Epidemiological Analyses of Idiopathic Pulmonary Arterial Hypertension in the Indian Cohort
Chaitra KL1, Nallari P1*, Sairam M1, Kumar BC1 and Sastry BKS2
1Department of Genetics, Osmania University, Hyderabad, Telangana, India
2Care Hospitals, Nampally, Hyderabad, Telanagana, India
- *Corresponding Author:
- Pratibha Nallari
Professor, Department of Genetics
Osmania University, Hyderabad
Telangana 500007, India
Tel: +91-8885486499
E-mial: prathinallari@gmail.com
Received Date: March 20, 2018; Accepted Date: May 24, 2017; Published Date: June 08, 2017
Citation: Chaitra KL, Nallari P, Sairam M, Kumar BC, Sastry BKS (2018) Epidemiological Analyses of Idiopathic Pulmonary Arterial Hypertension in the Indian Cohort. J Genom Gene Study Vol.1 No.1:2
Abstract
Idiopathic Pulmonary Arterial Hypertension (IPAH) is a subset of cardiovasculardisease, and the most neglected from the public point of view. Estimation of diseaseprevalence becomes difficult in the developing world because of economic,ethnic, socio-cultural and geographic diversity. Several patients may not reach centers equipped with diagnosing PAH, thus, only a small portion of the patients with the disease are captured in disease registries. Female predilection is commonly seen in IPAH with the female to male ratio ranging from 2:1 to 9:1. Clinical characteristics of IPAH patients in the present study were compared with those enrolled in Swiss Registry, SERAPHIN, ASPIRE, Pulmonary Hypertension Registry of the United Kingdom and Ireland, Korean Pulmonary Arterial Hypertension Registry and the French registry, with only Idiopathic cases being included in this study. This study attempts to characterize the epidemiological parameters in the Indian cohort with respect to IPAH.
Keywords
IPAH; Indian/cohort; Epidemiology; Female; Incidence; Prognosis
Introduction
Idiopathic Pulmonary Arterial Hypertension is a rare disorder, with increased pulmonary arterial pressure; maintained at >25 mmHg at rest or 30 mmHg during exercise. The prevalence of both PAH and IPAH is debatable as it varies in the former category with respect to high-risk groups, like HIV positives, sickle cell disease and systemic sclerosis each having a prevalence of 0.5%, 2-3% and 7-12% respectively [1]. Since IPAH is routinely misdiagnosed, the true prevalence remains unknown. In the US, its incidence is said to be 2-6 per million [2]. The worldwide incidence of IPAH is similar to that observed in the US, with minor variations. In France, a registry of IPAH patients showed a prevalence of 6 per million [3]. However, the prevalence of IPAH in Asia and India remains speculative. Female preponderance is commonly observed in IPAH, and it varies in different populations, with the ratio ranging from 2:1 to 9:1. In Europe, a higher incidence in females by about 2-4 times is seen, whereas, in the US, the ratio is close to 4:1. Although the reason for the female predilection is unknown, sex hormones seem to play a role in the pathogenesis of IPAH. A commonly observed characteristic is that females of child bearing age develop IPAH. A specific age for onset isn’t known, but the mean age at diagnosis seems to be 45 years [4]. Although, individuals in their fifth and sixth decades of life, are also known to be affected [5]. One of the major contributions of the multicenter study of the US National Institutes of Health (NIH) registry on IPAH was to recognize a highly variable clinical course of the disease. Keeping in view the poor prognosis, difficulty in diagnosis and limited therapeutic strategies, several countries have initiated their own national prospective registry to collect data on PAH patients in order to gain more insight on the natural history of PAH.
PAH Registries
As given in Table 1, the clinical characteristics of IPAH patients in the present study were compared with those enrolled in Swiss Registry, SERAPHIN, Assessing the Spectrum of Pulmonary hypertension Identified at a REferral centre (ASPIRE), Pulmonary Hypertension Registry of the United Kingdom and Ireland, Korean Pulmonary arterial Hypertension Registry and the French registry [3,6-10]. Though all the patients in the present study were recruited from a single centre, an attempt to describe the epidemiological features of IPAH from Indian population was made, with only Idiopathic cases being included in this study. The age and sex distribution of Indian cohort was found to be different from that of other registries. The IPAH patients in the present study are much younger (31.2 ± 11.2 yrs) in comparison to the mean age at diagnosis of patients reported by other countries. An explanation for this could be that the genetic constitution of the patients in the Indian subcontinent is substantially diverse and unique, and a compounded effect of the environmental triggers in the early predisposition of the disease can be an alternative explanation. Similar mean age was reported in patients of Japanese registry [11]. Female preponderance was reported in all registries with F:M ratio ranging from 1.5:1 to 6.41:1, except for ASPIRE which reported an F:M ratio of 0.62:1. The Indian cohort reports a sex ratio of 1.26:1, which is the lowest barring ASPIRE. The reason for this may be changes in the lifestyle of women in India compared to the rest of the world. Mean PAP of the present study group was also significantly higher than those of other registries, with the Korean group coming in a close second [6], highlighting the severity and survival state variation of the disease pattern. Establishment of various registries by different countries has enabled to gain information about this disease and design better therapeutic strategies. This comparative study has shown that minor and major differences do exist in different populations, pointing towards the variation in ethnicity with respect to IPAH. For instance, in most of the studies, PAH is detected late in the course of the disease while the mean age of onset in an Indian proband is more than a decade younger. It is observed that a majority of patients belonged to WHO Functional Class III/IV as compared to only 26% of patients in Indian cohort, pointing towards a later discovery of the disease and in advanced stages, which may lead to higher mortality contrary to their Indian counterparts, with the diagnosis being established in patients belonging to WHO Functional Class I/II, with a better survival rate and timely therapeutic management of the disease.
Table 1 Comparison of clinical profile of IPAH across the world.
| Swiss PH registry | SERAPHIN | ASPIRE | UK & Ireland | Korean Pulmonary Arterial Hypertension Registry | French Registry | Present Study | |
|---|---|---|---|---|---|---|---|
| N | 308 | 63 | 175 | 437 | 145 | 264 | 70 |
| Ethnicity | Swiss | Global | Caucasian (92%) | English & Irish | Korean | French | Indian |
| Age | 57 ± 16 | 49.1 ± 17.1 | 55 ± 16 | 50.1 ± 17.1 | 45 ± 15.7 | 50 ± 15 | 31.2 ± 11.2 |
| F:M | 1.5:1 | 6.14:1 | 0.62:1 | 2.37:1 | 2.72:1 | 2.1:1 | 1.26:1 |
| WHO I/II (%) | 25 | 49.1 | - | 15.5 | 36.6 | 25 | 74.3 |
| WHO III/IV (%) | 75 | 51 | 100 | 84.5 | 63.4 | 75 | 25.71 |
| mPAP mmHg | 48 ± 15 | 51.8 ± 17.6 | 53 ± 13 | 54.1 ± 17.1 | 74.1 ± 20.7 | 55 ± 15 | 97.7 ± 23.8 |
Demographic Characteristics
The epidemiological study is comprised of 200 controls and 70 IPAH patients (Table 2). At the time of enrollment into the study, the mean age of patients was 31.2 ± 11.2 yrs (range 10 to 60), while the mean age of controls was 33.4 ± 12.1 yrs. In the IPAH group, males had a mean age of 29 ± 7.6 yrs, while females had a higher mean age of 32.9 ± 13.3 yrs. Patients are generally afflicted in their 3rd-5th decade of life associated with high mortality rates (>50% at five years). The mean age at diagnosis was considered as the mean age at onset (AAO) of the disease, which was observed to be 26.9 ± 10.9 yrs. AAO was lower in men at 25 ± 7.6 yrs as compared to females at 28.5 ± 12.9 yrs (Table 2). The prognosis of the disease is very poor, with the mean survival age being 2-3 years from diagnosis. The lower age and mean age at onset in men compared to women points toward the underlying gender bias and genetic heterogeneity. Other factors such as developmental, anatomical and environmental factors also seem to influence the pattern of IPAH. Usage of tobacco and its products might also be contributing factors in men having a lower age at onset and early predisposition due to environmental triggers.
Table 2 Epidemiological characteristics in IPAH where p value is significant <0.05.
| Control N (%) | IPAH N (%) | χ2 | p value | |
|---|---|---|---|---|
| Total | 200 | 70 | -- | -- |
Gender |
||||
| Male | 100 (50) | 31 (44.3) | 0.68 | 0.41 |
| Female | 100 (50) | 39 (55.7) | ||
| Age (Mean ± SD) | ||||
| Male | 32.3 ± 4.8 | 29. 0 ± 7.6 | -- | -- |
| Female | 35.7 ± 6.5 | 32. 9 ± 13.3 | ||
| Total | 33.4 ± 12.1 | 31.2 ± 11.2 | ||
| Age at Onset (Mean ± SD) | ||||
| Male | -- | 25 ± 7.6 | ||
| Female | -- | 28.5 ± 12.9 | ||
| Total | -- | 26.9 ± 10.9 | ||
| Consanguinity | ||||
| Consanguineous | 30 (15) | 26 (37.1) | 15.46 | 0.000084 |
| Non- Consanguineous | 170 (85) | 44 (62.9) | ||
| Addictions | ||||
| Smokers | 46 (23) | 7 (10) | 5.55 | 0.01 |
| Non-smokers | 154 (77) | 63 (90) | ||
| Alcoholic | 50 (25) | 8 (11.4) | 5.56 | 0.01 |
| Non-alcoholic | 150 (75) | 62 (88.6) | ||
| Sudden Cardiac Death | -- | 29 (41.4) | -- | -- |
| Familial Status | -- | -- | -- | -- |
Medical and Family History
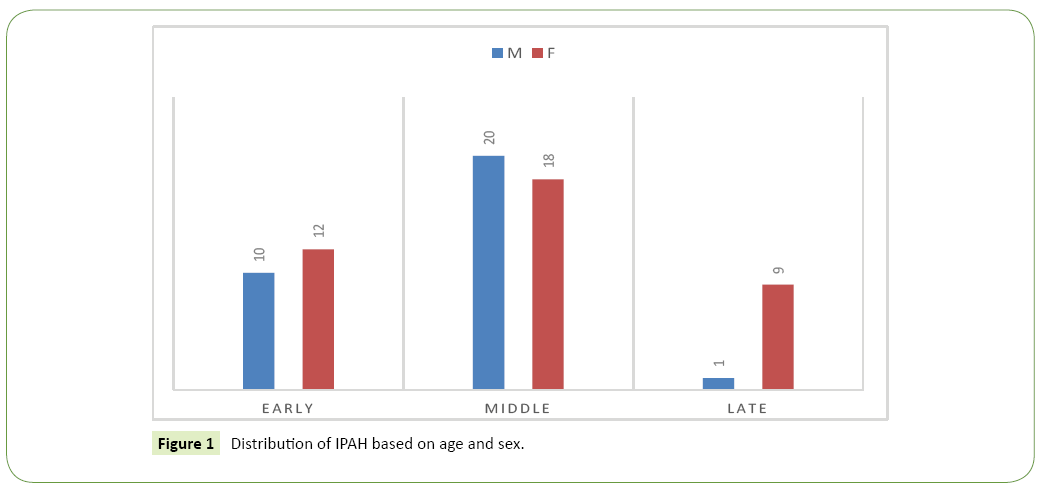
About 10% patients (n=7) reported to be previous or current cigarette smokers/tobacco users, and 11.4% patients (n=8) had a history of alcohol consumption, all of whom were males. Similarly, in the controls, the smokers (n=46) and alcoholics (n=50) were all males, and the difference in numbers between the two groups was significant (χ2, 5.55; p=0.01 and χ2, 5.56; p=0.01). Among the women, only 7.7% (3 of 39) developed the disease during their pregnancy. Family history of sudden cardiac death was present in 41.4% of patients, a high number incidentally, indicating that genetic or environmental variables, common in the family, may segregate in IPAH. Parental consanguinity was observed in 37.1% of cases and 15% of the controls with the difference being significant (χ2, 15.46; p=0.000018). High consanguinity may result in the segregation of recessive alleles harboured in the heterozygous parents/carriers to the off-springs leading to the manifestation of IPAH. None of the patients had a history of familial pulmonary arterial hypertension, although the role of common recessives in disease onset cannot be ruled out, as IPAH is a multifactorial disorder with both environmental and genetic factors contributing to the etiology of IPAH (Table 2). Based on the AAO of the disease, the cohort was subdivided into three groups: early (0- ≤ 20 yrs), middle (21-40 yrs) and late AAO (41-60 yrs). 31.4% of the cases (n=22) belonged to the early AAO class, 54.3% (n=38) belonged to the middle AAO group, and the remaining 14.3% (n=10) belonged to the late AAO class (Figure 1). The highest number of cases belonged to the middle AAO class, which is consistent with findings across the world [10]. Within these classes, the gender distribution (Males vs. Females) was 45.5% vs. 54.6%, and 10% vs. 90% in early and late AAO respectively. As can be seen, the proportion of females is higher in the early and late AAO classes, which perhaps can be attributed to hormonal fluctuations in the female system during menarche and menopause. Contrary to the above findings, the middle AAO group showed a male preponderance (M vs. F: 52.6% vs. 47.4%), a highly contrasting result, since IPAH is considered to affect individuals in 3rd and 4th decade of life, mostly young women [12]. This could be attributed to the fact that males in this age group are more likely to be influenced by stress and extrinsic/intrinsic environmental factors and addictions. The difference in ratio based on AAO suggests the possible role of different etiological agents / triggering factors in the onset of the disease and heterogeneity of the condition. In the present study, the male: female sex ratio was observed to be 1:1.26 which is quite contrary to the high female preponderance reported in IPAH by several studies, wherein the sex ratios varied from 1:1.7 to 1: 4.3 [13]. The reason for female preponderance to IPAH remains speculative, with theories of hormonal imbalances and selective loss of male fetus being suggested [14-16]. Estrogen is known to have an important role to play in vasculogenesis, and its improper functioning during menarche and menopause may lead to symptoms of IPAH, with a heavier hand in women compared to men.
Symptoms
The most common presenting symptom in patients was dyspnea (100%), followed by palpitations (78.6%). The frequency of other symptoms was as follows: presyncope (60%), syncope (48.6%), and angina (45.7%). Only 31.4% of the patients reported symptoms of Paroxysmal Nocturnal Dyspnea (PND); being comparatively high, pointing to the poor prognosis of IPAH (Table 3). Upon comparison of symptoms with respect to gender, it was observed that females predominantly experienced palpitation (52.7 vs. 47.3), angina (65.6 vs. 34.4), syncope (55.9 vs. 44.1) and presyncope (54.8 vs. 45.2), while a higher number of males experienced PND (54.5 vs. 45.5) than females. This may be a result of the compounded effect of genetic factors and environmental triggers, as it is known that women are predominantly affected by IPAH when compared to men. The World Health Organization classification of functional capacity, an adaptation of the New York Heart Association (NYHA) system, is helpful for qualitative assessment of activity tolerance of patients and useful in monitoring disease progression and response to treatment [13]. Assessment of the functional class (FC) has also been shown to have a prognostic significance [12]. The WHO Functional classification of PAH is now based on a modification of the NYHA system and takes syncope into account as a marker of functional status with a formal assessment of exercise capacity as an integral part of the evaluation of PAH. The functional status of the patients at diagnosis according to the WHO classification was as follows: 1.4% of the patients belonged to class I, 72.9% to class II, and 25.7% to class III (Table 4) which indicates that the patients are referred after 3 yrs of presenting symptoms and less awareness of the condition as some of the symptoms relate to asthmatic attacks. On examining the gender distribution with respect to the functional class, both genders predominantly belonged to Class II, although a greater number of female patients belonged to class III (61.1 vs. 38.9). This could be because of late diagnosis of female patients compared to males, at a stage when the disease progression occurs quickly.
Table 3 Frequency of symptoms presented in IPAH.
| Symptoms | Pooled N (%) | Males N (%) | Females N (%) |
|---|---|---|---|
| PND | 22 (31.4) | 12 (54.5) | 10 (45.5) |
| Palpitation | 55 (78.6) | 26 (47.3) | 29 (52.7) |
| Angina | 32 (45.7) | 11 (34.4) | 21 (65.6) |
| Syncope | 34 (48.6) | 15 (44.1) | 19 (55.9) |
| Pre-syncope | 42 (60) | 19 (45.2) | 23 (54.8) |
Table 4 Classification of IPAH into WHO functional class.
| Symptoms | Pooled N (%) | Males N (%) | Females N (%) |
|---|---|---|---|
| Dyspnea | 70 (100) | 31 (100) | 39 (100) |
| Functional Class I | 1 (1.4) | -- | 1 (2.6) |
| Functional Class II | 51 (72.9) | 24 (47.1) | 27 (52.9) |
| Functional Class III | 18 (25.7) | 7 (38.9) | 11 (61.1) |
ECG Findings
ECG is carried out to screen for a spectrum of anatomic, cardiac and arrhythmic problems, but its sensitivity to serve as an effective screening tool for PAH is still a dogma. However, in known IPAH cases, ECG contributes for monitoring and prognostic information [17]. Right ventricular hypertrophy may be demonstrated in IPAH by ECG. The incidence of right-axis deviation was observed in 82.3% of patients, incomplete to complete Right Bundle Branch Blockage in 30% of patients, while T wave inversions (V1 to V5, and V1 to V6) was observed in 47.7% of the cases. Other ECG changes that were present in a few patients are ST-T changes in II and III AVF, Sinus tachycardia, Sinus bradycardia and Sinus rhythm. A completely normal ECG was exhibited in a single case. The parameters of ECG reflect the severity and prognosis status of an IPAH proband.
Echocardiography Findings
Doppler echocardiography is performed to evaluate the level of RVSP and to assess the presence of associated anatomic abnormalities such as right atrial enlargement, right ventricular enlargement, and pericardial effusion [18]. The pulmonary artery pressure (sPAP) is considered equal to right ventricular systolic pressure (RVSP) in the absence of pulmonic valve stenosis or outflow tract obstruction. 2-D echocardiography findings in majority of patients revealed enlarged or dilated right atrium and ventricle and dilated pulmonary artery. Moderate to severe RV dysfunction was also seen in many cases. No thrombus formation was observed in any of the patients evaluated. All the cases exhibited normal LV function. Narrowed vascular lumen, vasoconstriction and increased pulmonary vascular resistance play a prominent role in about 20% cases of IPAH. Any change in vessel wall architecture would lead to increased resistance to blood flow and pulmonary arterial pressures. In general, the mean RVSP value was found to be 97.7 ± 23.8 mmHg; while in males, it was found to be 100.3 ± 24.5 mmHg, and 95.6 ± 23.3 mmHg in females. The Tricuspid regurgitation velocity (TR velocity) was found to be 4.5 ± 0.6 m/sec; with respect to gender, males exhibited a TR velocity of 4.5 ± 0.6 m/sec while females showed 4.4 ± 0.7 m/sec as given in Table 5. Higher RVSP and TR velocity are indicative of severity and poor prognosis in males compared to women, indicating a multifactorial mode of inheritance wherein the less affected sex (males) exhibit symptoms related to poor survival, prognosis, and severity. Hence, the threshold of parameters can be seen and is in corroboration with inheritance patterns. RVSP levels and TR velocities were estimated in the patients based on WHO functional capacity (Table 6). The RVSP levels were highest in patients with WHO class III functional capacity (100.5 ± 20.7 mmHg). A decrease in RVSP values was seen in patients with lower functional class. On the other hand, comparison of TR velocities among different functional classes showed a similar distribution across functional classes II and III, viz., 4.5 ± 0.7 m/sec and 4.4 ± 0.6 m/sec respectively. This is in accordance with the disease, as the severity of the disease increases in patients belonging to higher WHO functional class, and thus, higher RVSP and TR velocities.
Table 5 Mean RVSP values and TR velocities in IPAH.
| RVSP (mm Hg) X ± S.D. | TR velocity (m/sec) X ± S.D. | |
|---|---|---|
| Males | 100.3 ± 24.5 | 4.5 ± 0.6 |
| Females | 95.6 ± 23.8 | 4.4 ± 0.7 |
| Pooled | 97.7 ± 23.8 | 4.5 ± 0.6 |
Table 6 Mean RVSP values and TR velocities in IPAH based on WHO Functional Capacity.
| WHO Functional Class | N | RVSP (mm Hg) X ± S.D. | TR velocity (m/sec) X ± S.D. |
|---|---|---|---|
| I | 1 | 90 | 4.3 |
| II | 51 | 96.8 ± 25.1 | 4.5 ± 0.7 |
| III | 18 | 100.5 ± 20.7 | 4.4 ± 0.6 |
Conclusion
In conclusion, the cohort of the present study suggests that IPAH shows a highly variable clinical course with respect to different populations and highlights the need to understand/ identify the etiological agents/triggering factors and genetic factors in different ethnic groups that influence the expression of the disease and its clinical outcome. IPAH is the result of an interaction between a predisposing state and an inciting stimulus [19,20]. The multiple hits may consist of interactions of a genetic substrate with either a) a genetic condition such as a mutation or polymorphism, b) a coexisting disease or c) an environmental exposure. This promotes/warrants the need to strategize appropriate management of the condition based on ethnicity and other variables.
References
- Fonseca GHH, Souza R, Salemi VMC, Jardim CVP, Gualandro SFM (2012) Pulmonary hypertension diagnosed by right heart catheterisation in sickle cell disease. ERJ Open Res 39: 112-118.
- Badesch DB, Raskob GE, Elliott CG, Krichman AM, Farber HW, et al. (2010) Pulmonary arterial hypertension: Baseline characteristics from the REVEAL registry. Chest Journal 137: 376-387.
- Humbert M, Sitbon O, Chaoua A, Bertocchi M, Habib G, et al. (2006) Pulmonary arterial hypertension in France: Results from a national registry. Am J Respir Crit Care Med 173: 1023-1030.
- Frost AE, Badesch DB, Barst RJ, Benza RL, Elliott CG, et al. (2011) The Changing Picture of Patients With Pulmonary Arterial Hypertension in the United States. Chest Journal 139: 128-137.
- Yigla M, Kramer MR, Bendayan D, Reisner SA, Solomonov A (2004) Unexplained severe pulmonary hypertension in the elderly: report on 14 patients. Isr Med Assoc J 6: 78-81.
- Chung WJ, Park YB, Jeon CH, Jung JW, Ko KP, et al. (2015) Baseline Characteristics of the Korean Registry of Pulmonary Arterial Hypertension. Journal of Korean Medical Science 30: 1429-1438.
- Hurdman J, Condliffe R, Elliot CA, Davies C, Hill C, et al. (2012) ASPIRE registry: Assessing the Spectrum of Pulmonary hypertension Identified at a REferral centre. ERJ Open Res 39: 945-955.
- Ling Y, Johnson MK, Kiely DG, Condliffe R, Elliot CA, et al. (2012) Changing Demographics, Epidemiology, and Survival of Incident Pulmonary Arterial Hypertension. Am J Respir Crit Care Med 186: 790-796.
- Mueller-Mottet S, Stricker H, Domeninghetti G, Azzola A, Geiser T, et al. (2015) Long-Term Data from the Swiss Pulmonary Hypertension Registry. Respiration 89: 127-140.
- Simonneau G, Channick RN, Delcroix M, Galiè N, Ghofrani HA, et al. (2015) Incident and prevalent cohorts with pulmonary arterial hypertension: insight from SERAPHIN. ERJ Open Res 46: 1711-1720.
- Okada O, Tanabe N, Yasuda J, Yoshida Y, Katoh K, et al. (1999) Prediction of life expectancy in patients with primary pulmonary hypertension. A retrospective nationwide survey from 1980-1990. Internal Medicine 38: 12-26.
- D’Alonzo GE, Barst RJ, Ayres SM, Bergofsky EH, Brundage BH, et al. (1991) Survival in patients with primary pulmonary hypertension. Results from a national prospective registry. Annals of Internal Medicine, 115: 343-349.
- Rich S, Rubin LJ, Abenhail L (1998) Executive summary from the World Symposium on Primary Pulmonary Hypertension. The World Health Organization publication via the Internet.
- Fuster V, Steele PM, Edwards WD, Gersh BJ, McGoon MD, et al. (1984) Primary pulmonary hypertension: natural history and the importance of thrombosis. Circulation 70: 580-587.
- Kleiger RE, Boxer M, Ingham RE, Harrison DC (1976) Pulmonary hypertension in patients using oral contraceptives. A report of six cases. Chest 69: 143-147.
- Loyd JE, Butler MG, Foroud TM, Conneally PM, Phillips JA, et al. (1995) Genetic anticipation and abnormal gender ratio at birth in familial primary pulmonary hypertension. Am J Respir Crit Care Med 152: 93-97.
- Henkens IR, Gan CTJ, van Wolferen SA, Hew M, Boonstra A, et al. (2008) ECG Monitoring of Treatment Response in Pulmonary Arterial Hypertension Patients. CHEST Journal, 134: 1250.
- Galiè N, Torbicki A, Barst R, Dartevelle P, Haworth S, et al. (2004) Guidelines on diagnosis and treatment of pulmonary arterial hypertension. The Task Force on Diagnosis and Treatment of Pulmonary Arterial Hypertension of the European Society of Cardiology. Eur Heart J 25: 2243-2278.
- Machado RD, James V, Southwood M, Harrison RE, Atkinson C, et al. (2005) Investigation of second genetic hits at the BMPR2 locus as a modulator of disease progression in familial pulmonary arterial hypertension. Circulation 111: 607-613.
- Yuan JXJ, Rubin LJ (2005) Pathogenesis of pulmonary arterial hypertension: the need for multiple hits. Circulation 111: 534-538.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences