Comparison of Surgical and Medical Treatment in Patients with Haemorrhagic Stroke
Ashraf Mahmood1*, Asaad Zulfiqar2, Anjum Sheraz3
1Department of Neurosurgery, SIMS/ Services Hospital, Lahore
2Department of Neurology and Internal, SIMS/Services Hospital, Lahore
3Department of Medicine, SIMS/Services Hospital, Lahore
- *Corresponding Author:
- Ashraf Mahmood
Department of Neurosurgery,
SIMS/ Services Hospital,
Lahore,
Tel: 201 091949393;
E-mail: drashraf1964@gmail.com
Received Date: May 25, 2020; Accepted Date: August 23, 2021; Published Date: September 02, 2021
Citation: Ashraf M (2021) Comparison of Surgical and Medical Treatment in Patients with Haemorrhagic Stroke J Brain Behav Cogn Sci Vol: 4 No: 4.
Abstract
Optimal management of spontaneous intracerebral haemorrhage (ICH) remains one of the highly debated areas in the fields of neurosurgery. Earlier studies comparing open surgical intervention with best medical management failed to show a clear benefit. More recent experience minimally invasive techniques have shown greater promise. We present our experience of 46 patients who presented to neurosurgery, neurology, Medical, Surgical and allied specialities at SIMS / Services Hospital Lahore with clinical and CT scan Brain based diagnosis of Haemorrhagic Stroke and comparison as per outcome between Surgical and Medically treated patients. This is an ongoing study.
Keywords
Haemorrhagic stroke
Introduction
New guidelines for prevention of stroke were released dated October 28, 2014 by the American Heart Society (AHA).It points out that 76% of the strokes are first events” – emphasizing the importance of primary pre- vention.10 potentially risk factors explaining 90% of the risk of stroke [4].
| A | Genetic Factors | 1.Physical Inactivity and Dyslipidaemia |
| B | Diet and Nutrition | Hypertension Obesity Diabetes Smoking |
| C | Cardiac | 1.Atrial fibrillation |
| Conditions | 2.Asymtomatic Carotid Stenosis | |
| D | Haemotological Conditions | Sickle Cell Disease Hyperhomocystinurea Hypercoagulability Antiplatelet Agents; Aspirin |
Table 1: Risk factors for first stroke.
Material and Methods
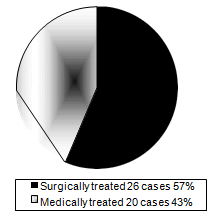
Out of total number of 46 patient on our ongoing study, these were broadly divided into two groups surgical and medical treated groups (Figure 1).
These were further discussed under inclusive and
exclusive criteria.
A. Inclusive Criteria.
B. Exclusive Criteria.
Inclusive Criteria
This was further discussed under:
Age / sex. GCS.
Volume and site of ICH.
Age / Sex Age
Age ranged from 28 – 70 year (mean 50.9 years) (Figure 2).
Sex
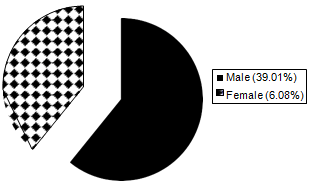
Out of 46 victims fulfilling the inclusion criteria, 28(39.1%) were male and 18 (6.08%) were female. (Figure 3)
GCS
9 out of 26 patients in surgical group presented with GCS less than 8 and 5 in medical group (Table 3), while 17 patients were GCS more then 9 and 15 res- pectively in surgical and medical group.
| Presenting GCS | No of cases | |||
|---|---|---|---|---|
| ≤ 8 | Surgical | 9 | Medical | 5 |
| ≥ 9 | Surgical | 17 | Medical 15 | |
Table 2: Glasgow Coma Scale (GCS).
Volume and Site of ICH (Cm)3
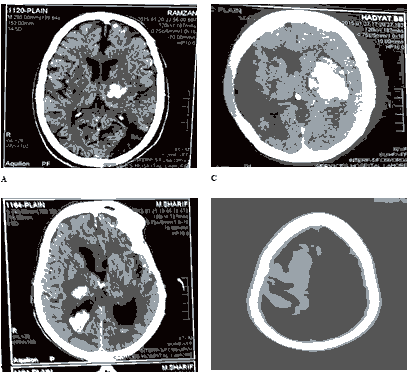
Regarding volume of ICH, 11 patients in surgical and 17 in medical groups were having between 30 – 60 (Cm)3 while 15 in surgical and 3 in medical group hav- ing > 60 (Cm)3 (Figure 4: a,b,c,d).
Exclusive Criteria
Comorbid Conditions like uncontrolled HTN, Co- agulopathies, uncontrolled DM, bronchopneu- monia. All these patients were excluded for surgi- cal group and were treated medically, but this was not a strict policy as if a medically treated deve- loped progressive neurological deficit, he was sup- posed to be transferred to the surgical group; al- though in our ongoing study, still we did not come across such patient but may be in future we can find such a case.
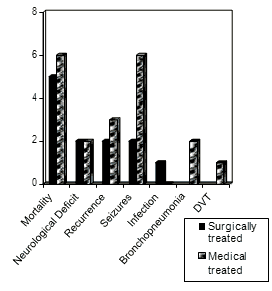
Complications (Fig. 5) Surgically Treated Patients (26) Mortality 5 (19%).
Neurological deficit 3 (11.5%).
Recurrence 2 (7.6%).
Seizures 1 (3.8%).
Medically Treated Patients (20)
Mortality 6 (30%).
Neurological deficit 2 (10%).
Recurrence 3 (15%).
Seizures 6 (30%).
Bronchopneumonia 2 (10%).
DVT 1 (5%).
Results
46 Adults patients meeting the inclusive criteria were included in our ongoing study, 26 patients in surgical group and 20 patients in medical group (Fig. 1).
5 out of 25 surgically patients were expired and the mortality was 25%.
Age
Age of these victoms ranged from 28 – 70 years. Mean (50.9 years).
Graph
Sex
Out of 46 victoms adult fulfilling the inclusion criteria, 28 were male (6.08%), 18 were female (39.1%) (Figure 3).
Complications
Surgically Treated Patients (26).
Mortality 5 (19.2%).
Neurological deficit 3 (11.5%).
Recurrence 2 (7.6%).
Seizers 1.
Infection 1 (Figure 5).
Medically treated patients (20)
Mortality 6 (30%).
Neurological deficit 2 (10%).
Recurrence 3 (15%).
Seizers 6.
Bronchopneumonia 2.
DVT 1 (Figure 5).
| Volume of ICH (cm3) | No of Patients | |||
|---|---|---|---|---|
| 30 – 60 | Surgical | 11 | Medical | 17 |
| > 60 | Surgical | 15 | Medical | 03 |
Table 3: Volume of ICH (cm3).
Discussion
Intracerebral Haemorrhage (ICH) is more than twice as common as Subarachnoid haemorrhage (SAH) and is much more likely to result in death or major disabi- lity than cerebral infarction or SAH.1
Out of a number of randomized clinical trials, only the results of 4 small randomized surgical trials (353 total patients) and 4 small medical trials (513 total pat- ients) of ICH had been published.13
Decompressive Hemicraniectomy with or without clot evacuation for large spontaneous supraten- torial haemorrhage.
Conclusion was early HC (Hemicraniectomy) with or without clot evacuation is feasible and safe for man- aging spontaneous ICH (Intracerebral haematoma) and recommendation was for patients with large non-domi- nant hemisphere ICH who were moribund at presentat- ion.
In one study over 7 years HC was performed in 73 patients with clot evacuation in 86% and HC alone in 14%. The average ICH volume was 81cc and the med- ian HC surface area was 105 cm2.26 comatosed pati- ents at initial presentation three month functional out- comes were favourable in 29%.Unfavourable in 44% and 27% patients expired. Admission GCS, dominant hemisphere ICH location and haematoma volume con- tributed significantly to the outcome.
Meta-Analysis of randomized studies of surgery for spontaneous supratentorial intracerebral hae- morrhage.
The efficacy of surgical treatment on supratentorial intracerebral haemorrhage (STICH) is not conclusive, although many studies have been performed. 2,3 Rele- vant factor such as injury inflicted to the brain by dif- ferent kinds of surgery, degrees of severity and locat- ion of intracerebral haemorrhage (UCH) should be tak- en into consideration for a better appraisal of too effi- cacy of surgery on STICH.6
In this study the appraised primary outcome was death and the secondary outcome was death or depen- dence.
In one study carried out in Korea, Moon KS et al, showed that craniotomy with removal of hemtoma confirmed good outcome amoung the 48.65% of vic- tims with intracerebellar hemorrhage [8].
Management of Hemorrhagic stroke can be carried out medically for selected patients; but surgery needs to be carried out in large number of victims.9-13
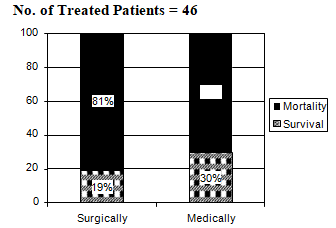
Out of 26 patients in surgical group 5 expired (19%), 21 survived (81%) mortality 19% but 21 survived pie diagram 3. In contrast out of 20 patients in medical tre- ated group, 06 expired (30%) while 14 survived (70%)(Figure6).
This again indicates a better outcome in surgical treated group vs medical treated group.
Conclusion
Optimal cure of spontaneous intracerebral haemorr- hage (ICH) is highly debatable neurosurgical problem. Past studies on comparison between surgical inter- vention with best medical management failed to show a clear improvement. However recent studies of mini- mally invasive techniques have shown greater pro- mise.5 As per our ongoing study better outcome in sur- gical survival group (81%) as compare to (70%) medi- cal treated group also confirms a better outcome in surgical treatment over the medical treatment.
So we still recommend early surgery for the vic- tims of hemorrhagic stroke weather open or minimally invasive particularly in our population.
References
- Imran Altaf and Anjum Habib Vohra (2014) Surgical manage- ment of spontaneous supratentorial intracerebral hemor- rhage. Pak J of Neurol. Surg 18: 39-43.
- Youshua Esquenazi, SeanI, Saritz, Ramy ElKhoury, Megan A, et al. (2015) Surgical treatment for intracerebral hemorrhage (STI- TCH): A single – center, randomized clinical trial 128: 117-122.
- Chih-Dong Yang, Yu-Weichzn, Hui-Chehwu (2014) Meta- Analysis of randomized studies of surgery for spon- taneous supratentorial intracerebral haemorrhage. For- moson. Journal of Surgery, June 3: 90-98.
- Margestern L B, Hemphill III J C, Becherk, Broderick J.P, ConullyJr. E S., et al. (2010) Guidelines for the management of spontaneous intra- cerebral hemorrhage: A guidelines for healthcare pro- fessionals from the American Heart Association/ Ame- rican stroke Association, stroke 41: 2108- 2129.
- Dey, Mahua MD; stodnik, Agnieszka MSc; Awad, Issam A (2014) MD Section Editor(S); Bendok, Bernard R. MD; Levy, Elad I.MD. Spontaneous intracerebral and Intraventricular hemorrhage: Advances Primary Inva- sive Surgery and Thrombolytic Evacuation, and Les- sons Learned in Recent Trials. Neurosurgery 74: 142-1501.
- A Devid Mendelow, Barbara A Gregson, Elise N Rowan, Gordan D Murray, et al. (2013) Anil Gholkar, Patrick M Mitchell. Early Surgery Versus initial Conservative Treatment in patients with spontaneous supratentorial lobar intracerebral hematoma (STICH): a randomized trial. The Lancet, 382: 397-408.
- Broderick J, Bott T, Tomsick T, Miller R, Huster G, et al. (v) Intra cerebral hemorrhage is more than twice as common as subarachnoid hemorrhage. J Neurosurg. 78: 188-191.
- Broderick JP, Adams HP, barson W et al. Guidelines for the Management of Spontaneous Intracerebral Hem- orrhage. Stroke 30: 905-915.
- Moon KS, Park HK, Yoon SM, Bae HG, Yun G, et al. (2006)Choi SK. Outcomes in the managenment of spontaneous cerebellar hemorrhage. J Korean Neurosurg Soc 40: 234-238.
- Hanggi D, Steiger HJ (2008) Spontaneous intracerebral hae- morrhage in adults: a literature overview, 150: 371-379.
- Chalela JA, Kidwell CS, Nentwich LM, Luby M, But-man JA, et al. (2007) Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective com- parison. Lancet 369: 293-298.
- Yamamoto T, Nakao Y, Mori K, Maeda M (2016) Endoscopic hematoma evacuation for hypertensive cerebellar hem- orrhage. Minim Invasive Neurosurg 49: 173-178.
- Guidelines for the Management of Spontaneous Intra- cerebral hemorrhage in – Mario Zuccarello, Derk Krieger, Marc Meyberg, Lewis Morgenstern, Christo- pher S (2019). Ogilvy, Paul Vespa, Joseph Broderick, Er Con- nolly, Edward Feldmann. Daniel Henley, Carlos Kase, Association Stroke Concil, High Blood.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences