Digital Gangrene as the Initial Presentation of Lupus Nephritis
B. Padmapriya, M. Edwin Fernando*, S. Thirumalvalavan and K. Thirumalvalavan
Department of Nephrology, Government Stanley Medical College, Chennai, India
- *Corresponding Author:
- M. Edwin Fernando
Department of Nephrology, Government Stanley Medical College, Chennai, India
E-mail:nephroeddy@gmail.com
Received date: June 06, 2024, Manuscript No. IPJRM-24-19150; Editor assigned date: June 08, 2024, PreQC No. IPJRM-24-19150 (PQ); Reviewed date: June 22, 2024, QC No. IPJRM-24-19150; Revised date: March 14, 2025, Manuscript No. IPJRM-24-19150 (R); Published date: March 21, 2025, DOI: 10.36648/IPJRM.8.2.51
Citation: Padmapriya B, Fernando ME, Thirumalvalavan S, Thirumalvalavan K (2025) Digital Gangrene as the Initial Presentation of Lupus Nephritis. J Ren Med Vol:8 No:2
Abstract
Systemic Lupus Erythematosus (SLE) is an autoimmune disease that can affect any organ, but SLE presenting with digital gangrene is very rare, less than 0.2%. Digital gangrene is a very serious manifestation as it may lead to ischemic necrosis and amputation. Digital gangrene is due to poor perfusion of digits, usually caused by peripheral vascular disease, vasculitis or vasospasm. This is a case report of a 50-year-old female who initially developed gangrene of the hands and feet, later presenting with rapidly progressing renal failure. Her diagnostic and therapeutic challenges were due to her atypical presentation and coexistent sepsis.
Keywords
Systemic Lupus Erythematosus (SLE); Digital Gangrene (DG); Cryoglobulinemia; Renal biopsy
Introduction
SLE is an autoimmune connective tissue disorder that can present in many ways. It affects almost all organs, including renal, cardiac, hematological, and pulmonary systems. In this condition, skin involvement is the most common manifestation.
But digital gangrene is rare in SLE as an initial presentation, it is less than 0.2%. Here, we are presenting one of such rare cases [1].
Case Presentation
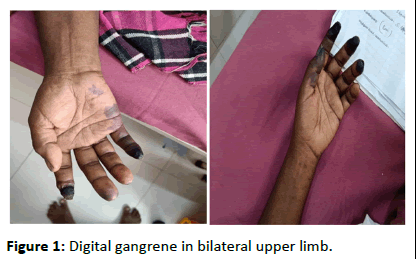
A 50-year-old lady with no pre-existent comorbidities developed hyperpigmentation of face and Blebs, gangrene of digits of hands and feet for 2 months for which she took treatment from local hospital. She presented to us with anuria and renal failure for one day. She was having gangrene of hands and feet with hyperpigmentation of face. On evaluation she was having renal failure with Cr of 6, Hb of 9.6, total wbc count initially was 16000. As her renal failure worsened she was initiated on haemodialysis. Initially possibility of scleroderma, MCTD, cryoglobulinemia, medium vessel vasculitis was considered due to gangrene. She was started on pulse steroid, heparin, plasmapheresis. On further evaluation ANA (IF) was 3+ positive (1:100 dilution), ANA profile-anti sm positive, APLA work up and cryoglobulinemia work up negative, she was stabilised and renal biopsy done showed crescentic glomerulonephritis showing 100% crescents and IF positive for IgG 3+ IgM C3 and c1q positive with features suggestive of class IV lupus nephritis. Further her anti PR3ANCA-neg, anti MPOweakly positive. Further she developed sepsis and septic shock and was started on IV antibiotics and inotropes. Her treatment for lupus nephritis was challenged due to underlying sepsis (CRP 300). Because of sepsis she was not a candidate for immunosuppression and for her aggressive lupus nephritis/ coexistent vasculitis she was treated with high dose IVIG. Her general condition improved; she was still dialysis dependent. Planned for immunosuppression once sepsis subsides, unfortunately patient attender not willing to continue the treatment and went on against medical advice, later we came to know she expired (Figures 1 and 2).
Figure 1: Digital gangrene in bilateral upper limb.
Figure 2: Digital gangrene in bilateral lower limb.
• CBC: TC 15000 DC: 95/2.3
• Hb: 9 gms
• MCV 81
• Platelet count 3.5 lakhs
• RFT: U 174 Cr 6.7, Na-133, K-3.5
• Urine routine could not be done.
• LFT: T.B–1.4 OT/PT 22/19 T.P 4.9 ALB 2.1
• PT/INR 15/1.1
• Lipid profile: TC 197 TGL 252
• CT chest: Normal
• ABG: pH 7.1 PCO 50 HCO 13 Ag 23
• CRP–235
• ANA–Positive (IF-1:100)
• RF–Negative
• ENA profile–Anti SM/nRNP positive
• Anti PR3 negative anti MPO–Weakly positive
• Anti LKM–Negative
• B2GP and ACL–Negative LA–Negative
• Cryoglobulin–Negative
• Echo: Normal
• CT abdomen: Fatty liver, moderate ascites
• ESR: 60 MM/HR
• TFT: TSH–1.1 IU/ML, FT3-2.29 pg/ml, FT4-1.02 ng/dl
• SR: Calcium-8.4 PO4-9 UA-5.5
• Viral markers–Negative
• Doppler scan: RT and LT upper and lower limb normal study
• Fundus normal
• C3-Low C4 low
Renal biopsy
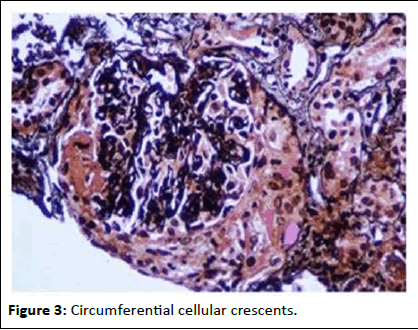
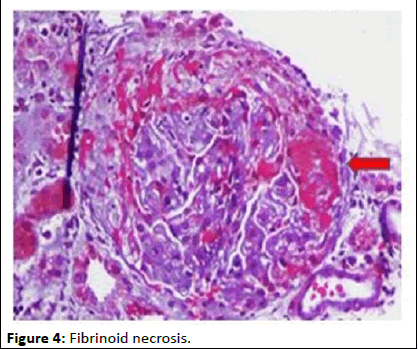
• LM: No sclerosis/7 glomeruli. Cellular crescents compressing capillary tuft in all glomeruli. Bowmans capsule rupture in 1 gi. Fibrinoid necrosis of tuft in 2 gi. No wireloop rhyaline thrombus. RBC cast in many tubules. Lymphatic infiltration in interstitium. No IF TA.
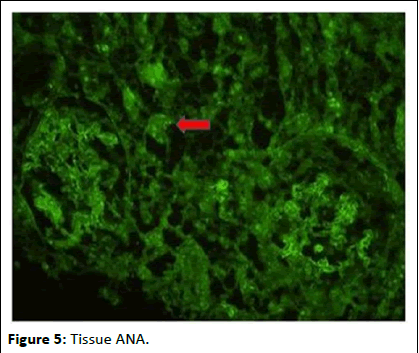
• IF: IgG3+C3 3+Cq 1+ on mesangium and glomerular capillary loops (Figures 3-5).
• IgG+ on tubular epithelial cell nuclei (Tissue ANA).
Diagnosis: Lupus nephritis class IV
Figure 3: Circumferential cellular crescents.
Figure 4: Fibrinoid necrosis.
Figure 5: Tissue ANA.
Discussion
Systemic Lupus Erythematosus (SLE) is an autoimmune disease affecting multiple organs and systems, characterized by an autoimmune response to nuclear antigens [2]. Young women are most likely affected by this disease. The pathophysiological mechanisms of digital gangrene in SLE are complex, involving thromboembolism, premature atherosclerosis, vasospasm, hypercoagulability, and vasculitis [3]. Among the cutaneous manifestations of SLE, digital gangrene is considered to be very rare. The most common cause of digital gangrene in SLE may be due to antiphospholipid syndrome, as SLE is the most common underlying disease of secondary APS. One form of SLE that was described frequently in patients with digital gangrene is Antiphospholipid Syndrome (APS). The digital gangrene in SLE appears to be rare after the age of 50 years [4]. The first case was described by Vocks, et al. in a 59-year-old female patient [5]. The second was reported by Nagai, et al. in a 50-year-old female patient followed for SLE since the age of 32 years with cutaneous, hematological, and neurological involvement [6]. With a cumulative incidence of 1.3%, digital gangrene is rare,but it is a very severe complication of SLE. It is the initial manifestation of the disease in only 0.2% of cases [7].
In 2009, a total of 2,684 patients with lupus were screened, and only 18 patients were found to have digital necrosis [8]. On a large study done on a cohort of lupus patients, seven out of 485 patients had evidence of digital gangrene [9]. Liu, et al. reported that the risk of digital amputation declines after early high-dose corticosteroid treatment [10]. Out of 344 patients, 20 cases of digital gangrene had also been reported among the Indian population in 2009, Out of these 20 patients digital gangrene as an initial presentation in 10 patients, the median duration of onset of the other 10 patients was 31.5 months. It shows that the prevalence of digital gangrene as an initial presentation is slightly higher in the Indian population [11].
Rosato et al. claimed that acute digital gangrene is never the first presentation of SLE [12].
In their study that was conducted in 1962, Dubois and Arterberry found that the latent period between diagnosing SLE and developing digital gangrene was from 1 to 18 years where Raynaud`s phenomenon preceded the digital gangrene [13].
Other predictive factors that were described in the literature include a long-standing history of SLE and elevated C-serum Reactive Protein (CRP) [14,15].
Conclusion
So, all these previous reports show Digital gangrene seen mostly at the late stage of this disease, and predictive factors for developing digital gangrene in SLE include long duration of disease, Raynaud phenomena, high CRP, and the presence of APS antibodies. Our case was unique in many ways: The age of the patient is not consistent with the age that was mostly reported, she had no previous episodes of Raynaud’s phenomenon and the only risk factor she had was high CRP, Overlap of lupus ANCA association is only 20%. In our case prominent 100% crescent formation and worse prognosis may be due to ANCA association, but it is still unclear whether or not the clinical outcomes of patients with crescentic glomerulonephritis differs according to ANCA association. Jarrot, et al. found that SLE associated with AAV may be a group of diseases called SLE/AAV overlapping syndrome. In Multiple Autoimmune Syndrome (MAS) with SLE background, Autoimmune Thyroid Disease (AITD), Sjogren's syndrome, and antiphospholipid antibody syndrome were most common, whereas vasculitis was rare [15]. Martin-Nares, et al. estimated the frequency of overlap between AAV and ADs.
During her hospital stay, she developed sepsis, which complicated the disease and posed a dilemma in managing immunosuppression.
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the forms, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Financial Support and Sponsorship
Nil
Conflict of Interest
There are no conflicts of interest.
References
- Boussaid S, Majdouba MB, Rekik S, Jemmali S, Zouaoui K, et al. (2022) Case Report: Extensive digital gangrene as a primary manifestation of late-onset systemic lupus erythematosus. F1000Res 11
[Crossref] [Google Scholar] [PubMed]
- Liu A, Zhang W, Tian X, Zhang X, Zhang F, et al. (2009) Prevalence, risk factors and outcome of digital gangrene in 2684 lupus patients. Lupus 18:1112-1118
[Crossref] [Google Scholar] [PubMed]
- Jeffery RC, Narshi CB, Isenberg DA (2008) Prevalence, serological features, response to treatment and outcome of critical peripheral ischaemia in a cohort of lupus patients. Rheumatology 47:1379-1383
[Crossref] [Google Scholar] [PubMed]
- Narshi C, Jeffery R, Isenberg DA (2009) Comment on: Prevalence, serological features, response to treatment and outcome of critical peripheral ischaemia in a cohort of lupus patients. Rheumatology 48:452-453
[Crossref] [Google Scholar] [PubMed]
- Rosato E, Molinaro I, Pisarri S, Salsano F (2011) Digital ulcers as an initial manifestation of systemic lupus erythematosus. Intern Med 50:767-769
[Crossref] [Google Scholar] [PubMed]
- Dubois EL, Arterberry JD (1962) Gangrene as a manifestation of systemic lupus erythematosus. JAMA 181:366-374
[Crossref] [Google Scholar] [PubMed]
- Herrick AL (2011) Contemporary management of Raynaud's phenomenon and digital ischaemic complications. Curr Opin Rheumatol 23:555-561
[Crossref] [Google Scholar] [PubMed]
- Yang S, Zhou J (2023) Systemic lupus erythematosus and antineutrocytic cytoplasmic antibody-associated vasculitis overlap syndrome presenting mainly with alveolar hemorrhage: A case report and literature review. Medicine 102:e36356
[Crossref] [Google Scholar] [PubMed]
- Hai A, Aslam M, Ashraf TH (2012) Symmetrical peripheral gangrene: A rare presentation of antiphospholipid syndrome. Intern Emerg Med 7:71-73
[Crossref] [Google Scholar] [PubMed]
- Vocks E, Welcker M, Ring J (2000) Digital gangrene: A rare skin symptom in systemic lupus erythematosus. J Eur Acad Dermatol Venereol 14:419-421
[Crossref] [Google Scholar] [PubMed]
- Nagai Y, Shimizu A, Suto M, Tanaka S, Yasuda M, et al. (2009) Digital gangrene in systemic lupus erythematosus. Acta Derm Venereol 89:398-401
[Crossref] [Google Scholar] [PubMed]
- Achour A, Mankaï A, Thabet Y, Sakly W, Braham F, et al. (2012) Systemic lupus erythematosus in the elderly. Rheumatol Int 32:1225-1229
[Crossref] [Google Scholar] [PubMed]
- Adelowo O, Olaosebikan H, Ajani W, Omosebi DT (2012) Digital gangrene as the initial presentation of systemic lupus erythematosus. BMJ Case Rep 2012:bcr2012006259
[Crossref] [Google Scholar] [PubMed]
- Jarrot PA, Chiche L, Hervier B, Daniel L, Vuiblet V, et al. (2016) Systemic lupus erythematosus and antineutrophil cytoplasmic antibody-associated vasculitis overlap syndrome in patients with biopsy-proven glomerulonephritis. Medicine 95:e3748
[Crossref] [Google Scholar] [PubMed]
- Rojas-Villarraga A, Amaya-Amaya J, Rodriguez-Rodriguez A, Mantilla RD, Anaya JM (2012) Introducing polyautoimmunity: Secondary autoimmune diseases no longer exist. Autoimmune Dis 2012:254319
[Crossref] [Google Scholar] [PubMed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences