Fatal Type-B Lactic Acidosis in Association with HIV Associated Lymphoma - A Case Report with Review of Literature
Asif Salim, Sara Chinthu, Shobhana Nayak Rao* and Pradeep Shenoy M
Department of Nephrology, K.S. Hegde Medical Academy, Medical Sciences Complex, Derlakatte, Mangalore 575013, Karnataka, India
- *Corresponding Author:
- Shobhana Nayak Rao
Associate Professor and Head, Department of Nephrology, K.S. Hegde Medical Academy, Derlakatte, Mangalore 575013, Karnataka, India
Tel: +91-824-2204471-76
E-mail: nayak_shobhana@rediffmail.com
Received date: June 27, 2017; Accepted date: June 27, 2017; Published date: July 24, 2017
Citation: Salim A, Chinthu S, Rao SN, Shenoy PM (2017) Fatal Type-B Lactic Acidosis in Association with HIV Associated Lymphoma- A Case Report with Review of Literature. Jour Ren Med Vol.1. No.2: 8.
Abstract
Hyperlactemia is defined as whole blood lactate levels > 2 mmol/L. Type-B lactic acidosis refers to conditions wherein overproduction of lactate is not related to reduction in tissue oxygen. The occurrence of severe lactic acidosis in malignancies is a rare and often pre-terminal complication. We present two HIV positive patients with type-B lactic acidosis as a pre-terminal event after being diagnosed with non –Hodgkins’ lymphoma. The first patient, a 45-year-old male, HIV positive since 2012 on therapy admitted with h/o of pedal edema, generalized weakness and decreased appetite 1 week duration. Abdominal ultrasound scan revealed bilateral moderate hydro-ureteronephrosis with large left pleural effusion, cytology revealed malignant serous lymphoma confirmed by supraclavicular lymph node biopsy. Before initiation of chemotherapy, his general condition rapidly worsened with onset of lactic acidosis (10 mmol/L) and he expired. The second patient, a 59-year-old male presented with acute hematemesis. He was detected to be HIV positive 2 months earlier and was on anti-retroviral therapy. Evaluation revealed a diagnosis of diffuse B large cell lymphoma extending from gastric fundus to pylorus. CT abdomen showed diffuse and extensive disease in the stomach with splenic, peritoneal, lung metastasis and diffuse intraabdominal lymphadenopathy. He was started on chemotherapy two days later, he had a massive hematemesis with deterioration in clinical condition, severe metabolic acidosis and hyperlactemia of 19 mmol/L. Patient expired despite bicarbonate infusion, high dose thiamine and hemodialysis. Type-B lactic acidosis is a rare event in hematological malignancies and often is a poor prognostic factor determining survival.
Keywords
Lymphoma; Malignancy; Lactic acidosis; Prognosis
Introduction
Hyperlactemia is defined as whole blood lactate levels > 2 mmol/L and is considered severe when levels are greater than 5 mmol/L. Based on the underlying pathophysiology, three different types of lactic acidosis have been described: Type-A and type-B and Type-D (1). Type-A lactic acidosis is seen in clinical conditions associated with tissue hypoxia as in hypovolemia, septic or cardiogenic shock. Type-B lactic acidosis is less common and refers to conditions wherein overproduction of lactate is not related to the reduction in tissue oxygen delivery. Depending on the etiology and associated disease, it is further sub classified as:
B1: Ketoacidosis, leukemia, lymphoma, AIDS.
B2: Medications like metformin, phenformin, antiretrovirals, sodium nitroprusside, ribavirin and toxins, cyanide and methanol.
B3: Pyruvate dehydrogenase deficiency, thiamine deficiency.
Type-D lactic acidosis is due to excessive production of Dlactic acid from intestinal bacterial proliferation, such as in short bowel syndrome, ischemic bowel disease, or small bowel obstruction. While mammals produce L-lactic acid, bacteremia produces the D-type lactic acid. The occurrence of severe lactic acidosis in malignancies is a rare and often pre-terminal complication. The underlying pathogenesis is poorly understood and the prognosis of such patients is poor. We present two HIV positive patients who presented with type-B lactic acidosis as a pre-terminal event after being diagnosed with non –Hodgkins’ lymphoma [1].
Case 1
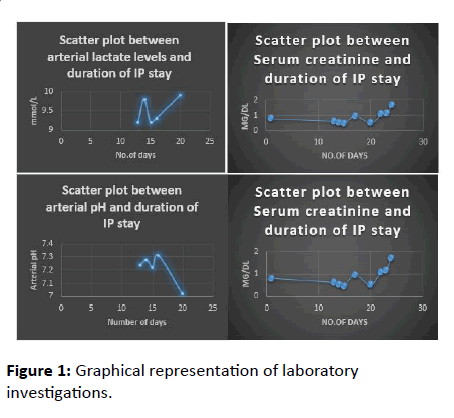
A 45-year-old male, diagnosed to be HIV positive since 2012 on antiretroviral therapy with lamivudine, efavirenz and tenofovir was admitted for complaints of pedal edema for 20 days, generalised weakness and decreased appetite of 1-week duration. He also had c/o pain in the lower limbs. There was also h/o associated redness and swelling in the left upper limb of almost 6 months duration which was being treated symptomatically at a local hospital. He gave a significant history of weight loss of 6 months duration. There was no history of fever/ vomiting/ cough/ dysuria/ hematuria. His CD4 count done after admission was 109 cells/cm2. There was no previous h/o of tuberculosis or malignancy in the past. On examination, he was moderately built though poorly nourished, he was afebrile and his vital signs were stable. He had oral thrush, left upper limb edema and erythema extending to the elbow with peaud’ orange appearance of the left lower arm with tenderness, bilateral lower limb edema with scrotal edema and bilateral supraclavicular lymphadenopathy. Respiratory system evaluation revealed decreased breath sounds and decreased vocal fremitus in the left subscapular area. The rest of the physical examination was unremarkable and no hepatosplenomegaly was noted. The results of the investigations findings are summarized in Table 1 and in Figure 1.
| Variables | Day 1 | Day 3 | Day 10 | Day 15 | Day 20 |
|---|---|---|---|---|---|
| Hemoglobin (gm/dl) | 9.2 | - | - | 10 | - |
| Total Leucocyte (count / cc/mm) | 11,300 | 20,750 | - | 21,000 | - |
| Blood urea (mg/dl) | 84 | 169 | 152 | 114 | 145 |
| Serum creatinine (ng/dl) | 3.6 | 7.04 | 3.6 | 1.89 | 2.35 |
| Serum bicarbonate(Meq/L) | - | - | - | 15 | - |
| Blood lactate(mmol/L) | - | - | - | 12.5 | 15 |
Table 1: Laboratory investigations of patient 1.
Ultrasound scan of the abdomen revealed bilateral moderate hydroureteronephrosis, with grade I-II renal parenchymal changes. Urinary bladder appeared partially distended with echogenic band adherent to the posterior wall – likely focal thickening. This was confirmed by CT scan of the abdomen which showed bulky kidneys with moderate hydronephrosis, perinephric fat stranding, thickening of bladder walls, retroperitoneal and mesenteric lymphadenopathy. There was large left sided pleural effusion with partial collapse of left lower lobe. He underwent double – J stent placement after urology consultation following which his renal functions steadily improved. He did not need dialysis at any time. Pleural fluid cytology showed multiple degenerating cells, and plenty of atypical large cells with eccentric round to oval nuclei, prominent nucleoli, abundant pale blue vacuolated cytoplasm and plenty of atypical mitosis, suspicious of malignant lymphoma probable primary serous effusion lymphoma. Left supraclavicular lymph node biopsy microscopy was suggestive of non-Hodgkin’s lymphoma. Skin biopsy from left upper limb revealed dermis showing sheets of tumour cells showing nuclear pleomorphism, inflammatory cells consisting of neutrophils and some debris can be seen amidst sheets of tumour cells infiltrating nerves and the features were suggestive of lymphoma infiltration in the skin. Therapeutic pleurocentesis was done for symptomatic relief and oncology service was consulted with plans to initiate him on chemotherapy, however his general condition rapidly worsened with worsening of lactic acidosis and he expired within a week after the diagnosis.
Case 2
A 59-year-old male with no previous co-morbid illness earlier presented with history of acute hematemesis 8 months earlier. An upper gastrointestinal endoscopy at that time had revealed a large gastric ulcer and this had been treated conservatively at a different centre along with blood transfusion. He had been asymptomatic till multiple bouts of vomiting and hematemesis 5 months later during which he was evaluated, detected to be HIV positive and then referred here for further management. He also gave a history of significant weight loss of about 20 kg over the last 6 months with poor appetite. He had been started on antiretroviral therapy with Lamivudine, Efavirenz and Tenofovir since the last 2 months, but no CD4 counts were available from previous records. On examination, he was moderately built, though poorly nourished, with severe pallor; supraclavicular lymphadenopathy was noted with 1-2 cm nodes which were hard and nodular. A well circumscribed hard mass measuring 12 × 12 cm was noted in the epigastric and umbilical area of the abdomen with no other organomegaly and no palpable lymphadenopathy. No ascites was noted. Upper gastrointestinal endoscopy revealed a diffuse irregular wall thickening of the stomach extending from the gastric fundus to the pylorus. Biopsy of this lesion revealed a diffuse B large cell lymphoma with CD 45, Ki 67 (70%) positivity on immunological profiling. CT abdomen showed diffuse and extensive disease in the stomach with splenic and peritoneal and lung metastasis and diffuse intraabdominal lymphadenopathy. He was started on chemotherapy with rituximab, cyclophosphamide, vincristine and prednisone. Two days after chemotherapy, he had a massive hematemesis causing hypovolemic shock requiring multiple blood and plasma expander therapy. Blood pressures picked up after this to 110 mm of Hg systolic. However, at this time, the serum lactate was noted to be high at 19 mmol/L with ABG showing severe metabolic acidosis with arterial ph of 6.9. Bicarbonate infusion along with high dose thiamine therapy was started, with improvement in blood ph to 7.2, venous bicarbonate to 14; however the blood lactate continued to be high at 18 mmol/L (Table 2). Slow low efficiency hemodialysis was planned, however the patient died before this could be initiated [2].
| Variables | Day 1 | Day 3 | Day 10 | Day 15 | Day 18 |
|---|---|---|---|---|---|
| Hemoglobin (gm/dl) | 4.2 | 8.9 | 10.7 | 8.7 | 8.2 |
| Total Leucocyte (count / cc/mm) | 16,400 | - | - | 23,000 | 12,900 |
| Blood urea (mg/dl) | 36 | - | - | 58.6 | 67.9 |
| Serum creatinine (mg/dl) | 0.8 | - | - | 0.53 | 0.97 |
| Serum albumin (gm/dl) | 1.8 | - | - | 1.8 | - |
| Serum bicarbonate (mg/dl) | - | - | - | 8.3 | 14.6 |
| Arterial pH | - | - | - | 6.98 | 7.25 |
| Blood lactate (mmol/L) | - | - | - | 19 | 18 |
Table 2: Investigations of patient 2.
Discussion
Pathophysiology of lactic acidosis: Lactic acid(LA) results from the binding of one molecule of lactate with one hydrogen cation Lactic acidosis is defined as LA levels in whole blood more than >5 mmol/L and a ph <7.30. In normal conditions, lactic acid is cleared by the liver (80% to 90%) after conversion to glucose via gluconeogenesis and the remainder by the kidneys. A better understanding of the mechanisms involved in the development of Type-B lactic acidosis in patients with cancer requires a review of the metabolism of a normal vs. a malignant cell [3].
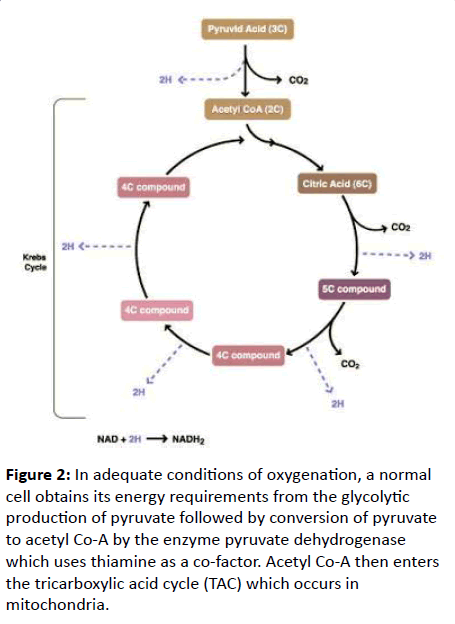
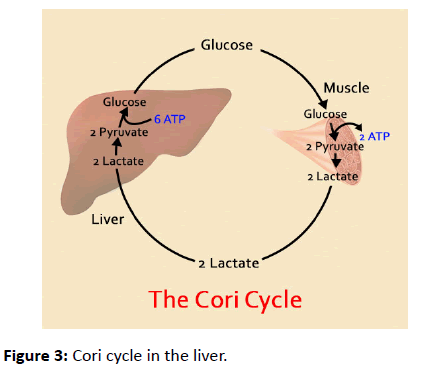
As shown in Figure 2, in adequate conditions of oxygenation, a normal cell obtains its energy requirements from the glycolytic production of pyruvate followed by conversion of pyruvate to acetyl Co-A by the enzyme pyruvate dehydrogenase which uses thiamine as a co-factor. Acetyl Co-A then enters the tricarboxylic acid cycle (TAC) which occurs in mitochondria. This process results in the production of 36 molecules of ATP from one single molecule of glucose. In the absence of oxygen, the TAC in mitochondria cannot occur and the cell then switches over to glycolytic pathway to derive energy. However, the glycolytic pathway is not energy efficient and can only supply 2 molecules of ATP by conversion of pyruvate to lactic acid [4]. LA is then recycled back to glucose in the liver by the gluconeogenic process known as the Cori cycle (Figure 3) in which 2 molecules of glucose produce 1 molecule of lactate.
Figure 2: In adequate conditions of oxygenation, a normal cell obtains its energy requirements from the glycolytic production of pyruvate followed by conversion of pyruvate to acetyl Co-A by the enzyme pyruvate dehydrogenase which uses thiamine as a co-factor. Acetyl Co-A then enters the tricarboxylic acid cycle (TAC) which occurs in mitochondria.
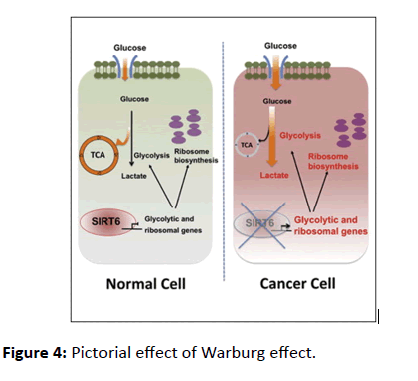
Pathophysiology of Type-B lactic acidosis in malignancy: Otto Van Warburg in 1924 demonstrated however [5] that tumour cells switched their metabolic pathways toward the glycolytic state, even in the presence of normal oxygen concentrations (Known as the Warburg effects or aerobic glycolysis). Additionally, since the Cori cycle requires 6 molecules of ATP to produce one single molecule of glucose, more energy is expended by the cell to regenerate glucose and in the conversion of glucose to lactate. The exact reasons for these metabolic changes in a tumor cell are not known. Vander Heyden et al. [6] proposed that these adaptive changes enabled cancer cells to acquire and metabolize nutrients that would favour cell proliferation over ATP production (Figure 4) The excessive production of lactic acid in patients with cancer is counterbalance by the Cori cycle in the liver favouring gluconeogenesis and hence most cancer patients do not manifest Type- B lactic acidosis. In a few subsets of patients, this metabolic machinery breaks down resulting in Type-B lactic acidosis.
The mechanisms proposed for the development of Type-B lactic acidosis in malignancy are the following:
• Decreased hepatic clearance of lactate, especially in patients with extensive liver metastasis.
• Aberrant Insulin-like Growth Factor (IGF) leading to an increase in glycolytic rate and over-expression of hexokinase Type-2, the rate -limiting enzyme involved in glucose consumption by the cell [7].
Vitamin deficiencies have also been associated in the development of lactic acidosis [8,9]. Thiamine deficiency interferes with the conversion of pyruvate into acetyl-Co-A since it is a co-factor for pyruvate dehydrogenase enzyme. Improvement after thiamine supplementation has been noted as well [10]. Another proposed mechanism has been embolization of malignant cells into the microvasculature causing a state of hypoperfusion and increase in anerobic metabolism [11] though this has not been proven.
The occurrence of Type B lactic acidosis is thought to be a rare complication of malignancy and was first described by Field et al. [12] in patients with acute leukemia in 1963. Since then, it has been reported more often in hematological malignancies such as leukemia and lymphoma and rarely in solid tumours such as lung, endometrial and breast cancers [13-15]. The occurrence of lactic acidosis in malignancy is of grave significance and generally portends a poor prognosis. Human immunodeficiency virus (HIV) infection results in impaired cellular immunity and pre-dispose persons to develop neoplasms [16]. 25% to 40% of HIV positive patients will develop a malignancy with non-Hodgkins’ lymphoma being the most common and accounting for approximately 10% of all malignancies. These lymphomas appear to be more common in males than in females regardless of antiretroviral use. Antiretroviral drugs such as zidovudine also have been associated with mitochondrial toxicity causing Type-B lactic acidosis.
Both of our patients developed lactic acidosis in association with rapidly proliferating malignancies that were related to HIV infection. In the second patient, lactic acidosis could be a combination of both Type A and B, however by the time the increased lactate levels were detected, the hemodynamic status of the patient had improved decreasing the probability of Type A lactic acidosis.
Therapeutic options: Treatment for malignancy associated Type B lactic acidosis have not been fully established or tested rigorously due to the rapidity of development and the overall poor prognosis of these patients. High dose thiamine has been tried, however it is not clear if prior vitamin levels were estimated. Since thiamine is a co-factor for pyruvate dehydrogenase enzyme, this would drive pyruvate towards synthesis of acetyl co-A instead of the production of lactic acid. Hemodialysis has been proposed as a way of clearing excess lactic acid and along with bicarbonate infusions has been used to tide over the crisis. However, none of these therapies have significantly improved patient survival till date
Conclusion
The occurrence of lactic acidosis in association with malignancy is a relatively rare event and usually occurs as a pre-terminal event regardless of treatment offered. Future research should focus on potential therapy based on pathogenetic mechanisms.
Conflict of Interest
The authors declare that they do not have any current conflict of interest and the article is submitted with the undertaking that it has not been submitted /accepted for publication elsewhere.
References
- Cohen R, Woods H (1976) Clinical and biochemical aspects of lactic acidosis. Blackwell Scientific Publications, Oxford, England.
- Brenner BM (2007) Brenner and Rector‘s the Kidney (8th edn) Saunders, Philadelphia p: 533-535.
- Gauthier PM, Szerlip HM (2002) Metabolic acidosis in the intensive care unit. Crit care clin 18: 289-303.
- Rovelli A, Bonomi M, Murano A, Locasciulli A, Uderzo C (1990) Severe lactic acisosis sue to thiamine deficiency after bone marrow transplantation in a child with acute monocytic leukemia. Hematologica 75: 579-581.
- Warburg O, Posener K, Negelein E, Tumoren UDSD (1924) Biochem Z 152: 319-344
- Heiden VMG, Cantley LC, Thompson CB (2009) Understanding the Warburg effect: The metabolic requirements of cell proliferation. Science 324: 1029-1033.
- Sillos EM, Shenep JL, Burghen GA, Pui C, Behm F, et al. (2001) Lactic acidosis: A metabolic complication of hematologic malignancies. Case Report and review of the literature. Cancer 92: 2237-2246.
- Kuba H, Inamura T, Ilezaki K, Kawashima M, Fukui M (1998) Thiamine-deficient lactic acidosis with brain tumor treatment. Report of three cases. J Neurosurg 89: 1025-1028.
- Oriot D, Wood C, Gottesman R, Huault G (1991) Severe lactic acidosis related to acute thiamine deficiency. JPEN. J Parenter Enteral Nutr 15: 105-109.
- Svahn J, Schiaffino M, Caruso U, Calvillo M, Minniti G, et al. (2003) Severe lactic acidosis due to thiamine deficiency in patient with B-cell leukemia/lymphoma on total parenteral nutrition during high- dose methotrexate therapy. J Pediatr Hematol Oncol 25: 965-968.
- Block JB (1974) Lactic acidosis in malignancy and observations on its possible pathogenesis. Ann N.Y. Acad Sci 230: 94-102.
- Field M, Block JB, Rall DD (1963) Lactic acidosis in acute leukaemia. Clin Res 11: 193-197.
- Claudino WM, Dias A, Tse W, Sharma VR (2015) Type B lactic acidosis: a rare but life threatening hematologic emergency. A case illustration and brief review. Am J Blood Res 5: 25-29.
- Friedenberg AS, Brandoff DE, Schiffman FJ (2007) Type B lactic acidosis as a severe metabolic complication in lymphoma and leukemia: a case series from a single institution and literature review. Medicine, Baltimore 86: 225-232.
- Ruiz JP, Singh AK, Hart P (2011) Type B lactic acidosis secondary to malignancy: case report, review of published cases, insights into pathogenesis, and prospects for therapy. Scientific World Journal 11: 1316-1324.
- Johnson CC, Wilcosky T, Kvale P (1997) Cancer incidence among an HIV–Infected cohort. Pulmonary complications of HIV infection Study Group. Am J Epidemiol 146: 470.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences