S, Gao F (2003) Discrepancies between clinical and postmortem diagnoses in critically ill patients: an observationsl study. Crit Care7:R129-R132.
- Blosser SA, Zimmerman HE, Stauffer JL (1998) Do autopsies of critically ill patients reveal important findings that were clinical undetected? Crit Care Med 26:1332-1336.
- Annane D, Bellisant E, Cavaillon JM (2005) Septic shock. Lancet365:63-78.
- Riederman NC, Guo RF, Ward PA (2003) The enigma of sepsis. J Clin Invest 112:460-467.
- Danai P, Martin GS (2005) Epidemiology of sepsis: recent advances. Curr Infect Dis Rep 7:329-334.
- Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, et al. (1992) SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 31:1250-1256.
- Calandra T, Cohen J, International Sepsis Forum Definition of Infection in the ICU Consensus Conference (2005) The International Sepsis Forum Consensus Conference on Definitions of Infection in the Intensive Care Unit. Crit Care Med 33:1538-1548.
- Fowler A, Collins L, de Ruiter A, Whittaker S, Kulasegaram R, et al. (2006) Multicentric Castleman's disease in a patient with HIV. Int J STD AIDS17:63-64.
- Munford RS, Suffredini AF (2005) Sepsis, severe sepsis, and septic shock. Douglas and Bennett's principles and practice of infectious diseases (8thedn.). Elsevier Churchill Livingstone, Pennsylvania, pp: 906-925.
- KumarV, Abbas A, Fausto N, Aster J (2005) Hemodynamic disorders, thromboembolic disease, and shock. Robbins and Contran pathologic basis of disease (9thedn.). Elsevier Saunders, Philadelphia, pp:119-144.
- Hotchkiss RS, Swanson PE, Freeman B, Tinsley KW, Cobb JP, et al. (1999)Apoptotic cell death in patients with sepsis, shock, and multiple organ dysfunction. Crit Care Med 27:1230-1251.
- Singer M, De Santis V, Vitale D, Jeffcoate W (2004) Multiorgan failure is an adaptive, endocrine-mediated, metabolic response to overwhelming systemic inflammation. Lancet 364:545-548.
- Levy RJ, Piel DA, Acton PD, Zhou R, Ferrari VA, et al. (2005) Evidence of myocardial hibernation in the sepsis heart. Crit Care Med 33:2752-2756.
- Villar J, Maca-Meyer N, Perez-Mendez L, Flores C (2004) Bench-to-bedside review: understanding genetic predisposition to sepsis. Crit Care 8:180-189.
- Tsokos M (2003) Immunohistochemical detection of sepsis-induced lung injury in human autopsy material. Legal Med5:73-86.
- Zhu BL, Ishikawa T, Michiue T, Quan L, Maeda H (2005) Postmortem serum endotoxin level in relation to the causes of death. Legal Med 7:103-109.
- Hirata, K., Miyagi, S., Tome, M. et al. (1988) Cor pulmonale due to tumour cell microemboli. Arch Intern Med148:2287-2289.
- Ha T, Grant D, Xia Y, Hua F, Ma J, et al. (2006) Glucan phosphate attenuates cardiac dysfunction and inhibits cardiac MIF expression and apoptosis in septic mice. Am J Physiol Heart Circ Physiol 291:H1910-H1918.
- Dimopoulos G, Piagnerelli M, Berre Ì J, Salmon I, Vincent JL(2004) Post mortem examination in the intensive care unit: still useful? Intens Care Med30:2080-2085.
- Loughrey MB, McCluggage WG, Toner PG (2000) The declining autopsy rate and clinicians’ attitudes. Ulster Med J69:83-99.
- Pastores SM, Dulu A, Voigt L, Raoof N, Alicea M, et al. (2002)Premortem clinical diagnoses and postmortem autopsy findings.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences