Implementation of In-Patient Anticoagulation Service in Malaysia
Mohamed Sahimi*
Department of Pharmacy, International Islamic University Malaysia, Pahang, Malaysia
*Corresponding Author:
Sahimi M
Department of Pharmacy
International Islamic University Malaysia
Pahang, Malaysia
E-mail: sahimimohd@gmail.com
Received Date: August 24, 2020; Accepted Date: September 07, 2020; Published Date: September 14, 2020
Citation: Sahimi M (2020) Implementation of In-Patient Anticoagulation Service in Malaysia. J Pharma Prac Edu Vol.3 No.3:31.
Abstract
Background: Anticoagulants are extensively used in the in-patient setting for the prevention and treatment of Venous Thromboembolism (VTE) and stroke prevention for Atrial Fibrillation. They are high-risk medications associated with a significant rate of medication errors among hospitalized patients. The Pharmacy Department in collaboration with Medical Department in Hospital Tengku Ampuan Afzan (HTAA) is seeking to expand anticoagulation services and standardize care by implementing an In-Patient Anticoagulation Service (IPACs) providing daily surveillance and dosing consultation for patients receiving Anticoagulant Therapy (ACT). The team comprises of consultant hematologist, pharmacists, general physician and medical officers. The objectives of this study are to describe the implementation and outcomes of an IPACs and identifying the issues in the management of ACT. The use of anticoagulant was retrospectively collected from IPACs data during the period February 2017 to December 2018.
Results: 320 patients were referred to IPAC, with 59% of them were female. Of 303 patients seen by IPACs team, 52.5% patients used for acute VTE, 19.5% were referred for anticoagulant reversal and 3.3% for recurrent VTE. Almost two-third (72.3%) of patients used warfarin followed by 20.5% used direct oral anticoagulant and 7.2% used either low molecular weight or heparin. Of 159 patients referred for acute VTE, only 33% of them received VTE prophylaxis. Issues that were identified were the inappropriate dose of Vitamin K for over-warfarinization and underutilisation of prothrombin complex concentrate in the setting of prolonged International Normalized Ratio (INR) with severe bleeding as well as doing daily INR leading to improper titration of warfarin. Unsupervised and improper dose of heparin infusion and patients discharged with longer appointment for INR monitoring are the main issues encountered in IPACs.
Conclusion: With the IPACs, the awareness of VTE prophylaxis and the issues that related to ACT were resolved. This service appears to enhance quality of patient care in ACT.
Keywords
Anticoagulant therapy; In Patients AntiCoagulant Service (IPACS); Warfarin, Direct oral anticoagulant; Heparin
Background
Anticoagulants are extensively used for the prevention and treatment of Venous Thrombosis (VTE) and prevention of stroke in atrial fibrillation. However, anticoagulants are high risk medications associated with a significant rate of medication errors due to the complex dosing nature, insufficient monitoring and inconsistent patient compliance [1]. Medication error related to anticoagulant often cause serious or fatal events. In particular, when patients were transferred from in-patient to outpatient setting [2].
In the out-patient setting, pharmacist-managed anticoagulation has been shown to decrease bleeding and thromboembolic events, as well as increasing the likelihood of a therapeutic international normalized ratio (INR) for patients on warfarin [3]. In Malaysia, pharmacist-managed Warfarin Medication Therapy Adherence Clinic (W-MTAC) was started since 2005 and already implemented in all major hospitals since 2010 [4]. Currently the service has not been started in the in-patient setting. The implementation of in-patient anticoagulation services in hospitals has been proven to help patients achieve their INR [5]. Target or activated Partial Thromboplastin Time (aPTT) goal in a shorter amount of time and decrease critical INR values during titration of warfarin dosing [6,7].
Introduction and Description of the Service
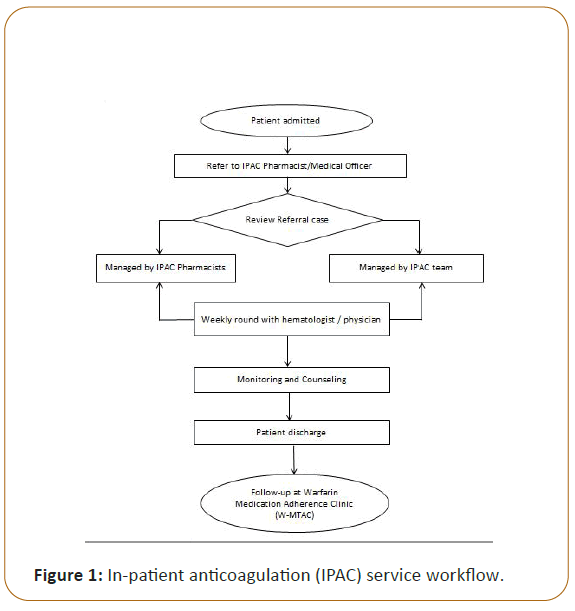
Hospital Tengku Ampuan Afzan (HTAA) is an 823-bed hospital and is one of major hospitals in Malaysia. The hospital's pharmacy department employs 108 full time pharmacists. W-MTAC was implemented in March 2008 and currently managing approximately 1050 patients. Pharmacistmanaged services were extended for consultations for in-patient anticoagulation management from February 2017. The In-Patient Anticoagulation Service (IPACs) served as one stop center for all departments in HTAA to standardize the practice of Anticoagulant Therapy (ACT) and provided consultative services for healthcare providers on anticoagulant management and related issues. The IPACs collaborated with consultant hematologist, general physician and medical officers. Seven IPACs pharmacists undergone two weeks of anticoagulant training program under Pharmaceutical Service Division (PSD) Ministry of Health (MOH) Malaysia. The training was conducted at training hospital and this is to assure all IPAC pharmacists have good competency in conducting ACT. To maintain the competency, they need to be credentialed by PSD MOH Malaysia. Patients who had problems and issues related with ACT were referred to the IPACs team through phone calls. The cases were reviewed by medical officer together with pharmacists and were discussed with consultant hematologist during grand ward round in weekly basis. Daily review was done by scheduled pharmacists to assess the accuracy of prescribed ACT (e.g., INR target based on indication, renal and liver functions, drug interactions, duration of ACT) (Figure 1). Due to manpower constraints, the IPACs were available only for working days from 8.00 am to 5.00 pm. Consultation through phone call can be made during weekends and public holidays.
Pharmacists also assess patients' eligibility for Direct Oral Anticoagulants (DOACs). Laboratory results were reviewed to ensure patients were closely monitored while they are on ACT. Patient newly started on anticoagulants will be counseled with related issues (e.g., INR target, dose, frequency, duration of treatment, side effects, adherence, drug and food interaction, signs and symptoms of bleeding) pertaining to ACT. Interventions and recommendations were documented in the standard clerking sheet. The cases were followed up until patients were discharged. Upon discharge, IPACs pharmacists ensure patients have proper follow up appointments at W-MTAC and the correct dose of anticoagulant as well as properly counseled regarding ACT. The objectives of this study are to define the implementation and outcomes of an IPACs and identifying the issues in the management of ACT.
Materials and Methods
As part of a Clinical pharmacy to improve the management of ACT, an IPACs comprising a pharmacist’s daily advice on ACT for in-patients, was started in HTAA. This was a single-center cohort study. In-patient hospitalization data for patients treated with ACT, which referred to IPACs between February 1, 2017, and December 31, 2018, were retrospectively evaluated. Before the implementation of the IPACs, the standard management cohort was managed separately by each department. Anticoagulation such as warfarin and heparin dosing were based on the doctors’ experience without any nomograms or standard dosing guidelines.
Results
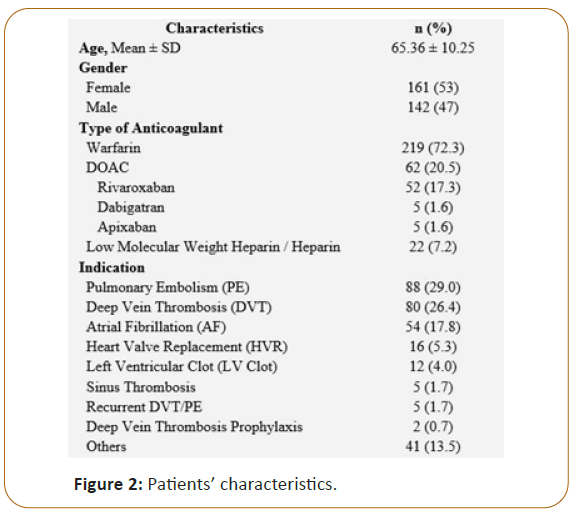
This study was approved by NMMR ethic committee. Total number of 303 cases were reviewed with 53% were female. Almost two-third (72.3%) of patients used warfarin followed by 20.6% used DOACs and 7.2% used either low molecular weight (LMWH) or heparin. The patient’s characteristics are described in Figure 2.
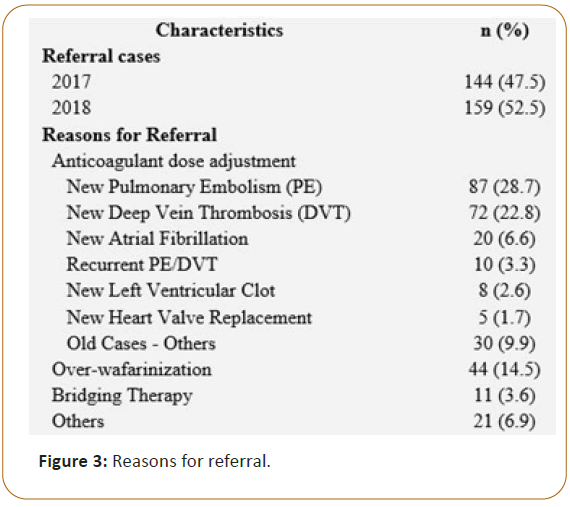
In our study (Figure 3), 232 (77%) patients were referred for dose adjustment and 44 (14.5%) patients were referred for over-wafarinization. Of 232 patients, 69% dose adjustment was done for new case of venous thromboembolism. More than 50% was referred due to provoke Deep Vein Thrombosis (DVT) and pulmonary embolism (PE). Cancer and immobilized was one of the provoking factors. These patients required short term ACT.
For all cases that were referred, IPAC pharmacists will counsel and reinforce patient education points including indication of anticoagulation, potential interaction with food and drugs, importance of adherence, administration of anticoagulants, and monitoring parameters (e.g., INR monitoring for patient on warfarin, renal functions for DOACs, and bleeding symptoms).
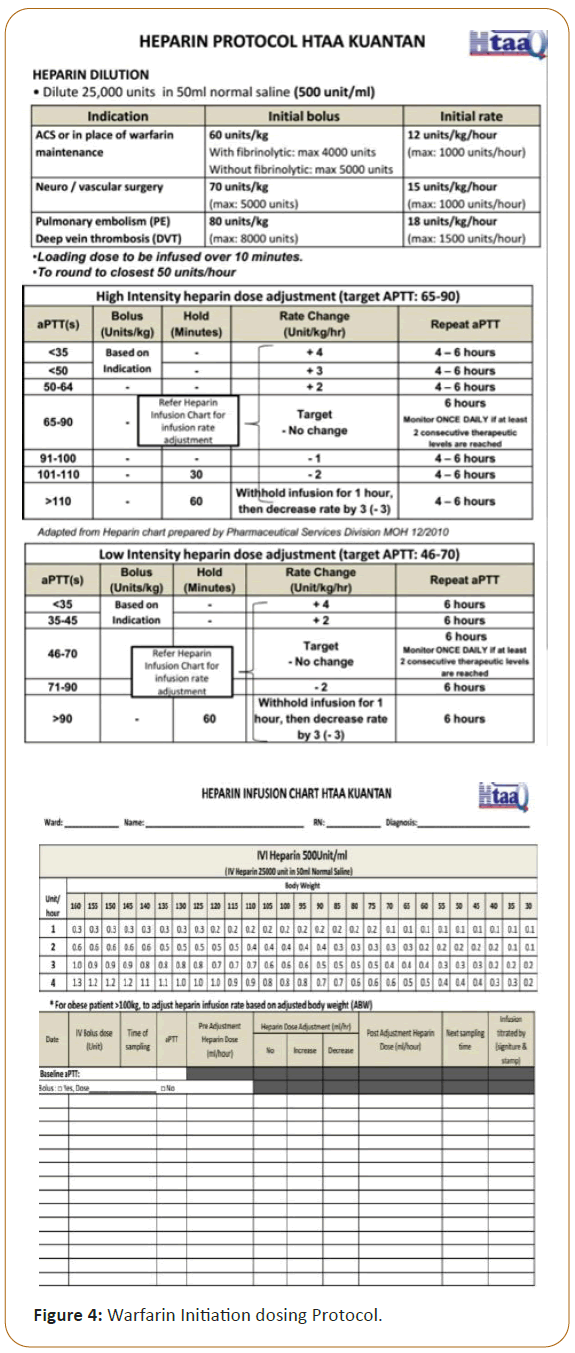
A retrospective data review showed four main variances related to ACT: 1) inappropriate administration of warfarin initiation dose, 2) inappropriate use of vitamin K, 3) inconsistent overlapping of heparin with warfarin, and 4) improper of patient education. Inappropriate dose adjustment on the 4th day is one of the common interventions. Supra-therapeutics INR have been recorded when dose was increased even though INR was >1.5 after initiation dose. This problem occurred because of daily monitoring of INR. To ease another prescriber on how to initiate and when to monitor INR, the IPAC pharmacists develop warfarin initiation protocol (Figure 4). In addition, dose adjustment for DOACs and LMWH were performed especially on patient with renal impairment. Although the patient renal function was worsening during hospital stay, the dose of DOACs and LMWH were not adjusted accordingly. In this instance, the IPAC team can identify the problems and intervene to change the dose based on the patients’ renal functions. Interventions related to anticoagulant reversal have been one of the prominent outcomes of this service. The prothrombin complex concentrate (PCC) was underutilized and inappropriate dose of Vitamin K was used for over-warfarinization cases. Vitamin K 10 mg daily was given for 3 days for patient with supra-therapeutic INR without bleeding tendency. For these cases, intervention of Vitamin K dose and advocating the use of PCC in the setting of over-warfarinization with life threatening bleeding were done. With the IPAC services, the total number of interventions pertaining to inappropriate dose of Vitamin K for over-warfarinization was reduced from 26 in 2017 to 18 cases in 2018.
Although the interventions are not significant, the IPAC service has also identified the gaps in treatment related to transition of care from in-patient to out-patient setting. Previously, improper documentation was encountered in warfarin book when patients were discharged to W-MTAC. Patients who newly started on warfarin or DOACs were also not properly counseled and discharged with insufficient history of ACT.
Besides that, non-standardization of heparin infusion monitoring aPTT vs. Prothrombin Time (PT) ratio has been used in this hospital. This issue caused improper dose of heparin infusion dose which led to failure on achieving aPTT or PT ratio target. Patients who received heparin infusion usually need closed monitoring to ensure they achieved the desired target to avoid bleeding or thrombosis. The IPAC team managed to standardize the heparin infusion monitoring using aPTT by developing new heparin protocol that needed to be used in HTAA.
Discussion
This study is the first evaluation of the outcomes of the IPACs in Malaysia. It provided critical information to the anticoagulation IPAC team for consideration of quality-improvement efforts. For example, many of the interventions were clinically important since they were related to inappropriate dosing and inappropriate selection of anticoagulants which can lead to bleeding or thrombosis. IPACs identified and resolved medication errors as well as optimized ACT through development of guidelines and protocols such as heparin protocol and warfarin dosing initiation and INR monitoring. A meta-analysis conducted by Hammond et al. in 2003 reviewed 54 separate studies that compared traditional drug management by physicians to inpatient drug management that had a pharmacist involved [8]. This meta-analysis found that 85% of the studies showed improvements in patient care when a pharmacist was added to the team compared to usual care management. These improvements included improved effectiveness, efficiency, and safety of the patient’s drug therapy.8 Most of the studies had shown that in-patient anticoagulation care and outcomes were significantly improved by a pharmacistmanaged anticoagulation service [6,9-11]. Currently, more studies had proven that pharmacist-managed in-patient anticoagulation care produced better outcomes [9,10,12]. Furthermore, although it was not significant, fewer adverse drug reactions and less supra-therapeutic INR were seen in pharmacists-managed than physicianmanaged care [13].
However, as a new service started in Malaysia, there are some challenges and barriers when implementing this new service. Compared to outpatient anticoagulation service (W-MTAC), IPACs is more challenging to do dose adjustment of warfarin when dealing with acutely ill patients with unstable conditions especially when there is a deterioration of renal and liver function during hospitalization. Some patients need lower initiation dose when antibiotics were given to treat infections. Bridging of anticoagulant before and after some procedures are time consuming and requires expert knowledge as the patients are highly at risk for thrombosis as well as bleeding.
Lack of awareness in initiating ACT for DVT prophylaxis was one of the reasons why patients develop PE and DVT especially in cancer and immobilized patients. Almost 80% of patients received prophylaxis after three to five days of hospital admissions. For Provoke DVT, the duration of ACT was three to six months [14,15]. unless for Cancer-Associated Thrombosis (CAT) which required longer duration of ACT. VTE was higher in cancer patients. It is currently estimated that the annual incidence of VTE in patients with cancer was estimated 0.5% compared to 0.1% in the general population. In CAT, active cancer accounts for 20% of the overall incidence of VTE.16 The recommendation duration of anticoagulation after a CAT episode is still debatable. Most guidelines suggested that the minimum duration of ACT for at least 6 months after the acute thrombotic event in cancer [16-20]. The extended duration of anticoagulation therapy after a CAT episode must be reevaluated in active cancer, metastatic disease or chemotherapy use patients because the risk factor for VTE recurrence is still present after the initial 6 months [16,17]. Many guidelines recommended the use of LMWH or DOAC for CAT. Nevertheless, despite guideline recommendations, the use of these ACT for CAT treatment is not easily done. DOACs are recommended over warfarin for treatment of non-cancer associated VTE and for stroke prevention in non-valvular atrial fibrillation by the American College of Chest Physicians (CHEST) [15,16]. However, budget constraint was the barrier in this service to use DOAC. Nevertheless, for patients who are eligible for DOAC, patient was suggested to self-purchase DOAC if the duration of treatment was less than six months. Unfortunately, higher costs and low patient adherence because of local pain due to the method of LMWH administration was another barrier. Also, both LMWH and DOAC should be avoided in renal impaired patients because the elimination of these drugs is via the kidneys, so the use of these ACT in patients with renal impairment requires more clinical attention. However, it is safe to be used in stable renal function but monitoring for bleeding complications and changes in renal function is still required [16-21].
Inadequate care transitions led to adverse outcomes especially when patients have complex or chronic medical conditions, including those on high risk anticoagulation therapy [22]. Thus, IPACs help to assure appropriate care transitions from in-patient to out-patient or other settings for patients receiving ACT. Documentation regarding ACT includes warfarin dosing and INR value during ward stay, INR target, duration for ACT and current dose were recorded in patient’s warfarin book prior to leaving the hospital. The collaboration of IPAC service with the W-MTAC has led to improved transitions of care. IPACs have identified and solved the issues on patients who have difficulty getting ACT information after discharged. Counselling related to ACT and follow-up date was arranged prior to discharge. Pharmacists who managed IPACs also see patients at WMTAC, which has opportunity to provide more information for a better understanding of in-patient issues. With this IPAC service, the team is able is to bridge the gap and provide the appropriate patient education as well as facilitate patient transfer to his preferred health clinic for anticoagulant monitoring.
Conclusion
Implementation of IPAC service identified and addressed issues related to ACT. Overall, IPACs appears to enhance quality of patient care in anticoagulation management which improves in-patient anticoagulation management, improves transitions of care and enhanced interdisciplinary practices.
Acknowledgments
We would like to thank the Director General of Health of Malaysia for granting us permission to publish this study, Pharmaceutical Service Division MOH and Tengku Ampuan Afzan Hospital.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- Dobesh PP, Trujillo TC, Finks SW (2013) Role of the pharmacist in achieving performance measures to improve the prevention and treatment of venous thromboembolism. Pharmacotherapy: J Hum Pharm Drug Therapy 33:650-664.
- Henriksen JN, Nielsen LP, Hellebek A, Poulsen BK (2017) Medication errors involving anticoagulants: Data from the Danish patient safety database. Pharmacol Res Perspect. 5:307.
- Garwood CL, Dumo P, Baringhaus SN, Laban KM (2008) Quality of anticoagulation care in patients discharged from a pharmacist-managed anticoagulation clinic after stabilization of warfarin therapy. Pharmacotherapy. J Hum Pharm Drug Therapy 28:20-26.
- Aidit S, Soh YC, Yap CS, Khan TM, Neoh CF, et al. (2017) Effect of standardized warfarin treatment protocol on anticoagulant effect: Comparison of a warfarin medication therapy adherence clinic with usual medical care. Front Pharmacol 8:637.
- Gupta V, Kogut SJ, Thompson S (2015) Evaluation of differences in percentage of international normalized ratios in range between pharmacist-led and physician-led anticoagulation management services. J Phar Pract 28:249-255.
- Lee T, Davis E, Kielly J (2016) Clinical impact of a pharmacist-led inpatient anticoagulation service: A review of the literature. Integr Pharm Res Pract 5:53.
- Donovan JL, Drake JA, Whittaker P, Tran MT (2006) Pharmacy-managed anticoagulation: Assessment of in-hospital efficacy and evaluation of financial impact and community acceptance. J Thromb Thrombolysis 22:23-30.
- Hammond RW, Schwartz AH, Campbell MJ, Remington TL, Chuck S, et al. (2003) Collaborative drug therapy management by pharmacists-2003. Pharmacotherapy 23:1210-1225.
- Wong YM, Quek YN, Tay JC, Chadachan V, Lee HK (2011) Efficacy and safety of a pharmacist-managed inpatient anticoagulation service for warfarin initiation and titration. J Clin Pharm Ther 36:585-591.
- Daniels PR, Manning DM, Moriarty JP, Bingener-Casey J, Ou NN, et al. (2018) Improving inpatient warfarin therapy safety using a pharmacist-managed protocol. BMJ open quality 7.
- Thompson SS, Hannan C, Holden L, Flickinger D (2012) Impact of an inpatient anticoagulation monitoring program. US Pharm 37, 1-11.
- Burnett A, D’Angio R, Earl LE, Garcia D (2011) Challenges and benefits of an inpatient anticoagulation service: One hospital’s experience. J Thromb Thrombolysis 31:344-352.
- Damaske DL, Baird RW (2005) Development and implementation of a pharmacist-managed inpatient warfarin protocol. In Bayl Univ Med Cent Proceedings 18: 397-400.
- Streiff MB, Agnelli G, Connors JM, Crowther M, Eichinger S, et al. (2016) Guidance for the treatment of deep vein thrombosis and pulmonary embolism. J Thromb Thrombolysis 41: 32-67.
- Guyatt GH, Akl EA, Crowther M, Gutterman DD, Schuünemann HJ (2012) Executive summary: Antithrombotic therapy and prevention of thrombosis: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 141: 7.
- Fernandes CJ, Morinaga LT, Alves JL, Castro MA, Calderaro D, et al. (2019) Cancer-associated thrombosis: The when, how and why. Eur Respir Rev 31;28.
- Chai-Adisaksopha C, Iorio A, Crowther MA, de Miguel J, Salgado E, et al. (2018) Vitamin K antagonists after 6 months of low-molecular-weight heparin in cancer patients with venous thromboembolism. Am J Med 131: 430-437.
- Lyman GH, Bohlke K, Khorana AA, Kuderer NM, Lee AY, et al. (2015) Venous thromboembolism prophylaxis and treatment in patients with cancer: American Society of Clinical Oncology clinical practice guideline update 2014. J Clin Oncol. 33:654.
- Watson HG, Keeling DM, Laffan M, Tait RC, Makris M, et al. (2015) Guideline on aspects of cancer-related venous thrombosis. Br J Haematol 170:640-648.
- Mandala M, Falanga A, Roila F. ESMO Guidelines Working Group (2011) Management of Venous Thromboembolism (VTE) in cancer patients: ESMO Clinical Practice Guidelines. Annals of Oncology 22: 85-92.
- Conway SE, Hwang AY, Ponte CD, Gums JG. (2017) Laboratory and clinical monitoring of direct acting oral anticoagulants: What clinicians need to know? Pharmacotherapy 37:236-248.
- Nutescu EA, Wittkowsky AK, Burnett A, Merli GJ, Ansell JE, et al. (2013) Delivery of optimized inpatient anticoagulation therapy: Consensus statement from the anticoagulation forum. Ann Pharmacother 47:714-724.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences