Current Knowledge, Attitude, and Practices towards Anthrax Infection Prevention among Community Members and Professionals in Sodo Zuriya District of Wolaita Zone, Southern Ethiopia/2021
Amare Abota Asha1, Liang Song2 and Wan Cheng Song 3*
1School of Public Health, Southern Medical University, Guangzhou, China
2School of Public Health, Southern Medical University, Guangzhou, China
3Department of Microbiology, School of public health, Southern Medical University, Guangzhou 510515, China
- *Corresponding Author:
- Prof. Wan Cheng Song
Department of Microbiology,
Southern Medical University,
Guangzhou 510515,
China,
Tel: 8620-13392127658;
E-mail: gzwcs@smu.edu.cn
Received Date: June 11, 2021 Accepted Date: June 25, 2021 Published Date: July 02, 2021
Citation: Asha AA, Liang S, Wan CS (2021) Current Knowledge, Attitude, and Practices towards Anthrax Infection Prevention among Community Members and Professionals in Sodo Zuriya District of Wolaita Zone, Southern Ethiopia/2021. J Zoonotic Dis Public Health Vol.5 No.4: 10.
Abstract
Background: Ethiopia is predominantly vulnerable to zoonotic diseases like anthrax; about 80% of households directly contact animals, creating an opportunity spread of disease. Anthrax is an endemic disease throughout the country. Despite this, there is a scarcity of information related to knowledge and other human behavioral practices towards anthrax infection among different community members at a country level and particularly in this study area.
Objective: This study aims to assess the current Knowledge Attitude and Practices (KAP) towards anthrax prevention amongst community members (livestock owners, consumers) and professionals (medical and veterinary) in Sodo Zuriya District of Wolaita Zone, Southern Ethiopia.
Methodology: Community-based cross-sectional study was conducted among livestock owners, consumers, and professionals from October 01/2020-April 30/2021. A structured questionnaire was used to assess the KAP of the 384 study participants aged 18- >60 years old within selected PA’s/Kebeles of the study area. Data were collected via questioners administered through personal face-to-face interviews, entered into an MS Excel spreadsheet, and then exported to SPSS version 26 for further analysis.
Results: The overall knowledge level of community members was 64% and professionals 91% regarding awareness of the disease, its cause, zoonotic nature, preventability, and knowledge on at least one (clinical symptoms, mode of transmission, and possible prevention methods) of the disease both in humans and animals. Livestock owners who had never been to school were found to be 4.4 times less knowledgeable about anthrax than those who had completed 1st degree and above level education (OR: 0.12; 95% CI: 0.001-0.146; p < 0.001). Similarly, farmers had good knowledge about the disease in compression with the self-employed workers (OR: 9.34; 95% CI: 3.34-26.0; p < 0.001). In consumers lower knowledge level related to anthrax infection was seen in age group 18-35 years old (OR: 0.095; 95% CI: 0.24– 0.38; p = 0.001) and in illiterate (OR: 0.246; 95% CI: 0.125– 0.48; p < 0.001) individuals; when compared to age category > 60 years old and one who achieved a 1st degree and above level of education. And the association was statistically significant. Most community members were involved in risky practices such as consumption of raw meat (82.4%), improper carcass disposal (36.7%), seldom using PPE (67%), and habit of home slaughter (76%).
Conclusion: This study demonstrates better knowledge but a low level of the desired attitude and existence of high-level risky practices among community members associated with human and animal anthrax within the study area.
Keywords
Anthrax prevention, raw-meat-consumption, Knowledge-attitudepractice, Ethiopia
Introduction
Background
Ethiopia has the 2nd largest human population in Africa and the largest livestock population on the continent [1]. The country is mainly vulnerable to zoonotic diseases because its economy is primarily dependent on agriculture. About 80% of households directly contact domestic animals, creating an opportunity for infection and spread of disease [2]. Zoonosis is any disease or condition naturally transmissible from vertebrate animals to humans and vice-versa [3]. Anthrax is a potentially fatal naturally occurring infectious zoonotic disease of warm-blooded animals that primarily affects herbivorous mammals [4]. Anthrax is known by several names worldwide, such as charbon, wool sorter’s disease, rag pickers’ disease, malignant carbuncle, malignant pustule, and Siberian ulcer [5]. Due to its widespread distribution and its potential use as a biological weapon (bioterrorism), anthrax is also believed as a global public health threat [6]. It has a disproportionate impact on the livelihood of livestock owners. Mainly, the public health and livestock product quantity and quality in impoverished rural communities in anthrax-endemic countries are severely affected, resulting in devastating economic loss and loss of livestock product market due to reduced consumer confidence [7]. However, many of those affected countries have inadequate and unorganized anthrax prevention programs/strategies [8]. In endemic areas, the massive mortality rate of animals can disturb the subsistence livelihood for families and distress the local agricultural sector [8].
Anthrax is an endemic/prevalent disease in Ethiopia, which occurs every summer (May and June) and reaches an overwhelming occurrence rate in years with heavy rainfall every year (“anthrax season”) in several farming zones of the country and causing disease both in humans and animals. In Ethiopia, one previous study indicated that anthrax is the most important zoonotic disease, second to rabies, which is dealt with by one health approach [1]. Though suspected human and livestock anthrax cases are reported from several country districts, few of those were officially confirmed by relevant government institutions (laboratories) [9]. The occurrence of disease outbreaks in a particular location mostly depends on interacting factors; stated unique characteristics of the bacterium, environmentally related features, animal densities, and human activities. In Ethiopia, raw and undercooked meat consumption and low awareness about anthrax have enhanced the risk of contracting the disease [10,11].
In Ethiopia, explicitly in the southern part, research was not done to understand the knowledge, attitudes, and practices towards anthrax prevention and control measures among different community members. Moreover, most anthrax prevention and control activities depended on managing an outbreak, including treating sick animals and vaccination of animals at risk [8]. Most of the available publications in the county dealt about the clinical and epidemiological aspect of the disease, rather than human behavior. This study assessed current knowledge, attitude, and practices towards human and animal anthrax prevention among the community members (livestock owners, consumers), medical and veterinary health professionals in the Sodo Zuriya District of Wolaita Zone Southern Ethiopia. The findings of this study may give pertinent information to the Federal, local governments, and other relevant organizations for the development of strategies and policies that positively impact human behaviors regarding anthrax and other zoonotic disease prevention and control activities.
Statement of the problem
Anthrax continues to persist globally, with an estimated 20,000 to 100,000 incidence cases yearly, and it is highly affecting rural areas in developing nations like Ethiopia [12]. In Ethiopia, human behavior plays a crucial role in the persistence of anthrax due to animals are an essential asset to society. There is a cultural practice of consuming raw (uncooked) meat in every corner of the country. Most community members share the same shelter with animals. Consequently, the death of an animal causes consumption of infected meat and use of animal products, which potentially lead to infections.
Moreover, the level of understanding, attitudes, and practices towards human and animal anthrax infection among different community members are not well studied at country basses, particularly in the study area. Hence, this study aims to generate information related to anthrax infection prevention through assessing current knowledge, attitude, and practices among Community members and professionals) in Sodo Zuria District of Wolaita Zone, Southern Ethiopia, through a cross-sectional quantitative study.
Objectives
General objective: To determine the current knowledge, attitudes, and practices towards human and animal anthrax prevention amongst community members (livestock owners, consumers), medical, and veterinary health professionals in Sodo Zuriya District of Wolaita Zone, Southern Ethiopia.
Specific objectives:
• To determine the current knowledge related to anthrax prevention and control activities amongst community members and experts in the study area.
• To interpret the attitudes towards anthrax infection prevention among community members and professionals
• To assess the existing detrimental practices among study participants that might enhance the probability of contracting the disease
• To recommend measures to improve the control of animal anthrax and the prevention of human anthrax.
Operational definitions
Kebele: The smallest administrative unit of Ethiopia, 4th level administrative division of the regional government, similar to a ward or PA (Peasants Association), a neighborhood or a localized and delimited group.
Wereda: The 3rd level administrative division of the regional state in the Ethiopian context, it is more extensive than Kebele and smaller than Zone, similar to the district.
Zone: It is the 2nd level administrative division of the regional state in Ethiopia, larger than wereda but smaller than the Regional State.
Community member: It infers respondents (aged ≥ 18 years) who participated in the questionnaire surveys (which include livestock owners and animal product consumers). It is only used to differentiate attendants who are not medical or veterinary professionals.
Consumer: it refers to a person who uses meat and other animal products as a food source.
Attitudes: This is a positive or negative evaluation of something, like people, objects, or ideas. In this study, the concepts used to refer to the feelings of community members and professionals towards anthrax and how it is perceived as a public and animal health problem.
Medical professionals: Include all human health workers such as; doctors, clinicians, nurses, and community health workers
Knowledge: In this study, knowledge means awareness of or knowing the disease anthrax, its cause, clinical symptoms, route of transmission, and available prevention mechanisms.
Practices: actual action and or behaviors of community members and professionals undertaking to avoid contracting the human and animal anthrax infection
Veterinary professional: In the case of this study, it refers to veterinarians and assistant veterinarians who work in governmental institutions supporting animal health.
Materials and Methods
Study design
A cross-sectional quantitative study was done to assess the current knowledge, attitude, and practices towards human and animal anthrax infection prevention among community members and professionals. The community-based structured questioner survey was conducted within selected PA’s of Sodo Zuria District of Wolaita Zone, Southern Ethiopia.
Study area and period
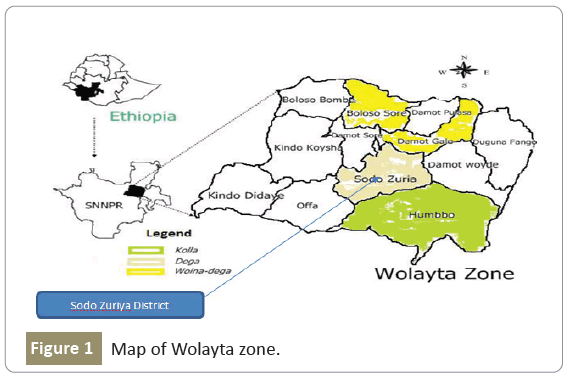
Sodo Zuriya district is one of the districts in Wolaita Zone, Southern Ethiopia. The district is subdivided into 19 kebeles (the smallest administrative unit in Ethiopia) and surrounded by the East and North-East by Damot Woyede and Damot Galle Districts, in the South by Humbo and Offa Districts, in the West, Northwest, and Southwest by Kindo Koyisha, Boloso Sore, and Offa Districts, respectively. It is located at an altitude of 1500-2958 meters above sea level, and its annual rainfall ranges from 1200 mm to 1300 mm. Geographically, the district is located approximately between 60 50’N-70 53’N latitudes and 370 36’ E-370 53’ E longitudes. Agro-ecologically characterized as woynadega (Midland-87%) and Dega (Highland-13%). It is located at 327 kms (Kilometers), far from Addis Ababa, the capital city of Ethiopia,and 160 kms from Hawassa, the regional capital. Based on the last 2007 census, it had a total population of 162,691, of whom 80,022 were men and 82,689 women [13]. A community-based cross-sectional study was conducted among livestock owners, consumers, and professionals from October 01/2020-April 30/2021 (Figure 1).
Sample size determination
A total of 10 kebeles (PA’s) were selected from the 19 kebeles found in the district using the lottery method. The sample size was calculated using the single population proportion formula [14] that is
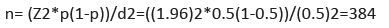
This is by considering the following assumptions: there has been no previous study on the knowledge, attitude and anthrax prevention practices in the study area and recent study conducted in the northern Ethiopia shows magnitude of knowledge of anthrax prevention among livestock owners was found to be 55.8%, the sample size was calculated by considering the assumptions of 50% prevalence, 95% confidence interval (Z=1.96) and 5% margin of error (d=0.05) revealed=384 [40]. A systematic random sampling method was used to select 384 participants, of whom 240 were livestock owners, 102 were consumers, and 42 were and medical and vet professionals) from 10 selected kebeles. In addition, for community members (livestock owners and consumers), the sampling interval (K) was determined by using the data obtained from the Kebele administration office and the initial assessment result. Among professionals, those at work duty and volunteer to fill questioner were selected by lottery method during data collection.
Sampling technique and source of data
Primary data was collected using a pre-tested questionnaire. Furthermore, to keep the consistency, the questionnaire was first translated from English to Amharic (national language), then to a local language called “Wolaitta,” and finally retranslated to English by a professional translator. Data was collected through an interview-administered structured questionnaire. The questionnaires were focusing on;
a) Socio-demographic characteristic of the respondent (such as; sex, age, educational attainments, occupation, profession,residence, religion), animal ownership, the purpose of animal husbandry, and source of information
b) Knowledge questions (e.g., knowing the disease, its cause, clinical symptoms, mode of transmission, prevention and control measures of human and animal anthrax),
c) Attitude assessing questions (e.g., considering anthrax as community problem or not, the importance of vaccination, recalling outbreak occurrence time, medical and vet professional’s exposure to the causative agent, the direct impact of Bacillus anthracis spore in animals and humans, meat inspection related questions) and
d) Community practices (e.g., husbandry, meat consumption, timely vaccination) towards human and animal anthrax infection in the study area.
Moreover, it contains three type of questioners; type I, prepared for livestock owners, type II, medical and veterinary professionals, and type III for animal product consumers. Questioners for livestock owners and professionals almost similar, with minimal differences between them, whereas it incorporates more technical points for medical and vet workers regarding the disease. Questionnaires for consumers were also similar to the other two types, but it emphasizes attitudes towards meat inspection and consumption practices. Besides, one-day intensive training on the study’s objective and the confidentiality of information was given to data collectors and supervisors.
The relevant secondary data related to both animal and human anthrax were collected from Zonal Health Department and Zonal livestock and fishery resource development department of Wolaita Zone with their corresponding offices at the district level. And population data were obtained from the Ethiopian Central Statistics Agency database. Other important information’s related to the topic abstracted from several known published articles and unpublished papers.
Quality management
A pre-test was conducted in selected kebeles among livestock owners, consumers, and professionals. Five percent of the total sample size was chosen to standardize the questionnaires. Identified problems during the pre-test were corrected before starting actual data collection. Data collection was crosschecked daily for their extensiveness, reliability and accuracy by the principal investigator. The reliability of the study results was assured by implementing quality control measures during the pre-analytical, analytical, and post-analytical quality control steps.
Data processing and analysis
Data collected from questioner survey was edited, cleaned, and entered into an MS excel sheet and exported to a Statistical Package for Social Science (SPSS) version 26 for further analysis. Descriptive statistics such as frequencies and proportions were computed to summarize the variables. The logistic regression model was used for some selected knowledge-related variables in the process. A p-value of less than 0.05 at the bivariate and multivariable logistic regression analysis was considered statistically significant.
Ethical considerations
The ethical approval of this study was obtained from the institutional ethical review committee of Southern Medical University, School of public health. Permission letters were obtained from the regional Livestock and Fishery Resources Development Bureau, Wolaita Zone Livestock and Fishery Resources Development department, and Sodo Zuriya District (Health office, Livestock and Fishery Resources Development office) the research was carried out. The purpose of the study was clearly explained to all livestock owners, consumers, and professionals of study participants before obtaining a verbal/ written informed consent.
Study participants
All livestock owners, consumers, and veterinary and medical professionals who were selected to participate in this study and filled the questionnaire during the data collection period.
Inclusion and exclusion criteria
Inclusion criteria: Livestock owners, consumers, and veterinary and medical professionals who had lived in the study area for more than six months before the commencement of this study volunteered to participate in the study and gave consent and assent were included.
Exclusion criteria: Attendants aged below 18 years, respondents who were unable or refused to respond to the questionnaire and with any social and physical condition that would limit the ability to participate in the study during data collection were excluded from the study.
Study variables
Independent variables: socio-demographic characteristics (e.g., gender, age, level of education, occupation, profession, residence, and religion), animal ownership were used as independent variables.
Dependent variables
Knowledge on anthrax: Knowing the disease, its cause, clinical symptoms, mode of transmission, prevention and control measures of human and animal anthrax.
Attitude towards anthrax: Assessing anthrax as community problem or not, the importance of vaccination, recalling outbreak occurrence time, medical and vet professional’s exposure to the causative agent, the direct impact of Bacillus anthracis spore in animals and humans, meat inspection related questions).
Community practices: Husbandry practices, meat consumption, timely vaccination, use of PPE, use of lime while burying the carcass was analyzed.
Results
Socio-demographic information’s of the participants
A total of 384 community members (livestock owners and consumers) and professionals (veterinarians and medical experts) have participated in this study with the proportion of 240 (62.5%),102 (26.5%), and 42 (11%) respectively. Most of the respondents were males, which accounts for 68.8% (264) of the total surveyed 384 participants and the remaining 31.2% (120) were females. This result is in line with the fact that men dominate the country’s livestock industry, especially large animals. The majority of the study population was in the age group of 36-60 (56.8%) years, indicating that livestock owners were mainly adults. More than two-thirds of 169 (44%) of respondents were urban dwellers preceded by peri-urban 123 (32%), and the remaining 92 (24%) were rural inhabitants. The majority of participants attained primary 81 (21%) and secondary 79 (20.57%) education. A more significant proportion of the study population were farmers, 187 (49%), mainly dependent on mixed crop-livestock farming. Most (52%) respondents were Protestant Christians, 43% were Orthodox Christians, and the remaining 5% comprised (Catholic 4% and 1% Muslims) (Table 1).
| Characteristics | Category | Livestock owners n=240 | Consumers n=102 | Professionals n=42 | Cumulative | ||||
|---|---|---|---|---|---|---|---|---|---|
| Frequency | % | Frequency | % | Frequency | % | Frequency | % | ||
| Sex | Male | 166 | 69 | 71 | 69.6 | 27 | 64 | 264 | 69 |
| Female | 74 | 31 | 31 | 30.4 | 15 | 36 | 120 | 31 | |
| Age | 18-35 | 77 | 32 | 44 | 43.1 | 25 | 59.5 | 146 | 38 |
| 36-60 | 150 | 63 | 51 | 50 | 17 | 40.5 | 218 | 57 | |
| Above 60 | 13 | 5 | 7 | 6.9 | - | - | 20 | 5 | |
| Education | Illiterate | 39 | 17 | 18 | 17.6 | - | - | 57 | 15 |
| Informal | 37 | 15 | 8 | 7.8 | - | - | 45 | 12 | |
| Primary and Junior | 58 | 24 | 23 | 22.5 | - | - | 81 | 21 | |
| Secondary | 57 | 24 | 22 | 21.7 | - | - | 79 | 21 | |
| Diploma | 32 | 13 | 14 | 13.7 | 14 | 33 | 60 | 16 | |
| Degree and above | 17 | 7 | 17 | 16.7 | 28 | 67 | 62 | 16 | |
| Occupation | Farmer | 150 | 63 | 37 | 36.3 | 187 | 49 | ||
| Employee | 34 | 14 | 24 | 23.5 | 42 | 100 | 100 | 26 | |
| Unemployed | 21 | 9 | 22 | 21.6 | - | - | 43 | 11 | |
| self- employed | 35 | 14 | 19 | 18.6 | - | - | 54 | 14 | |
| Profession | AHP | - | - | - | - | 22 | 52 | 22 | 52 |
| HHP | - | - | - | - | 20 | 48 | 20 | 48 | |
| Religion | Protestant | 117 | 49 | 52 | 51 | 31 | 74 | 200 | 52 |
| Orthodox | 116 | 48 | 41 | 40.2 | 9 | 21 | 166 | 43 | |
| Muslim | 1 | 0.5 | 2 | 2 | 0 | 0 | 3 | 1 | |
| Catholic | 6 | 2.5 | 7 | 6.9 | 2 | 5 | 15 | 4 | |
| Residence | Urban | 94 | 39 | 56 | 54.9 | 19 | 45 | 169 | 44 |
| Peri-urban | 76 | 32 | 31 | 30.4 | 16 | 38 | 123 | 32 | |
| Rural | 70 | 29 | 15 | 14.7 | 7 | 17 | 92 | 24 | |
| Livestock Ownership | Yes | 240 | 100 | - | - | - | - | 240 | 62 |
Table 1: Socio-demographic information of study participants.
Livestock ownership and purpose of animal husbandry
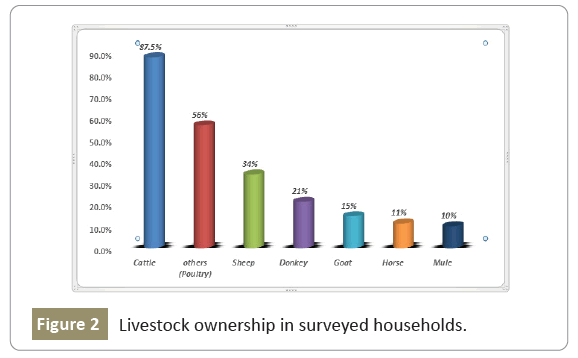
From a total of 384 participants, 240 (62.5%) community members were livestock owners. Many animal species were found in the surveyed households, including cattle, sheep, goats, poultry donkeys, horses, and mule (Figure 2).
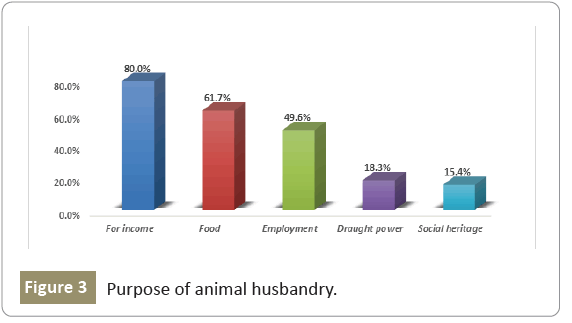
The multiple response question results revealed that cattle (87.5%), poultry (56%), and sheep (34%) were the most commonly kept species. Donkeys, Goats, horses, and mules were also popular but at a lower frequency. Most livestock owners were kept animals for income and food (mainly for meat and milk). Moreover, some others raise animals for employment, draught power use (especially equines), and social heritage for pleasure (Figure 3).
Source of information
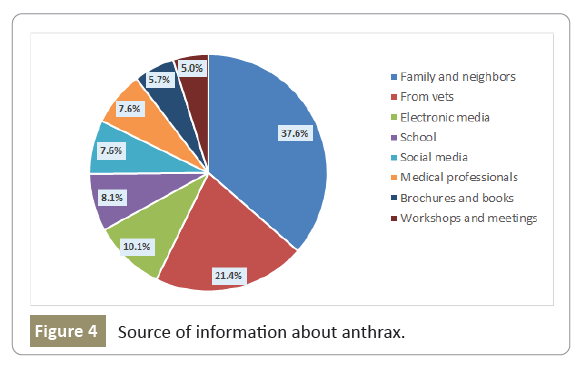
The typical source of information about anthrax was through personal contacts within community members (families, friends, and neighbors, 37.6). While 21.4% of respondents received information about the disease from animal health professionals, 10.1% from electronic media (like TV and radio), and 8.1% were studied at school. Some others were informed through social media (7.6%), human health professionals (7.6%), various books and brochures (5.7%), and the remaining respondents from different meetings and workshops (5%) (Figure 4).
Livestock owner’s knowledge (heard about anthrax, its cause and preventability)
Most livestock owners, 77% (184/240), heard about the disease anthrax, and they locally called it “Duluwa,” but 23% of participants didn’t know the disease. Although more than half of livestock owners, 54% (130/240), knew the cause of anthrax was germs, but 44% of participants did not know the cause of the disease. About 20% of respondents said that a spider bite could cause an anthrax infection, 17% believed it was God-given, and 7% thought it was a manifestation of an evil spirit. Of the 240 respondents, 155(65%) knew anthrax is a preventable disease, 85(35) claimed that it is not preventable condition (Table 2).
| Have you heard about the disease called anthrax? (n=240) | Cause of anthrax (n=240) | Do you think anthrax is a preventable disease? (n=240) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Yes (n, %) | No (n, %) | Germs | Evil spirit | God given | Spider bite | Do not know | Yes | No | |
| (n, %) | (n, %) | (n, %) | (n, %) | (n, %) | (n/%) | (n/%) | ||||
| Sex (n=240) | Male | 132/79 | 34/21 | 92/55 | 13-Aug | 33/20 | 25/15 | 03-Feb | 117/70 | 49/30 |
| Female | 52/70.3 | 22/29.7 | 38/51 | 04-May | 08-Nov | 23/31 | 01-Feb | 38/51 | 36/49 | |
| Total | 184/77 | 56/23 | 130/54 | 17-Jul | 41/17 | 48/20 | 04-Feb | 155/65 | 85/35 | |
| Age (n=240) |
18-35 | 60/78 | 17/22 | 39/51 | 08-Oct | 15/19.5 | 15/19.5 | 0(0) | 38/49 | 39/51 |
| 36-60 | 113/75 | 37/25 | 84/56 | 08-May | 25/17 | 29/19 | 04-Mar | 106/71 | 44/29 | |
| > 60 | Nov-85 | Feb-15 | 7/53.8 | 1/7.7 | 1/7.7 | 4/30.8 | 0/0 | Nov-85 | Feb-15 | |
| Total | 184/76.7 | 56/23.3 | 130/54 | 17-Jul | 41/7 | 48/20 | 04-Feb | 155/65 | 85/35 | |
| Education (n=240) | Illiterate | 24/61.5 | 15/38.5 | 15/38.5 | 03-Aug | Jul-18 | 14/36 | 0 | 18/46 | 21/54 |
| Informal | 26/70 | Nov-30 | 18/49 | 03-Aug | Jul-19 | Sep-24 | 0 | 22/60 | 15/40 | |
| Grade 1-8 | 42/72 | 16/28 | 25/43 | 05-Sep | 18/31 | Sep-16 | 01-Feb | 38/65 | 20/35 | |
| Grade 9-2 | 48/84 | Sep-16 | 37/65 | 0 | 07-Dec | Nov-19 | 02-Apr | 39/68 | 18/32 | |
| Diploma | 28/87.5 | 4/12.5 | 23/72 | 4/12.5 | 0 | 4/12.5 | 01-Mar | 23/72 | Sep-28 | |
| Degree and above | 16/94 | 01-Jun | Dec-70 | 02-Dec | 02-Dec | 01-Jun | 0 | 15/88 | 02-Dec | |
| Total | 184/76.7 | 56/23.3 | 130/54 | 17-Jul | 41/7 | 48/20 | 04-Feb | 155/65 | 85/35 | |
| Occupation (n=240) | Farmer | 121/81 | 29/19 | 75/50 | 09-Jun | 30/20 | 32/21 | 04-Mar | 96/64 | 54/36 |
| Employee | 30/88 | 04-Dec | 24/70.6 | 5/14.7 | 4/11.8 | 01-Mar | 0 | 24/71 | Oct-29 | |
| Unemployed | 13/62 | Aug-38 | 14/66.7 | 0 | 2/9.5 | 5/23.8 | 0 | 14/67 | Jul-33 | |
| Self- employed | 20/57 | 15/43 | 17/48.6 | 3/8.6 | 5/14.3 | 10/28.6 | 0 | 21/60 | 14/40 | |
| Total | 184/77 | 56/23.3 | 130/54 | 17-Jul | 41/7 | 48/20 | 04-Feb | 155/65 | 85/35 | |
| Urban | 73/78 | 21/22 | 54/57.4 | 3/3.2 | 5/5.3 | 29/31 | 03-Mar | 55/58 | 39/42 | |
| Peri-urban | 56/74 | 20/26 | 39/51.3 | 4/5.3 | 21/27.6 | 11/14.5 | 1/1.3 | 55/72 | 21/28 | |
| Rural | 55/79 | 15/21 | 37/52.9 | 10/14.3 | 15/21.4 | 8/11.4 | 0 | 45/64 | 25/36 | |
| Total | 184/77 | 56/23.3 | 130/54.2 | 17-Jul | 41/17 | 48/20 | 4/1.7 | 155/65 | 85/35 | |
| Religion (n=240) | Protestant | 94/80 | 23/20 | 59/60 | 10/8.6 | 27/23 | 19/18.4 | 01-Jan | 80/68 | 37/32 |
| Orthodox | 87/75 | 29/25 | 68/58 | 06-May | 13-Nov | 27/23 | 03-Mar | 73/63 | 43/37 | |
| Muslim | 0 | 1/100 | 1/100 | 0 | 0 | 0 | 0 | 1/100 | 0 | |
| Catholic | Mar-50 | Mar-50 | Feb-33 | Jan-17 | Jan-17 | Feb-33 | 0 | Jan-17 | May-83 | |
| Total | 214/89 | 26-Nov | 130/54.2 | 17/7.1 | 41/17 | 48/20 | 4/1.7 | 155/65 | 85/35 | |
Table 2: Animal owner’s Knowledge (knew anthrax, its cause and preventability).
A logistic regression model was used to determine the effect of socio-demographic factors (such as sex, age, level of education, occupation, residence, and religion) on the knowledge of anthrax in general, its cause, and preventability. Hence, level of education and type of occupation had a statistically significant association with knowledge of the disease. Respondents who had never been to school (illiterates) were found to be 4.4 times less knowledgeable about anthrax than those who had completed a first degree and above level education (OR: 0.12; 95% CI: 0.001- 0.146; p<0.001). Similarly, farmers had good knowledge about the disease when compared with the self-employed (merchants, artisan, daily labor) (OR: 9.34; 95% CI: 3.34-26.0; p<0.001). Whereas gender, age, residence, and religion had not been found statistically significant related to knowledge of anthrax.
Moreover, regarding knowledge on the preventability of the disease, gender, age, and level of education showed a statistically significant relation. Male respondents knew more about whether the condition is preventable or not when compared to their counterparts (females) with (OR: 2.0; 95% CI: 1.087-3.689; p=0.026), participants with younger age 18-35 years old (OR: 0.78; 95% CI: 0.15-0.419; p=0.003) and illiterate (OR: 0.62; 95% CI: 0.01-0.340; p=0.001) had lower knowledge on the preventability of the disease than those who aged above 60 years old and had a high level of education (completed the first degree and above) respectively.
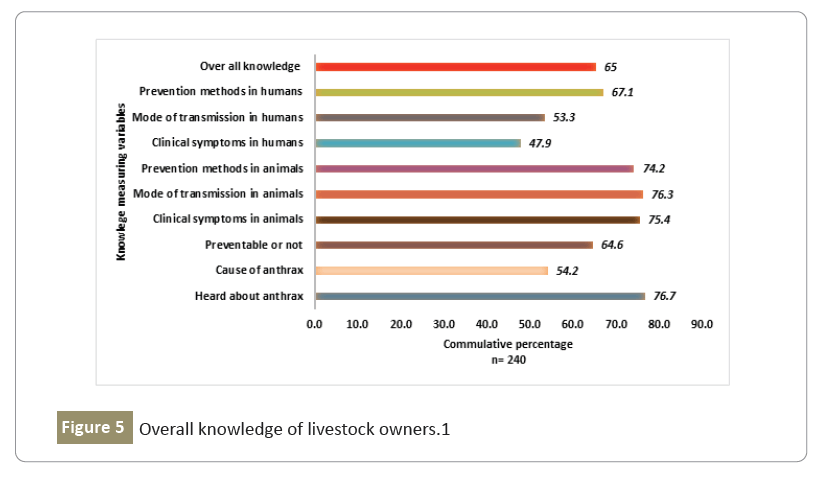
Overall Knowledge of livestock owners
The overall knowledge of livestock owners regarding heard about anthrax, cause, its preventability, and knowledge of at least one (clinical symptoms, mode of transmission, and possible prevention methods) of the disease both in humans and animals was found to be 65% (Figure 5).
Consumer’s knowledge (heard about anthrax, zoonotic nature and preventability)
Of the total of 102 potential animal product consumers in Sodo Zuriya district, 76(74.5%) had heard about anthrax (locally known as ‘Duluwa’) but, 26(25.5%) of them did not know the disease. About 64 (63%) of the participants mentioned that anthrax could have been transmitted from animals to humans. However, 38(37%) of the respondents did not know whether it is transmissible or not. Furthermore, more than half of participants, 61(60%), believed that anthrax is a preventable disease; nonetheless, 41(40%) consumers did not know it is preventable or not (Table 3).
| Variable | Have you heard about the disease called anthrax? (n=102) | knowledge on zoonotic feature(n=102) | Do you think anthrax is a preventable disease? (n=102) | ||||
|---|---|---|---|---|---|---|---|
| Yes (n/%) | No (n/%) | Yes (n/%) | No (n/%) | Yes (n/%) | No (n/%) | ||
| Sex (n=102) | Male | 57(80) | 14(20) | 43(61) | 28(39) | 46(65) | 25(35) |
| Female | 19(61) | 12(39) | 21(68) | 10(32) | 15(48) | 16(52) | |
| Total | 76(74.5) | 26(25.5) | 64(63) | 38(37) | 61(60) | 41(40) | |
| Age (n=102) | 18-35 | 28(64) | 16(36) | 29(66) | 15(34) | 27(61) | 17(39) |
| 36-60 | 41(80) | 10(20) | 32(68) | 19(37) | 31(61) | 20(39) | |
| > 60 | 7(100) | 0 | 3(43) | 4(57) | 3(43) | 4(57) | |
| Total | 76(74.5) | 26(25.5) | 64(63) | 38(37) | 61(60) | 41(40) | |
| Education (n=102) | Illiterate | 8(44) | 10(56) | 6(33) | 12(67) | 6(33) | 12(67) |
| Informal | 4(44) | 5(56) | 3(33) | 6(67) | 5(56) | 4(44) | |
| Primary and Junior | 16(70) | 7(30) | 12(52) | 11(48) | 9(39) | 14(61) | |
| Secondary | 18(86) | 3(14) | 16(76) | 5(24) | 12(57) | 9(43) | |
| Diploma | 13(93) | 1(7) | 11(79) | 3(21) | 12(86) | 2(14) | |
| Degree and above | 17(100) | 0 | 16(94) | 1(6) | 17(100) | 0 | |
| Total | 76(74.5) | 26(25.5) | 64(63) | 38(37) | 61(60) | 41(40) | |
| Occupation (n=102) | Farmer | 24(65) | 13(35) | 18(49) | 19(51) | 18(49) | 19(51) |
| Employee | 24(100) | 0 | 21(87.5) | 3(12.5) | 22(92) | 2(8) | |
| Unemployed | 16(73) | 6(27) | 18(82) | 4(18) | 10(45.5) | 12(54.5) | |
| Self employed | 12(63) | 7(37) | 7(37) | 12(63) | 11(58) | 8(42) | |
| Total | 76(74.5) | 26(25.5) | 64(63) | 38(37) | 61(60) | 41(40) | |
| Residence (n=102) | Urban | 41(73) | 15(27) | 39(70) | 17(30) | 34(61) | 22(39) |
| Peri-urban | 27(87) | 4(13) | 17(55) | 14(45) | 21(68) | 10(32) | |
| Rural | 8(53) | 7(47) | 8(53) | 7(47) | 6(40) | 9(60) | |
| Total | 76(74.5) | 26(25.5) | 64(63) | 38(37) | 61(60) | 41(40) | |
| Religion (n=102) | Protestant | 42(81) | 10(19) | 36(69) | 16(31) | 31(60) | 21(40) |
| Orthodox | 27(66) | 14(34) | 21(51) | 20(49) | 24(58.5) | 17(41.5) | |
| Muslim | 2(100) | 0 | 1(50) | 1(50) | 2(100) | 0 | |
| Catholic | 5(71) | 2(29) | 6(86) | 1(14) | 4(57) | 3(43) | |
| Total | 76(74.5) | 26(25.5) | 64(63) | 38(37) | 61(60) | 41(40) | |
Table 3: Consumers knowledge (anthrax, zoonotic nature and preventability).
Age (OR: 0.095; 95% CI: 0.24-0.38; p=0.001) and education level (OR: 0.246; 95% CI: 0.125-0.48; p<0.001) found to be statistically significant. Hence, lower knowledge level related to anthrax infection was seen in age group 18-35 years old and in illiterate individuals; when compared to age category above 60 years old and one who achieved a first degree and above level of education. On the other hand, education (OR: 0.495; 95% CI: 0.35-0.70; p<0.001), (OR: 0.433; 95% CI: 0.29-0.65; p<0.001) found to be the only statistically significant predictor for knowledge of zoonotic nature of the disease and whether knowing it is preventable or not respectively. The other demographic variables such as gender, occupation, residence, and participants’ religion were not statistically significant (p>0.05). However, as the education level increased, the odds of awareness about anthrax, zoonotic nature, and prevention measures increased significantly (p<0.05).
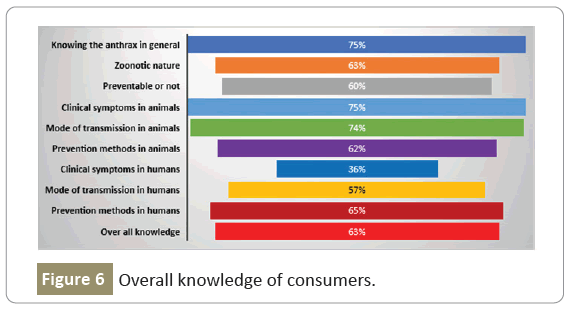
Overall knowledge of consumers
The overall knowledge of consumers regarding heard about anthrax, cause, zoonotic nature, and knowledge of at least one (clinical symptoms, mode of transmission, and possible prevention methods) of the disease in humans and animals was 63% (Figure 6).
Professionals’ knowledge (etiology, zoonotic nature and preventability)
The majority of professionals, 90.5% (38/42), knew the cause of anthrax as bacteria, but the remaining 9.5% of respondents claimed that the virus caused it. Similarly, a higher proportion 83% (35/42) of experts declared that anthrax is transmitted from animals to humans. In contrast, seventeen percent of them believed that it has not zoonotic importance. Even though eighty- eight percent (37/42) of human and animal health professionals thought that anthrax is preventable, the rest, 12%, recognized it as an unpreventable condition (Table 4).
| Variable | Knowledge of etiology | Knowledge of zoonotic nature | Do you think anthrax is a preventable disease? | ||||
|---|---|---|---|---|---|---|---|
| Bacteria (n/%) | Virus (n/%) | Yes (n/%) | No (n/%) | Yes (n/%) | No (n/%) | ||
| Sex (n=42) | Male | 26(96) | 1(4) | 26(96) | 1(4) | 24(89) | 3(11) |
| Female | 12(80) | 3(20) | 9(60) | 6(40) | 13(93) | 2(7) | |
| Total | 38(90.5) | 4(9.5) | 35(83) | 7(17) | 37(88) | 5(12) | |
| Age(n=42) | 18-35 | 23(88.5) | 3(11.5) | 22(85) | 4(15) | 23(85.5) | 3(11.5) |
| 36-60 | 15(94) | 1(6) | 13(81) | 3(19) | 14(87.5) | 2(12.5) | |
| Total | 38(90.5) | 4(9.5) | 35(83) | 7(17) | 37(88) | 5(12) | |
| Education | Diploma | 10(71) | 4(27) | 10(71) | 4(29) | 12(86) | 2(14) |
| Degree | 22(100) | 0 | 19(86) | 3(14) | 19(86) | 3(14) | |
| Msc and above | 6(100) | 0 | 6(100) | 0 | 6(100) | 0 | |
| Total | 38(90.5) | 4(9.5) | 35(83) | 7(17) | 37(88) | 5(12) | |
| Profession (n=42) | Vet | 21(95.5) | 1(4.5) | 19(86) | 3(14) | 20(91) | 2(9) |
| Medical worker | 17(85) | 3(15) | 16(80) | 4(20) | 17(85) | 3(15) | |
| Total | 38(90.5) | 4(9.5) | 35(83) | 7(17) | 37(88) | 5(12) | |
| Residence (n=42) | Urban | 18(95) | 1(5) | 17(89.5) | 2(10.5) | 17(89.5) | 2(10.5) |
| Peri-urban | 14(87.5) | 2(12.5) | 12(75) | 4(25) | 13(81) | 3(19) | |
| Rural | 6(86) | 1(14) | 6(86) | 1(14) | 7(100) | 0 | |
| Total | 38(90.5) | 4(9.5) | 35(83) | 7(17) | 37(88) | 5(12) | |
| Religion (n=42) | Protestant | 28(90) | 3(10) | 25(81) | 6(19) | 28(90) | 3(10) |
| Orthodox | 7(87.5) | 1(12.5) | 8(100) | 0 | 7(50) | 1(50) | |
| Catholic | 3(100) | 0 | 2(67) | 1(33) | 2(67) | 1(33) | |
| Total | 38(90.5) | 4(9.5) | 35(83) | 7(17) | 37(88) | 5(12) | |
Table 4: Professionals Knowledge (etiology, zoonotic nature, and preventability).
Male participants, aged 36-60 years old, and respondents who completed the first degree and above level education had better knowledge than females, 18-35 years old, and diploma holders. Moreover, veterinarians and experts who work around urban areas better understand (cause, zoonotic nature, and preventability) of the disease than medical professionals and experts who work around rural areas. A logistic regression model was used to determine a statistical association between socio- demographic factors and the three (etiology, zoonotic nature, & preventability) knowledge variables. None of them was found to be statistically significant.
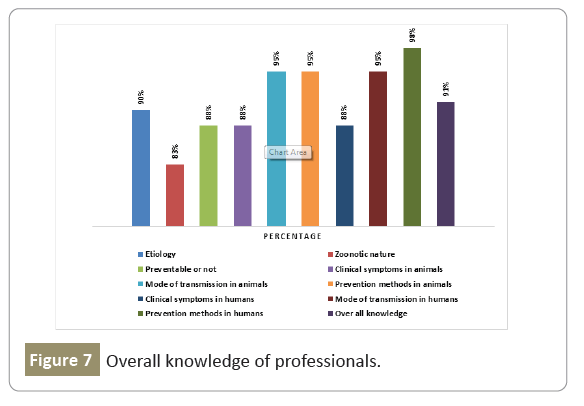
Overall knowledge of medical and veterinary professionals
The general knowledge of experts regarding the cause, zoonotic nature, preventability, and knowledge of at least one (clinical symptoms, mode of transmission, and possible prevention methods) of the disease in humans and animals was 91% (Figure 7).
Participant’s knowledge related to animal anthrax
Respondents were assessed by basic knowledge questions related to the disease, such as clinical symptoms, transmission mode, and prevention measures.
Livestock owners: the number of livestock owners’ who knew one or more right symptoms, transmission ways, or control/prevention methods of anthrax in animals was 75.4% (181/240), 76.3% (183/240), and 74.2% (178/2400), respectively. Respondents who did not know clinical symptoms, transmission ways, or control/prevention means of anthrax were 24.6% (59/240), 23.8% (57/240), and 25.8% (62/240) respectively. Sudden death was the most selected choice from the list of clinical symptoms provided in the questionnaire for animal owners and answered by 181 out of 240 participants. Similarly, the most responded answer regarding the transmission mode was ‘ingesting blood- contaminated grass’ 123 (51.3%) participants selected it, and ‘burry all anthrax suspected carcass’ 138 (57.7%) reported most from a list of anthrax prevention methods question by livestock owners. Nonetheless, seventy-five (31.3%) participants believed that animal anthrax could be prevented using traditional medicine.
Consumers: When asked about the clinical signs, ways of transmission, and prevention methods of animal anthrax, 76(74.5%), 75(73.5%) and 63(61.8%) respondents knew one or more exact clinical symptoms, transmission ways of the disease and knowledge about prevention means of animal anthrax respectively. Surprisingly, above 41% of animal product consumers believed that anthrax could be prevented using traditional medicines (Table 5).
| Variable | Knowledge of etiology | Knowledge of zoonotic nature | Do you think anthrax is a preventable disease? | |||
|---|---|---|---|---|---|---|
| Frequency (n=240) | % | Frequency (n=42) | % | Frequency (n=102) | % | |
| Do you know the clinical symptoms of anthrax in animals? | ||||||
| Yes | 181 | 75 | 37 | 88 | 76 | 74.5 |
| NO | 59 | 25 | 5 | 12 | 26 | 25.5 |
| Clinical symptoms of anthrax in animals (Ç?, Ỹ) | ||||||
| Sudden death | 181 | 75 | 33 | 78.6 | 66 | 64.7 |
| Bleeding from natural orifices | 74 | 31 | 28 | 66.7 | 56 | 54.9 |
| Unclotted dark red blood | 63 | 26 | 20 | 47.6 | 59 | 57.8 |
| Incomplete rigor mortis | 55 | 23 | 13 | 31 | 53 | 52 |
| Do you know the transmission routes of anthrax in animals? | ||||||
| Yes | 183 | 76 | 40 | 95.2 | 75 | 73.5 |
| NO | 57 | 24 | 2 | 4.8 | 27 | 26.5 |
| Anthrax transmission in animals (Ç?, Ỹ) | ||||||
| By licking other sick animals | 125 | 52 | 18 | 42.9 | 35 | 34.3 |
| By ingesting blood contaminated grass | 123 | 51 | 33 | 78.6 | 43 | 42.2 |
| Through drinking contaminated water | 101 | 42 | 19 | 45.2 | 43 | 42.2 |
| By licking anthrax dead bones | 104 | 43 | 27 | 64.3 | 41 | 40.2 |
| Through contaminated soil | 108 | 45 | 26 | 61.9 | 42 | 41.2 |
| Via flies | 95 | 40 | 11 | 26.2 | 39 | 38.2 |
| Do you know the prevention measures of anthrax in animals? | ||||||
| Yes | 178 | 74 | 40 | 95.2 | 63 | 61.8 |
| NO | 62 | 26 | 2 | 4.8 | 39 | 38.2 |
| Anthrax prevention in animals (Ç?,Ỹ) | ||||||
| Burn all suspected anthrax animal carcasses | 91 | 38 | 32 | 76.2 | 63 | 61.8 |
| Bury all suspected anthrax carcasses | 138 | 58 | 30 | 71.4 | 62 | 60.8 |
| Vaccinate animals | 125 | 52 | 39 | 88.1 | 63 | 61.8 |
| Using Traditional medicine | 75 | 31 | 4 | 9.5 | 42 | 41.2 |
(Ç?) This symbol denotes multiple answers allowed and (Ỹ) this symbol refers to – the question was asked only if participants indicated that ‘yes,’ for knowledge questions
Table 5: Knowledge of anthrax among participants reported having heard about the anthrax in the Sodo Zuriya District, Southern Ethiopia, 2021.
Professionals: The proportion of veterinarians and medical professionals who indicate one or more correct symptoms, transmission ways, and prevention methods of anthrax in animals were 37(88.1%), 40(95.2%), and 40(95.2%), respectively. About twelve percent of respondents did not know clinical signs or symptoms of the disease in animals, and only 4.8% did not know about the transmission and prevention methods. Crucially Sudden death (78.6%) and ingestion of blood (spore) contaminated grass (78.6%) and animal vaccination (88.1%) were highly reported symptoms, transmission routes, and prevention measures of anthrax respectively. Surprisingly, 5(9.5%) of animal and human health professionals believe that herbal or traditional medication plays an essential role in anthrax prevention.
Comparing participants’ knowledge about clinical symptoms, transmission modes, and prevention methods of animal anthrax within three categories (i.e., livestock owners, consumers, and professionals) showed a statistically significant association. Professionals had better awareness than livestock owners and consumers. Professionals found to be (OR: 7.2; 95% CI: 1.628-31.84 p=0.009) seven times better knowledgeable than consumers regarding transmission modes of anthrax in animals. Similarly, they had twelve times (OR: 12. 381; 95% CI: 2.832- 54.129; p=0.001), two times (OR: 1.777; 95% CI: 1.086-2.910; p=0.001) better knowledge related to anthrax prevention measures than consumers and animal owners’ respectively.
Whereas there was no statistically significant relationship found among three categories when comparing knowledge related to clinical symptoms of anthrax in animals.
Participant’s knowledge related to human anthrax
In this survey, respondents evaluated by basic knowledge assessing questions related to the disease, such as knowledge on clinical symptoms, mode of transmission, and prevention measures of anthrax in humans.
Livestock owners: Though one hundred fifteen (48%) animal owners highlighted at least one correct answer about the clinical symptoms or signs of anthrax in humans, above half (52%) of the study population did not know the clinical symptoms of the disease. Among clinical symptoms skin rash/wound was the most prominent known clinical sign indicated by all 100% (115/115) participants who knew symptoms of the disease in humans. More than half a proportion of 53.3%, 67% of respondents indicated one or more transmission methods and prevention methods of anthrax in humans, respectively. The most frequently responded transmission route of anthrax from animals to humans was through consumption of dead animal meat/carcass 99% (127/128) and avoid skinning of anthrax dead cadaver was found to be the most frequently answered prevention method by 99% (160/161) interviewers (Table 6).
| Variable | Knowledge of zoonotic nature | Knowledge of zoonotic nature | Knowledge of zoonotic nature | |||
|---|---|---|---|---|---|---|
| Frequency (n=240) | % | Frequency (n=42) | % | Frequency (n=102) | % | |
| Do you know the transmission routes of anthrax in animals? | ||||||
| Yes | 115 | 47.9 | 37 | 88.1 | 37 | 36.3 |
| No | 125 | 52.1 | 5 | 11.9 | 65 | 63.7 |
| Clinical symptoms of anthrax in humans (Ç?, Ỹ) |
n=115 | n=37 | n=37 | |||
| Fever and excessive sweating | 76 | 66 | 27 | 73 | 34 | 92 |
| Skin rash/wounds | 115 | 100 | 29 | 78 | 35 | 95 |
| Cough | 75 | 65 | 11 | 30 | 26 | 70 |
| GIT symptoms (diarrhea, vomiting) | 72 | 63 | 21 | 57 | 21 | 57 |
| Irritability | 64 | 56 | 10 | 27 | 24 | 65 |
| Do you know the transmission routes of anthrax? | ||||||
| Yes | 128 | 53.3 | 40 | 95.2 | 58 | 56.9 |
| No | 112 | 46.7 | 2 | 4.8 | 44 | 43.1 |
| Anthrax transmission routes in humans (Ç?, Ỹ) |
n=128 | n=40 | n=58 | |||
| While slaughtering and skinning the dead animal |
127 | 99 | 29 | 73 | 58 | 100 |
| Handling hides, wool, or hair of dead animals | 115 | 90 | 27 | 68 | 56 | 97 |
| Consuming dead animal meat | 122 | 95 | 34 | 85 | 57 | 98 |
| Handling infected carcass or bone | 97 | 76 | 22 | 55 | 52 | 90 |
| Do you know the control measures of anthrax? | ||||||
| Yes | 161 | 67.1 | 41 | 97.6 | 66 | 64.7 |
| No | 79 | 32.9 | 1 | 2.4 | 36 | 35.3 |
| Control measures of anthrax in humans (Ç?, Ỹ) |
n= 161 | n= 41 | n= 66 | - | ||
| Avoiding contact with anthrax infected animals | 147 | 91 | 32 | 78 | 59 | 89 |
| Avoiding eating anthrax infected animal products |
114 | 71 | 24 | 59 | 48 | 73 |
| Burn anthrax suspected carcasses | 86 | 53 | 28 | 68 | 44 | 67 |
| Bury all anthrax suspected carcasses | 132 | 82 | 28 | 68 | 44 | 67 |
| Avoiding skinning anthrax dead cadaver |
160 | 99 | 31 | 76 | 45 | 68 |
| Animal vaccination | 115 | 71 | 40 | 98 | 38 | 58 |
(Ç?) This symbol denotes multiple answers allowed and (Ỹ) this symbol refers to – the question was asked only if participants indicated that ‘yes,’ for knowledge questions.
Table 6: Knowledge of anthrax among participants that reported having heard about the anthrax, in the Sodo Zuriya District, Southern Ethiopia, 2021.
Consumers: Only 36.3% of participants responded to one or more right answers about clinical symptoms of human anthrax; the rest majority (63.7%) did not know the clinical signs of anthrax in humans. The well-known symptom of human anthrax among consumers was skin rash or wounds (34.3%). Fifty-seven percent of participants knew at least one transmission way of anthrax in humans, with Slaughtering/skinning dead animals 100% (58/58) was the most reported transmission route. About 65% of participants indicated at least one prevention measure, and they declared that avoiding contact with anthrax infected animals (58%) found to be the most effective means of control in human beings.
Professionals: When asked about human anthrax, most veterinarians and medical experts knew one or more clinical symptoms, transmission ways, and prevention measures were 88%, 95%, and 98%, respectively. Skin rash/wounds (69%),consumption of dead animal meat/carcass (81%), and animal vaccination (95%) were the most frequently responded answers.
Generally, Professionals have a better understanding of modes of transmission, clinical symptoms, and prevention measures of human anthrax than livestock owners and consumers. Professionals’ respondents were found to be (OR: 15.172; 95% CI: 3.477-66.200; p<0.001) fifteen times than consumers regarding knowledge on transmission modes of anthrax in humans. Similarly, professionals twenty-two times (OR: 22.4; 95% CI: 2. 95- 169.4; p=0.003) more knowledgeable than consumers regarding anthrax prevention measures awareness. Likewise, the greater level of understanding found among professional’s (OR: 13.00; 95% CI: 4.700-35.957; p<0.001) and livestock owners (OR: 1.616; 95% CI: 1.004-2.603; p<0.001) regarding knowledge related to clinical symptoms of anthrax in humans when compared to consumers.
Participants attitudes towards human and animal anthrax
Livestock owners’ attitude: Of 240 animal owners in the study area, only 70 (29.2%) thought that anthrax could not be transmitted among humans, and only 60 (25%) had indicated they were sure that it could not be transmitted among animals. When asked about the seriousness of animal and human anthrax in and around their locality, about 101 (42%) respondents declared that animal anthrax is a problem in their community, but only 55 (23%) reported human anthrax as a problem. Forty-seven percent (113) respondents were sure that animals’ vaccination could help prevent anthrax infection in humans; the rest 53% (127) interviewers had a poor attitude about it. More than threequarters of participants (78.3%) replied that vaccinate animals to protect them from anthrax infection. Interestingly about 47.1% (113) participants responded to protect humans too. Whereas some participants declared that they vaccinate animals because of others, do so 11.3% (27) and 23 (9.6%) owners reported that they forced by government officials (Table 7).
| Variable | Response | Frequency | Percent |
|---|---|---|---|
| Does anthrax transmit among humans? (n=240) | Yes | 99 | 41.3 |
| No | 70 | 29.2 | |
| Do not know | 71 | 29.6 | |
| Does anthrax transmit among animals? (n=240) | Yes | 155 | 64.6 |
| No | 60 | 25 | |
| Do not know | 25 | 10.4 | |
| Do you think that animal anthrax is a problem in your locality? (n=240) | Yes | 101 | 42.1 |
| No | 83 | 34.6 | |
| Do not know | 56 | 23.3 | |
| Do you think that human anthrax is a problem in your locality?? (n=240) | Yes | 55 | 22.9 |
| No | 117 | 48.8 | |
| Do not know | 68 | 28.3 | |
| Do you think that vaccination of animals can help to prevent anthrax in humans? | Yes | 113 | 47 |
| (n=240) | No | 57 | 23.8 |
| Do not know | 70 | 29.2 | |
| What provokes you to take your animals for vaccination? (n=240) (Ç?, Ỹ) | To protect animals | 188 | 78.3 |
| Because others do so | 27 | 11.3 | |
| To protect humans | 113 | 47.1 | |
| 23 | 9.6 | ||
| How frequently animal vaccination against anthrax done in your locality? (n=240) | Twice a year | 64 | 26.7 |
| Once a year | 142 | 59.2 | |
| Never Vaccinated | 34 | 14.2 | |
| Others (More than 2 times, no fixed time) | 2 | 0.8 |
Table 7: Attitude towards human and animal anthrax among livestock owners in the Sodo Zuriya District, Southern Ethiopia, 2021.
Consumer’s attitude and practices: Most consumers 84 (82.4%) had a culture of consuming raw or undercooked meat, which is not a good practice. Most respondents reported that they only got meat for consumption during holy days/special occasions (39.2%) and some others eat meat once per month (38.2%). Meat sources were indicated by respondents as follows: 66.7% (68/102) from authorized butcher shops, 31/102(30.4%) from unauthorized butcher shops, 11% (11/102) from street sellers, 4% (4/102) from farmers, and 17% (17102) from other sources (such as; home slaughter, slaughter in a group with community members). Although the majority of consumers, 91.2% (93/102), thought that the meat had been inspected by veterinarians before being distributed to the public, 76% (77/101) of respondents indicated that they had a practice of home slaughter with their community members and shared the meat that has not been inspected by veterinarians. About 59% (60/102) participants believed that eating uninspected beef/mutton with hot pepper sauce locally called “Daxa” could prevent them from getting sick (Table 8).
| Question | Response | Frequency | Percent |
|---|---|---|---|
| Do you consume raw (undercooked) meat? (n=101) | Yes | 84 | 83 |
| No | 17 | 17 | |
| Frequency of meat consumption (n=101) | Daily | 3 | 3 |
| Weekly | 19 | 18.8 | |
| Monthly | 39 | 38.6 | |
| Only in holydays | 40 | 39.6 | |
| Others (3 x /week, 2 x /month) | 2 | 2 | |
| Source of meat (Ç?, Ỹ) (n=101) | Authorized Butchers shop | 68 | 66.7 |
| Street sellers | 11 | 10.8 | |
| Farmers | 4 | 3.9 | |
| unauthorized butcher | 31 | 30.4 | |
| 17 | 16.7 | ||
| Do you think that meat has been inspected by vets before being distributed to the public? (n=102) | Yes | 93 | 91.2 |
| No | 9 | 8.8 | |
| Do you practice home slaughter (meat that has not inspected by the vet)? (n=101) | Yes | 77 | 76 |
| No | 24 | 24 | |
| Do you think that eating uninspected meat with hot pepper sauce” daxa" can prevent you from getting sick?(n=102) | Yes | 60 | 59 |
| 42 | 41 |
(Ç?) This symbol denotes multiple answers allowed and (Ỹ) this symbol refers to – the question was asked only if participants indicated that ‘yes,’ for attitude and practice questions.
Table 8: Attitude and practices towards human and animal anthrax among consumers in the Sodo Zuriya District, Southern Ethiopia/2021.
Professional’s attitude: Sixty-seven percent of respondents stated that animal anthrax is a severe problem in their locality, and 38.1% of veterinarians and medical workers declared that human anthrax is also an issue in their community. Thirty-eight percent of respondents indicated that there was an anthrax outbreak in their locality. The majority of interviewers recalled the outbreak encountered before this year (73.8%), while 9.5% of participants stated that anthrax outbreak occurred within this year at the time of the interview. But about 16.7% of experts did not remember the exact period when it was encountered. When asked about how vaccination protects an animal from anthrax, the majority (71.4%) of respondents believed that vaccination could enhance an animal’s immunity (Table 9).
| Question | Response | Frequency | Percent |
|---|---|---|---|
| Do you think that animal anthrax is a problem in your locality? (n=42) | Yes | 28 | 66.7 |
| No | 13 | 31 | |
| Do not know | 1 | 2.4 | |
| Do you think that human anthrax is a problem in your locality? (n=42) | Yes | 16 | 38.1 |
| No | 24 | 57.1 | |
| Have you had an anthrax outbreak in your locality? (n=42) | Yes | 16 | 38.1 |
| No | 23 | 54.8 | |
| Do not know | 3 | 7.1 | |
| When did the anthrax outbreak occur in your locality? (n=42) | Within this year | 4 | 9.5 |
| Before this year | 31 | 73.8 | |
| Do not remember | 7 | 16.7 | |
| How vaccination protects an animal? (n=42) | It makes an animal strong | 4 | 9.5 |
| It makes an animal healthy | 14 | 33.3 | |
| It enhances an animal immunity | 30 | 71.4 | |
| Do you think that medical workers in their workplace could contract anthrax? (n=42) | Yes | 24 | 57.1 |
| No | 17 | 40.5 | |
| No response | 1 | 2.4 | |
| Have you had any experience of touching the blood of a severely sick animal without an adequate PPE? (n=22) | Yes | 14 | 63.6 |
| No | 8 | 36.4 | |
| Have you had any experience of touching a patient's wound/skin rushes without adequate PPE? (n=20) | Yes | 6 | 30 |
| No | 14 | 70 | |
| Do you think that Bacillus anthracis spores in soil pose a direct risk of infection for human beings? | Yes | 27 | 64.3 |
| No | 15 | 35.7 | |
| Do you think that Bacillus anthracis spores in soil do pose a direct risk of infection for livestock? | Yes | 38 | 90.5 |
| 4 | 9.5 |
(Ç?) This symbol denotes multiple answers allowed and (Ỹ) this symbol refers to–the question was asked only if participants indicated that ‘yes,’ for attitude questions.
Table 9: Attitude and practices towards anthrax among vets and medical professionals in the Sodo Zuriya District, Southern Ethiopia, 2021.
More than half (57.1%) health workers claimed that health care workers in their workplace might be exposed to anthrax, and about 30% of them had the experience of touching a patient’s wound/skin rushes without adequate PPE. Though, 78.6% of respondents thought that veterinarians in their work might contract anthrax, and 63.6% of animal health workers had an experience touching the blood of severely sick animals without an adequate PPE. The proportion of respondents that thought Bacillus anthracis spores in soil can pose a direct risk of infection for livestock was 90.5% (38/42). In comparison, 64.5% (27/42) had a negative attitude because they alleged that Bacillus anthracis spores in soil could pose a direct risk to humans. Table 9 conveys the summary information to shed some light on the professional’s perspective.
Practices towards human and animal anthrax among livestock owners
More than half of animal owners practice a mixed husbandry system (51.3%), encompassing free-range and zero-grazing types. Some other respondents rely only on one system; 30.8% of respondents practice zero grazings, while the remaining (17.9%) said free-range grazing was their favorite choice. Surprisingly,most (36.7%) respondents who participated in this interview experienced throwing the carcass into the jungle or paddle when an animal died suddenly. The rest, 33.8% had a practice of burying the carcass, 14.6% had an experience of informing veterinarians, 10.6% call in butcher and 4.6% respondents had a tradition of slaughtering an animal that has died of unnatural causes and sharing the meat among the community members (Table 10).
| Question | Response | Frequency | Percentage |
|---|---|---|---|
| Which type of animal husbandry do you practice? (n=240) |
Zero grazing | 74 | 30.8 |
| Mixed - free-range and zero-grazing | 123 | 51.3 | |
| Free-range | 43 | 17.9 | |
| When your animal dies suddenly, what would you do? (n=240) | Slaughter and share the meat with the community | 11 | 4.6 |
| Call in the butcher | 25 | 10.4 | |
| Call in the veterinarian | 35 | 14.6 | |
| Bury the carcass | 81 | 33.8 | |
| Threw the carcass into the puddle or jungle | 88 | 36.7 | |
| Would you use lime while burying the anthrax suspect carcass? (n=81) | Yes | 44 | 54.3 |
| No | 37 | 45.7 | |
| Do you use PPE while touching anthrax suspect carcass? (n=240) | Yes | 80 | 33.3 |
| No | 160 | 66.7 | |
| Were your animals vaccinated against anthrax? (n=240) | Yes | 171 | 71.3 |
| No | 59 | 24.6 | |
| Do not know | 10 | 4.2 | |
| If yes, which animal species were vaccinated? (n= 171) (Ç?, Ỹ) | Cattle | 166 | 97.1 |
| Goats | 30 | 17.5 | |
| Donkey | 41 | 24 | |
| Sheep | 72 | 42.1 | |
| Horse | 22 | 12.9 | |
| Mule | 20 | 11.7 | |
| If no, why your animals not vaccinated? (n=59) (Ç?, Ỹ) | To save money by vaccinating only some animals |
9 | 15.3 |
| Not necessarily to vaccinate | 8 | 13.6 | |
| Shortage of vaccine | 11 | 18.6 | |
| It may damage such particular animal species |
9 | 15.3 | |
| No awareness | 14 | 23.7 | |
| 8 | 13.6 |
(Ç?) This symbol denotes multiple answers allowed and (Ỹ) this symbol refers to–the question was asked only if participants indicated that ‘yes,’ for practice questions.
Table 10: Practices towards human and animal anthrax among livestock owners in the Sodo Zuriya District, Southern Ethiopia, 2021.
Out of 81 participants who had burying carcasses, about 44(54%) animal holders use lime while burying the carcass. On the other hand, only about 33% (80/240) of animal keepers use personal protective equipment such as gloves and face masks made from local material while handling the carcass. Regarding animal vaccination majority (71%) of livestock owners had the practice to vaccinate their animals against anthrax. Cattle (97.1%) were the most vaccinated animal species, followed by sheep (42.1%) and donkeys (17.1%). The absence of awareness about the importance of vaccination (23.7%), shortage of vaccine (18.6%), and saving money (15.5%) were the most prominent reasons forwarded by animal owners who did not vaccinate their animals against anthrax. Results are illustrated in Table 10.
Discussion
The current study applied a broad concept in terms of human and animal anthrax's knowledge, attitude, and practices by livestock owners, consumers and, veterinary and medical professionals in Sodo Zuriya District of Wolaita Zone, Southern Ethiopia. It opens the door for future findings, research, surveillance, prevention, and control efforts of human and animal anthrax in the study area and throughout the country.
In the current study, the social-demographic characteristics of participants revealed that 69.2% were males and 30.8% females. Although an Ethiopian Demographic data shows that the proportion of males and females are almost similar, there were a significantly higher number of males than female respondents in this study [15]. It can be attributed to the fact that females are less likely to be listed as household heads and that males dominate animal rearing. Most respondents fall in age between 36-60 years of age (62.5%); this result was in line with the actual country’s demographics data, which infers about (56%) of the total population categorized under the working-age group [16]. Regarding employment/occupation, most respondents were farmers (62.5%); this is similar to the fact that agriculture is the livelihood of most Ethiopians. The labor force engaged in the agriculture sector was about 73% of the total population [17]. The majority of respondents had some primary/elementary (24.2%) and secondary level of education (23.8%); in contrast, the education survey shows above half (53.3%) of the total population had little or no education [18]. It might be due to most participants involved in this survey were from urban and peri-urban areas where access to education was comparatively better than rural areas. A vast majority (62.5%) of farmers in this study area keeps livestock; this is consistent with more than 70% of the total population raise animals in the country [19].
The most common source of information about anthrax was through personal contacts within community members (families, friends, and neighbors, 37.6). Similarly, according to the health and demographic survey of the country, the majority of respondents have no access to media (TV, Radio, newspapers) at least once a week (74% of women and 62% of men) [18]. It indicates the level of exposure to mass media found to be low in Ethiopia.
Knowledge
The study findings show that current knowledge of human and animal anthrax varies among different categories (livestock owners, consumers, and professionals) and socio-demographic factors. In this study, the overall knowledge level of community members found to be 64% (livestock owners 65%, consumers 63%) regarding awareness of the disease in general, its cause, zoonotic nature, preventability, and knowledge on at least one (clinical symptoms, mode of transmission and possible prevention methods) of the disease both in humans and animals. This result was consistent with the findings from the Tigray region of Northern Ethiopia 62% but higher than that of the study conducted in Jimma, Southwestern Ethiopia 55.4% and KAP assessment result about milk quality and common zoonotic diseases in smallholder dairy production chain in selected sites of southern Ethiopia [20-22]. In contrary, this result was lower than study conducted in Zambia 88% Zimbabwe 71.5%, Kenya 77.9% [23-25].
The proportion of professionals who knew the cause, zoonotic nature, preventability, and knowledge of at least one (clinical symptoms, mode of transmission, and possible prevention methods) of the anthrax was 91%. Hence, compared to other similar studies conducted on the Northern Ethiopia/Tigray Region 55.7%, the result found to be much higher [26]. This variance might be due to in the current study area; both human and animal health professionals had more experience of handling anthrax cases and had better access to information of the disease.
Generally, this study revealed that livestock owners better understand modes of transmission, clinical symptoms, and prevention measures of human and animal anthrax than consumers but less knowledgeable than medical and veterinary professionals. It could be due to experts have better education and case handling experience. In comparison, consumers who never participated in animal husbandry practices had low exposure to animal diseases like anthrax to acquire lesser knowledge about the disease. A similar study conducted in Ghana to assess KABP of anthrax different community members revealed that the proportion of consumer's (81.6%) knowledge was found to be lesser when compared to other community members (96%). According to study done in northern Ethiopia showed professional's knowledge of animal and human anthrax better than other community members [20].
Attitude
Most animal owners who participated in this study thought that anthrax could be transmitted among humans and animals. Anthrax is not a contagious disease. It can’t be transmitted from an infected person to a healthy person through the aerosol and ingestion route. Still, in some rare cases, the person-to-person transmission may occur with cutaneous anthrax, where discharges from skin lesions might be infectious [27]. Likewise, according to OIE, it does typically not spread from animal to animal, too [5]. Most livestock owners did not have sufficient information about the seriousness of anthrax around their surroundings; only 22.9%, 42% of respondents knew about human and animal anthrax seriousness, respectively. Though, the Zonal livestock and fishery resource-development department record indicated a recent anthrax outbreak in the study area since 2020 G.C (2012 E.C). However, medical and veterinary professionals have a good attitude towards the severity of the disease around their locality. This implies experts have not created sufficient attitude-altering tusks at a community level; there is a gap in knowledge transfer from professionals to community members. On the contrary, one recent study conducted in the Amhara region of Ethiopia indicated more than 67% of study participants testified that anthrax was a health problem of their community. On the other hand, similar survey done in Tigray Region disclosed about 9.8% community members taught that animal anthrax was a severe problem of their locality and 11.3% believed human anthrax was a problem in the study area [11,20].
In the current study, about 53% of respondents did not have appropriate information about animal vaccination in preventing anthrax in humans. Out of fifty-three percent, 23.8% of participants taught that animal vaccination is not related to anthrax prevention in humans, while 29.2% did not know whether it is helpful or not. A similar study in Northern Ethiopia (Tigray region) indicated only 32.4% of participants believed that vaccinating animals could help anthrax prevention efforts in humans [20]. The current study disclosed that 59% of study participants believed that eating uninspected beef/mutton with hot pepper sauce locally called “Daxa” could prevent them from getting sick.
It could indicate excessive community dependence on herbs and spices, which they believed could prevent some form of infectious disease. Some other study done in Ghana explained the presence of similar community belief, which reported that cooking meat or carcasses of an animal that has died of un-natural conditions with herbs could prevent diseases like anthrax [26].
The proportion of respondents that thought Bacillus anthracis spores in soil can pose a direct risk of infection for livestock was 90.5% (38/42). In comparison, 64.5% (27/42) had a negative attitude because they alleged that it could pose a direct risk to humans. It could be due to some professionals have difficulty remembering what they have learned at school in the past and a low level of commitment/engagement to update themselves through reading and gathering information related to the disease. In general, despite livestock owners and consumers had negative attitudes towards most anthrax prevention related tusks, but professionals had a good attitude.
Practices
We found most animal owners in the study area practice a mixed (free-range and zero-grazing unit) system. It could be due to the study area situated at the highland part of Zonal administration, where the grazing land coverage is lower compared with midland and lowland altitude areas. Moreover, about eighteen percent of participants were only involved in free-range grazing practice, which most likely exposes an animal to Bacillus anthracis spores while grazing.
The findings of this study indicated that about 71% of animal owners in Sodo Zuriya District had a practice of vaccinating their animals against anthrax. However, the Zonal vaccination record showed that most livestock owners in the district did not vaccinate their animals. According to LFRDD, anthrax vaccine coverage of the district was only fifty-nine percent. In Ethiopia, animal anthrax vaccine is available, and NVI entirely carries out its production. Vaccine delivery to communities and zonal administrations made through livestock bureaus and agencies of concerned regional states. Despite the fact that vaccines are provided at a minimal cost in the district, the vaccination achievement was not satisfactory. This could be due to low commitment of institutional leaders to avail all desired amount of vaccine for vet clinics and weak performance of experts to administer all planed dosage of vaccine to target animals.
Regarding proper disposal of the carcass, in this study, most participants had risky practice. Only 33.8% of community members had a habit of burying the carcass, and about 14.6% had an experience of calling veterinarian following the death of an animal. The rest was involved in harmful practices such as; threw the carcass into the jungle or paddle, reaching to the wrong person (butchers), and practice of slaughtering an animal that has died of an unknown cause. Surprisingly, most (36.7%) respondents who participated in this interview experienced throwing the carcass into the jungle or paddle when their animal died suddenly. In contrast, a recent study in southern Kenya revealed, following sudden death of an animal 61.1% of study participants reported that they would skin animals before burial, while 28.8% would either burn or bury the cadaver, only 4.6% (15/329) would contact vet service provider and 5.5% (18/329) would share the meat among community members [28]. The difference could be due to the presence or absence of a robust health education system related to zoonotic disease, culture, and life experience of participants among the two study areas.
Fifty-four percent of participants had a practice of using lime while burying the carcass. Previously, there was a recommendation to use lime for anthrax disinfection when burying an animal dead of anthrax. However, recent scientific work revealed that exposure of anthrax spores to calcium (calcium oxide) might help in their survival and viability, so it is not recommended to use lime for agricultural anthrax disinfection [29]. Therefore, the use of lime while burying the carcass should be considered one of poor community practice conducted by majority of respondents.
Only about 33% of animal owners use personal protective equipment (such as glove and face musk) made from local material while handling the carcass of suddenly dead animals. It might be due to some practice or habits require some amount of ransom to be spent on PPE, such as goggles, gloves, and boots. However, having adequate knowledge and attitudes, individuals cannot convert these into practice due to financial constraints. The finding of this survey also indicated that PPE usage among professionals was also found to be very low. However, the proportion of medical workers using PPE was found to be better than animal health workers. This could be because there will be insufficient PPE supply by government bodies in veterinary care institutions, lack of willingness of professionals to use PPE, and absence of strict directive, which enforce PPE usage in the veterinary clinic or animal health post.
Amazingly, 82.4% of respondents had a habit of raw or undercooked meat consumption practice. It could be due to improper social and cultural tattoos that encourage consumption of raw meat in the form of “Kurt or Kitfo” is better than cooked one and the deeply established traditional habit of eating raw or undercooked meat throughout the country. This finding aligns with a previous study in Nazareth Town, Ethiopia, which revealed Over 86% of the study participants had a habit of raw or undercooked mutton consumption [30]. Generally, consuming undercooked or raw animal products is a well-established risk factor for acquiring many zoonotic diseases, including anthrax in an area. Even though in Ethiopia, meat consumption amount is not adequate compared to the rest of world countries. However, large and small ruminants were sometimes butchered for the sole purpose of selling within the community.
Moreover, on special occasions, in most parts of the country, people have a cultural ceremony of slaughtering an animal and sharing the meat among the group, called “Kircha,” which Ethiopians consider as their social capital [31]. Some other previous studies explained that an unknown amount of live animals sold for home slaughter and consumption purposes in the Ethiopian market [33]. Despite most consumers, 91.2% thought that meat had been inspected by veterinarians before being distributed to the public, but 76% of consumers indicated that they had a practice of home slaughter with their community members and shared the meat that has not been inspected by veterinarians. This could be due to an inadequate level of community awareness on the importance of inspected meat over an uninspected one, and attitude of undermining the consequence of zoonotic risks. The study conducted in Konso, Southern Ethiopia also showed most of the food animals in the study area were slaughtered without any veterinary supervision or inspection. In general, most community practices were risky, that could impose public health hazards directly or indirectly, and the community practices found to be poor among the participants [33].
Conclusions
In Ethiopia, emerging zoonotic diseases, such as anthrax that have acquired global significance seriously affect the livestock sector in the country. Therefore, this study aimed to assess the current level of knowledge, attitude, and practices towards anthrax prevention among the community members and professionals in the Sodo Zuriya district of Wolaita Zone, Southern Ethiopia. Based on the quantitative cross-sectional survey and secondary data record from zonal livestock and fishery department record of the study area, the following opinions narrated.
• The study revealed that participant's knowledge regarding the cause, zoonotic importance, clinical symptoms, mode of transmission, prevention, and control methods of anthrax were above average. Socio-demographic factors such as gender, age, education, and type of occupation had a statistically significant association with awareness of the disease and its preventability among livestock owners. Likewise, age and education were statistically significant predictors of knowing anthrax, its zoonotic importance, and preventability among consumers. Generally, for all knowledge assessing questions, livestock owners had better awareness than the consumers but a lower understanding than professionals. Knowledge difference among the three categories, such as livestock owners, consumers, and professionals, showed a statistically significant association. However, this knowledge is not usually practical. Most people continue to consume uninspected raw or undercooked meat, fail to vaccinate their animals, unable to use PPE, and embraces enormous risky cultural practices. The knowledge among the community members has been enhanced over time by awareness created by veterinarians and health extension workers due to frequent anthrax outbreaks.
• There was a negative attitude towards anthrax among animal owners and consumers. However, human and animal health workers who participated in this survey had a positive attitude towards the disease. In this study, most community members had negative attitudes regarding the seriousness of the condition, use of anthrax vaccine in animals, and meat inspection related aspects.
• Some practices performed by the community and professionals were significant risk factors of anthrax existence in an area. Exercises such as free gazing system, consumption of raw or undercooked meat, the experience of touching suspect without appropriate personal protection equipment, improper disposal of the carcass (use of lime while burying), the cultural habit of home or community slaughter, and failure to vaccinate all livestock.
Generally, this study demonstrates better knowledge but a low level of the desired attitude and existence of high-level risky practices among community members related to human and animal anthrax in the study area. Hence, the findings from this study can be used as a baseline for the national anthrax awareness campaigns and modify the approach towards prevention and control strategy of disease, giving more emphasis on knowledge, attitude, and practice change. Moreover, other research and innovations regarding the overall aspect of the disease in human behavior are needed and extended to other countries regions. Finally, based on the above conclusions, the following recommendations forwarded:
Recommendations
• The government should develop an easily applicable anthrax policy to address prevention and control measures such as vaccination, regular surveillance, proper carcass disposal, and appropriate PPE usage among both human and animal health caretakers and community members. And there should be regular updates and reviews of this policy.
• Rigorous training and targeted community health education for livestock owners and animal product consumers are needed to enhance their understanding of overall aspects of the anthrax. Moreover, collaborative actions needed to create community awareness about meat and milk safety; especially this should be operated under a “One Health approach” umbrella.
• The government should facilitate mass media communications in local and national languages with simple messages, including details describing human and animal anthrax (such as; pathognomonic clinical symptoms, mode of transmission and prevention measures, risky community practices) channeled through government and community networks regularly.
• Institutional and human resource (veterinary and medical professionals) capacity-building efforts should be strengthened to diagnose zoonotic diseases like anthrax for early outbreak detection and subsequent interventions.
• The collaboration among the human and veterinary health sectors and others, such as environmental protection agencies, policymakers, and NGOs, should be encouraged to strengthen the community's overall health knowledge, attitudes, practices, and beliefs toward anthrax.
• The community members should strictly follow seasonal animal anthrax vaccination calendar to vaccinate their animals against anthrax, which could help to prevent their livestock and themselves from getting anthrax infection.
• The community members should cease consumption of raw meat that has not been inspected by veterinarians, use appropriate personal protective equipment’s while handling anthrax suspect carcass, quit the practice of throwing anthrax dead cadaver in to the jungle or puddle and must stop application of lime while burying anthrax dead carcass.
• Both medical and veterinary Professionals should use appropriate personal protective equipment while handling anthrax suspect patient and should have to update their knowledge always with new scientific findings and innovations related to the disease anthrax.
Limitations
The primary limitation to the generalization of this study is made by using mainly quantitative data, which is collected from an individual informant and some secondary information obtained from different governmental organizations. Qualitative data such as focused group discussions were not included in this paperwork, which may enhance the reliability of the findings. However, by considering such a fact, we used comprehensive and multiple questioners with both open and close-ended queries and detailed discussion of results in the context of relevant literature. These measures helped to minimize the effect of limitation in our study. Second, this study was not intended to estimate the prevalence of anthrax in the study area to confirm the disease's magnitude. Therefore, further research to ascertain the extent of the problem in humans and animals should be undertaken.
Acknowledgments
First of all, I would like to thank the most gracious and almighty God, without his support, this work will not come into reality.
Next, I would like to express my deepest gratitude to my supervisor, Professor Wan Cheng Song, whose guidance, support, and encouragement I will never forget. I have benefited significantly from his wealth of knowledge and meticulous editing.
I acknowledge the generous opportunities created by the Ministry of Commerce (MOFCOM) of the People’s Republic of China to study at the university of wisdom (SMU).
I am highly indebted to the community members and professionals who generously took the time to participate in my research and provided valuable information during the questionary survey. I owe deepest gratitude to my numerous friends who endured this long process with me. My special thanks to Mr. Enkeshe Loha, who particularly coordinated all data collection processes.
My sincere gratitude goes to the livestock and fisheries department of Wolaita Zone and other regional, zonal, district level institutions, directly and indirectly, involved in this research work for their significant contribution.
Finally, my warm and heartfelt thanks go to my beloved wife (Selamawit Milkias) as well as other family members for their tremendous support, hope, and love they had given to me.
Competing interests
The authors declaring that they have no competing interests.
Authors contributions
Amare AA (Author): designed the study and wrote the draft of the manuscript, Liang S (Co-author): edited the article and involved in the data analysis and Wan CS critically revised the article for important intellectual content.
References
- Pieracci EG, Hall AJ, Gharpure R, Haile A, Walelign E, et al (2016) Prioritizing zoonotic diseases in Ethiopia using a one health approach. One Health 2(1): 131-135.
- Leta S, Mesele F (2014) Spatial analysis of cattle and shoat population in Ethiopia: growth trend, distribution and market access. SpringerPlus 3(1): 310.
- World Health Organisation. Zoonoses. 2020
- World Health Organization. Anthrax in humans and animals. 4th edition. 2008
- World Organisation for Animal Health. Anthrax. 2018
- Doganay M, Demiraslan H (2015) Human anthrax as a re- emerging disease. Recent Pat Antiinfect Drug Discov 10(1):10- 29.
- Seid K, Derso T, Shiferaw AM (2019) Knowledge of anthrax infection prevention and its associated factors among livestock owners in Sekotazuria district, Wag-himra zone, northeast, Amhara region Ethiopia: Cross Sectional Study.1(1):1-16.
- Vieira AR, Salzer JS, Traxler RM, Hendricks KA, Kadzik ME, et al (2017) Enhancing Surveillance and Diagnostics in Anthrax- Endemic Countries. Emerg Infect Dis 23(13):S147-S153.
- Shiferaw G (2004) Anthrax in Wabessa village in the Dessie Zuria district of Ethiopia. Rev Sci Tech 23(3): 951-956.
- Mwakapeje ER, Hogset S, Softic A, Mghamba J, Nonga HE, et al (2018) Risk factors for human cutaneous anthrax outbreaks in the hotspot districts of northern Tanzania: an unmatched case-control study. R Soc Open Sci 5(9):1-13.
- Seid K, Shiferaw AM, Yesuf NN, Derso T, Sisay M. (2020) Livestock owners' anthrax prevention practices and its associated factors in Sekota Zuria district, Northeast Ethiopia. BMC Vet Res 16(1): 39.
- Carlson CJ, Kracalik IT, Ross N, Alexander KA, Jones MEH, et al (2019) The global distribution of Bacillus anthracis and associated anthrax risk to humans, livestock and wildlife. Nat Microbiol 4(8): 1337-1343.
- CSA Ethiopia (2007) Population and Housing Census 2007-SNNPR Statistical.
- Daniel WW, Cross CL (2018) Biostatistics: a foundation for analysis in the health sciences.
- IndexMundi. Ethiopia Sex ratio. 2020
- Bekele A, Lakew Y (2014) Projecting Ethiopian demographics from 2012-2050 using the spectrum suite of models. Policy 1(1): 1-6.
- FAO- Ethiopia: National gender profile of agriculture and rural livelihoods. (2019) Sustainable Development Goals Fund. 84.
- Demographic and Health Survey (2016) Central Statistical Agency, Addis Ababa, Ethiopia.
- Relief Web (2019) The future of livestock in Ethiopia: Opportunities and challenges in the face of uncertainty.
- Romha G, W Girmay (2020) Knowledge, Attitude and Practice towards Anthrax in Northern Ethiopia: a mixed approach study. BMC Infect Dis 20(1):814.
- Semu DT, Fekede D, Tigre W, Regassa A (2013) Perception of the public on the common zoonotic diseases in Jimma, Southwestern Ethiopia. Int J Med Med Sci 5(6): 279-285.
- Gebremedhin SG, Mequnnent SE, Gichamo AA (2020) Assessment of knowledge, attitudes and practices of people about milk quality and common zoonotic diseases in small holder dairy production chain in selected sites of southern Ethiopia. Int J Adv Res Biol Sci 7(8): 25-36.
- Sitali DC, Mumba C, Skjerve E, Mweemba O, Kabonesa C, et al (2017) Awareness and attitudes towards anthrax and meat consumption practices among affected communities in Zambia: A mixed methods approach. PLOS Negl Trop Dis 11(5): e0005580.
- Chikerema SM, Matope G, Pfukenyi DM (2013) Awareness and attitude toward zoonoses with particular reference to anthrax among cattle owners in selected rural communities of Zimbabwe. Vector Borne Zoonotic Dis 13(4): 243-249.
- Chacha IN (2017) Knowledge, Attitudes And Practices Regarding Anthrax Among Community Members, Health And Veterinary Workers In Maragua, Kenya. University of Nairobi.
- Opare C (1999) Knowledge, Attitudes, Beliefs and Practices of Inhabitants of the Tamale Municipality on Antrhax: Implications for the Prevention of Human Anthrax. University of Ghana.
- Center of Disease Control and Prevention. How People Get Anthrax. 2020
- Mbai JM, Omolo JO, Wamamba D, Maritim D, Gura Z, et al (2021) Assessment of knowledge, attitudes and practices towards anthrax in Narok County, Southern Kenya. Pan Afr Med J 38(1): 120.
- Himsworth CG (2008) The danger of lime use in agricultural anthrax disinfection procedures: the potential role of calcium in the preservation of anthrax spores. Can Vet J 49(12): 1208- 1210.
- Negash T, Tilahun G, Medhin G (2007) Seroprevalence of Toxoplasma gondii in Nazareth Town, Ethiopia. Cent Afr J Med 53(9-12): 47-51.
- Seleshe S, Jo C, Lee M (2014) Meat Consumption Culture in Ethiopia. Korean J Food Sci Anim Resour 34(1): 7-13.
- Avery A (2004) Red meat and poultry production and consumption in Ethiopia and distribution in Addis Ababa. ILRI.
- Kussia GG, Ayano AA (2018) A habit of raw farm animal blood consumption and public awareness about associated health risks in Konso district. MOJ Anat & Physiol. 5(6): 350-355.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences