ISSN : 2574-2825
Journal of Nursing and Health Studies
Medication Errors Related to High Alert Medication
Nipul Kapadia*, Sachin Raval and Parag Gadhave
Apollo Hospitals International Limited, Ahmedabad, India
- *Corresponding Author:
- Kapadia N
Apollo Hospitals International Limited
Ahmedabad, India
Tel: 07698815153
E-mail: sachinr@apolloahd.com
Received date: October 04, 2017; Accepted date: October 16, 2017; Published date: October 21, 2017
Citation: Kapadia N, Raval S, Gadhave P (2017) Medication Errors Related to High Alert Medication. J Nurs Health Stud Vol.2:No.3:15. doi: 10.21767/2574-2825.100021
Abstract
Objective: The aim of this study was to compare the trend of medication error due to high alert medications before and after re-implement revised strategies of high alert medications.
Methods: The data of medication errors from January 2017 to April 2017 were collected and medication errors happened due to high alert drug was identified. Analyzed the high alert medication errors and calculate the rate of errors. Develop strategies and re-implement in medication process.
The data of high alert medication errors during May 2017 to August 2017 were collected. The percentage of occurrence and severity of high alert medication error were identified and calculated.
Results: Frequency of high alert medication errors were reduced considerably after developing and implementing of preventive strategy of high alert medication.
Conclusion: The developed strategies for prevention the high alert medication reduce the high alert Medication errors. However, the surveillance of the high alert medication error rate should be further monitored and strategies to be continuously monitored for its effectiveness.
Keywords
High alert medication; Medication error
Introduction
A medication error (ME) is any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the health care professional or patients [1].
Approximately, 30% of problem occurs during hospitalization are related to medication error. India records 5.2 million medical injuries a year 2016; 43 million people are injured worldwide each year due to unsafe medical care. A number of studies have shown that medication errors are one of the main causes leading to disability and death in up to 6.5% of hospital admissions [2].
In tertiary care hospital there is multiple number of prescription on daily basis with multiple type of patient. Use of all type of high alert medication was prescribed for the patient. Vast drug formulary was to be maintained for all type of medicine including high alert medicine. All this thing leads to increases probability of error related high alert medication and required a strong system to reduced or prevent the medication error for patient safety, more focus on high alert medication related error due to seriousness of this type of error.
In a tertiary care hospital in Ahmedabad accredited with JCI and NABH, one study was conducted to reduce the medication error related to high alert medication.
In initials stage errors related concentrated electrolytes and insulin was more, as concentrated electrolyte was not checked by double nursing and not sign by two nursing staff for administration of medication. LASA medication errors in dispensing of medicine were more confusing and storage needs to separate. In case of insulin self-administration and verbal order from doctor to nurse after informing RBS. This are the major observation which causes the near miss errors.
Material and Methods
Inclusion criteria
Analysis was done for type c medication errors only. Medication error which is reported in hospital for admitted patient taken under consideration. High alert medication error was as per drug and therapeutic committee approved high alert medication list of organization.
Errors reporting by the pharmacy, nursing and doctors are very less and clinical pharmacist reported the errors during daily ward round are taken for the study.
Exclusion criteria
Outpatient department errors were not considered for study.
Need of Study/Project
Phase 1 (Problem identification)
The data of high alert related medication errors during January 2017 to April 2017 were prospectively collected. The stages of medication error; prescribing error, transcribing error, dispensing error, and administration error were identified and high alert ME rate was calculated using following equation.
High Alert Me Rate= Number of High Alert Medication Errors/ Number of Total Χ 100
Phase 2 (Problem monitoring and elimination)
The collected medication errors were presented to the Drug and Therapeutic Committee (DTC) of the hospital. The strategies for prevention of medication errors were constructed by DTC follow the causes of error; high alert drugs storage in pharmacy, labeling of high alert drugs, training for high alert drug to doctors, pharmacy and nursing, Prescription in drug chart, Updating of high alert drugs list, Attention towards high alert drugs in ward round [3].
The target groups of constructed strategies were including doctor, pharmacist, and nurse. The data of medication errors during May 2017 to August 2017 were collected. The high alert ME were identified and calculated as mention previously. Reducing of ME related to high alert drugs was monitored. The redeveloped prevention strategies were focused in topics including high alert drugs storage in pharmacy, routinely training for high alert errors, proper communication with doctors, nurse and pharmacist.
Cytotoxic medications: ME related to cytotoxic medication was the most serious ME error. For chemotherapy new protocol format was developed with details of dose calculation with BSA and standard dose. Protocol has to be signed by consultant, ward doctor, pharmacist and nurse with double checking. Pre- medication was PAT verified by clinical pharmacist and after started chemo patient observation by nurse for ADR management. To avoid exposure related issues all dilutions are strictly in biological safety cabinet (class II, Type B1) with safety of pharmacist, medicine and environment [4].
Concentrated electrolyte managements: Administration of concentrated electrolyte in patient need to double sign by nurses in drug chart. Caution label prepared and stick on every conc. Electrolyte before dispensing from IP Pharmacy. No stock in ward or bed side should kept issue only unit dose. No verbal order is allowed for any medicine. Clinical pharmacist reviews the medicine order for dose and dilution instruction and indication before administrating the medicine. New Software was prepared for Concentrated Electrolyte checking on daily basis.
Insulin: Insulin is considered to regulates the metabolism of carbohydrates, fats and protein by promoting the absorption of glucose from the blood into fat, liver and skeletal muscle cells. Some of the most common insulin related problems that can occur. If the nurse/patient forgets a previous injection and give another before it’s necessary. Nurses are distracted and accidentally inject too much [5]. Patient refuses to eat or forget to eat or have an unexpected mealtime delay but the nurse administers the insulin. If the patient is given a morning dose at night, or vice versa can happen if any verbal orders in case of insulin are given. The main problem related to verbal order. To avoid verbal order strictly follow the policy of no verbal order. Education related to administration of insulin for nursing and self-administration leaflet was made by pharmacy department. Continues education for dosing scale of insulin for doctors was arranged. Opening and discard label was made compulsory for storage of insulin vial at bed side to avoid storage error.
Heparin: In case of heparin, hemorrhage can occur at virtually any site in patients. An unexplained fall in hematocrit, fall in blood pressure. Sever hypertension or spinal anesthesia, major surgery or patient diagnosed with hemophilia, thrombocytopenia and some vascular purpuras. These are some conditions in which increased danger of hemorrhage.
Heparin dose was needed to calculate by clinical pharmacist. Dosage should be regulated by frequent blood coagulation tests. Opening and discard label is made compulsory for storage medicine at bed side. High alert label is pasted from IP Pharmacy on each and every injection. Continue the round by pharmacist for monitoring high alert medicine.
Narcotics: These are the drug having capacity of addiction hence may get abuse in hospital by healthcare worker or patient. Due to this narcotic have to monitor more specifically in tertiary care hospital. All prescriptions related to narcotics was strictly under observation to clinical pharmacist and medical admin. Triplicate prescription is used to is issued narcotics to patient with proper documentation. Administration of narcotics dose is under observation of doctors only. Discard of unused medicine by nursing under observation of pharmacist or doctors. Storage of narcotics in double lock and Prescription should be in capital and written by only registered doctors with MBBS only. Since we have strict follow up of this protocol no any error reported related narcotics.
LASA drugs storage: It observed that LASA drug was put in the same place or near each other. Then Pharmacy Department modified drug shelf and rearrange drugs. From our observation Tall man lettering was not found to be very effective to prevent LASA medication errors [6]. In addition, the printed reflect sticker was used for identification (LASA drugs were kept separately in rack). Update the list of LASA medication on the basis of medication errors. Published in every ward/ICUs. Implemented Separate storage in ICU/Wards for LASA Medications.
To avoid dispensing of adult and pediatric medicines interchangeability they were kept separated. The drug and therapeutic committee consider the drug items that may cause ME such as drug that had two strengths and same drug with multiple brands.
Training for high alert medications: For the updating of medicine dose knowledge and prescription writing in drug chart for new resident doctors, training lectures were conducted. Frequently occurred errors found for example i) Inj. Cefoprim (Cefuroxime sodium) as brand name and Inj. Cefepim as generic name get confused and ii) Unapproved abbreviations were found a contributing factor for high alert ME, such as Inj. Heparin 5000 units (it should be write as Inj. Heparin 5000 unit) may read as 50000.
Regular Medication Safety Round by senior pharmacist and Clinical Pharmacist in Wards/ICUs to prevent the medication errors and on job training is given to Nurses and Doctors. During the round errors was identified and on the spot education was given to concern persons.
For nursing error spotted was wrong transcription for example Inj. Fosolin 150 mg was transcribed as Inj. Fosaran 150 mg. Nurses were trained for the high alert drugs.
Pharmacy staff was trained for reimplementation of read back policy, read drug label before dispensing and not to dispense by physical appearance, double check medicine before dispensed. Reconfirm the medicine order from consultant regarding any discrepancy/doubt [7].
Updating of high alert Drug LIST: As per ISMP (Institute of Safe Medication Practice) new updated list for high alert drug was introduced by combined efforts of doctor, Pharmacy and Nursing department as per the drug availability at ABMH and trend of errors [8]. Updated list was distributed to all wards and pharmacies. Additionally, error based list was developed by clinical pharmacy contains (Table 1).
| 1 | Hosit (Methylcobalamin) | Strocit (Citecholin) |
| 3 | Midzee (Midazolam) | Azee (Azithromycin) |
| 4 | Fosolin (Fosphenytoin) | Fosaran (Fosaprepitent) |
| 5 | Metro (Metronidazole) | Meronem (Meropenam) |
| 6 | Mesna (Uromitexan) | Mesna neb. (Mistabron) |
Table 1: High alert drug list.
Audit by clinical pharmacy
Ward rounds are conducted on daily basis and error found are informed to concerned doctors and corrected immediately and summarized report discuss in PTC. Transcription by medication nurse on hospital integrated system is proof read by clinical pharmacy online (before it dispensed) by concerned pharmacy store. Random stock audits are conducted timely to assure the compliance of high alert drug storage policy.
Result and Discussion
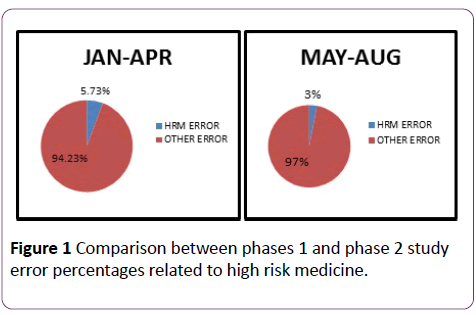
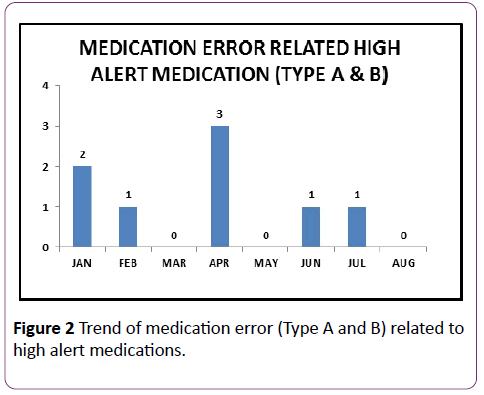
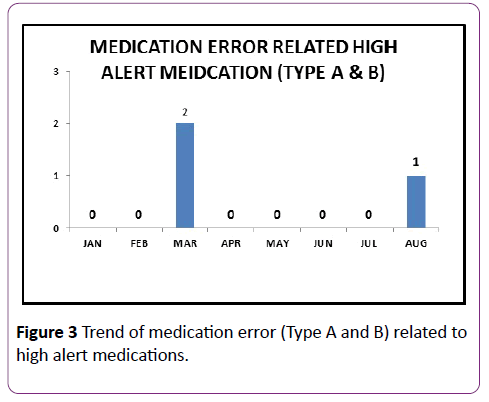
These figure show that there is significant decrease in errors related to high alert medicine and also it is observed that total error also somewhat decreases in trend due to daily round by pharmacy and continued education to nursing staff and Doctors (Figures 1-3).
Conclusion
The developed strategies for the prevention of high alert medications successfully reduce the errors. However, the surveillance of the high alert medication error rate should be further monitored and strategies to be continuously monitored for its effectiveness.
References
- Kenagy JW, Stein GC (2001) Naming, labeling and packaging of pharmaceuticals. Am J Health Syst Pharm 58: 2033-2041.
- Chadwick M (2003) Look-alike sound-alike health product names. Health Canada Workshop, Canada.
- Joint Commission on Accreditation of Healthcare Organizations (2001) High Alert Medication drug names. Sentinel Event Alert.
- ISMP Medication Safety Alert! Volume 1, Issue 17, August 28, 1996.
- ISMP Medication Safety Alert! Volume 3, Issue 12, June 17, 1998.
- ISMP Medication Safety Alert! Volume 6, Issue 21, October 17, 2001.
- The United States Food and Drug Administration. Medication errors.
- https://www.nccmerp.org/pdf/ indexBW2001-06-12.pdf.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences