Correlation of Intracranial Hemorrhage and Anticoagulant Medications
Marian SK*, Shreedip P, Timothy W, Keith C and Justus B
CoxHealth, Springfield, USA
- *Corresponding Author:
- Marian SK
CoxHealth
Springfield
USA
Tel: 860-299-5755
E-mail: marian.krasowski@coxhealth.com
Received date: October 10, 2018; Accepted date: November 06, 2018; Published date: November 12, 2018
Citation: Marian SK, Shreedip P, Timothy W, Keith C, Justus B (2018) Correlation of Intracranial Hemorrhage and Anticoagulant Medications. J Surgery Emerg Med Vol.2 No.2:19
Abstract
Abstract With the population of the elderly projected to increase exponentially in the next 10 years, it is becoming even more essential to investigate what causes the elderly to require medical attention. The population in this study involves originates from an area where there is a large elderly population who frequently require hospitalization after a fall, many of whom are taking anticoagulant medications. Objective: This study is aimed at finding statistical correlation in one of the seemingly more common occurrences among Trauma Surgeons in our Level 1 Trauma Center, an elderly patient who suffered a fall and was found to have an intracranial hemorrhage while taking anticoagulants. Design: Retrospective analysis of data from a Level 1 Trauma Center Registry. Setting: Level 1 Trauma Center in Springfield, MO. Data collected October 1, 2015 to February 1, 2017. Measurements: Age, Injury Severity Score (ISS), Type of intracranial hemorrhage, Patient Arrival Date and Time, Discharge Date and Time, Post ED Disposition, Discharge to Location. Results: With the relative risk being greater than one we can conclude there is an increased risk of intracranial hemorrhage (ICH) with the use of anticoagulation in patients greater than age 65 and older. Subdural hematoma was the most common type of ICH in both the anti-coagulated and non-anti coagulated population. Limitations: Retrospective analysis. Accuracy of data depends on accuracy of charted information. Conclusions: Elderly populations are most likely to suffer significant injury with falling from the same level due to a slip or trip and the most common type of ICH was the subdural type across all scenarios of these populations. Patients are more likely to develop ICH if they are on anticoagulants. We were also able to determine that the anticoagulated population is older on average compared to the nonanticoagulated population. Additionally, the anticoagulated population was more likely to be taking Warfarin only for anticoagulation and this same population was more likely to have a SDH. Anticoagulants were statistically shown to increase one’s risk of death due to a fall and subsequent ICH.
Keywords
Hemorrhage; Warfarin; Subdural hematomas; Anticoagulant
Introduction
More than 800,000 patients a year suffer a fall and are subsequently hospitalized for a head injury [1]. Falls are the most common cause of brain injuries related to trauma among adults aged 65 and older and lately have resulted in a statistically significant increase in emergency department visits, hospitalizations and deaths [2]. The population in the USA age 65 and older is 50.8 million as of July 1, 2017 and continues to grow [3]. The number of people aged 65 and older is projected to be 98.2 million in 2060 which will equate to nearly one in four U.S. Residents [4] With the population of the elderly increasing exponentially and an increasing number of those elderly patients taking anticoagulant medications, a deeper look into the risk anticoagulant medications put on the elderly population for an intracranial hemorrhage (ICH) is needed. In this study, we hypothesize that a patient taking an anticoagulant medication will be at a higher risk for an ICH. Since subdural hematomas (SDH) are common in elderly patients due to generalized cerebral atrophy and increased venous fragility associated with aging, we hypothesize that if an elderly patient were to suffer an ICH then it's more likely to be a SDH. We also hypothesize that taking an anticoagulant increases the risk of death due to an ICH. Therefore, we theorize that if an elderly patient who is taking an anticoagulant medication is more at risk of death than if they were not taking an anticoagulant.
Methods
Data was obtained from the CoxHealth level 1 trauma center database in Springfield, MO. We queried all trauma patients from October 1, 2015 to February 1 2017 and found 3062 trauma patients of all ages. We subsequently filtered to look for patients with an ICH as well as patients taking an anticoagulation medication vs. no anticoagulation medication. We accomplished this by using unique identifier codes via the CV5 report writer program.
Results
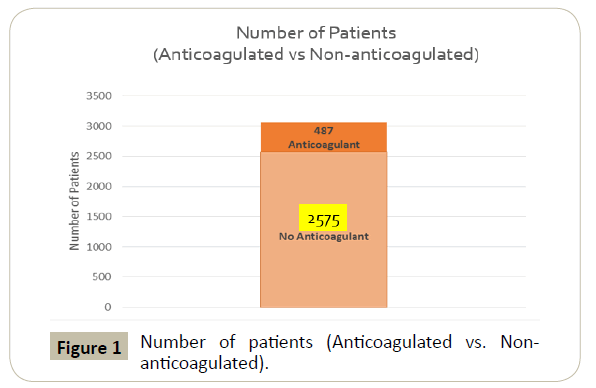
Out of 3062 total patients of all ages, 487 were taking anticoagulant medications while 2575 patients were not Figure 1. Of the 487 anticoagulated, 93 patients (19.1%) developed an ICH and of these 93 patients, nine had expired from their injuries (9.7%).
In the 2575 non-anticoagulated group, 194 patients developed ICH (7.5%) and of these 194 patients, 17 had expired (8.8%).
Age
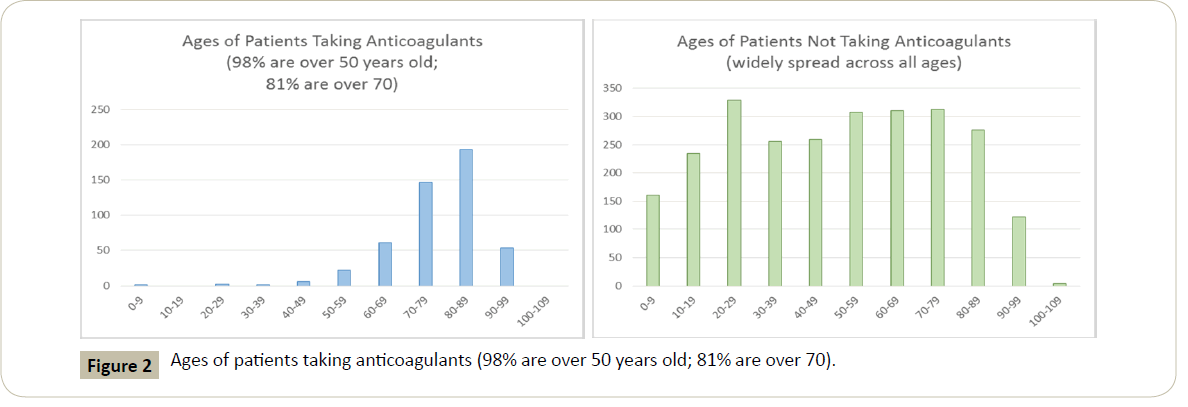
The mean age of the total population studied was 79 years old. In the 487 anticoagulated patients, the mean age was 76.2 while that of the non-anticoagulated population was 70.8 years old (Figure 2).
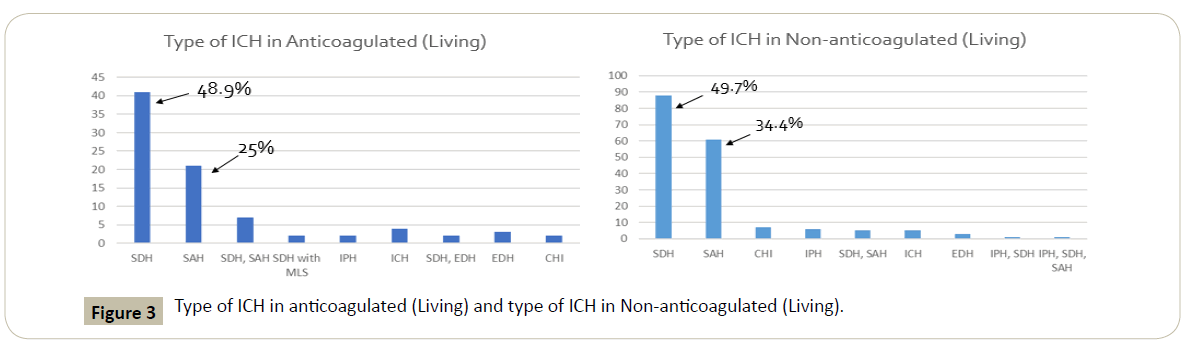
Types of ICH
In those patients taking anticoagulants, SDH and SAH were the most common at 48.9% and 25% respectively. Similarly, in the non-anticoagulation group, SDH and SAH were again the most common with 49.7% and 34.4% respectively.
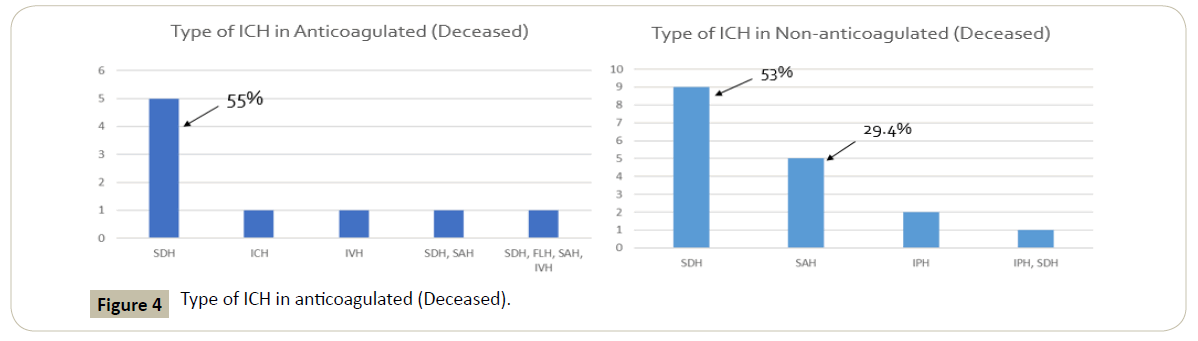
Injury associated with death
The most common ICH involved in patients that died in the anticoagulated group was SDH totaling 55% while all other types of ICH in this group was lower in comparison. In the nonanticoagulated population that had an ICH, the most common ICH involved was SDH at 53% of patients but this time SAH was significantly increased at 29.4% compared to the anti-coagulated population (Figure 3).
Type of anticoagulation and reversal in living
The most common anticoagulation used in the living ICH group was warfarin alone, (25 of the 84 patients). In addition, a combination of warfarin and aspirin occurred in 13 patients along with two other occurrences of a combination therapy. This makes warfarin part of 40 of the occurrences of ICH. 15 out of 25 of those patients on warfarin alone suffered a SDH. The second most common being a combination of Clopidogrel and Aspirin (15 of the 84 patients). Out of the 84 patients on any type of anticoagulation 61 of 84 patients did not require reversal (Figure 4).
Type of anticoagulation and reversal in deceased
In the deceased anticoagulated ICH group, the most common Figure 1 anticoagulation was warfarin alone (3/9) with Warfarin and Aspirin being second most common (2/9). SDH was the most common ICH type in the deceased group and 6 out of 9 patients did not require reversal. The average age of that group was 79 years old. In the deceased non-anti coagulated ICH population, SDH was again the most common type of ICH totaling 10 of 17.
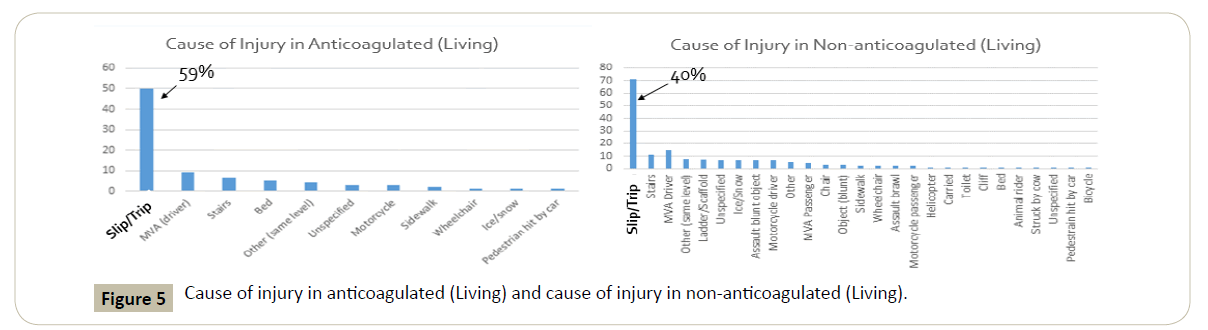
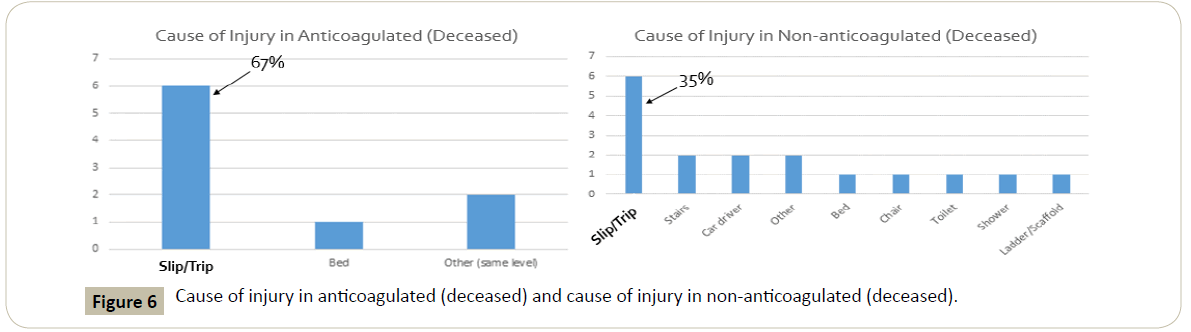
Cause of injury
Fifty of the 84 patients in the living anticoagulated ICH group were injured because of a slip or trip. All other types of injury included motor vehicle accidents (MVA), falling down stairs, falling from the bedside, motorcycle, sidewalk, wheelchair, ice/ snow, and a pedestrian hit by a car. For comparison, the second most common cause of injury in this population was a MVA at nine occurrences. The most common cause for injury in this population is overwhelmingly a slip or trip, which translates to low impact, short distance falls from about 3 feet according to registry criteria. In the deceased anticoagulated ICH population, the injury from a slip or trip was again the most common at six of nine patients.
In the non-anticoagulated population, the cause for injury was again overwhelmingly due to a slip or trip in both the living and deceased at 71/177 (40%) and 6/17 (35%) respectively. The second most common in the living population here was again a MVA however, that was lower in comparison at only 13 patients with the rest of the causes much lower than that. It is also important to note that our data showed other low impact falls that comprised a significant amount when totaled together. This included falls from a bedside, chair, toilet, and shower (Figures 5 and 6).
Gender
Our data showed that as far as gender goes, there were no statistically significant differences between the occurrence of an ICH overall and no difference between the type (SAH and SDH).
Percent increase and relative risk
In any case, there was about a 2% increase in the likelihood of an ICH if a patient is using an anticoagulant. More specifically, there is about a 1.3% increase in the likelihood of a SDH if a patient is using an anticoagulant while the increase in likelihood of an SAH among those taking an anticoagulant is around 0.5%.
The relative risk (RR) was calculated at 1.09, concluding that there is an increased risk of ICH in anticoagulated patients.
Discussion
One of the more common scenarios encountered in our trauma center located near a high population of the elderly is the elderly anticoagulated patient who presents after a fall with an ICH and has an INR out of range for surgery. Some of the reasons why anticoagulants are thought to increase the risk of ICH includes:
1. Increased age and use of anticoagulants increases risk of ICH independently of one another.
2. There is a small increase in risk of ICH from anticoagulant use so it is significant enough to trial different anticoagulants to search for incidence of deaths from ICH.
3. Currently Warfarin alone increases risk for ICH after trauma, making it important to determine INR range and fatality rate in these patients.
The elderly are more susceptible to intracranial hemorrhages, specifically subdural hematomas, in part due to their susceptibility to falls and brain atrophy from the normal aging process [5]. Falls are the main cause of injuries and accidental deaths in older people. The normal changes associated with aging all contribute to this common scenario. Some of the more common conditions that contribute to an increased likeliness of a fall includes poor hearing and eyesight. Illnesses and physical conditions can affect strength and balance. Poor lighting, throw rugs, and even small dogs can make someone more likely to slip or trip. The side effects of some medicines can upset balance and make a fall more likely. Medicines for depression, sleep problems and high blood pressure often cause falls. Some medicines for diabetes and heart conditions are common cause for concern with falling as well, which in the elderly, are some of the most common prescribed medicines. The chance of a fall can also increase if a routine medication has been changed within the past two weeks [6].
With all of these causes for concern in mind, it’s also important to consider the known death rates associated with falls in the elderly. These death rates in the U.S. have increased by 3.0% per year from 2007 to 2016 [7]. Furthermore, falls are the leading cause of injuries requiring emergency treatment in adults aged 65 and older and lead to more hospital admission and deaths than any other type of trauma [8]. Identification of the causes for life threatening injury is an important topic that needs constant research in order to help improve the causes for injury and death in this population. One of the main facets of this effort is screening and prevention.
The Stopping Elderly Accidents, Deaths & Injuries (STEADI) helps healthcare providers make fall prevention routine. This is something that needs to be done by all health care providers at each visit [9]. Providers should:
1. Ask patients if they have fallen in the past year, feel unsteady, or worry about falling.
2. Review medications and stop, switch, or reduce the dose of medications that could increase the risk of falls.
3. Recommend vitamin D supplements.
Along with the risks of falling combined with atrophy of the brain due to normal aging, there is an increased risk in ICH and death in the elderly. These falls lead to head trauma that can cause rupture of bridging veins in the brain of a patient. These veins are susceptible to rupture mainly in the elderly because atrophy of the brain from aging causes these vessels to stretch, reducing their ability to compensate for movement of the brain during a fall [10].
Compared with children, elderly persons who fall are 10 times more likely to be hospitalized and eight times more likely to die as the result of a fall [10]. Data indicates that the trauma patient with preinjury anticoagulation such as warfarin or even aspirin who has an intracranial injury has a four to five-fold higher risk of death than the non-anticoagulated patient [11].
Among patients with ICH, prior use of non-oral anticoagulants (NOACs) or warfarin was associated with higher in-hospital mortality compared with no oral anticoagulants (OACs). Prior use of NOACs, compared with prior use of warfarin, was associated with lower risk of in-hospital mortality [12].
Fall injuries associated with rugs and carpets are common and may cause potentially severe injuries. Older adults, their caregivers, and emergency and primary care physicians should be aware of the significant risk for fall injuries and of environmental modifications that may reduce that risk.
Conclusion
Through this retrospective analysis, we can confirm elderly populations are still most likely to cause significant injury via falling from the same level due to a slip or trip and the most common type of ICH was the subdural type across all scenarios of these populations. Patients are more likely to develop ICH if they are on anticoagulants. We were also able to deduce that the anticoagulated population is older on average compared to the non-anticoagulated population. Additionally, the anticoagulated population was more likely to be taking Warfarin only for anticoagulation and this same population was more likely to have a SDH. Lastly, considering the relative risk calculated, it seems as though anticoagulants do increase risk of death due to a fall that results in ICH.
References
- (2018) Important Facts About Falls. Retrieved July 3 from https://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html
- (2018) Traumatic Brain Injury in the United States. Accessed July 18 https://www.cdc.gov/traumaticbraininjury/pdf/blue_book.pdf
- (2018) United States Census Bureau Quick Facts. Accessed July 18 https://www.census.gov/quickfacts/fact/table/US/PST045217
- (2018) United States Census Bureau Facts for Features Released April 10, 2017. Accessed July 18 https://www.census.gov/newsroom/facts-for-features/2017/cb17-ff08.html
- (2018) Neuroscience Basic Core III Traumatic Epidural vs Subdural Hematoma. Accessed August 3, https://casemed.case.edu/clerkships/neurology/neurlrngobjectives/epidural%20and%20su bdural.html.
- (2018) What causes Falls in the Elderly? How can I prevent a Fall? Available at https://www.aafp.org/afp/2000/0401/p2173.html Accessed August 3.
- (2018) Deaths from Falls Among Persons Aged 65 and older – United States, 2007-2016 Available at: https://www.cdc.gov/mmwr/volumes/67/wr/mm6718a1.htm Accessed August 3, 2018.
- Slipping and tripping: fall injuries in adults associated with rugs and carpets.
- STEADI Materials for Healthcare Providers. Available at:
- (2018) Falls in the Elderly. Available at https://www.aafp.org/afp/2000/0401/p2159.html Accessed August 3.
- (2018) Intracranial complications of preinjury anticoagulation in trauma patients with head injury. Available at: https://www.ncbi.nlm.nih.gov/pubmed/12394864 Accessed August 3.
- (2018) Association of Intracerebral Hemorrhage among Patients Taking Non-Vitamin K Antagonist vs Vitamin K Antagonist Oral Anticoagulants with In-hospital Mortality Available at: https://www.ncbi.nlm.nih.gov/pubmed/29372247 Accessed August 13.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences