Criteria Useful in Measurement of Pain and Monitoring Treatment Outcomes
Farzana Mitra1*, Shahead Chowdhury1, Mike Shelley2 and Petra Buettner3
1The Townsville Pain Management Clinic, The Townsville Hospital, Townsville, QLD 4814, Australia
2Bundaberg Hospital, Bundaberg, QLD, Australia
3Discipline of Public Health and Tropical Medicine, James Cook University, Townsville, QLD 4811, Australia
- Corresponding Author:
- Farzana Mitra
The Townsville Pain Management Clinic
The Townsville Hospital, Townsville, QLD 4814, Australia
Tel: +61-7-4796 2231
E-mail: farzana_mitra@health.qld.gov.au
Received date: March 13, 2018; Accepted date: April 09, 2018; Published date: April 16, 2018
Citation: Mitra F, Chowdhury S, Shelley M, Buettner P (2018) Criteria Useful in Measurement of Pain and Monitoring Treatment Outcomes. J Anaesthesiol Crit Care Vol.1 No.2:6
Abstract
Objective: Persistent pain has profound effects on the health and quality of life. A reliable, comprehensive yet simple, measurement tool is essential for research, optimising clinical practice and treatment outcomes for persistent pain patients. We seek to devise a tool to aid physicians in assessing persistent pain.
Design: A scoring tool was developed to measure the direct and indirect markers of persistent pain across the following domains: Score of pain(S), Physical activity (P), Additional medication (A), Additional GP/ED visit (A), Sleep quality (S), Mood (M) and Side-effects of pain medication (S). These characteristics were rated and scored monthly in persistent pain patients for 9 months. SPAASMS score was inversely proportional to improved pain management.
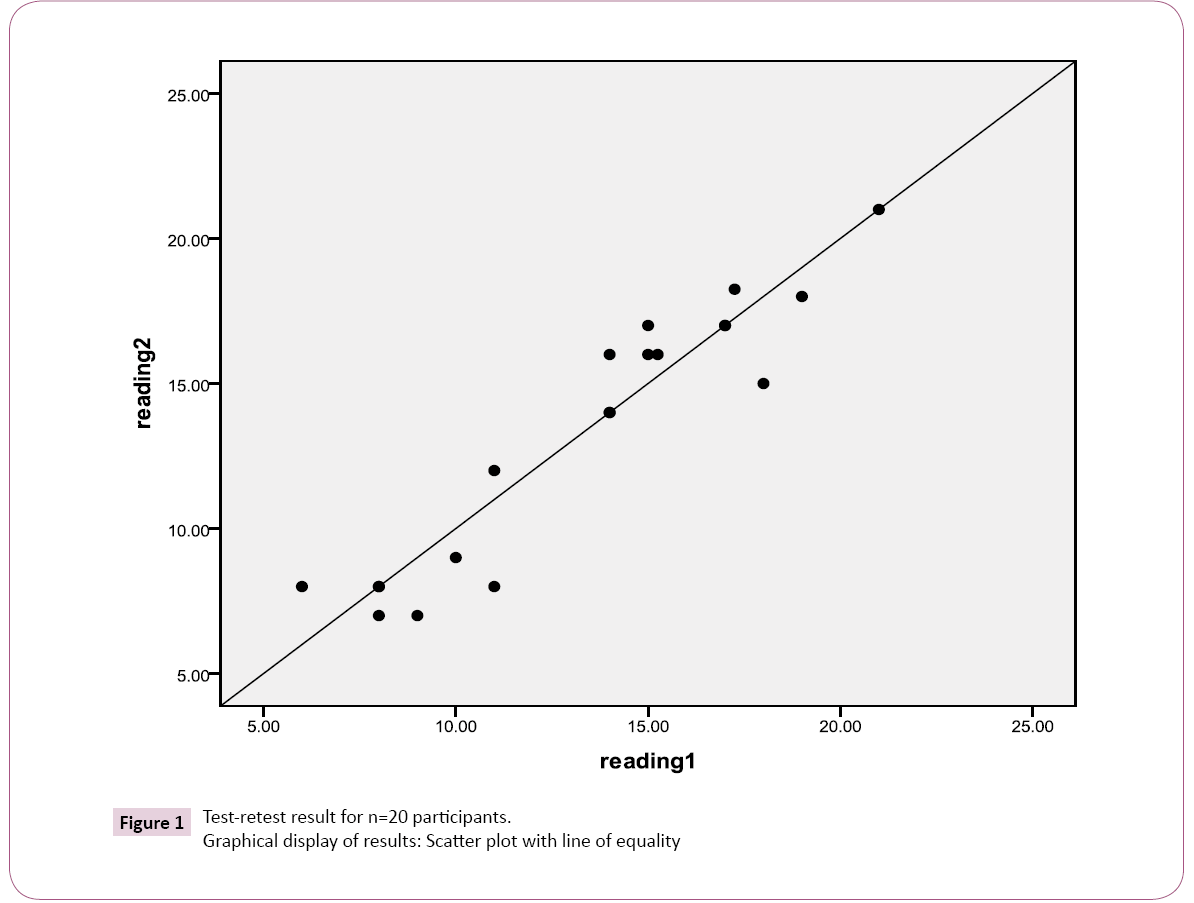
Results: The test-retest analysis for SPAASMS score (n=20) showed a concordance correlation coefficient of 0.94; 95%-confidence interval=0.86, 0.97 and Cronbach’s alpha for Reading 1 and 2 were 0.66 (p=0.001) and 0.67 (p<0.001), respectively. Comparison of the score with the Numerical Rating Scale (NRS), Physical Disability Index (PDI), Depression, Anxiety, Stress Scale (DASS21) and a combined score of NRS, PDI and DASS21 showed improved sensitivity except for DASS21. The score declined when patients responded well but remained high in patients not responding to treatment or increased with precipitating events like further trauma. With optimum relief, scores remained static.
Conclusion: SPAASMS is a simple, rapid and comprehensive tool which quantifiably indicated the progress of the patient under treatment. It can also be used to determine symptoms which have not responded to it.
Keywords
Persistent pain; Assessment tool; NRS; PDI; DASS21
Introduction
Persistent pain has been described as continuous or recurrent pain of sufficient duration and intensity to adversely affect a patient’s well-being, mood, level of functioning and quality of life. A reliable measurement tool is essential for research, optimising clinical practice and treatment outcomes for patients with persistent pain [1,2]. According to Gatchel [3], physical and psychogenic pain hurt equally.
Persistent pain has profound changes on a patient’s activity, mobility, sleep, social life, leisure activities, mental health and quality of life [4]. Single dimensional scales like the Numerical Rating Scale (NRS), the Visual Analogue Scale (VAS), the Verbal Rating Scale (VRS) or multi-dimensional scales like Wisconsin Brief Pain Inventory, McGill Pain questionnaire etc are used for measurement of pain. Other scales, e.g. Depression, Anxiety, Stress Scale (DASS21) and PDI (Pain Disability Index) may be used to measure some components of persistent pain, like psychological and physical factors, respectively. The Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) recommendations are very useful for measurement of clinical trial outcomes for medicines used for persistent pain [5]. The Norwegian Pain Society has also recommended a fourpage, 31 item screening questionnaires for treatment outcomes [6]. These scales and recommendations are comprehensive and precise. However, these tools may prove lengthy and tedious for patients experiencing intense pain. For persistent pain clinicians it is important to have a concise, time efficient tool and to evaluate progress of treatment. Successive reduction of SPAASMS (the new measurement tool) scores should indicate clinical improvement of the seven components of persistent pain.
Method
Pain is a multidimensional subjective experience [7]. The effects of persistent pain may include poor sleep, restricted mobility, decreased activity, poor mood, greater use of medications and more health practitioner visits. Therefore, SPAASMS score includes the majority of these components.
Score of pain
Turk and Melzack have stressed on intensity as the most salient feature of pain [8]. As intensity of pain is a subjective experience and there is no equipment at present to measure pain, we rely on the patient’s self-report for monitoring intensity. Common measures used in this context are VRS, VAS and NRS. The NRS can be presented graphically or delivered verbally. As the monthly assessments would be done by telephone and NRS was easily understood by patients, it was convenient for our purpose. It has been shown that NRS has greater power to detect pain intensity than VRS and it is superior to VAS in terms of comprehension by patients [2]. Also, from review by Williamson and Hoggart [9], it appears that VAS is the least sensitive, though easy to use. VAS has the highest failure rate. Repeated scores using VAS can vary by as much as 20%. Therefore, NRS was chosen above others. Reduced scores of pain intensity indicate successful treatment.
Physical activity
Physical activity levels are considered as an important factor in pain assessment which could indicate functional outcomes such as improved activities of daily living (ADL) like household chores, walking, working or travel [10-12]. In 1985, Linton [13] found that activity and pain levels were related, only when based on overall physical functioning. This relationship gradually disappears when the activity becomes more specific and objective as would happen, when measures like the Assessment of Motor and Process Skills (AMPS) or similar other measures are applied. A more recent study found that more than two-thirds (68%) of the persistent pain patients considered improvement in daily activities as necessary for a successful outcome [14]. Thus, any measure indicating successful treatment needs to show increased activity levels.
Mood
Mood defined as a state of mind or emotion. A World Health Organization (WHO) study showed that 22% of primary care patients are suffering from constant debilitating pain and are four folds more likely to have a depression or anxiety mood disorder than the patients without persistent pain [15]. Similarly, Patten et al. [16] in a large-scale study in Canada, showed that long-term pain increases the risk of major depression. Several studies found increased depression rates with a persistent pain condition [17]. Increased number of painful sites or more diffuse pain increases the risk of depressive illness [18]. Gambassi [19] discussed in a review that pain and depression share genetic factors, biological pathways and neurotransmitters. The IMMPACT study (2003) has recommended emotional functioning as one of six outcome domains to be considered in assessing persistent pain [5]. Therefore, we have included mood as one of the major components for clinical assessment in our SPAASMS scale.
Sleep
Studies have demonstrated the inverse relationship between sleep quality and pain [20,21]. Insomnia increases severity of pain [22]. A study has found that in comparison to healthy controls, subjects with fatigue and pain experience poor sleep. These patients also experience higher incidence of depression and functional disability [23]. In their study, McCracken and Iverson [24] found that patients with insomnia reported greater pain intensity. For improvement in persistent pain to be inferred, problems with sleep need to be measured and reduced. Whether it is a cause or consequence of the pain condition, sleep disorders must be treated in the same way as pain [25]. Further, several studies have used assessment of insomnia based on the patient’s self-description as poor sleepers and good sleepers or satisfactory and unsatisfactory sleep groups [26-28]. Therefore, quality of sleep has been used in SPAASMS as one of the multidimensional constructs. It was self-rated from very good to poor and scored accordingly.
Side effects
NSAIDS and opioids have been used widely for non-malignant pain for several years [29]. Opioids have a range of adverse, unpleasant side effects of which nausea; constipation, vomiting, drowsiness and cognitive impairment of varying degrees have been reported by patients [30]. Lately, the use of other synthetic and semi-synthetic opioids like transdermal Fentanyl and Buprenorphine for treatment of persistent pain has added to the list of unwanted side-effects of local irritation, rashes and skin eruptions [31,32]. These adverse reactions may compromise drug compliance.
Therefore, the severity of reaction to the medication and patients’ compliance with it are important factors to consider in the management plan. Therefore, the side effects of medication have been accounted for in SPAASMS assessment and are selfrated by patients as nil, mild, moderate or severe side effects.
Additional medication
Medical management of persistent pain often involves a combination of analgesic, psychiatric and/or neuropathic medications [29]. The results of a Finnish study indicate that daily or continuous pain of high intensity resulted in increased frequency of analgesic medication use [33]. Historically, successful pain management has been indicated by decreased frequency of medication use [34]. For moderate to severe persistent pain, long acting opioids, either in the form of oral or trans-dermal medications, are used. They may be used with acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs) for treatment of mild intermittent pain flares. Short acting opioids are often used for moderate to severe break-through pain [29]. Therefore, the frequency of medication used, is an important factor to be considered in persistent pain assessment. We postulate that decreased frequency of medication, especially short acting opioids, would follow decreased pain intensity and frequency of pain flares, because of better pain management.
Additional GP/ED visit
One Australian study has found that patients with back pain visit GP 2.4 times more than patients without it [35]. Another study in UK concluded that medically unexplained abdominal pain, chest pain, headache, and back pain accounted for a significant proportion of consultations in secondary health care facility [36]. Researchers have also reported that depressive symptoms were the major predictor for frequent GP visit [37] and persistent pain frequently co-exists with depressive illness [15]. Therefore, we considered patients’ frequency of Doctor visits for pain relief should also be one of the factors to be determined in assessing persistent pain.
The SPAASMS score was designed to measure the direct and indirect markers of persistent pain, across the above seven domains. For simplicity and ease of administration each component except pain, was self-rated by patients from 0 to 3* on a scale based on severity of symptoms. For pain measurement NRS was used on a scale of 0 to 10*. SPAASMS was recorded and scored to a maximum of 25 at the initial assessment before starting the treatment, excluding side effects of medication. The subsequent score was a maximum of 28 including the side effects (Table 1).
| Pain on Numerical Rating Scale | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||
| No pain |  |
Most pain | ||||||||||
| 0 | 1 | 2 | 3 | |||||||||
| Activity and mobility | Very good | Good | Fair | Nil | ||||||||
| Additional pain medication | Nil | <4 times/month | <8 times/week | >8 times/week or daily | ||||||||
| Additional GP/ED visits | Nil | Once a month | Once a week | >5/month | ||||||||
| Sleep Quality | Very good | Good | Fair | Poor | ||||||||
| Side Effects | Nil | Mild | Moderate | Severe | ||||||||
| Mood | Very Good | Good | Fair | Low | ||||||||
| Total Score=25 (Initial) Total Score=28 (Monthly) |
||||||||||||
Table 1: SPAASMS score card.
Procedure
A study was conducted to test if the SPAASMS scale would indicate treatment efficacy for persistent pain patients. DASS21 is an internationally validated tool to assess Depression, Anxiety and Stress symptoms whereas; PDI is a measure for Disability. Concurrent validity was assessed via the correlation between SPAASMS, DASS21 and PDI at the end of the study, over 9 months. The study was conducted according to ethical guidelines approved by Townsville Hospital Ethics committee.
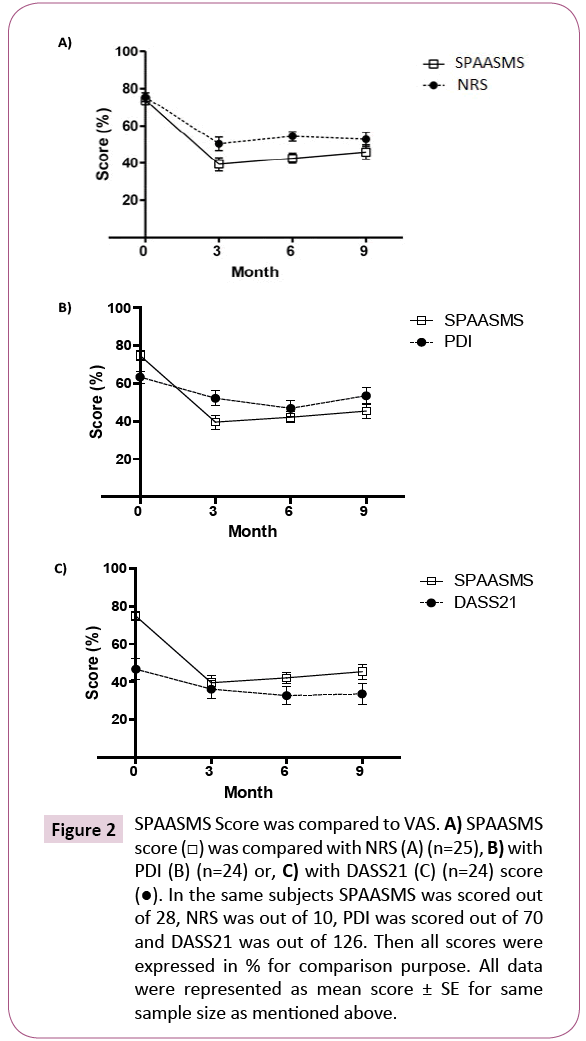
Patients
Patients’ details are outlined in Table 2. In brief, 25 adult patients (mean age (± SD) 47.96 years (± 13.27); 16 male and 9 females) being treated for persistent pain (mean duration (± SD) 13.52 years (± 12.87)) were recruited at the Townsville Hospital Pain Management Clinic. Their progress on treatment was studied using the SPAASMS scale. For uniformity, opioid naïve patients having persistent pain for more than one year, for the greater part of the day or night and deemed appropriate for treatment with transdermal patches were recruited. After history taking, clinical examination, appropriate investigations, and evaluation, treatment was initiated by the senior clinician conducting this trial. The patients were titrated to optimal doses of medications and followed up every three months by for consultation by the same clinician. During treatment, the patients were asked to keep a record of any additional medicines or doctor visits that they made for break through pain and record any increase in daily activities. Patients who had unsatisfactory relief, developed unacceptable or severe adverse reaction/s during their treatment, were given alternative treatment and discontinued from followup. The rest were monitored monthly for 9 months. Monthly SPAASMS scoring was done by an interviewer telephonically using a predetermined, structured questionnaire. The senior clinician evaluated the patients’ progress independently over nine months. Details of any aggravation or improvement of symptoms observed during the three monthly clinical assessments were recorded. Additional support was provided when deemed necessary. Patients completed the DASS21 and PDI questionnaires every three months for comparison with SPAASMS. The final scores of SPAASMS were recorded and the results were collated. A graph was charted following the patients’ progress (Figures 2A and 2B).
| Serial No. | Age | Gender | Diagnosis | Duration Illness (years) |
|---|---|---|---|---|
| 1 | 68 | M | CLBP | 20 |
| 2 | 45 | F | CRPS | 3 |
| 3 | 58 | F | Osteoarthritis, CLBP | 20 |
| 4 | 46 | F | Shoulder Pain | 3 |
| 5 | 59 | F | CLBP | 12 |
| 6 | 34 | M | CLBP, Psoriatic arthritis | 12 |
| 7 | 41 | F | CLBP | 5 |
| 8 | 24 | F | Fibromyalgia, Seronegative Arthritis | 1 |
| 9 | 49 | F | CLBP, Sciatica | 20 |
| 10 | 40 | M | Compression Fracture - spine | 12 |
| 11 | 22 | F | CLBP, Cervical pain | 5 |
| 12 | 53 | M | Osteoarthritis, carpal tunnel syndrome | 34 |
| 13 | 43 | M | CLBP, Cervical pain | 3 |
| 14 | 56 | F | CLBP, Cervical pain | 20 |
| 15 | 39 | M | CLBP | 18 |
| 16 | 65 | F | CLBP, knee pain | 6 |
| 17 | 59 | F | CLBP, Failed back syndrome | 15 |
| 18 | 67 | F | CLBP | 6 |
| 19 | 43 | M | CLBP | 25 |
| 20 | 72 | F | CLBP, Cervical pain | 50 |
| 21 | 39 | M | Coccygeal Fracture | 1 |
| 22 | 32 | F | CLBP, Cervical pain | 1 |
| 23 | 38 | F | CRPS-arm, CRPS - leg | 4 |
| 24 | 62 | M | CLBP | 41 |
| 25 | 45 | F | Cervical pain | 1 |
CLBP: Chronic Low Back Pain; CRPS: Complex Regional Pain Syndrome
Table 2: Participant demographics.
Statistical analysis
Overall assessment of reliability was conducted using the testretest data. A scatter plot was used for graphical assessment of reliability. A concordance correlation coefficient (CCC) was calculated [38]. Cronbach’s alpha was calculated to assess internal consistency of SPAASMS using SPSS (SPSS Inc., PASW version 18, Chicago, Illinois). All other statistical analyses were performed using GraphPad software (Version 5, GraphPad Software, Inc., and La Jolla, CA, USA). Clinical measures concerning pain intensity (NRS), DASS21, PDI, etc., were based on mean, SE and range. Two-way repeated measurement ANOVA was used for comparison between SPAASMS and NRS, DASS21, PDI or NPD, followed by Bonferroni post-tests. Pearson’s correlation coefficient (r-square) was computed to examine the correlation between SPAASMS, NRS, PDI or DASS21scores. The relationship between SPAASMS and NRS or NPD was not checked as NRS was one component of the SPAASMS score card. P values of less than 0.05 were considered as statistically significant.
Results
Twenty patients were interviewed by phone twice (readings 1 and 2), 2 to 4 days apart telephonically. Then a scatter plot was made and CCC was calculated as 0.94 with 95%-confidence interval=0.86, 0.97 (Figure 1) showing high reliability of SPAASMS scoring. Cronbach’s alpha for readings 1 and 2 were 0.66 (P=0.001) and 0.67 (P<0.001), respectively.
We compared SPAASMS with the most vital factor in pain assessment, NRS (Figure 2A). SPAASMS scores showed a similar trend to NRS. Initial scores for SPAASMS and NRS were almost identical. However, with initiation of treatment SPAASMS scores were persistently lower, with scores at 6 months being statistically significant from NRS (P<0.05). No significant differences between SPAASMS and PDI scores were detected throughout the study (Figure 2B). R square for the correlation between SPAASMS and PDI was 0.84 (P=0.085). In contrast, DASS21 scores were always lower in comparison to SPAASMS scores (Figure 2C). The difference between the two scales was significant only at 0 month (P=0.001). R square for the correlation between SPAASMS and DASS21 was 0.89 (P=0.056).
Figure 2: SPAASMS Score was compared to VAS. A) SPAASMS score (□) was compared with NRS (A) (n=25), B) with PDI (B) (n=24) or, C) with DASS21 (C) (n=24) score (â—ÂÂ). In the same subjects SPAASMS was scored out of 28, NRS was out of 10, PDI was scored out of 70 and DASS21 was out of 126. Then all scores were expressed in % for comparison purpose. All data were represented as mean score ± SE for same sample size as mentioned above.
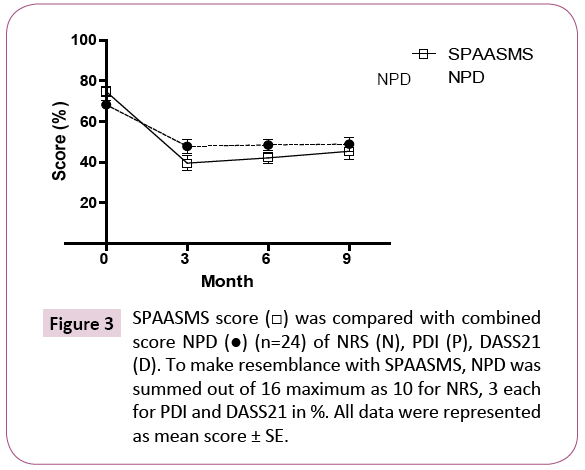
In clinical practice, we consider pain intensity, depression and physical ability as the most important factors to assess persistent pain. Therefore, we compared SPAASMS with combined NRS, PDI and DASS21 scores (NPD) (Figure 3). There was no significant difference between NPD and SPAASMS (P>0.05; respectively).
Discussion
In the present study we have designed the SPAASMS scale to aid clinicians, assessing the progress of a patient on a treatment plan, in a practical and time efficient manner. SPAASMS has taken into consideration Turk et al.’s [39] recommendations that a new measure is required with comparable psychometric properties to existing measures but less onerous for patients to complete. The SPAASMS scale has also endeavoured to incorporate the IMMPACT recommendations to assess pain levels, physical activity, and mood as they would have the most impact on a patient and determine the severity of a patient’s distress [5]. A review determined that quality of sleep, greater usage of medications and of health resources would be the other indirect important markers of the persistent pain condition. Selfreport was used for the assessment of the patient’s condition as advocated by Katz and Melzack [40]. NRS represented more than 35% of SPAASMS score as it measures the most vital component of persistent pain. The remaining six components of assessment were rated equally.
The Reliability Test for SPAASMS score was excellent (Figure 1). Lower NRS indicated patients’ improvement in intensity of pain after treatment (Figure 2A). However, SPAASMS score was even lower than NRS throughout the study. We assume that SPAASMS reflected a greater response to treatment as it included other components of persistent pain assessment. In Figure 2B, PDI and SPAASMS scores both showed a decrease. However, SPAASMS score was lower than PDI that may suggest a better reflection of the treatment response. Again, physical disability as reflected by the multidimensional PDI may not be directly related to persistent pain intensity, however global physical activity levels as reflected by improved ADL are related to pain intensity [13]. Functional improvement in disability may not immediately follow an improvement to nociception because of other factors like deconditioning, wasting of muscles or depression [41]. In addition, the decreased pain intensity could improve other factors like sleep or mood relatively rapidly. Therefore, PDI score may not improve as quickly as SPAASMS. This might have been reflected in the relatively higher PDI scoring. The SPAASMS scale indicated a general tendency in improvement which was maximal at the end of third month as compared to DASS21 (Figure 2C). However, DASS21 seemed to be a more sensitive indicator as it has components to measure different aspects of psychological distress that is, Depression including Anxiety and Stress. No significant difference between SPAASMS and NPD scores was found (Figure 3). During the initial 3 months, SPAASMS and NPD scores declined progressively signifying a successful response to treatment. Individual patient’s scores remained high when they did not respond to treatment or, increased briefly with some precipitating event like unusual increased activity or further trauma. From the 6th month, the trend reversed in both scoring. At the same time, it was clinically observed that several patients developed tolerance or side effects to opioids leading to additional doctor visits and medications. All these changes were more marked in SPAASMS score than NPD. Thus, the initial assessment at the beginning of the study and the progress of the patients’ condition after starting treatment was reflected more strongly on the SPAASMS score. This was likely due to additional indicators of persistent pain being included in this score.
Thus, the SPAASMS score card had the advantage of being a simple, time efficient bed-side clinical assessment tool, and easy for patients. Possibly the most important advantage of the tool was that it indicated specific symptoms of persistent pain, to which the patient had not responded. Further assistance could then be provided, addressing the need according to sub-scale score indications. The scale could also be delivered by phone or by consultation. Furthermore, the patient could be shown objective progress regarding their treatment. However, in this study patients’ satisfaction or rating of improvement/worsening of the pain condition and their dispositions data were not included [42].
The Reliability Test for SPAASMS score was excellent (Figure 1). Hence, we believe that there would be very little room for error. But it would have to be confirmed by larger studies. We do not know what influence, larger number of patients or those on placebo would have on the total scores and rating; future research could be directed to address this variation. This scoring was used only on adults with no intellectual disability, we do not know if this could be used on children or elderly with failing memory. The SPAASMS scoring could be tried on a larger number of patients to test the accuracy of the scoring.
Conclusion
We thus propose the SPAASMS score card as a reliable clinical tool for a rapid measurement of persistent pain. Further refinement of structure and component of SPAASMS, tested on larger number of patients may be regarded in the future.
Acknowledgement
This study was funded by the Private Practice Research Fund of Townsville. The authors thank Ms Helen Karami for collection of Data, Senior Clinical Psychologists Frank McDonald, and Dana Corden for comments and suggestions. We also thank Sameer Mitra for assistance with information technology. The authors have no conflicting financial interests.
References
- Kroenke K (2009) Measuring and distilling the impact of pain. Pain 142: 7-8.
- Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, et al. (2008) Assessment of pain. Br J Anaesth 101: 17-24.
- Gatchel RJ (1999) Perspective on pain: A Historical Overview. In; Gatchel RJ, Turk DC, eds. Psychosocial Factors in Pain Critical Perspective. Guilford Press, New York, pp: 3-17.
- Turk DC, Flor H (1999) Chronic Pain: A Biobehavioral Perspective. In; Gatchel RJ, Turk DC, eds. Psychosocial Factors in Pain. Critical Perspective. Guilford Press, New York, pp: 18-34.
- Turk DC, Dworkin RH, Allen RR, Bellamy N, Brandenburg N, et al. (2003) Core outcome domains for chronic pain clinical trials: IMMPACT recommendations. Pain 106: 337-345.
- Fredheim OM, Borchgrevink PC, Landmark T, Schjødt B, Breivik H (2008) A new schedule for the inventory of pain. Tidsskr 5 Nor Laegeforen 128: 2082-2084.
- Melzack R (2003) Introduction: The pain revolution. In: Melzack R, Wall PD eds. Handbook of Pain Management. Churchill Livingstone, Edinburgh, Scotland, pp: 1-9.
- Turk DC, Melzack R (2001) The measurement of pain and the assessment of people experiencing pain. In; Turk DC, Melzack R (Third Edition) Handbook of Pain Assessment. Guilford, New York, London, pp: 5-8.
- Williamson A, Hoggart B (2005) Pain: A review of three commonly used pain rating scales. J Clin Nurs 14: 798-804.
- Waehrens EE, Amris K, Fisher AG (2010) Performance-based assessment of activities of daily living (ADL) ability among women with chronic widespread pain. Pain 150: 535-541.
- De Gagné TA, Mikail SF, D'Eon JL (1995) Confirmatory factor analysis of a 4-factor model of chronic pain evaluation. Pain 60: 195-202.
- Holroyd KA, Malinoski P, Davis MK, Lipchik GL (1999) The three dimensions of headache impact: Pain, disability and affective distress. Pain 83: 571-578.
- Linton JL (1985) The relationship between activity and chronic back pain. Pain 21: 289-294.
- Robinson ME, Brown JL, George SZ, Edwards PS, Atchison JW, et al. (2005) Multidimensional success criteria and expectations for treatment of chronic pain: The patient perspective. Pain Med 6: 336-345.
- Gureje O, Von Korff, Simon GE, Gater R (1998) Persistent pain and well-being: A World Health Organization study in primary care. JAMA 280: 147-151.
- Patten SB, Beck CA, Kassam A, Williams JV, Barbui C, et al. (2005) Long-term medical conditions and major depression: Strength of association for specific conditions in the general population. Can J Psychiatry 50: 195-202.
- Lépine JP, Briley M (2004) The epidemiology of pain in depression. Hum Psychopharmacol 1: S3-7.
- Croft P, Schollum J, Silman A (1994) Population study of tender point counts and pain as evidence of fibromyalgia. BMJ 309: 696-699.
- Gambassi G (2009) Pain and depression: The egg and the chicken story revisited. Arch Gerontol Geriatr 1: 103-112.
- Moldofsky H (2001) Sleep and pain. Sleep Med Rev 5: 385-396.
- Tang NK, Wright KJ, Salkovskis PM (2007) Prevalence and correlates of clinical insomnia co-occurring with chronic back pain. J Sleep Res 16: 85-95.
- Call-Schmidt TA, Richardson SJ (2003) Prevalence of sleep disturbance and its relationship to pain in adults with chronic pain. Pain Manag Nurs 4: 124-133.
- Belza BL (1995) Comparison of self-reported fatigue in rheumatoid arthritis and controls. J Rheumatol 22: 639-643.
- McCracken LM, Iverson GL (2002) Disrupted sleep patterns and daily functioning in patients with chronic pain. Pain Res Manag 7: 75-79.
- Marty M, Rozenberg S, Duplan B, Thomas P, Duquesnoy B, et al. (2008) Quality of sleep in patients with chronic low back pain: A case-control study. Eur Spine J 17: 839-844.
- Pilowsky I, Crettenden I, Townley M (1985) Sleep disturbance in pain clinic patients. Pain 23: 27-33.
- Atkinson JH, Ancoli-Israel S, Slater MA, Garfin SR, Gillin C (1988) Subjective sleep disturbance in chronic back pain. Clin J Pain 4: 225-232.
- Morin CM, Gibson D, Wade J (1998) Self-reported sleep and mood disturbance in chronic pain patients. Clin J Pain 14: 311-314.
- MARCUS DA (2000) Treatment of non-malignant chronic pain. Am Fam Physician 61: 1331-1338.
- Furlan AD, Sandoval JA, Mailis-Gagnon A, Tunks E (2006) Opioids for chronic noncancer pain: A meta-analysis of effectiveness and side effects. CMAJ 174: 1589-1594.
- Nelson L, Schwaner R (2009) Transdermal fentanyl: Pharmacology and toxicology. J Med Toxicol 5: 230-241.
- Likar R, Kayser H, Sittl R (2006) Long-term management of chronic pain with transdermal Buprenorphine: a multicentre, open-label, follow-up study in patients from three short-term clinical trials. Clin Ther 28: 943-952.
- Turunen JH, Mäntyselkä PT, Kumpusalo EA, Ahonen RS (2005) Frequent analgesic use at population level: Prevalence and patterns of use. Pain 115: 374-381.
- Gatchel RJ (1999) Perspective on Pain: A Historical Overview. In; Gatchel RJ, Turk DC, eds. Psychosocial Factors in Pain Critical Perspective. Guilford Press, New York, p: 12.
- Knox SA, Britt H (2004) The contribution of demographic and morbidity factors to self-reported visit frequency of patients: A cross-sectional study of general practice patients in Australia. BMC Fam Pract 5: 17.
- Reid S, Wessely S, Crayford T, Hotopf M (2001) Medically unexplained symptoms in frequent attenders of secondary health care: Retrospective cohort study. BMJ 322: 767.
- Dowrick CF, Bellón JA, Gómez MJ (2000) GP frequent attendance in Liverpool and Granada: The impact of depressive symptoms. Br J Gen Pract 50: 361-365.
- Lin LI (1989) A concordance correlation coefficient to evaluate reproducibility. Biometrics 45: 255-268.
- Turk DC, Dworkin RH, Burke LB, Gershon R, Rothman M, et al. (2006) Developing patient reported outcome measures for pain clinical trials: IMMPACT recommendations. Pain 125: 208-215.
- Katz J, Melzack R (2001) The McGill pain questionnaire: Development, psychometric properties and usefulness of the long form, short form and short form-2. In: Turk DC, Melzack R, (Third Edn) Handbook of Pain Assessment. Guilford, New York, London, p: 49.
- Fordyce W, McMahon R, Rainwater G, Jackins S, Questad K, et al. (1981). Pain complaint-exercise performance relationship in chronic pain. Pain 10: 311-321.
- Dworkin RH, Turk DC, Wyrwich KW, Beaton D, Cleeland CS, et al. (2008) Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain 9: 105-121.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences