Like a Prisoner in Azkaban: Medical Clearance of the Pediatric Psychiatric Patient
1Menninger Department of Psychiatry and Behavioral Sciences, Baylor College of Medicine, Houston, Texas, USA
2Section of Emergency Medicine, Baylor College of Medicine, Houston, Texas, USA
3Department of Emergency Medicine, Keck School of Medicine of USC, Los Angeles, CA, USA
4Section of Emergency Medicine, Baylor College of Medicine, 1504 Taub Loop, Houston, Texas, USA
- *Corresponding Author:
- Veronica Tucci
MD, JD
Assistant Professor Section of Emergency Medicine, Baylor College of Medicine
1504 Taub Loop, Houston, Texas, 77030 USA.
Tel: 713-873-7045
Fax: 713-873-2325
E-mail: vtuccimd@gmail.com
Received date: March 14, 2016; Accepted date: April 29, 2016; Published date: May 06, 2016
Citation: Onigu-Otite E, Oyebadejo AO, Moukaddam N, et al. Like a Prisoner in Azkaban: Medical Clearance of the Pediatric Psychiatric Patient. Pediatr Emerg Care Med Open Access. 2016, 1:1.
Abstract
Patients presenting with behavioral and psychiatric emergencies represent over 7% of all pediatric Emergency Department (ED) visits. Emergency personnel provide not only acute crisis intervention and stabilization but are tasked with “medically clearing” these children and adolescents for inpatient treatment. As will be discussed in this review article, the goal of medical clearance is to ensure that the patient’s condition is caused by true psychological pathology as opposed to underlying medical problems and that these patients may be safely be transferred to inpatient facilities. The extent of laboratory and ancillary testing is hotly debated and the process as a whole is crippled by the lack of interdisciplinary consensus between emergency physicians, pediatricians as well as emergency and inpatient psychiatrists. This article proposes an algorithm to help guide the process of medical clearance of the pediatric psychiatric patient.
Keywords
Pediatric medical clearance; Medical screening; Medical stability; Psychiatric; Behavioral emergencies in children and adolescents
Introduction
“You can exist without your soul, you know, as long as your brain and heart are still working. But you’ll have no sense of self anymore, no memory, no anything. There’s no chance at all of recovery. You’ll just-exist. As an empty shell. And your soul is gone forever lost.” Harry Potter and the Prisoner of Azkaban. Fans of the Harry Potter series know that the teenage protagonist’s most diabolical adversary is not one of his childhood bullies, Draco or Dudley. Nor is it his seemingly nasty (but ultimately, complicated) professor, Severus Snape. Nor is it even his archnemesis and the embodiment of evil, Lord Voldemort. Rather, when his truest fears are revealed, it is the Dementor that appears to torment Harry. Teaching him how to conjure the patronus charm, while watching him fail time and time again, is a difficult task for his friend and teacher, Professor Lupin. Too bad chocolate cannot aid in our patients’ recovery from real life “dementor” attacks. Indeed, the struggle is real, the road to recovery often long and unfortunately, it is not paved with Twix or Snickers bars. Without access to such a powerful and immediate treatment, emergency physicians (EPs) and psychiatrists must whip out their magic stethoscopes and medically evaluate and clear these patients for admission to inpatient psychiatric facilities for treatment and stabilization and in the process, emergency providers must not become casualties themselves to the “demented” medical clearance process. Once on the wards, the inpatient psychiatry team can guide the patient in their application of the “patronus charm” and help the patient combat their Dementor.
According to the National Comorbidity Study-Adolescent Supplement (NCS-A), 22% of all children and adolescents in the United States will meet criteria for a mental health disorder with severe enough distress or impairment to warrant emergent intervention during the course of their lifetime [1]. Moreover, regardless of the need for crisis intervention, a total of 51% of children and adolescents will satisfy the DSM-IV criteria for a mood, anxiety, behavioral, eating or substance abuse disorders across their lifetime and a striking 40% of youth involved in the NCS-A study reported more than one lifetime disorder (i.e., concomitant depression and anxiety) [1]. The prevalence of crippling behavioral and psychiatric illness is indeed higher than many common childhood illnesses, e.g., asthma and insulindependent diabetes, which garner substantially more attention and public resources. The World Health Organization has also estimated that by 2020, neuropsychiatric disorders will be one of the top 5 causes of morbidity, mortality, and disability for children. The scope of the problem in the United States is best captured by the Center for Disease Control’s own statistics where suicide is now the third leading cause of death among adolescents aged 10-14, the second among persons aged 15-34 years. Additionally, among students in grades 9-12 in the U.S. during 2013: 17.0% of students seriously considered attempting suicide in the previous 12 months, 13.6% of students made a plan about how they would attempt suicide in the previous 12 months, 8.0% of students attempted suicide one or more times in the previous 12 months and 2.7% of students made a suicide attempt that resulted in an injury, poisoning, or an overdose that required medical attention [2].
More than 13 million children require mental health or substance abuse service annually. It is, therefore, unsurprising that as the gatekeeper to crisis intervention services, EPs are seeing an increasing demand for pediatric mental health services and psychiatric emergencies now represent over 7.2% of all pediatric Emergency Department (ED) visits [3,4]. Data reviewed from 2002 to 2006 on 16,154 presentations by 12,589 pediatric patients (≤17 years old) showed that among children and adolescents who presented to the ED for mental health concerns, being female, older in age, receiving social assistance, and having an initial visit for a mood disorder or psychotic-related illness were associated with return for further care [5]. 6.1 and 8.7% of patients diagnosed with a mood disorder and psychotic-related illness, respectively, returned to the ED within 72 hours of discharge. 28.5% of patient with a mood disorder and 36.6% of those with a psychotic-related illness returned to the ED during the study period [5]. In 2014, Pittsenbarger and Mannix noted an increase in psychiatric ED visits for uninsured and publicly insured children and adolescents between 2001 and 2010. The authors recognize uncertainty as to whether this trend is caused by an increased prevalence of disease, an increased severity and/or a lack of outpatient resources [6]. Although many providers expect the Affordable Care Act to reduce the number of uninsured pediatric psychiatric patients coming to the ED, as of this publication, there is no data supporting this belief. Additionally, although the rates of psychiatric visits for underinsured pediatric patients have increased, the rates of admission or transfer from EDs for pediatric psychiatric diagnoses have not increased considerably, including for the underinsured [7]. Similarly, there was no rise in the number of pediatric patients with psychoses and suicide attempts -two categories of diagnoses generally seen in EDswhich suggests that the overall increase in pediatric mental health ED visits may have been due to non-urgent mental health conditions [7].
Pediatric psychiatric emergencies
The American Psychiatric Association (APA) defines a psychiatric emergency as "an acute disturbance in thought, behavior, mood, or social relationship, which requires immediate intervention as defined by the patient, family, or social unit" [8]. This classification embraces both functional and organic disease processes, which are separate but often intertwined. Thus, distinguishing both processes often a challenge. Psychiatric emergencies in the pediatric population differ from those in adults in several important ways. They often occur within the context of a crisis such as with patients’ families, homes, schools, peers, and other social systems [9,10].
In recent decades, there has been a nationwide decrease in mental health services which has led to increased burden on the ED to manage mental health crises. EDs are increasingly serving as the safety net for underserved pediatric patients who have mental health issues. A comprehensive emergency psychiatric evaluation may take several hours or longer to complete. The ED is rarely an optimal setting for assessing the patient while attending to patient and family anxiety. Moreover, obtaining a psychiatry consult can result in extended lengths of stay and prolonged stays may be more detrimental to pediatric than adult patients. Despite the potential harm of extended stays, inpatient and outpatient mental health treatment resources are limited, especially for pediatric patients, requiring EDs to hold pediatric psychiatric patients for prolonged, resource intensive periods of time [7,11]. Compared to other ED visits, pediatric mental health visits were more likely to arrive by ambulance, be triaged to rapid evaluation, and be admitted or transferred. Patients were almost twice as likely to have a length of stay over four hours for mental health visits as for other visits. This extended stay was not explained by observed differences in evaluation, treatment or disposition. Among mental health visits, patient age 6 to 13 years, intentional self-injury, ordering of laboratory studies, patient transfer, and metropolitan hospital location all predicted extended stays. Lengths of stay also increased over the study periods [11-13].
Medical clearance
“Medical clearance” is a term used to refer to the medical evaluation of patients whose symptoms seem to be psychiatric in origin. The ambiguity of this term [14] is only magnified in the pediatric patient population. Unfortunately, there is no interdisciplinary agreement regarding the standards for medical clearance of the emergency pediatric psychiatric patient. None of the member organizations for providers who routinely treat pediatric patients with psychiatric problems and crisis including the American College of Emergency Physicians (ACEP), the APA, The American Association of Emergency Psychiatry (AAEP) and the American Academy of Pediatrics (AAP) have a policy addressing medical clearance of the pediatric psychiatric patient. Indeed, ACEP’s policy specifically excludes the pediatric population from its recommendations on medical clearance of psychiatric patients.
Despite the lack of interdisciplinary consensus, the goal of medical clearance is to determine if psychiatric symptoms are due to a medical illness or substance use, and importantly, to assess and treat any medical illness requiring acute intervention [14]. Specifically, the objective of medical clearance is to determine that within reasonable medical certainty, there is no known contributory medical cause for the patient's presenting psychiatric complaints that requires acute intervention or that represents a medical emergency and that the patient is stable enough for the transfer to the intended dispositional setting (e.g., a general or psychiatric hospital, outpatient treatment setting or no follow up treatment) [15]. The medical assessment of the psychiatric patient involves a comprehensive history, a physical and mental status examination, and, when indicated, ancillary testing [16]. Notably, medical clearance does not guarantee the absence of ongoing medical issues, which may necessitate further diagnostic evaluation, monitoring and treatment. Likewise, it does not guarantee that there are no undiagnosed medical conditions.
Clinical evaluation
Providers should perform a comprehensive history and physical examination to identify any organic etiologies for the patient’s presentation and ascertain whether the patient’s symptoms and/or behavior poses or reveals a medical threat (e.g., a toxic ingestion or head trauma) that must be addressed during their ED stay [17-19]. The distinction of functional versus organic etiology is imperative, as the latter is often reversible, and failure to diagnose an organic etiology may be catastrophic. Table 1 provides historic elements that may help distinguish organic from psychiatric disorders.
| Organic | Functional |
|---|---|
| Age <13a or >40 without previous psychiatric diagnosis | Previous psychiatric diagnosis, Age >13 and<40 years (peak onset 15-30 years) |
| Rapid onset and progression of symptoms | Insidious development of symptoms |
| Visual or tactile hallucinations | Auditory hallucinations |
| History of substance abuse | No history of substance abuse |
| New medications or changes in medication dose | No new medications NOR medication dosage changes |
| Seizures | No seizures |
| No family history of psychiatric disorders | Family history of psychiatric disorderb |
aOnset of primary psychotic disorders including very early onset schizophrenia prior to age 13 is quite rare, typically 1 per 40,000. Onset of primary psychotic disorders prior to age 18 typically occurs 1 per 10,000; b5-20 times higher rate in first degree relatives of patients with psychiatric disorders compared to the general public (up to 60% concordance in monozygotic twins)
Table 1: Historical features distinguishing organic causes of psychiatric complaints from functional pathology.
Physicians should have a low threshold to evaluate for selfinjurious behavior [18]. Prior psychiatric history is important to identify. However, the presence of a psychiatric diagnosis does not preclude an organic cause of the patient’s current symptoms and presentation [20,21].
History
The history should include a detailed description of recent symptoms and behavior changes. Although this history may be provided by the patient, an attempt should also be made to get collateral information from as many sources as possible including the family, friends, care providers, EMS providers and police. These additional sources can provide a baseline for the patient’s symptoms and confirm the story (especially if the patient’s mental capacity is impaired or not known). This information is also helpful if the patient is unable or unwilling to provide a history. A sudden change in behavior in a patient without a psychiatric history or abrupt deterioration in a patient with an underlying psychiatric disorder should prompt a search for underlying organic etiology [22-25]. The Brief Psychiatric Rating Scale for Children (BPRS-C) and the Prodromal Questionnaire Brief Version (PQ-B) could be considered in screening for psychotic symptoms [26,27].
Medical problems presenting as psychiatric complaints
Throughout history, vague and unusual symptoms have been attributed by physicians to psychiatric conditions, but later revealed to be due to organic disease. King George the III’s “insanity” was, in fact, a classic case of porphyria [28]. It is essential for EPs to be cognizant of these psychiatric mimics. An exceptional number of medical etiologies may present with psychiatric complaints or exacerbate symptoms of previously diagnosed psychiatric problems.
Table 2 providers a list of organic diseases that may masquerade as psychiatric disorders. This list is not meant to be comprehensive but rather to provide examples to the busy EP.
| System-Category | Medical Conditions |
|---|---|
| Autoimmune Disorders: | Anti-NMDA Receptor Encephalitis, Multiple Sclerosis, Myasthenia Gravis, Systemic Lupus Erythematosus |
| CNS Diseases: | Chronic Traumatic Encephalopathy (CTE), Seizures (e.g., Temporal Lobe Epilepsy), Space-Occupying Lesions, Traumatic Brain Injury |
| Electrolyte Derangement: | Hypercalcemia |
| Endocrine Disorders: | Addison’s Disease, Diabetic Ketoacidosis, Hyperthyroidism, Hypothyroidism (including Myxedema Coma), Hypoglycemia, Insulinoma, Panhypopituitarism, Pheochromocytoma |
| Environmental: | Hypothermia, Hyperthermia |
| Hematologic Disorders: | Thrombotic Thrombocytopenic Purpura, Porphyria |
| Hereditary Metabolic Disorders: | Niemann-Pick Type C, Tay-Sachs Disease (late onset forms), Urea Cycle Disorders, Wilson’s Disease |
| Infectious Disorders: | Cerebral Malaria, Herpes Encephalitis, Cryptococcal Meningitis, Neurocysticerosis, Neurosyphillis, Sepsis, HIV |
| Medication-Induced Symptoms/Side Effects/Withdrawal: | Antipsychotic Medications, Anxiolytics, Benzodiazepines, Over-the-counter Medications such as Dextromethorphan, Prescription Pain Medications, Psychostimulants, Iatrogenic steroids, withdrawal syndromes including delirium tremens |
| Metabolic Disorders: | Hepatic Encephalopathy, Paraneoplastic Syndromes, Uremia |
| Nutritional Deficiencies: | Vitamin B-12, Wernicke’s Encephalitis and Korsakoff Syndrome |
| Poisonings: | Botulism, Carbon Monoxide, Heavy Metals |
| Substance Use/Intoxication: | Anabolic Steroid Abuse, Alcohol Use or Intoxication, Cannabis Use, Cocaine Use/Intoxication, Hallucinogen use, Inhalant abuse, Synthetic Cannabis Use, Synthetic Cathinones (bath salts), etc. |
Table 2: Organic conditions masquerading as psychiatric pathology.
Table 3 also provides a list of comorbid and confounding conditions seen in pediatric patients presenting with psychiatric and behavioral disturbances.
| Autism Spectrum Disorder |
|---|
| Intellectual Disability |
| Other Neurodevelopmental Disorders (e.g., global developmental delay, prenatal alcohol or drug exposure) |
| Speech and Language Disability |
| Substance Use or Abuse |
| Trauma and Stressor-Related Disorders (e.g., adjustment, reactive attachment, or post-traumatic stress disorders) |
Table 3: Comorbid and confounding conditions in the pediatric population.
Physical examination findings
As with all ED patients, vital signs are VITAL. It is often difficult to obtain vital signs in a combative patient. However, accurate vital signs are essential for triaging and stabilizing pediatric psychiatric patients because any abnormality may reflect a serious underlying medical etiology (e.g., toxidrome).
Patients who are acutely intoxicated, disoriented or who have self-inflicted injuries should have a thorough and detailed physical examination. In the absence of altered mental status or a history concerning for trauma or ingestion, the extent of the physical examination in the ED will be dictated by the patient’s chief complaint, history and review of systems. As a general rule, providers should perform a focused physical examination of pediatric patients to identify whether there is a medical condition that is causing or exacerbating the patient’s symptoms, or diagnoses that may need treatment or special care (e.g., G tube) that cannot be managed in an inpatient psychiatric setting. The limitations of inpatient psychiatric facilities in managing complex or labor intensive co-morbid medical conditions are generally included in each facility’s exclusionary criteria and such exclusions are separate from the process of medical clearance or stability and beyond the scope of this article. Tables 4 and 5 provide several examples of physical examination findings suggestive of organic etiologies and which may help the EP differentiate functional from psychiatric pathology.
| Organ System | Physical Sign and Possible Pathology |
|---|---|
| Head | Battle Sign concerning for skull fracture |
| Eye | Nystagmus concerning for intoxication or CNS pathology; Raccoon eyes concerning for head trauma; Kayser-Fleischer ring concerning for Wilson’s disease |
| Neck | Thyroid enlargement concerning for thyroid storm; +Brudnizki or Kernig Signs concerning for meningitis |
| Cardiovascular | Tachycardia concerning for acute intoxication or withdrawal; Rub concerning for pericardial effusion concerning for lupus |
| Pulmonary | Tachypnea concerning for hypoxia or an underlying acidosis |
| Abdomen | Guarding concerning for obstruction or intussusception; Ascites/anasarca concerning for liver pathology |
| Extremity | Edema suggestive of liver or renal pathology |
| Skin | Petechiae concerning for meningitis or thrombotic thrombocytopenic purpura; Jaundice concerning for liver failure; Rash in a butterfly distribution concerning for lupus |
| Neuro | Cranial nerve abnormalities concerning for stroke, encephalitis, meningitis, space-occupying lesion; Gait abnormalities concerning for nutritional deficiencies |
Table 4: Physical examination signs suggestive of underlying organic pathology.
| Organic/Functional | Psychiatric |
|---|---|
| Abnormal Vital Signs | Normal Vital Signs |
| Fluctuating Level of Consciousness | Consistent Level of Consciousness |
| Focal Neurological Findings | Normal Neurologic Examination |
| Evidence of Trauma (e.g., raccoon eyes, Battle Sign) | No evidence of Trauma |
| Abnormal Dermatologic Manifestations (e.g., rashes, purpura, jaundice) | No skin changes |
| Abnormal Mini-Mental Examination or Quick Confusion Scale | Normal Mini-mental or Quick Confusion Scale Examination |
Table 5: Comparison of physical examination features distinguishing organic causes of psychiatric complaints from primary psychological or functional pathology.
Deficiencies in the ED assessment
Although there are no studies that specifically address the quality of the physical examination in pediatric psychiatric population performed by emergency providers, multiple studies have questioned the thoroughness and accuracy of history taking and physical examinations performed and documented in the adult arena. Table 6 provides examples of poor documentation practices in pediatric populations.
| Past Medical History | Failure to confirm patient’s past medical and psychiatric history including any suicide attempts and inpatient hospitalizations |
| Past Surgical History | Failure to document the patient’s past surgical history, which may impact presentation (e.g., VP shunt, pituitary adenoma resection) |
| Family history | Failure to document hereditary diseases (e.g., Wilson’s disease, pernicious anemia) and psychiatric conditions with high first degree relative prevalence |
| Medication history | Failure to document medications including over the counter and herbal medications and any changes in dose |
| History of Present Illness | Failure to take a detailed history leading to present ED visit |
| Review of systems | Failure to conduct a review of systems to capture items that the patient may not attribute as being related to current condition |
| Physical Examination | Failure to address abnormal vital signs and get a complete set (including temperature) Failure to document cardiopulmonary status Failure to perform a basic abdominal examination Failure to perform an examination of the skin Failure to perform an adequate neurologic exam (e.g. Alert and oriented status, cranial nerve exam, gait, strength, sensation) Failure to perform a psychiatric exam |
Table 6: Poor history and physical examination documentation.
Inaccurate history and physical examinations lead to missed and delayed diagnoses directly impacting patient safety because most inpatient psychiatric facilities have limited capabilities to diagnose or manage many urgent and emergent medical conditions. Poor history and physical examinations also lead to an increased reliance on laboratory testing and imaging, increasing the cost of the medical evaluation as well as the length of stay of the patient in the ED.
Interestingly, one study actually found that younger psychiatric patients had a greater chance of a missed medical diagnosis. The authors theorized that providers erroneously assumed that younger patients were healthier with less co-morbidities at baseline and consequently, they did not need to perform as comprehensive of a medical assessment as they did in older patients [29].
Ancillary testing
Laboratory testing of pediatric psychiatry patients presenting in acute care settings differ by hospital and is often driven by accepting psychiatric facilities. The necessity of ancillary investigations including laboratory and radiological tests is often a point of disagreement among interdisciplinary teams involved in pediatric psychiatry patient care in emergency settings [30]. In Zun’s study, 507 EPs and 65 psychiatrists in Illinois were surveyed about use of ancillary testing in the medical clearance of psychiatric patients. Physicians could select tests that were routinely performed in their practice and those that were required for all medical clearances. The investigators found that psychiatrists and EPs required similar testing. However, routine testing varied between EPs and psychiatrists, signifying that there is a difference in the approach to the patient. The most common routinely ordered and always required tests by both EPs and psychiatrists were a urine drug screen, alcohol level, and complete blood count. Of possible medical clearance tests, electroencephalograms, computed tomography scans, and lumbar punctures were least commonly ordered. The estimated cost of required testing was $101 to $200 for EPs and $201 to $300 for psychiatrists [31].
Donofrio’s study, in one pediatric emergency department of 1082 psychiatric visits including 871 with screening laboratory examinations, found that no patient had an organic etiology of their symptoms diagnosed based only on the results of the screening laboratory examinations [32]. Moreover, the only disposition change based solely on a screening test was that a patient found to have a positive pregnancy test was admitted to a medical ward rather than transferred to a psychiatric hospital. No patient had an urgent management change based only on the laboratory screening process. Twenty-five patients with non-contributory history and physical exams had non-urgent management changes, such as treatment of anemia, based on their test results. The investigators suggested development of guidelines limiting recommended ancillary testing in pediatric psychiatric patients to those tests indicated based on history and physical exam. The authors did suggest that routine pregnancy testing may be beneficial in postpubertal females to guide psychotropic medication selection.
Santiago’s study of 210 pediatric ED patients who required psychiatric evaluation also found that screening laboratories were of low yield, with no non-medically indicated test altering acute patient management [11]. In the 54 patients who had non-medically indicated laboratories done at the request of psychiatry for the purpose of admission or transfer, the only abnormal laboratories were 1 abnormal complete blood count, 2 abnormal transaminases, 1 positive urine drug screen (UDS) and 1 abnormal urinalysis.
UDSs can be useful in detecting the presence of substances which may contribute to behavioral emergencies. However, no nationally representative studies are available on the utility of routine urine drug testing in pediatric psychiatry emergency patients. Several studies demonstrate significant concordance of patient-disclosed substance use and UDS results. UDS sensitivity is relatively low (49.09%), but specificity is high (96.95%) [33,34]. In Fortu’s retrospective study of 652 8-17 year olds presenting to the ED, medically indicated and routine-driven UDSs were studied [35]. Patients presenting with seizures, altered mental status, syncope, headache, ingestion, chest pain/palpitation, shortness of breath, sexual assault, or those brought in for motor vehicle accident (MVA) were considered to have medically indicated UDSs. Patients who presented with aggression, out-ofcontrol behavior, intentional self-inflicted wounds, or symptoms of depression without evidence of drug or alcohol ingestion or altered mental status were considered to have routine-driven UDSs. Routine-driven UDSs contributed no additional information and did not impact immediate management leading the authors to conclude that pediatric patients with straightforward psychiatric complaints may be medically cleared without a UDS. Furthermore, adolescent drug users may ingest substances to mask identification of their drug use [36].
Psychiatric patients are often brought to EDs for medical clearance prior to being transferred to inpatient psychiatry units. There are no nationally representative studies of pediatric mental health patients evaluated in EDs for medical clearance. A retrospective study of 789 pediatric psychiatric patients evaluated in one pediatric ED for medical clearance after being placed on an involuntary psychiatric hold in a pre-hospital setting concluded that 72 (9.1%) required medical screening. The charges for laboratory tests, secondary ambulance transfers and sitter wages for the 789 patients were $1,241,295, or US$17,240 per patient determined to require a medical screen. The median charge for blood and urine testing per patient screened was $1,235. The investigators suggested the application of basic criteria in the pre-hospital setting (unrelated medical complaint, altered mental status, ingestion, hanging, traumatic injury, rape) to determine which patients required transport to an ED rather than a psychiatric facility in order to decrease health care costs [32].
Psychotropic medications are increasingly prescribed for pediatric mental health conditions [37-40]. There is evidence that psychotropic medications are prescribed more often in underinsured patients, a population which accounts for disproportionate number of ED mental health visits [41,42]. Pediatric patients on multiple medications are at greater risk of drug-drug and drug-disease interactions. Children with complex chronic conditions have an increased risk of ED visits associated with adverse drug events, when compared to children without chronic conditions, including mental health conditions. Those taking psychotropic agents are among the groups with the highest rates of ED visits [39,40,43,44].
Moreover, the total number of potential adverse effects was positively predicted by the number of DSM-IV categories diagnosed, and by the presence of impulsivity and oppositionality [43]. 50-75% of pediatric medication use has been estimated to be off-label [45]. Off-label use raises the degree of uncertainty regarding a drug's safety [45]. Patients can present with sedation, confusion, cardiovascular dysfunction, and metabolic derangements. Assessment and management of these presentations requires an index of suspicion, an attentive symptom and medication history, physical examination, and targeted interventions [46].
Historically, the use of pemoline highlights the challenges of drug safety in youth. Pemoline, a medication that had been used to treat ADHD and narcolepsy, was pulled by the FDA after children taking the medication started developing liver failure [47,48]. Psychiatric adverse drug experiences with certain drugs are more prominent in children, often resulting in new psychiatric symptoms [49,50]. For example, psychiatric symptoms including disturbance in attention, disorientation, memory impairment, depression, irritability, hostility, agitation, aggression, anxiousness, dream abnormalities, hallucinations, insomnia, restlessness, suicidal thinking and behavior and tremor have been noted with leukotriene inhibitors [51]. Resulting in an FDA black box warning. Suicidal behaviors and depressed mood have been also reported with isotretinoin. It is critical for acute care practitioners to be aware of the psychopharmacology and side effects of medications used to treat pediatric patients, including on- and off-label use.
Conclusion
Best practice in medical clearance of pediatric patients with mental health emergencies is controversial. AAEP, AAP, ACEP and the APA all advocate for increased mental health resources, improved pediatric mental health tools for the ED, increased mental health insurance coverage, adequate reimbursement at all levels, endorsement of education and research for mental health emergencies, and acknowledgment of the importance of the child's medical home. Unfortunately, despite such advocacy, there is no interdisciplinary agreement with respect to the requirements for medical clearance of pediatric psychiatric patient [52,53].
Several solutions have been suggested to address the challenges of treating patients with psychiatric complaints in medical EDs including employment of mental health screening and specialized care models to reduce hospitalization, return ED visits, and length of ED stay [34,54,55]. These promising potential solutions require further investigation. Health care systems and individual medical centers should strive for multidisciplinary collaboration to improve the continuum of care, promote improved identification of children and adolescents with mental health disorders, and promote early recognition and intervention, which are key to effective referral and treatment [56]. The actions and directions taken in the ED are a vital part of the child's treatment and longterm care [56]. Each pediatric patient encounter, including visits and management in acute care settings for mental health visits should be viewed as a point of care within the larger continuum of patient care. Although the use of the ED as a gateway to mental health treatment is suboptimal, it is the reality in many hospitals [57-60].
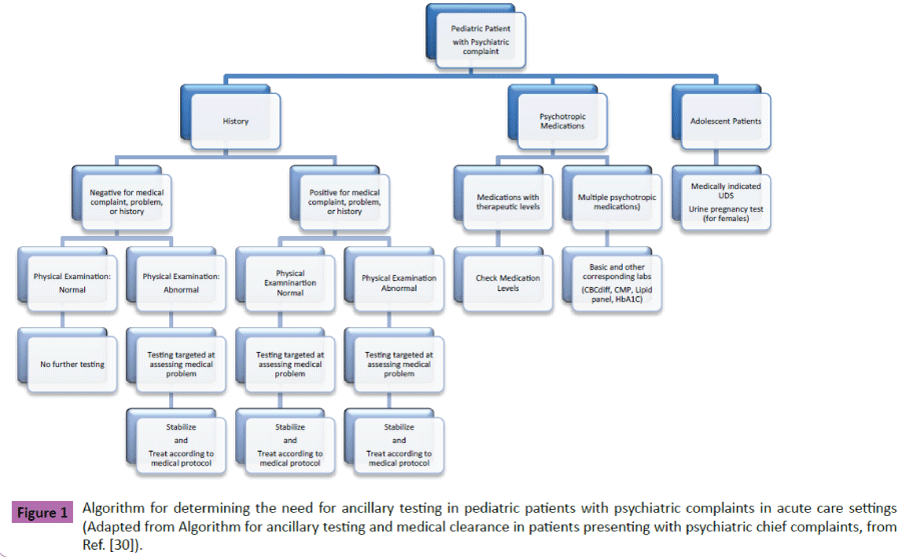
Given that EDs are currently tasked with the medical clearance of pediatric patients with psychiatric complaints, EPs must ensure the best possible care for all patients presenting for care. Pediatric patients presenting to the ED with mental health complaints sometimes have underlying medical conditions contributing to their symptoms. Missing the diagnosis of underlying medical conditions, adverse medication effect(s) or misdiagnosing a medical illness as psychiatric in origin can be catastrophic. A comprehensive history and physical examination are fundamental to identifying underlying medical conditions. Based on the available evidence, laboratory and ancillary testing should be ordered as indicated based on clinical assessment. In Figure 1, we propose an algorithm to guide clinicians in performing medical clearance examinations of pediatric patients with psychiatric complaints. In the future, guidelines from organizations such as AAEP, AAP, ACEP and APA are needed to further improve the medical care of pediatric patients with mental health complaints.
References
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevol S, et al. (2010) Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). J AmAcadChild Adolesc Psychiatry 49: 980-989.
- Centers for Disease Control and Prevention (CDC) & National Center for Injury Prevention and Control (2015) Suicide Facts at a Glance 2015.
- Lynch S, Bautista M, Freer C, Kalynych C, Hendry P (2015) Child Mental Health Services in the Emergency Department: Disparities in Access. PediatrEmergCare 31: 473-478.
- Hoyle JD, White L J (2003) Pediatric mental health emergencies: summary of a multidisciplinary panel. PrehospEmergCare 7: 60-65.
- Newton AS, Ali S, Johnson DW, Haines C, Rosychuk RJ, et al. (2010) Who comes back? Characteristics and predictors of return to emergency department services for pediatric mental health care. AcadEmergMed 17: 177-186.
- Pittsenbarger ZE,Mannix R (2014) Trends in pediatric visits to the emergency department for psychiatric illnesses. AcadEmerg Med21: 25-30.
- Sills MR, Bland SD (2002) Summary statistics for pediatric psychiatric visits to US emergency departments, 1993-1999. Pediatrics 110:40.
- Allen MH,EalZJ (2002) APA task force on psychiatric emergency services: report and recommendations regarding psychiatric emergency and crisis services. American Psychiatric Association,pp:1-100.
- Horowitz LM, Bridge JA, Pao M, Boudreaux ED (2014) Screening youth for suicide risk in medical settings: time to ask questions.AmJPrevMed47: 170-175.
- Pon N, Asan B, Anandan S, Toledo A (2015) Special Considerations in Pediatric Psychiatric Populations. EmergMedClinNorth Am 33: 811-824.
- Santiago LI, Tunik MG, Foltin GL, Mojica MA (2006) Children requiring psychiatric consultation in the pediatric emergency department: epidemiology, resource utilization, and complications. PediatrEmergCare 22: 85-89.
- Case SD, Case BG, Olfson M, Linakis JG, Laska EM (2011) Length of stay of pediatric mental health emergency department visits in the United States. JAmAcadChild AdolescPsychiatry 50: 1110-1119.
- Alpern ER, Stanley RM, Gorelick MH, Donaldson A, Knight S, et al. (2006) Epidemiology of a pediatric emergency medicine research network: the PECARN Core Data Project. PediatrEmerg Care 22: 689-699.
- Weissberg MP (1979) Emergency room medical clearance: an educational problem. AmJPsychiatry 136: 787-790.
- Zibulewsky J (2001) The Emergency Medical Treatment and Active Labor Act (EMTALA): what it is and what it means for physicians Proc. BaylUniv MedCent 14: 339-346.
- Zun LS (2005) Evidence-based evaluation of psychiatric patients. JEmergMed28: 35-39.
- Larkin GL, Smith RP, Beautrais AL (2008) Trends in US emergency department visits for suicide attempts, 1992-2001. Crisis 29: 73-80.
- Riba M, Hale M (1990) Medical clearance: fact or fiction in the hospital emergency room. Psychosomatics 31: 400-404.
- Shah SJ, Fiorito M, McNamara RM (2012) A screening tool to medically clear psychiatric patients in the emergency department. JEmergMed 43: 871-875.
- Baca CB, Vickrey BG, Caplan R, Vassar SD, Berg AT (2011) Psychiatric and medical comorbidity and quality of life outcomes in childhood-onset epilepsy. Pediatrics 128:1532-1543.
- Spady DW, Schopflocher DP, Svenson LW, Thompson AH (2005) Medical and psychiatric comorbidity and health care use among children 6 to 17 years old. ArchPediatrAdolescMed 159: 231-237.
- Cummings M, Berkowitz SJ, Scribano PV (2012) Treatment of childhood sexual abuse: an updated review. CurrPsychiatry Rep 14: 599-607.
- OlshakerJS, Browne B, Jerrard DA, Prendergast H, Stair TO (1997) Medical clearance and screening of psychiatric patients in the emergency department.AcadEmerg Med 4: 124-128.
- Irons MJ, Farace E, Brady WJ, Huff JS (2002) Mental status screening of emergency department patients: normative study of the quick confusion scale. AcadEmerg Med 9: 989-994.
- Kara S (2002) Behavioral emergencies: Differentiating medical from psychiatric disease. Emerg Med Pract 4: 1-20.
- Avalon Social Services (2016) Avalon Social Services Brief Psychiatric Rating Scale for Children (BPRS-C).
- Loewy RL, Pearson R, Vinogradov S, Bearden CE, Cannon TD (2011) Psychosis risk screening with the Prodromal Questionnaire-brief version (PQ-B). SchizophrRes 129: 42-46.
- Macalpine I, Hunter R (1966) The "insanity" of King George 3d: a classic case of porphyria. BrMed J 1: 65-71.
- Tintinalli JE, Peacock FW, Wright MA (1994) Emergency medical evaluation of psychiatric patients. AnnEmerg Med 23: 859-862.
- Tucci V, Siever K, Matorin A, Moukaddam N (2015) Down the Rabbit Hole: Emergency Department Medical Clearance of Patients with Psychiatric or Behavioral Emergencies. EmergMedClinNorth Am 33: 721-737.
- Zun LS, Hernandez R, Thompson R, Downey L (2004) Comparison of EPs' and psychiatrists' laboratory assessment of psychiatric patients. AmJEmergMed 22: 175-180.
- Donofrio JJ, Santillanes G, McCammack BD, LamCN, Menchine MD, et al. (2014) Clinical utility of screening laboratory tests in pediatric psychiatric patients presenting to the emergency department for medical clearance. AnnEmergMed63: 666-675.
- Shihabuddin BS, Hack CM, Sivitz AB (2013) Role of urine drug screening in the medical clearance of pediatric psychiatric patients: is there one? PediatrEmerg Care 29: 903-906.
- Hamm MP, Osmond M, Curran J, Scott S, Ali S, et al. (2010) A systematic review of crisis interventions used in the emergency department: recommendations for pediatric care and research. PediatrEmergCare 26: 952-962.
- Fortu JM, Kim IK, Cooper A, Condra C, Lorenz DJ(2009) Psychiatric patients in the pediatric emergency department undergoing routine urine toxicology screens for medical clearance: results and use. PediatrEmerg Care 25: 387-392.
- Arcinegas-Rodriguez S, Gaspers MG, Lowe MC (2011) Metabolic acidosis, hypoglycemia, and severe myalgias: an attempt to mask urine drug screen results. PediatrEmerg Care 27: 315-317.
- Olfson M, Marcus SC, Weissman MM, Jensen PS (2002) National trends in the use of psychotropic medications by children. J AmAcadChild AdolescPsychiatry 41: 514-521.
- Bhatara V, Feil M, Hoagwood K, Vitiello B, Zima B (2004) National trends in concomitant psychotropic medication with stimulants in pediatric visits: practice versus knowledge. J AttenDisord 7: 217-226.
- Zito JM, Safer DJ, dosReis S, Gardner JF, Magder L, et al. (2003) Psychotropic practice patterns for youth: a 10-year perspective. Arch PediatrAdolesc Med 157: 17-25.
- Dosreis S, Zito JM, Safer DJ, Gardner JF, Puccia KB (2005) Multiple psychotropic medication use for youths: a two-state comparison. JChild AdolescPsychopharmacol 15: 68-77.
- Martin A, Van HT, Stubbe D, Sherwin T, Scahill L (2003) Multiple psychotropic pharmacotherapy among child and adolescent enrollees in Connecticut Medicaid managed care. PsychiatrServ 54: 72-77.
- Martin A, Sherwin T, Stubbe D, Van HT, Scahill L (2002) Datapoints: use of multiple psychotropic drugs by Medicaid-insured and privately insured children. PsychiatrServ 53: 1508.
- Ninan A, Stewart SL, Theall LA, Katuwapitiya S,Kam C (2014) Adverse effects of psychotropic medications in children: predictive factors. JCanAcad Child AdolescPsychiatry 23: 218-225.
- McIntyre RS,Jerrell JM (2009) Polypharmacy in children and adolescents treated for major depressive disorder: a claims database study. JClinPsychiatry 70: 240-246.
- Zito JM, Derivan AT, Kratochvil CJ, Safer DJ, Fegert JM (2008) Off-label psychopharmacologic prescribing for children: history supports close clinical monitoring. Child AdolescPsychiatry MentHealth 2: 24.
- Rasimas JJ,Liebelt EL (2012) Adverse Effects and Toxicity of the Atypical Antipsychotics: What is Important for the Pediatric Emergency Medicine Practitioner. ClinPediatrEmergMed 13: 300-310.
- WHOPharmaceuticals Newsletter (2005) World Health Organization.
- Etwel FA, Rieder MJ, Bend JR, Koren G (2008) A surveillance method for the early identification of idiosyncratic adverse drug reactions. Drug Saf 31: 169-180.
- Drozdowicz LB,Bostwick JM (2014) Psychiatric adverse effects of pediatric corticosteroid use. Mayo ClinProc 89: 817-834.
- Glauser TA (2004) Effects of antiepileptic medications on psychiatric and behavioral comorbidities in children and adolescents with epilepsy. Epilepsy Behav 3: S25-S32.
- Philip G, Hustad C, Noonan G, Malice MP, Ezekowitz A, et al. (2009) Reports of suicidality in clinical trials of montelukast. JAllergy ClinImmunol 124: 691-696.
- Dolan MA, Mace SE (2006) Pediatric mental health emergencies in the emergency medical services system. AnnEmergMed 48: 484-486.
- Dolan MA, Fein JA (2011) Pediatric and adolescent mental health emergencies in the emergency medical services system. Pediatrics 127: e1356-e1366.
- Williams JR, Ho ML, Grupp-Phelan J (2011) The acceptability of mental health screening in a pediatric emergency department. PediatrEmergCare 27: 611-615.
- Grover P, Lee T (2013) Dedicated pediatric behavioral health unit: serving the unique and individual needs of children in behavioral health crisis. PediatrEmergCare 29: 200-202.
- Baren JM, Mace SE, Hendry PL, Dietrich AM, Grupp-Phelan J (2008) Children's mental health emergencies-part 1: challenges in care: definition of the problem, barriers to care, screening, advocacy, and resources. PediatrEmergCare 24: 399-408.
- Clemans-Cope L, Kenney G, Waidmann T, Huntress M, Anderson N (2015) How Well Is CHIP Addressing Health Care Access and Affordability for Children? AcadPediatr 15: S71-S77.
- Lukens TW, Wolf SJ, Edlow JA, Shahabuddin S, Allen MH, et al. (2006) Clinical policy: critical issues in the diagnosis and management of the adult psychiatric patient in the emergency department. AnnEmerg Med 47: 79-99.
- Murray CJ, Lopez AD, Jamison DT (1994) The global burden of disease in 1990: summary results, sensitivity analysis and future directions. BullWorld Health Organ 72: 495-509.
- Simon AE,Schoendorf KC (2014) Emergency department visits for mental health conditions among US children, 2001-2011. ClinPediatr(Phila) 53: 1359-1366.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences