Comparison of Recombinant and Urinary HCG on Oocyte/Follicle Ratio and Oocytes Maturation in Advanced Maternal Age
Zakwan Khrait*
Specialist Reproductive Endocrinology and Infertility, Medcare Fertility Center, Jumeira 3, Dubai, UAE
- *Corresponding Author:
- Zakwan Khrait
Specialist Reproductive Endocrinology and Infertility
Medcare Fertility Center, Jumeira 3, DUBAI, UAE
Tel: +971555242644
E-mail: zakwankhrait@hotmail.com
Received date: August 27, 2017; Accepted date: September 18, 2017; Published date: September 26, 2017
Citation: Khrait Z (2017) Comparison of Recombinant and Urinary HCG on Oocyte/Follicle Ratio and Oocytes Maturation in Advanced Maternal Age. J Reproductive Endocrinol Infert Vol.2:24. doi: 10.21767/2476-2008.100024
Copyright: © 2017 Khrait Z. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Objectives: To study the efficacy of recombinant HCG (rHCG) compared to urinary HCG (uHCG) for triggering of ovulation and stimulation of final Oocyte maturation in advanced age woman with the poor ovarian response that underwent ovarian stimulation and ICSI.
Design: This study was an observational study performed in Medcare Fertility Centre, DUBAI, UAE between April 2016 to July 2017. This study was reviewed and approved by the institutional review board and Ethics Committee of Medcare Fertility Centre.
Patients: Sub fertile couples undergoing triggering of ovulation as part of an assisted reproductive cycle using either recombinant HCG versus urinary HCG.
Interventions: rHCG preparations versus uHCG for triggering of ovulation. Dose, route and schedule of rHCG and uHCG injected were considered.
Primary outcomes: Measure the numbers of oocytes retrieved per number of aspirated follicles and determines the Oocytes/follicles ratio. Secondary outcomes measures were the total number of oocytes retrieved, the number of mature oocytes.
Results: The primary outcome indicated that uHCG was more effective than rHCG in regards to the number of follicles retrieved. The ratios of oocytes retrieved per follicle and total matured oocyte per oocyte retrieved is also greater for Pregnyl (uHCG).
Conclusion: The two types of HCG ( uHCG and rHCG), both medicines have effect on triggering ovulation and stimulation of maturation of oocytes. But with advanced maternal age there is a clear significant effect on the ratio of total matured oocyte per oocyte retrieved which is greater for Pregnyl (uHCG).
Pregnyl therefore has more effect on triggering ovulation and oocyte maturation in comparison with rHCG. For antagonist protocol was the preferred medicine is Ovitrelle® (rHCG) while, for Long Agonist, the preferred triggering medicine is Pregnyl® (uHCG).
Keywords
Human chorionic gonadotropin (HCG); In-vitro fertilization (IVF); Oocyte/Follicle ratio; Advanced maternal age; Poor Ovarian response
Introduction
Luteinizing hormones (LH) surge is essential in the final stages of follicular maturation for triggering follicle rupture, expelling the oocyte from the follicle. In addition, the LH surge promotes luteinization, forming an active corpus luteum. These effects of LH are essential for conception to occur. In assisted conception, human follicle (HCG) has been used for several years to mimic the endogenous LH surge due to considerable structural similarities between HCG and human LH, and hence both hormones stimulate the same receptor [1]. Human Chorionic Gonadotrophin (HCG) has been used for over 25 years as a therapeutic analogue for LH to induce ovulation in women [2]. Specifically, in patients undergoing In-vitro fertilization (IVF) cycles, follicular stimulation with Gonadotrophins (urinary or recombinant FSH and LH) [3,4] is followed by administration of HCG, which is used for inducing final follicular maturation and formation of the corpus luteum [5].
For at least 3 recent decades, uHCG is collected from urine of pregnant women, which has been clinically used for triggering of ovulation and luteinization in anovulatory women [6]; however, there are potential disadvantages associated with uHCG, including interbatch inconsistencies; large quantities of starting material required for purification; possible contamination by other urinary proteins that may result in local, post-injection side-effects experienced by some patients; and a movement to avoid human source materials [7].
More recently, recombinant HCG (rHCG) with high specific activity has become available. Recombinant HCG is produced in a Chinese hamster ovary cell line expressing the genes for the alpha and beta subunits of HCG, and the protein is purified using stepwise chromatography [6]. The pharmacokinetic profile of rHCG is comparable to that of uHCG with linearity over a dose range of 500–20,000 IU and a terminal elimination half-life of approximately 30 h [8,9].
The objective of this study was to evaluate the clinical outcomes of patients undergoing IVF using rHCG, compared with patients using uHCG for final follicular maturation in IVF programme. Patients recruited for this study are those with a poor responder indications needing assisted reproduction. The effect of findings in the poor ovarian response patients was evaluated in addition to the type of HCG [10].
Material and Methods
Study design
This observational study was conducted using data accumulated in a group practice that utilizes a single IVF laboratory (Medcare Fertility Clinic- DUBAI). This study was reviewed and approved by the institutional review board and Ethics Committee of Medcare Fertility Centre and all volunteers for participation in this study were informed regarding the purpose and method of the study.
All Poor responder patients undergoing IVF from April 2016 to July 2017 “16 months”, (were available for review), and Institutional review board approval was not collected because this was an observational study which was not routinely done.
The patients for the study were considered according to the Bologna criteria definition of poor ovarian response (POR) in a simple and reproducible manner, at least two of the following three features must be present: (i) advanced maternal age or any other risk factor for POR; (ii) a previous POR; and (iii) an abnormal ovarian reserve test. The aim was to study randomized controlled trials (RCTs) comparing rHCG preparation with uHCG for inducing final follicular maturation in patients undergoing assisted conception and methods of randomization and allocation concealment were considered.
Patient selection
Patients were advanced age women undergoing triggering of ovulation as part of an assisted reproductive cycle using either rHCG preparation versus uHCG in the protocol of ovulation induction. A total of 85 patients were eligible using the inclusion criteria for ovarian stimulation cycles by the ICSI program for Oocytes freezing (Pooling) and were recruited into this study. These Inclusion criteria are:
• Age≥38 years.
• Basal Follicular Stimulation Hormone (FSH)<16 IU/L.
• Low ovarian reserve based on antral follicle count≤5.
• Low Antimullerian Hormone (AMH)≤0.8 ng/mL.
The patients were stimulated and treated in the same clinic and by same physicians and Embryology team.
Drug administration
The rHCG preparation versus uHCG for triggering of ovulation, drug dose, route and schedule of rHCG and uHCG injected were considered. Patients underwent ovarian stimulation by either GnRH Agonist Long Protocol (Gonapeptyl0.1, Ferring Pharmaceuticals, Germany) or GnRH antagonist protocol (Cetrorelix Acetate Injection®; Cetrotide®, Serono, Italy). Ovarian stimulation was administered as recombinant FSH (rFSH; Gonal- F®, Serono) alone or in combination with human menopausal Gonadotrophins (Menopure®, Ferring Pharmaceuticals, Kiel, Germany).
Group A: Patients who received an intramuscular injection urinary HCG (PREGNYL®, Organon, Oss, The Netherlands) 10,000 IU.
Group B: Patients who received a subcutaneous injection of 250 μg recombinant hCG (Ovitrelle®, Merck Serono, Modugno- Italy).
Monitoring of cycle was done by serial vaginal ultrasonography and measurement of serum Estradiol level, stimulation sheets were well completed with the number of follicles with different sizes. When at least two dominant follicles reached to 18 mm in mean diameter or two follicles with a mean diameter larger than 16 mm diameter and one by mean diameter>18 mm was observed in vaginal sonography, the patients were randomly divided according to the Triggering Medicine into two groups:
Oocyte retrieval
In both groups, Transvaginal ultrasound-guided oocyte retrieval by using a 17 gauge needle was performed 35 hours after menopausal injection. The numbers of retrieved oocytes were recorded. Standard laboratory protocols were followed and approximately two hours after retrieval the cumulus cells were removed and an assessment of Oocyte maturity under an inverted microscope (germinal vesicle, metaphase I, metaphase II, atretic or degenerative) were made. Metaphase II oocytes (mature oocytes) were characterized by the presence of the first polar body, metaphase I oocytes was characterized by the absence of both germinal vesicle and first polar body and prophase I oocytes was characterized by its distinct germinal vesicle.
Outcome assessment
Primary Outcomes: The primary outcome was (i) the numbers of oocytes retrieved per number of aspirated follicles; and (ii) find out Oocytes/follicles ratio.
Secondary Outcomes: Secondary outcome was (i) the number of mature oocytes obtained; maturation rates of oocyte was defined as the numbers of mature oocytes per numbers of total retrieved oocytes.
Statistical analysis
Statistical analysis was carried out using the statistical package for the social science (IBM SPSS version 20.0 for Windows).
Results
For the study, A total of 94 patients participated, and were divided into two groups, group A (received uHCG) 51 patients, and group B (received rHCG) 43 patients respectively.. Basic characteristics of patients observed include age, number of total number of follicles; oocyte and matured oocyte retrieved were expressed in mean, standard deviation, minimum and maximum values and shown in Table 1.
| Age | No. of follicles<14 mm | No. of oocytes retrieved | No. of matured oocytes retrieved | |
|---|---|---|---|---|
| Mean | 41.51 | 6.77 | 5.81 | 4.5 |
| Standard deviation | ± 2.53 | ± 4.19 | ± 3.96 | ± 3.22 |
| Minimum | 38 | 1 | 0 | 0 |
| Maximum | 46 | 18 | 17 | 14 |
Table 1: Baseline characteristics of all patients treated with uHCG or rHCG (n=94).
Group A and B were also assessed individually in the similar fashion and shown in Table 2 and Table 3.
| Age | No. of follicles<14 mm | No. of oocytes retrieved | No. of matured oocytes retrieved | |
|---|---|---|---|---|
| Mean | 41.29 | 7.27 | 6.69 | 5.33 |
| Standard deviation | ± 2.41 | ± 4.26 | ± 4.14 | ± 3.47 |
| Minimum | 38 | 1 | 1 | 1 |
| Maximum | 46 | 18 | 17 | 14 |
Table 2: Baseline characteristics of patients treated with uHCG (n=51).
| Age | No. of follicles<14 mm | No. of oocytes retrieved | No. of matured oocytes retrieved | |
|---|---|---|---|---|
| Mean | 41.77 | 6.16 | 4.77 | 3.51 |
| Standard deviation | ± 2.67 | ± 4.07 | ± 3.51 | ± 2.60 |
| Minimum | 38 | 1 | 0 | 0 |
| Maximum | 46 | 17 | 16 | 14 |
Table 3: Baseline characteristics of patients treated with rHCG (n=43).
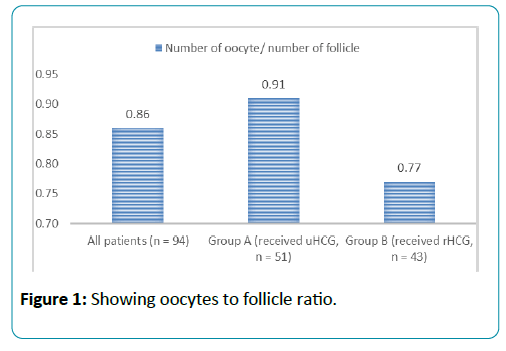
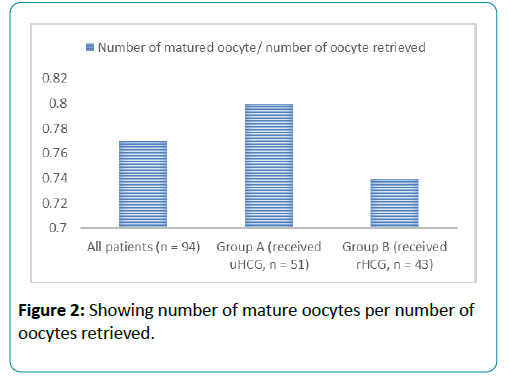
Retrieved oocyte to follicle ratio was shown in Table 4 and Figure 1. Mature oocyte to retrieved oocyte ratio was shown in Table 5 and Figure 2. Finally, an independent sample t-test was done which showed significant differences in the number of oocytes retrieved and the number of matured oocyte between group A and B (p-value 0.019 and 0.006 respectively).
| All patients (n=94) | 0.86 |
| Group A (received uHCG, n=51) | 0.91 |
| Group B (received rHCG, n=43) | 0.77 |
Table 4: Number of oocytes per number of follicles.
| All patients (n=94) | 0.77 |
| Group A (received uHCG, n=51) | 0.8 |
| Group B (received rHCG, n=43) | 0.74 |
Table 5: Number of matured oocyte per number of oocyte retrieved.
An independent samples t-test was conducted to compare the number of oocytes retrieved and the number of mature oocytes in uHCG and rHCG groups.
There was a significant difference in the scores for the number of oocytes retrieved in two groups (p-value=0.019, mean difference 1.92 when uHCG>rHCG, df: 92, SE: 0.80).
There was also a significant difference in the scores for the number of matured oocyte in two groups (p-value=0.006, mean difference 1.82 when uHCG>rHCG, df: 92, SE: 0.64).
Discussion
This study was observe and compare two HCG types (uHCG and rHCG) and their effect on follicular Triggering, number of oocytes retrieved and total number of matured oocyte in relation to advanced maternal age in women with poor ovarian response and the primary outcome indicated that indeed uHCG was more effective than rHCG in regards to the number of follicles retrieved, The ratios of oocytes retrieved per follicle and total matured oocyte per oocyte retrieved is also greater for Pregnyl (uHCG).
Pregnyl therefore has more effect on triggering ovulation increasing retrieval and oocyte maturation, This is contrary to the result of the study by The European Recombinant Human Chorionic Gonadotrophin Study Group 2000, which found that recombinant HCG is associated with more improvement in stimulation of ovulation and with more matured oocyte and improved tolerance and is thus likely to have higher patient acceptability which is a clear, clinical advantage.
In this study, we observed that uHCG performed well at every stage. So, to sum up, urinary HCG shows higher efficacy than recombinant HCG in terms of the number of oocytes per aspirated follicles and oocyte maturation in selected patients undergoing ICSI. However, larger randomized trials are needed to generalize the use of uHCG over HCG.
Conclusion
The two types of HCG ( uHCG and rHCG), both medicines have effect on triggering ovulation and stimulation of maturation of oocytes. But with advanced maternal age there is a clear significant effect on the ratio of total matured oocyte per oocyte retrieved which is greater for Pregnyl (uHCG).
Pregnyl therefore has more effect on triggering ovulation and oocyte maturation in comparison with rHCG.
For antagonist protocol was the preferred medicine is Ovitrelle® (rHCG) .while for Long Agonist, the preferred triggering medicine is Pregnyl® (uHCG).
Implications for Research
Wide analysis is needed between urinary and recombinant HCG to assess the role of rHCG and uHCG in bringing about follicular development and matured oocytes retrieval.
Acknowledgement
I will like to thank Medcare Fertility Clinic- DUBAI and all patients who participated in this study.
References
- Pierce DW, Parson TF (1981) Glycoprotein hormones: Structure and function. Annu. Rev. Biochem 50: 465-495.
- Gemzell C. (1965) Induction of ovulation with human gonadotropins. Recent Progress in Hormone Research 21: 179-204.
- Caglar GS. (2005) Recombinant LH in ovarian stimulation. Reproductive BioMedicine Online 10, 774-785.
- Gomez Palomeres JL (2005) LH improves early follicular recruitment in women over 38 years old. Reproductive BioMedicine Online 11, 409-414.
- Humaidan P, Ejdrup Bredkjaer H, Bungum L, Bungum M, Grondahl ML, et al. (2005) GnRH agonist (buserelin) or hCG for ovulation induction in GnRH antagonist IVF/ICSI cycles: a prospective randomized study. Hum Reprod 20: 1213-1220.
- Lei Z, Mishra S, Zou W, Xu B, Foltz M, et al. (2001) Targeted disruption of luteinizing hormone/human chorionic gonadotropin receptor gene. Mol Endocrinol 15: 184-200.
- The European Recombinant Human Chorionic Gonadotrophin Study Group (2000) Induction of final follicular maturation and early luteinization in women undergoing ovulation induction for assisted reproduction treatment-recombinant HCG versus urinary HCG. Hum Reprod 15: 1446-1451.
- Lathi RB, Milki AA (2001) Recombinant gonadotropins. Current Womens Health Reports 1, 157-163.
- Trinchard Lugan I, Khan A, Porchet HC, Munafo A (2002) Pharmakokinetics and pharmacodynamics of recombinant human chorionic gonadotropin in healthy male and female volunteers. Reproductive BioMedicine Online 4, 106-115.
- Chang P, Kenley S, Burns T (2001) Recombinant human chorionic gonadotropin (rhCG) in assisted reproductive technology: results of a clinical trial comparing two doses of rhCG (Ovidrel) to urinary hCG (Profasi) for induction of final follicular maturation in in vitro fertilization-embryo transfer. Fertility and Sterility 76, 67-74.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences