Complicated Idiopathic Ileo-ileal Intussusception in a 45-year-old Male: A Case Report
Nkembe Marius Nkembe1*, Clarence Mbanga2 and Valirie Ndip Agbor3
1Franciscan Catholic Health Centre Mayo Darle, Adamawa Region, Cameroon
2Mankon Sub-divisional Hospital, Mankon, Northwest Region, Cameroon
3Ibal Sub-divisional Hospital, Oku, Northwest Region, Cameroon
- *Corresponding Author:
- Nkembe Marius Nkembe
Franciscan Catholic Health Centre Mayo Darle, Adamawa region, Cameroon
Tel: 00237675393276
E-mail: mariusnkembe@yahoo.com
Received date: April 19, 2016; Accepted date: May 25, 2016; Published date: May 29, 2016
Citation: Nkembe NM, Mbanga C, Agbor VN (2018) Complicated Idiopathic Ileo-ileal Intussusception in a 45-year-old male: A Case Report. Int J Case Rep Vol.2 No.3.
Copyright:© 2018 Nkembe NM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Intestinal intussusception is a surgical emergency often responsible for bowel obstruction in children below three years of age. Intussusception occurring in adults is rare. In fact, it represents just 5% of all intussusceptions, of which only 1% present with complications such as bowel obstruction and peritonitis. We present the case of an idiopathic ileoileal intussusception in a 45-year-old male, presenting as peritonitis.
Case presentation: A 45-year-old male from the Adamawa region of Cameroon, with no peculiar past medical history, presented with a four days history of exacerbating abdominal pains, repeated vomiting and obstipation. Clinical and paraclinical findings were in favor of peritonitis. An exploratory laparotomy was done, and an ileoileal intussusception seen per-operative. The intussusceptum was necrotic and the intussuscipiens oedematous and perforated. Both (intussuscipiens and intussusceptum) were void of any structural lesions responsible for the intussusception. Resection and anastomosis was done, followed by post-operative antibiotherapy. The postoperative period was unremarkable and the patient was discharged on day 10. A follow up visit for 2 weeks after discharge revealed a healing abdominal wound and normal bowel functions.
Conclusion: Intussusception is rare in adults, and its complications even rarer. We described a rare case of idiopathic intussusception in an adult presenting as peritonitis. We therefore advise that physicians working in emergency departments consider intussusception in adults presenting with peritonitis.
Keywords
Idiopathic; Intussusception; Adult; Peritonitis; Case report
Background
Intussusception is a condition in which part of the intestine (intussusceptum) enfolds into an adjoining part of the intestinal lumen (intussuscipiens), usually resulting in bowel obstruction [1]. Intussusception is the most common cause of bowel obstruction in the paediatric population, where it is most often idiopathic [2,3]. Intussusception is a rarity in adults. It represents only 5% of all cases of intussusception, and is mostly secondary to an underlying medical condition such as a tumour [1]. In adults, the classic triad of pain, hematochezia and a palpable mass is most often absent as nonspecific chronic symptoms predominantly dominate the clinical presentation [4]. This makes it difficult to arrive at a definitive diagnosis prior to surgery. In children, management is most often by an imaging technique (Barium enema) whereas in adults, surgery is usually required to correct the problem [5]. Intussusception in adults is rare, and its complications such as bowel obstruction and peritonitis even rarer. A detailed search of MEDLINE through PubMed from inception to 11 January 2018 revealed three cases of idiopathic intussusception in adults have been reported to the best of our knowledge in sub-Saharan Africa and just one case of adult intussusception presenting as peritonitis [6]. Herein, we present a case of an idiopathic ileoileal intussusception in a 45- year-old male complicated by peritonitis secondary to bowel perforation.
Case Presentation
A 45-year-old male farmer from the Adamawa region of Cameroon with an unremarkable past history, was rushed into the emergency department of our institution, following the worsening of a four days history of intermittent and Para-umbilical abdominal pains, associated to repeated bouts of coffee brown vomitus and constipation. He consulted at a remote health centre two days before and was given intravenous analgesics after suspicion of an acute abdomen, before referral. However, a two day delay in arrival to our health facility after referral was noted due to financial reasons.
Physical examination revealed an irritable patient screaming in agonizing pain which was alleviated upon adoption of the lateral recumbent position. He equally presented with a fever of 38.5°C, tachycardia at 115 beats per minute and a blood pressure of 100/60 mmHg. The abdomen was flat, stationary during breathing, rigid (cardboard rigidity) with generalize guarding and bowel sounds were absent. The rigidity prevented deep palpation of the abdomen. Hernia orifices were not bulging. Rectal exam revealed a rectum void of faecal material and a tender Douglas pouch. A full blood count done revealed an elevated white cell count at 17800 cells/μl with granulocytic predominance. A diagnosis of peritonitis was made and the decision for an exploratory laparotomy taken. The patient and caregivers were immediately counseled, and requested to sign an informed consent. Pre-operatory workups (bleeding time, clotting time, and Human immune-deficiency virus serology and serum creatinine) were urgently done and all found to be unremarkable. The Anaesthesiologist was consulted, a stat dose of intravenous antibiotics (two grams of Ceftriaxone) and fluid bolus (1000cc of normal saline) administered, catheters (nasogastric and urinary) placed and the patient was quickly rushed to the operating theatre and prepared for surgery.
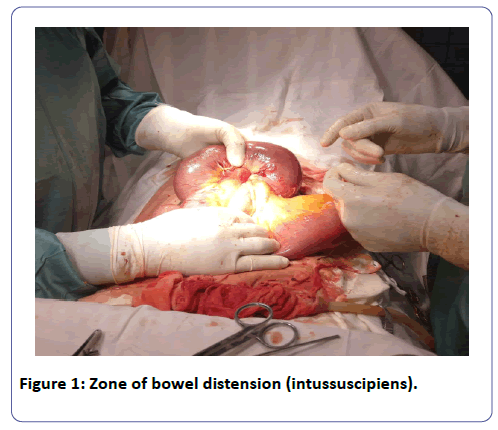
We proceeded with the traditional full-length midline incision, dissecting the skin and underlying tissues, layer by layer. Per-operative findings revealed a pus-like fluid oozing out of the peritoneum, a dilated portion of the small intestine suggestive of an Ileoileal intussusception, and a 2 cm large perforation on the intussuscipiens (Figure 1). The intussuscipiens was oedematous, friable and twisted around the mesenteries at its neck making reduction difficult (Figure 1).
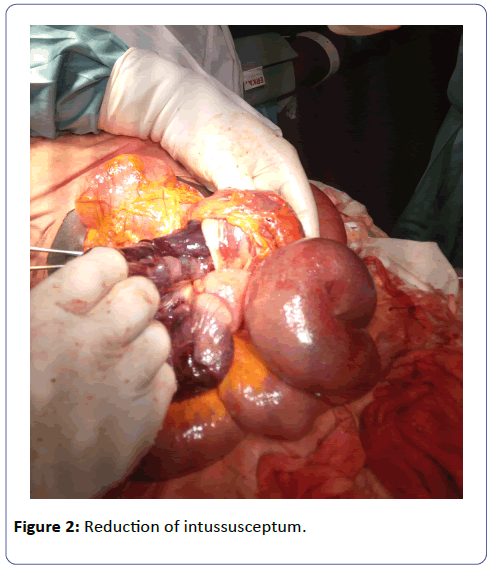
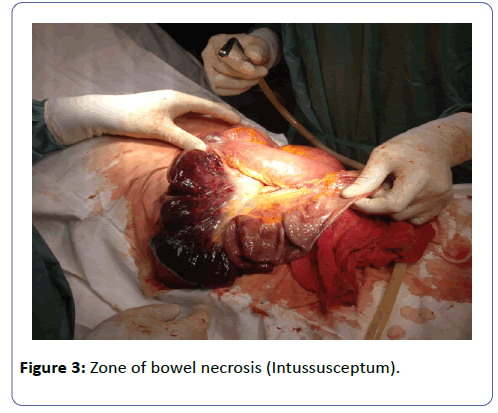
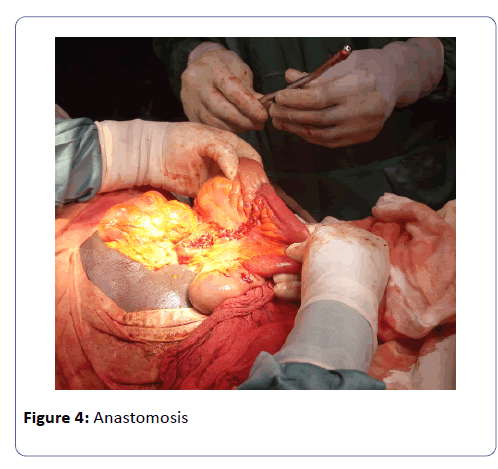
The mesenteries around the neck of the intussuscipiens were ligated and the intussusception was then reduced by gentle traction and retrograde pressure from the apex, revealing a segment of necrotic bowel of about 28 cm long (Figures 2 and 3). The necrotic bowel was resected and an ileoileal anastomosis was done (Figure 4). Further exploration of the abdominal cavity did not reveal any other abnormality. Peritoneal lavage was done with lukewarm normal saline, a drain placed and abdomen closed. Post-operative management consisted of intravenous triple antibiotherapy (ceftriaxone two grams daily, Gentamycin 80 mg 12 hourly and Metronidazole 500 mg eight hourly) and analgesics (tramadol 100 mg 12 hourly) for five days; intravenous Ranitidine 50 mg (prevention of stress ulcers) eight hourly and intravenous fluids (2000cc daily) for two days. The post-operative period was unremarkable. The nasogastric tube and urinary catheter was removed on post-operative day one and progressive oral sips started on post-operative day two. The abdominal drain was removed on post-operative day five, and the patient was discharged on post-operative day ten with no fresh complaints. A follow-up visit two weeks after discharge revealed good surgical wound healing and full restoration of bowel function.
Discussion
Barbette reported the first case of intussusception in Amsterdam in 1674 [7]. This was then further elaborated in 1789 by John Hunter [8]. Sir Jonathan Hutchison performed the first surgery on a child with intussusception in 1871 [9].
This disease has long been considered one of infancy and early childhood. It is rare in adults with a child to adult ratio of nearly 20:1 [10]. Adult intussusception thus represents 5% of all intussusception. In children, nearly 80% are idiopathic whereas in adults a defined aetiology is always found in 90% of cases [11]. Malignant neoplasms are the leading cause of intussusception in adults, accounting for 66% of colonic intussusception and 30% of small bowel intussusception [11]. The most common malignant cause of large bowel intussusception is colon adenocarcinoma, whereas metastasis is usually responsible for most intussusceptions of the small bowel [12,13]. Other lesions incriminated include, adenomatous polyps, lipomas, fibromas, harmatomas, adhesions from previous abdominal surgery, cystic fibrosis, scleroderma, coeliac disease, inflammatory bowel disease, appendicitis and rectal foreign bodies [14]. Only sixteen per cent of small bowel and 5% of large bowel intussusception are idiopathic [14].
Intussusception is classified according to their location into four categories: entero-enteric (ileoileal), which is confined to the small bowel; colo-colic, which involves the large bowel only; and ileo-colic and ileo-caecal, where the lead point is the ileocaecal valve [11].
Most case reports on adult intussusception were ileo-colic in nature and were either secondary to intestinal lipomas, a malignancy, Crohn’s desease, Merkel’s diverticulum or other benign intestinal lesions [11,14-16]. Just three cases of idiopathic adult intussusception have been reported in Sub-Saharan Africa [6]. Most of these cases were uncomplicated and chronic in presentation. Our case was peculiar in that it was an ileoileal idiopathic intussusception presenting with peritonitis.
The clinical presentation of intussusception in adults is diverse, with the triad of cramping abdominal pains, currant-jelly stools and a palpable tender abdominal mass very rare [4]. The presenting symptoms in adults are nonspecific with majority of cases being reported as chronic, consistent with partial bowel obstruction [5,11]. Chronic intermittent cramping abdominal pains, nausea, vomiting, gastro-intestinal bleeding especially among the elderly, and constipation are usually the presenting complaints in adults [14,17]. Our patient however came in with an acute presentation due to the complications which already ensued. Our patient equally denied episodes of abdominal pains, constipation and vomiting in the past. We therefore had a case of a sudden onset of bowel intussusception in an adult of unknown aetiology.
Intussusception usually results from an imbalance in the longitudinal forces along the intestinal wall, which causes one area of bowel to invaginate into the lumen of the adjacent bowel [18]. If the progression is rapid, and the mesentery lax, an ileoileal intussusception can progress into the colon and even prolapse out of the anus [18]. Other complications of intussusception include; bowel obstruction, intestinal haemorrhage, necrosis and perforation, and sepsis from an undetected peritonitis [19]. The presentation of our patient could be explained by the fact that the obstruction which follows intussusception causes accumulation of gas and fluid within the intestinal lumen proximal to the site of obstruction. The resulting bowel distension and rise in intraluminal pressure impairs micro vascular perfusion to the intestines (lymphatic, venous and finally arterial) leading to ischemia, necrosis, gangrene and ultimately perforation. The sipping of bowel contents together with commensal germs into the peritoneum then causes peritonitis. Our patient presented with this complication probably due to the late arrival at the emergency department.
Abdominal computed tomography scan is the goal standard for the diagnosis of adult intussusception, where a soft tissue intestinal mass with an outer intussuscipiens and a central intussusceptum appearing as a “target” or a “sausage-shaped” is the pathognomonic scan sign [14,20]. Other helpful imaging techniques include: air-fluid levels on a plain abdominal X-ray if there is already obstruction and the “doughnut sign” on abdominal sonography if done at the early stages [20]. Although, a plain abdominal X-ray and ultrasonography are cheap and readily available in resource-limited settings, their use in clinical practice is limited by: their low sensitivity, operator dependence and poor image quality due to the presence of gas in the intestines, especially in the later stages of bowel obstruction [10,21]. Our patient presented with clinical peritonitis and anguishing abdominal pains, hence further imaging investigations were not dimmed necessary given the fact that the diagnosis of peritonitis is mostly clinical.
Given that the aetiology and diagnosis of adult intussusception is often vague and taking into cognizance the high incidence of malignancy as aetiology, the preferred treatment is usually bowel resection during an exploratory laparotomy or laparoscopy [12]. Pre-operative pneumatic or hydrostatic reduction is not suggested as definite treatment for adults as is the case with children [11]. Bowel resection taking into consideration the location and pathologic characteristics of the underlying lesion is the management of choice [12,22]. Reduction of the intussusceptum before resection remains controversial. However in elderly individuals (greater than 60 yrs), given the high incidence of malignancy, it is recommended not to reduce the intussusception as reducing may increase the risk of intraluminal seeding, venous dissemination, perforation and peritoneal seeding of tumour cells [10,11]. However several others believe that the risks are theoretical and that gentle traction should be attempted in selected cases to avoid unnecessary resection of healthy bowel [10,23]. In this case we performed reduction by gentle traction despite the fact that the intussuscipiens was already oedematous, perforated and friable, this in a bit to avoid unnecessary resection of healthy bowel.
Conclusion
Intussusception is rare in adults, and its complications are even rarer. Pre-operative diagnosis is difficult, especially when presenting with a complication. The diagnosis of intussusception therefore warrants a high index of suspicion by emergency physicians when faced with a case of peritonitis. Treatment is most often by bowel resection with or without prior reduction depending on the presentation and aetiology.
Authors’ Contributions
NMN: managed the patient, acquisition of data and write-up of initial manuscript; CM: acquisition of data and critical revision of manuscript; VNA: acquisition of data and critical revision of manuscript; all authors read and approved the final manuscript.
Acknowledgement
The authors would like to thank the patient and his family for allowing them to publish this work and to thank the staff of the Franciscan catholic health centre for their assistance in managing the patient.
References
- Intussusception - Symptoms and causes - Mayo Clinic https://www.mayoclinic.org/diseases-conditions/intussusception/symptoms-causes/syc-20351452 (accessed 6 January 2018).
- Chalya PL, Kayange NM, Chandika AB (2014) Childhood intussusceptions at a tertiary care hospital in northwestern Tanzania: a diagnostic and therapeutic challenge in resource-limited setting. Ital J Pediatr 40: 28.
- Edino ST, Ochicha O, Mohammed AZ, Anumah M (2003) Intussusception in Kano: a 5-year analysis of pattern, morbidity and mortality. Niger J Med 12: 221-224.
- Segovia-Lohse HA (2011) Adult intussusception with perforation and secondary peritonitis. Case report. Cir Cir 79: 252-255, 274-277.
- Azar T, Berger DL (1997) Adult intussusception. Ann Surg 226: 134-138.
- Gbenga OJ, Olusoga AO, Taye IJ, Adetunji OJ, Brown AD, et al. (2017) Intussusception in Adult : Case Series and Literature Review. Int J Health Sci Res 7: 325-330.
- de Moulin D (1985) Paul Barbette, M.D.: a seventeenth-century Amsterdam author of best-selling textbooks. Bull Hist Med 59: 506-514.
- Master surgeon: John Hunter. - Version details Trovehttps://trove.nla.gov.au/work/10458233?q&versionId=12183686 (accessed 6 January 2018).
- Wales AE (1963) Sir Jonathan HUTCHINSON, 1828-1913. Br J Vener Dis 39: 67-86.
- Gupta RK, Agrawal CS, Yadav R, Bajracharya A, Sah PL (2010) Intussusceptions in Adults: A Retrospective Interventional Series of Cases. Heal Renaiss 8: 158-165.
- Marinis A, Yiallourou A, Samanides L, Dafnios N, Anastasopoulos G, et al. (2009) Intussusception of the bowel in adults: a review. World J Gastroenterol 15: 407-411.
- Barussaud M, Regenet N, Briennon X, de Kerviler B, Pessaux P, et al. (2006) Clinical spectrum and surgical approach of adult intussusceptions: a multicentric study. Int J Colorectal Dis 21: 834-839.
- Nagorney DM, Sarr MG, McIlrath DC (1981) Surgical management of intussusception in the adult. Ann Surg 193: 230-236.
- Lu T, Chng Y (2015) Adult intussusception. Perm J 19: 79-81.
- Yalamarthi S, Smith RC (2005) Adult intussusception: case reports and review of literature. Postgrad Med J 81: 174-177.
- Singhal S, Singhal A, Arora PK, Tugnait R, Tiwari B, et al. (2012) Adult ileo-ileo-caecal intussusception: case report and literature review. Case Rep Surg 2012: 4.
- Begos DG, Sandor A, Modlin IM (1997) The diagnosis and management of adult intussusception. Am J Surg 173: 88-94.
- Intussusception: Practice Essentials, Background, Etiology and Pathophysiologyhttps://emedicine.medscape.com/article/930708-overview#a5 (accessed 14 January 2018).
- Intussusception: Practice Essentials, Background, Etiology and Pathophysiologyhttps://emedicine.medscape.com/article/930708-overview#a7 (accessed 14 January 2018).
- Gayer G, Zissin R, Apter S, Papa M, Hertz M (2002) Pictorial review: adult intussusception--a CT diagnosis. Br J Radiol 75: 185-190.
- Minaya Bravo AM, Vera Mansilla C, Noguerales Fraguas F, et al. (2012) Ileocolic intussusception due to giant ileal lipoma: Review of literature and report of a case. Int J Surg Case Rep 3: 382-384.
- Olasky J, Moazzez A, Barrera K, Clarke T, Shriki J, et al. (2009) In the era of routine use of CT scan for acute abdominal pain, should all adults with small bowel intussusception undergo surgery? Am Surg 75: 958-961.
- Akagi I, Miyashita M, Hashimoto M, Makino H, Nomura T, et al. (2008) Adult intussusception caused by an intestinal lipoma: report of a case. J Nippon Med Sch 75: 166-170.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences