Hepatoblastoma as a Cause of Precocious Puberty
1Temple University Hospital, Diagnostic Radiology 3401 North Broad Street, Philadelphia, PA 19140, USA
2The Childrens Hospital of Philadelphia, Diagnostic Radiology 34th St and Civic Center Blvd, Philadelphia, PA 19104, USA
- *Corresponding Author:
- Farouk Dako
Temple University Hospital
Diagnostic Radiology 3401 North Broad Street
Philadelphia, PA 19140, USA
Tel: 2673091241
E-mail: fdako123@gmail.com
Received date: March 05, 2018; Accepted date: March 11, 2018; Published date: March 19, 2018
Citation: Dako F, Back S, Bellah R. Hepatoblastoma as a Cause of Precocious Puberty. J Clin Radiol Case Rep 2018, Vol.2 No.1:03.
Copyright: © 2018 Dako F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Hepatoblastoma is the most common primary hepatic tumor in children. Precocious puberty is a rare paraneoplastic syndrome that can occur in male children with hepatoblastoma as a result of elevated human chorionic gonadotropin (HCG). The clinical signs of precocious puberty may be detected months before the physical effects of tumor growth such as abdominal pain and distension. Therefore, consideration of hepatoblastoma in young boys presenting with precocious puberty can lead to earlier detection, diagnosis, treatment and thus arrest further virilization. This report describes the presentation, imaging and relevant laboratory findings in two pediatric patients with hepatoblastoma presenting with precocious puberty.
Keywords
Hepatoblastoma; Precocious puberty; Human chorionic gonadotropin
Introduction
While there is debate about the age at which puberty begins, one definition of precocious puberty is the onset before 8 years of age in girls and 9 years of age in boys [1]. Precocious puberty is either central, (gonadotropin dependent) from the early maturation of the hypothalamicpituitary- gonadal axis or peripheral (gonadotropin independent) from autonomous hormone production. The current imaging evaluation of precocious puberty typically includes brain MRI if laboratory findings favor central precocious puberty, of which hypothalamic hamartoma is the most commonly associated lesion [2].
If peripheral precocious puberty is suspected, imaging work up typically includes scrotal and adrenal US to exclude sex cord-stromal tumors of the testis and adrenal cortical neoplasms respectively [2]. Precocious puberty is uncommonly caused by neoplasm therefore clinical suspicion of this possibility is needed to help avoid a delay in diagnosis [3].
Neoplastic causes of precocious puberty commonly include brain, gonadal, adrenocortical, and germ cell tumors; hepatoblastoma is only rarely noted [2,3].
Hepatoblastoma is the most common primary hepatic tumor in children [4]. It causes increased serum alphafetoprotein (AFP) and rarely, increased levels of human chorionic gonadotropin (HCG) [2]. HCG is biologically similar to luteinizing hormone and can stimulate testosterone production by testicular Leydig cells leading to isosexual precocious puberty [2,5]. Even rarer, hepatoblastoma can directly produce testosterone, without elevated HCG levels, and result in precocious puberty [6].
Case 1
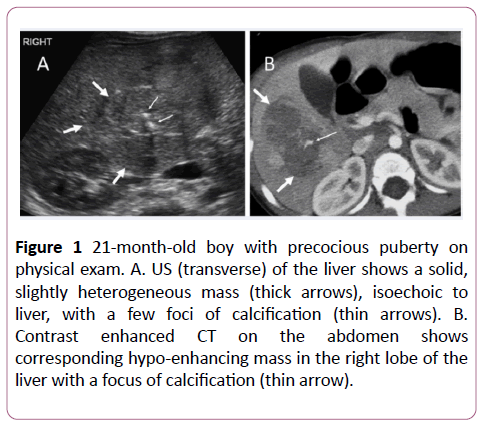
A 21-month old boy presented with a three-week history of pubic hair growth. Labs revealed elevated serum AFP of 27,107 ng/mL (normal <12 ng/mL) and b-hCG of 84 mIU/mL (normal <2 mIU/mL). Ultrasound (US) surveillance of the abdomen demonstrated a 6 × 5 cm heterogeneous mass in the right hepatic lobe with two areas of focal calcification and mild vascularity on color Doppler. Contrast CT subsequently showed a heterogeneous, hypo-enhancing mass limited to the right hepatic lobe with focal areas of calcification (Figure 1).
Figure 1: 21-month-old boy with precocious puberty on physical exam. A. US (transverse) of the liver shows a solid, slightly heterogeneous mass (thick arrows), isoechoic to liver, with a few foci of calcification (thin arrows). B.Contrast enhanced CT on the abdomen shows corresponding hypo-enhancing mass in the right lobe of the liver with a focus of calcification (thin arrow).
He was transferred to our institution, where he underwent a right lobe hepatectomy. Pathology confirmed hepatoblastoma with “mixed epithelial and mesenchymal type with teratoid”; surgical margins were negative. The patient received two cycles of adjuvant chemotherapy. The AFP and b-hCG levels returned to normal three months after surgery. There was no new evidence of virilization after surgery. There was no evidence of tumor recurrence or metastasis 3 months after surgery.
Case 2
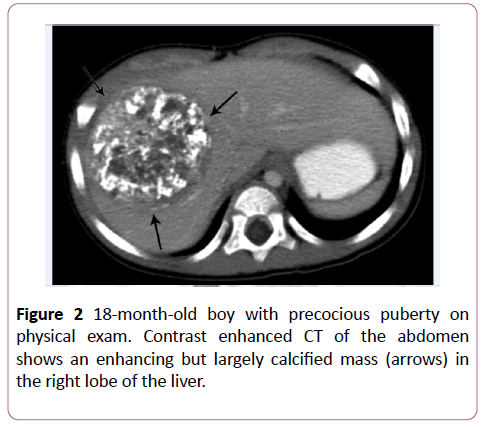
An 18-month old boy presented with penile enlargement and pubic hair. Labs revealed elevated serum AFP of 30,475 ng/mL (normal <12 ng/mL) and b-hCG of 41 mIU/mL (normal <2 mIU/mL). Focused US showed normal adrenal glands. Contrast CT of the abdomen showed a 6.5 × 6.7 cm heterogeneous hypo-enhancing, partially calcified mass in the right hepatic lobe (Figure 2). No additional lesions or abnormalities were present in the chest, abdomen, and pelvis. The patient underwent a right hepatectomy. Pathology confirmed hepatoblastoma “mixed epithelial and mesenchymal type, with extensive osseous metaplasia”. The surgical margins were clear. Following surgery, the patient received adjuvant chemotherapy. There was no evidence of recurrence 14 years following surgery.
Discussion
Hepatoblastoma often presents as an enlarging abdomen due to mass effect and nonspecific symptoms including anorexia and weight loss [2]. About 68% of cases present in the first 2 years of life and 90% present before 5 years of age [2]. Metastatic disease is present at diagnosis in 10-20% of patients and is most common in the lungs, which is also the most frequent site of relapse [7]. Hepatoblastoma may be associated with syndromes, including Beckwith-Wiedemann, Gardner, familial adenomatous polyposis, type 1A, glycogen storage disease, and trisomy 18 [3]. As a result, these patient populations are screened by US. At US, hepatoblastoma is most often hyperechoic relative to adjacent liver. On CT, it is often well circumscribed and slightly hypoattenuating and hypoenhancing relative to the adjacent liver parenchyma on unenhanced and contrast-enhanced images respectively. MRI usually shows a mass that is hypointense on T1-weighted images and hyperintense on T2-weighted images relative to adjacent liver parenchyma [2].
In each of the patients we describe, a liver mass was found during evaluation for precocious puberty, in which, elevated levels of HCG were thought to have resulted in clinical signs of virilization. CT in both patients displayed a heterogeneously hypo-enhancing right hepatic lobe mass with associated calcification, similar in appearance to those described in a previous reported case [8]. The imaging characteristics of hepatoblastoma reflect its histologic composition [2]. The mixed epithelial and mesenchymal hepatoblastoma subtypes appear more heterogeneous due to osteoid, cartilaginous, and fibrous components (as seen in our cases) while the epithelial subtype typically demonstrates a homogeneous imaging appearance [2]. There are no imaging features noted on our cases to differentiate HCG producing hepatoblastoma from its non-HCG producing counterpart however, this is an area for potential future research.
In previous reported cases of hepatoblastoma presenting with precocious puberty in boys 3 years of age and younger, many were diagnosed with hepatoblastoma months after the initial signs of virilization were observed [3,8,9]. One factor that could, perhaps, contribute to such delay in diagnosis is that the current diagnostic work up of precocious puberty in a male child does not routinely include complete abdominal imaging [2,10]. An elevated AFP, as noted in both of our cases, should warrant evaluation to exclude a neoplastic etiology in this age group.
Conclusion
The imaging evaluation of a young boy with precocious puberty typically does not include imaging of the liver. Hepatoblastoma may be an uncommon cause of isosexual precious puberty in a young boy due to tumor secretion of HCG. This consideration should prompt inclusion of hepatic imaging in the diagnostic evaluation of peripheral precocious puberty if testicular and adrenal imaging examinations are normal.
References
- Parent AS, Teilmann G, Juul A, Skakkebaek NE, Toppari J, et al. (2003) The timing of normal puberty and the age limits of sexual precocity: variations around the world, secular trends, and changes after migration. Endocrine Reviews 24: 668-693.
- Chung EM, Biko DM, Schroeder JW, Cube R, Conran RM (2012) From the radiologic pathology archives: precocious puberty: radiologic-pathologic correlation. Radiographics 32: 2071-2099.
- Wendt S, Shelso J, Wright K, Furman W (2014) Neoplastic causes of abnormal puberty. Pediatric Blood & Cancer 61: 664-671.
- Chung EM, Lattin Jr GE, Cube R, Lewis RB, Marichal-Hernández C, et al. (2011) From the archives of the AFIP: pediatric liver masses: radiologic-pathologic correlation part 2. Malignant tumors. Radiographics 31: 483-507.
- Atay Z, Yesilkaya E, Erdeve SS, Turan S, Akin L, et al. (2016) The etiology and clinical features of non-CAH gonadotropin-independent precocious puberty: a multicenter study. The Journal of Clinical Endocrinology & Metabolism 101: 1980-1988.
- Galifer RB, Sultan C, Margueritte G, Barneo G (1985) Testosterone-producing hepatoblastoma in a 3-year-old boy with precocious puberty. Journal of Pediatric Surgery 20: 713-714.
- Herzog CE, Andrassy RJ, Eftekhari F (2000) Childhood cancers: hepatoblastoma. The Oncologist 5: 445-453.
- Al-Jumaily U, Sammour I, Al-Muhaisen F, Ajlouni F, Sultan I (2011) Precocious puberty in an infant with hepatoblastoma: a case report. Journal of Medical Case Reports 5: 422.
- Eren E, Demirkaya M, Çakir EDP, Sevinir B, Saglam H, et al. (2009) A rare cause of precocious puberty: hepatoblastoma. Journal of Clinical Research in Pediatric Endocrinology 1: 281.
- Carel JC, Leger J (2008) Precocious puberty. New England Journal of Medicine 358: 2366-2377.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences