Comparative Tick-Borne Encephalitis (Virus) Surveillance in Belgium 2009-2015: Experiences with Diagnostic Tests, Sentinel Species and Surveillance Designs
Sophie Roelandt1*, Vanessa Suin2, Steven Van Gucht2,3, Yves Van der Stede3 and Stefan Roels4
1Unit of Epidemiology, Risk Assessment and Surveillance (ERASURV), Operational Directorate of Interactions and Surveillance, Veterinary and Agrochemical Research Centre (CODA-CERVA), Brussels, Belgium
2National Reference Centre of TBEV, Viral Diseases, Communicable and Infectious Diseases, Scientific Institute of Public Health (WIV-ISP), Brussels, Belgium
3Department of Virology, Parasitology and Immunology, University of Ghent, Merelbeke, Belgium
4Unit of Orientation and Veterinary Support (OVS), Operational Directorate of Interactions and Surveillance, Veterinary and Agrochemical Research Centre (CODA-CERVA), Brussels, Belgium
- *Corresponding Author:
- Sophie Roelandt
Unit of Epidemiology
Risk Assessment and Surveillance (ERASURV)
Operational Directorate of Interactions and Surveillance
Veterinary and Agrochemical Research Centre (CODA-CERVA)
Brussels, Belgium
Tel: +32-2-379-0430
E-mail: sophie.roelandt@coda-cerva.be
Received Date: December 14, 2016; Accepted Date: July 19, 2017; Published Date: July 26, 2017
Citation:Roelandt S, Suin V, Gucht SV, Stede YV, Roels S (2017) Comparative Tick- Borne Encephalitis (Virus) Surveillance in Belgium 2009-2015: Experiences with Diagnostic Tests, Sentinel Species and Surveillance Designs. J Zoonotic Dis Public Health. 1:4.
Abstract
When it is not overtly affecting human beings, the Tick-Borne Encephalitis Flavivirus (TBEV) remains mostly unnoticed during its enzootic cycles within vectors and unaffected animal species. Until recently, Belgium was “presumed” free of this important neuro-pathogenic virus without any scientific substantiation. Nonetheless, Belgium is clearly at risk of Tick-Borne Encephalitis (TBE) emergence and incursions from endemic zones in the neighboring countries.
This comparative review paper describes 5 Belgian veterinary serological studies with enzyme-linked immunosorbent assays and seroneutralisation tests (ELISA/ SNT), in which several surveillance schemes were used (active/passive, risk-/ laboratory-/range-based) in classic TBE sentinel species (dogs, cattle, roe deer, wild boar). Additionally, passive syndromic surveillance in two medical laboratories resulted in inconclusive medical data. Details are given on the scientists’ experiences with available first/second line diagnostic tests and with the different surveillance methods/survey designs.
Each of the veterinary studies clearly demonstrated the presence of TBEV-specific antibodies in Belgian sentinels, sometimes even at high seroneutralisation (SNT) titers, while the medical data remain so far inconclusive, despite positive reactions of some patients in some TBEV-tests. These results have substantiated our suspicion of TBEV-presence in Belgium from 2010 onwards and have allowed sentinel comparisons based on “suitability criteria”. Furthermore, the studies have highlighted the need for further veterinary validation of commercial ELISA-tests in comparison to the gold standard SNT.
Keywords
Tick-borne encephalitis (virus); Wild boar; Roe deer; Sentinel species; Seroneutralisation test
Introduction
The Western/European subtype of Ticktick-Borne Encephalitis Virus (W/Eu-TBEV) or Frühsommer Meningoenzephalitis (FSME) has been the most important, highly pathogenic and neurotropic arthropod-borne flavivirus in Europe for a long time [1-4]. This flavivirus is carried by tick vectors: Mostly by sheep ticks Ixodes ricinus [5,6] and to some extent by the ornate dog tick Dermacentor reticulatus [7].
Tick-Borne Encephalitis (TBE) has become a considerable public health risk in many European countries with currently on average 3,000 hospitalized encephalitis-meningitis-myelitis cases per year, and with long-term sequelae and disability in up to 60% of patients [3-4,8]. The strong increases (1970-2000) and fluctuations (>2000) in human TBE incidence in Central and Eastern European countries and the emergence of the disease in Scandinavian countries and France (>2000), have sparked international concern and research [1,9-16].
In general, domestic and wild animals appear to be relatively less frequently infected and affected by TBEV. Although in most of the infected animal species there is viremia and seroconversion without clinical signs [17-24], TBEV can nevertheless cause general and multifocal neurological clinical signs in dogs and horses [25-31]. Additionally, domestic animals may carry infected ticks from endemic to non-endemic areas and into close vicinity of humans [17,20,27,32-36].
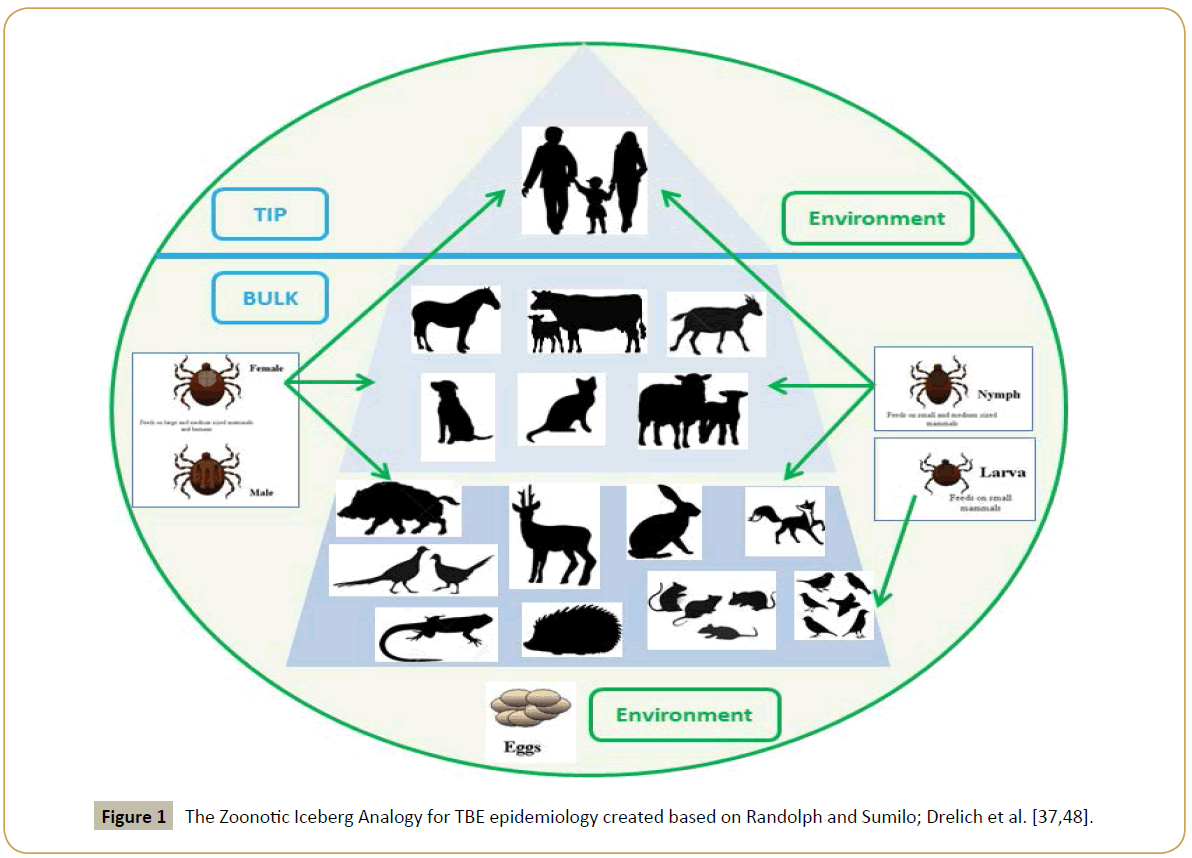
The zoonotic iceberg analogy, as proposed by Randolph and Sumilo [37], allows capturing the complexity of real-life TBEV epidemiology and surveillance (Figure 1). It has been amply shown in several countries that the majority of human TBEV exposures do not lead to clinical signs; hence the confirmed cases represent only the very tip of the zoonotic iceberg [37,38]. When it is not overtly affecting human beings, the TBE-flavivirus remains mostly unnoticed during its enzootic cycles within its vectors and unaffected animal species [37,38]. This “bulk” of the iceberg may be much larger and may involve a large variety of domestic and wild animal species, all known to be I. ricinus hosts [20,24].
As a natural result, there can exist discordance between clinical case prevalence in humans and the prevalence of TBEV in ticks and sentinels in an endemic area [39-44]. For these ecoepidemiological reasons, it is stated by international bodies and many scientists that medical TBE case reporting alone is unreliable to characterize a geographical area or public health risk, even in regions where TBE is highly endemic [4,8,45].
Consequently, both veterinary and tick studies have clearly proven their added value in known TBE endemic areas and specifically in areas or countries with few or no human cases and/or few suspected/endemic areas, as an early warning for suspected endemic areas, such as in Norway, Denmark, Japan, the Netherlands, Luxembourg, Spain. Veterinary TBEV sentinel surveillance studies were recently reviewed [29,46,47]. Appendix A for a reproduction of the review tables in Roelandt, 2016 [47].
Despite a total lack of confirmed human TBE cases in Belgium, here are strong suspicions in the Belgian medical-scientific community that some cases may have occurred in the last decade (pers. comms.) and favorable environmental/climatological (a) biotic conditions for Ixodid ticks and TBEV are present. Belgium is clearly at risk of TBE emergence and incursions from endemic zones in neighboring countries Germany and France [48,49].
The aim of this paper is to review the TBEV surveys performed by different Belgian research institutes in humans and in sentinel animal species between 2000 and 2016. The goal of this comparative paper is to draw some lessons from these studies to enable the design of a potential future national one health TBE(V) surveillance and to estimate the public health risk of this emerging tick-borne disease for Belgium.
Materials, Medical and Veterinary Belgian TBEV Studies*
In the following subsections, the diagnostic tests and survey designs of each of the five Belgian TBEV-studies will be briefly described. These survey characteristics are then summarized in Table 1. There are restrictions on the availability of raw materials or information from the studies to which the authors did not participate… *Any materials, raw data and protocols associated with each original publication should be requested from the respective contact authors.
| Medical Surveillance | QAMH | IPH | ITM |
|---|---|---|---|
| Year Sampled | 2000-2009 | 2009-2014 | 2014-2016 |
| Sampling | Hospitals | Lyme Referral Hospital |
Hospitals |
| Strategy | Passive (catchment area) | Passive/Enhanced (catchment area) |
Passive (catchment area) |
| Criteria Humans | Tick bite Lyme or TBE suspected Clinical CNS | Lyme or TBE suspected Clinical CNS + Lyme tests negative |
Lyme or TBE suspected Clinical CNS |
| Sample Size | n=359 | n=113 | n=40 |
| Detection Limit 95% confidence | ≥0.85% | ≥2.50% | ≥7.50% |
Table 1: Summary of sampling strategies in Belgian medical surveys. Strategy, sample sizes, selection criteria and potential TBEV-seroprevalence detection limits if TBEV is present.
Medical passive surveillance in Humans
During 2000-2016, no autochthonous TBE cases were reported and the virus was not considered to be endemic in Belgium [8,50- 52]. In this time frame, there was only one published paper which tried to identify TBE in four human patients with a viral CNS infection of unknown etiology from Belgium. None of the four Belgian patients included in this study were confirmed as a TBE case [53]. During this whole period, passive medical surveillance was performed at only one laboratory at a time: Queen Astrid Military Hospital, i.e. QAMH (QAMH, 2000-2011), the Belgian Institute of Public Health (IPH, 2010-2015) and the Institute of Tropical Medicine, i.e. ITM (ITM, 2014-ongoing) (Table 1).
The QAMH (Brussels) performed the first serological first-line screening with the Virotech® IgG/IgM ELISA (Sekisui Diagnostics®- Genzyme Virotech) in 359 suspect tick bite and neurology patients. Of these, 55 tested IgG positive (15.32%) and 19 tested IgM positive (5.29%). However, none of these results could be confirmed in SNT and patient histories are unknown.
Since 2010, the TBE National Reference Centre (NRC) at the Institute of Public Health, i.e., IPH (Brussels) has used the European case definition [8,54] and has offered serological and Polymerase Chain Reaction (PCR) screening to the medical sector as part of a diagnostic service of the referral laboratory and a limited passive surveillance system with voluntary reporting of Central Nervous System (CNS) cases 8. During 2010-2016, the Belgian TBE-NRC (WIV-ISP) has been using Progen Immunozym FSME/TBEV IgM and IgG kits to screen human patients [55,56] and the TBEV-SNT as a confirmation test [57]. SNT-results from ≥1/10 onwards are considered sufficiently protective against clinical TBE, but titers are usually much higher after full vaccination [58-60]. Additionally, comparative immunofluorescence assay IFA Biochips (Mosaic 3, Euroimmun®, Germany) [61] and qRT-PCR been available at the IPH and current best practices in TBE-diagnostics are followed.
As such, TBE tests have been performed on patients suspected of neuroborelliosis and on cases that were sent by general practitioners or hospitals based on direct TBE clinical suspicion. In 60 samples from 2009, 10 reacted in IgG ELISA (borderline or positive), one was positive in IgM-ELISA and seven reacted positive in SNT. In 2014, 53 suspected patients were tested and a total of 18 samples were IgG-ELISA-positive or -borderline, while three were SNT-positive, but none were IgM-ELISA-positive.
No samples were positive for all three tests together, and since convalescent (paired) samples were not available and the TBE/ flavivirus vaccination status of the patients is unknown, the interpretation of these results remains inconclusive. So far, six imported cases of human TBE imported from Scandinavia, Austria, Kyrgyzstan and Slovenia have been confirmed by the IPH.
Currently, the ITM (Antwerp) is hosting the TBEV-NRC. None of the Belgian medical samples submitted in between 2014-16 were positive in serology (n=40) or PCR (n=25), while occasional imported travel related cases (approximately 1 per year) continue to be diagnosed. This is more or less the expected number, considering that ECDC and other data sources reported a total of only 38 travel-related cases for the whole EU for 2012.
Veterinary surveys in Belgian dogs, cattle and wild boar
In the three studies by Roelandt and others [62-64], a commercially available enzyme-linked immunosorbent assay (Immunozym FSME/TBE IgG All Species-ELISA®, Progen Biotechnik GmbH, Heidelberg, Germany) was used for first-line detection of TBEV-specific IgG-antibodies. This non-competitive indirect assay uses horseradish peroxidase–Protein G conjugate to detect IgG against whole TBE-virus. Using standard curves, sample concentrations were read in Vienna Units per ml (VIEU/ ml). Sera with <53 VIEU/ml were negative, sera with >126 VIEU/ ml were positive and those between 53 VIEU/ml and 126 VIEU/ ml were classified borderline (Table 2).
| Sentinel Animals | Dogs Belgium |
Cattle Belgium |
Wild boar Flanders |
Roe Deer Wallonia |
Roe Deer Flanders |
|---|---|---|---|---|---|
| Year Sampled | 2008 | 2010 | 2013 | 2007-2009 | 2007-2013 |
| Sampling | Laboratories 2 FL+1 W |
Winterscreening Cross-sectional | FL range: LIM+ANT-WFL Disease Surveillance | W range: Surveillance Network | FL range: Volunteer Network |
| Strategy | Convenience (Catchment) |
Risk ~ Lyme/TBEV 4 Provinces East BE | Convenience (Hunters–Vets) | Convenience (Hunters) | Convenience (Hunters) |
| Criteria Animals | None | ≥2 years old (pasture access) | Representative of population and range | Shot | Shot or found dead |
| Sample Size | n=880 dogs from 293 communities | n=650 cattle from 44 herds/communities | n=238 wild boar from 14 communities | n=498 from 28 forest districts |
n=98 from 7 hunting areas |
| Detection Limit 95% confidence | ≥0.35% | ≥0.55% | ≥1.25% | ≥0.60% | ≥3.00% |
Table 2: Summary of sampling strategies in Belgian veterinary sentinel strategies. Strategy, sample sizes, selection criteria and potential TBEVseroprevalence detection limits if TBEV is present.
The seroneutralisation test TBEV-SNT is the gold standard for TBEV diagnosis [65] and was always used following the “rapid fluorescent focus inhibition test” protocol: RFFIT in microtiter plates using Vienna units per ml (VIEU/ml) [57]. SNT test panels are necessary in order to distinguish the cross-reacting flaviviral antibodies (other SNT tests), so that one can estimate true TBEV-seroprevalence in each species and can evaluate veterinary ELISA screening accuracy. The latter can be performed with accepted gold standard evaluation techniques, including two-by-two table parameters and ROC-curves [66]. As much as possible, the relevant combinations of species serum+flavivirus exposure control samples (positive/negative) were used for each test [47].
In the Belgian canine study, serum samples of Belgian dogs were obtained from three diagnostic laboratories from Northern (n=688) and Southern Belgium (n=192). Since the true diagnostic sensitivity and specificity of the ELISA kit were unknown for dogs, we lowered the cut-off by 15% compared to the kit cut-off (>53 → >45 VIEU/ml). ELISA-positive (>126 VIEU/ml), borderline (>53 VIEU/ml) and near-borderline (>45 VIEU/ml) samples were subjected to TBEV-SNT. One dog was confirmed TBEV seropositive. Several ELISA-positive and (near)borderline sera underwent seroneutralisation and hemagglutinin inhibition tests to rule out West Nile and Louping Ill viruses, but tested negative. The clinical history of the seropositive dog could not explain beyond doubt where and when TBEV infection was acquired [62].
In the Belgian cattle study a targeted, risk-based subselection (age >2 years, pasture access, Eastern provinces) of a cross-sectional sampling design was used to perform serological screening on Belgian cattle (n=650), selected from the 2010 Belgian national cattle winterscreening surveillance serum bank. All samples were subjected to the gold standard TBEV Seroneutralisation Test (SNT). Seventeen bovines were seropositive (titer>1/15) and six had borderline results (1/10<titer<1/15). The accuracy of the SNT was confirmed in a mouse inoculation test. The overall bovine TBEV-seroprevalence in the targeted area was estimated between 2.61 and 4.29%. This confirms the presence of infected foci in Belgium for the first time. Further surveillance in cattle, other sentinels, ticks and humans at risk is recommended to further determine the location and size of endemic foci and the risk for public health [63].
In the Flemish wild boar study, TBEV serological screening was performed on sera from (Sus scrofa; n=238), within the frame of a Flemish wildlife surveillance. These sera were collected in 2013 throughout the whole Flemish wild boar population range (northern Belgium) by hunters and vets. All samples were subjected to gold standard TBEV seroneutralisation (SNT). Seven wild boars were seropositive and showed moderate to high SNT-titers-three had borderline results. Seroprevalence was estimated around 4.20% (95% CI: 1.65-6.75%). Other Flaviviridae (Classical Swine Fever, West Nile Fever, Louping Ill viruses) were ruled out and thirteen available tonsils tested negative in TBEV RT-PCR [47,64].
In Walloon roe deer study [67], 498 hunted roe deer (Capreolus capreolus) sera were collected in Wallonia (southern Belgium) between 2007 and 2009, through an active surveillance program [68]. The animals originated from 28 forest districts uniformly distributed in the four provinces of southern Belgium (no map available). The sera were tested using the Immunozym FSME TBE IgG All Species ELISA (Progen Biotechnik) and 62 sera (12.4%) were ELISA-positive. Five highly ELISA-reactive sera were analyzed further in SNT and two displayed a significant SNT-titretiter (1:20 and 1:160). The two SNT-positive roe deer were sampled in 2008 and 2009 and originated from two different forest districts. Larger-scale screenings are being carried out by the University of Liège to evaluate the potential TBE risk areas in this region [67].
In the Flemish roe deer study [69], hunted roe deer sera were collected in Flanders (northern Belgium) between 2008 and 2013. A total of n=98 samples were examined for specific TBEV IgG antibodies using RFFIT-SNT. An antibody prevalence of 4.90% was found (95% CI: 1.61-11.70%) and the two TBEV-seropositive samples presented with relatively low titers (1/16). These results resembled those of other European studies and would suggest potential presence of TBEV in Flemish roe deer. It was concluded that roe deer, being omnipresent and increasing in abundance, offer good possibilities for comparative European sero-surveillance of several ruminant and zoonotic, including TBEV [69].
Results and Discussion
Sampling strategies and detection limits
Tables 1 and 2 summarize and compare the sampling strategies and detection limits to be expected from the given sample size. Passive studies, such as the medical ones in this case, often lack the sensitivity to detect rare and emerging diseases [70]. Passive and convenience active sampling are per definition opportunistic and quite cost-effective, but the results are not always representative of larger general populations, due to potential selection bias [71]. Risk-based targeted sampling equally does not allow study results to be extrapolated to non/low-risk areas but gives the worst case scenario and increases probability to detect an emerging disease early, i.e. even at very low prevalence. On the other hand, a fully randomized national sampling for an emerging disease in a very low prevalence situation (such as Belgium) may be cost-prohibitive due to unrealistically high sample sizes that would be required.
As follows from general epidemiological theory and for any sampling strategy (even convenience), a larger the sample size will result in a lower the detection limit (Table 2) and a higher precision in the estimates (Table 3). As such, especially the current human passive surveillance (ITM: n=40) and Flemish roe deer sample (n=98) theoretically needed a relatively higher presence of >3-5% for emerging TBEV to be detectable in the respective Belgian populations. A 100% negative survey may indicate true absence or a hidden presence below the detection limit [72]. The detection limits were thus generally lower for the larger animal studies and in the face of a higher expected exposure lower on the iceberg: this is a win-win situation with more potential precision in the seroprevalence estimates.
| Species | Sample Size |
ELISA+ | SNTpos%+SNTNI% | Belgium Free of TBE ~SNT/ELISA? | Original Study, Year |
|---|---|---|---|---|---|
| Human | n=359 | IgG: 15.32% IgM: 5.29% | - | No, and Prev <10-15% (Pdisease: <0.0001) | QAMH, pers. comm., 2015 |
| Human | n=113 | IgG: 24.78% IgM: 0.88% | 8.12%+0.90% Prev: 9.02% (3.61-14.09%) | No, and Prev <8-35% (Pdisease: <0.0001) | IPH, pers. comm., 2015 |
| Human | n=40 | IgG: 0.00% IgM: 0.00% | 0.00%+0.00% Prev: 0.00% | Yes, or Prev <7% (Pdisease: 0.0547) | ITM, pers. comm., 2016 |
| Dog | n=880 | IgG: 1.13% | 0.11%+0.00% Prev: 0.11% (0.0-0.3%) | Yes, or Prev <0.55% (Pdisease: 0.0842) | Roelandt et al., 2011 |
| Roe Deer | n=498 | IgG: 12.4%° | 0.4%+0.00% Prev: 0.4% (0.00 -0.95%)* | Yes, or Prev <1.25-15% (Pdisease: 1.000) | Linden et al., 2012 |
| Cattle | n=650 | IgG: 3.85% | 2.61%+0.92% Prev: 3.45% (2.12-4.96%) | No, and Prev <3.5% (Pdisease <0.05) | Roelandt et al., 2014 |
| Roe Deer | n=98 | - | 5.1%+0.00% Prev: 5.1% (2.20-11.39%) | No, and Prev <7% (Pdisease: 1.000) | Tavernier et al., 2015 |
| Wild Boar | n=238 | IgG: 5.46% | 2.91% (2.56 8.31%) | No: Prev ≥2.5% (Pfree <0.001) | Roelandt et al., 2016 |
SNT: Sero Neutralisation Test (+: Positive result; +/-: Doubtful); ELISA: Enzyme-Linked Immunosorbent Assay; n: Sample Size; (values): Wald 95% Confidence Interval; Prev: Prevalence; *Underestimation as not all ELISA-positives were confirmed/tested in SNT [47]
Table 3: Available TBEV seroprevalence and freedom data in Belgium, anno 2016.
Prevalence and freedom estimates
Prevalence and freedom calculations were performed similarly for all Belgian studies and are summarized in Table 3. Confidence intervals (95% Wald if n>100 or Agresti-Coul if n<100) were calculated on the results and the probabilities of freedom (Prevalence=0.00%) were calculated in EpiTools (Survey Toolbox® AusVet1.04 and https://epitools.ausvet.com.au) [73] and WinEpiscope®2.0 [74], according to the Cameron and Baldock probability formulae [73,75], with a range of design prevalences (cattle: 0.1-50%; wild boar: 0.1-10%; dogs: 0.1-1%; humans: 0.1- 35%; Roe deer 0.1-15%) and with the conservative or progressive (SNT-borderline samples as negatives or positives) number of TBE-reactors when applicable. In all species, the observed number of positive reactors (IgG and/or SNT) was always too high to substantiate freedom of TBEV for the targeted population/ geographical area (p-values <0.05), at the diverse retrospective design prevalences.
At first sight, the studies seem to contradict each other (TBEV Freedom: yes/no?). However, those that seem to indicate “Freedom” (Yes) seem to suffer from a low sample size and high detection limit (ITM), or from incomplete/no verification of test results with SNT. These studies are not able to distinguish between a truly free population and a population with prevalence below the detection limit. On the other hand, the IPH human study cannot be considered a real “No freedom” either, as the SNT and ELISA results was always conflicting in individual patients and relevant patient history was incomplete.
Veterinary ELISA evaluation against gold standard SNT
In Dogs, several false positive samples were observed in ELISA (~1%). It was also clear that the canine cut-off of this ELISA kit needs further evaluation, especially to improve sensitivity and to avoid false negatives, since the SNT-positive sample was only borderline in ELISA, where we used a lower cut-off of 45 VIEU/ml (Table 4) [47].
| Diagnostic Test Accuracy of the Progen All-species IgG-ELISA | ||||
|---|---|---|---|---|
| Species Total Sample | SNT DIL50 Threshold | ELISA Parameter | Results | Sample Size Used for Calculation |
| Humans (n=113) |
≥1/15 | DSe | 0.90 (0.55-1.00) | n=10 |
| DSp | 0.82 (0.74-0.89) | n=101 | ||
| Dogs n=880 |
≥1/5 | DSe | 1.00 (2.50-1.00) | n=1 |
| DSp | 0.99 (0.98–1.00) | n=879 | ||
| Cattle (n=650) |
- | DSe | Min: 0.13 (0.00-0.27) Max: 0.17 (0.00-0.21) |
n=18-23 |
| Min: ≥1/15 Max: ≥1/10 |
DSp | Min: 0.89 (0.87-0.92) Max: 0.97 (0.96-0.98) |
n=627 | |
| - | AUC ROC | Min: 0.5489 (0.51-0.59) Max: 0.5535 (0.51-0.59) |
n=650 | |
| Wild Boar (n=238) |
- | DSe | Min: 0.40 (0.12-0.74) Max: 0.57 (0.18-0.90) |
n=7-10 |
| Min: ≥1/15 Max: ≥1/10 |
DSp | Min: 0.91 (0.86-0.94) Max: 0.92 (0.88-0.95) |
n=228 | |
| - | AUC ROC | Min: 0.60 (0.33-0.87) Max: 0.69 (0.37–1.00) |
n=238 | |
Table 4: Diagnostic Test Accuracy of the Progen All-species IgG-ELISA. Adapted from (Roelandt, 2016) ELISA accuracy parameters as compared to TBEV Seroneutralisation Test (SNT) as gold standard test. DIL50: 50% endpoint titer cut-off: Titer causing 50% reduction in fluorescent foci [78]. DSe/ DSp: Relative diagnostic sensitivity or specificity; AUC ROC: Area under the receiver operating curve; Min: With borderline SNT as true positives; Max: With borderline SNT as true negatives.
In Cattle, the IgG protocol of the Progen ELISA® seemed to have an extremely low relative sensitivity DSe in cattle (DSe<20%), combined with a fairly reasonable relative specificity (DSp ≥90%), both compared to SNT at sensitive (1/10 DIL50) or specific (1/15 DIL50) serial dilution thresholds. The precision, predictive values, Cohen’s kappa and Youden index also followed similar trends, indicating an overall low capacity of this test/protocol to distinguish and correctly classify TBEV seropositive and negative cattle. When inspecting the cattle ROC-curves (area under the curve: AUC=54-55%), it was felt that no great improvement could be made to this particular protocol by changing the cut-off in this species. A traditionally calculated cut-off based on the negative sample population (c=μneg+2*SDneg with μ=mean and SD=standard deviation) would still have led to a large amount of miss-classification [47].
In Wild Boar, using the manufacturer’s cut-offs and an alternately positive or negative interpretation of SNT-borderline results, the IgG protocol of this ELISA showed low diagnostic sensitivity and good diagnostic specificity: DSe min-max: 40-57% and DSp min-max: 91-92%, with when SNT-borderlines were assumed to be true positives (min) or true negatives (max) respectively. ELISA agreement (kappa) with the SNT was judged only “slight to fair” (0.18-0.22). Currently, the ELISA overall discriminatory ability (area under the curve=AUC) was only 59% or 69% in wild boar at 1/15 or 1/10 SNT thresholds respectively. Additionally, receiver operating curve (ROC)-analysis showed that for early detection screening purposes with SNT follow-up, the ELISA cut-off might be placed as low as 35 Vienna-units: this would result in improved DSe (70-71%) at the cost of DSp (64.04-69.74%) [47].
In humans, the IgG All Species-ELISA® kit can theoretically be used for TBEV testing in all species, including humans. In humans, this ELISA has a reported diagnostic sensitivity of 97% and analytical specificity of 99% for IgG [76]. Considering the SNT as a gold standard, IgG was not as accurate as predicted by the firm, with a DSe of around 90% and a DSp of around 82%.
In all datasets, we should bear in mind that due to the relatively small “positive” sample sizes available, the ELISA DSe estimates are not very precise and may not even be completely accurate, by chance. Whereas in animals the (sometimes extremely) low DSe seemed to be the major problem, in humans DSp was relatively lower, indicating relatively more false positives in the IgG All Species ELISA. The flaviviral cross-reactions interfering with ELISA-DSp are well known from the literature, are also present in haemagglutination inhibition testing (HIT), and can be resolved by confirmation testing with batteries of SNT and IFAT-tests. The causes for the unsatisfactory veterinary DSe results [47], on the other hand, are largely unknown as this problem has not been described yet.
What is clear for TBEV is that veterinary ELISA’s have not been validated in large published European field studies or proficiency tests except the study from Reed and Muench [77]. Manufacturer’s studies remain unpublished and do not seem to have included sufficient numbers of (low/high) seropositive/ negative control samples from low prevalence areas, such as the Low Countries. As a result, the kit-protocols may actually not be fit for this new particular screening purpose/area (Table 4) [78].
Alternatively, there may be E-protein mutations present changing the antigenicity of the local Belgian TBE-virus, which has not been found, characterized yet. The hosts (animals) may also be the cause, through short antibody longevity (months rather than years?) or through bad serum quality, or they may undergo a very/too low TBEV-exposure from a (very) low tick-prevalence environment [47].
Confirmation testing and validation
In the human-based studies, flaviviral confirmation testing was not performed, despite the fact that–considering Spatio-temporal tick exposure, travel and vaccination history-cross-reactions are possible between Tick-Borne Encephalitis Virus (TBEV)/West Nile Virus (WNV)/Japanese Encephalitis Virus (JEV)/Yellow Fever Virus (YFV)/Dengue Viruses (DENV1-4) and very few false positives are to be expected in TBEV-SNT [61,79-81]. This is currently a major gap in the medical diagnosis of aseptic meningitis, for which up to 75% of cases remain etiologically undiagnosed, even in 2016 [51,82-85].
The veterinary studies on dogs, cattle and wild boar documented some of the very common flaviviral cross-reactions in first/second line testing. One of the dogs reacted more strongly to Louping Ill virus haemagglutination inhibition testing (LIV-HIT) than to TBEV-SNT, and some of the wild boar showed a relatively lower reaction in LIV-HIT and/or high reaction in Usutu Virus (USUV) and West Nile Virus (WNV)-SNT (Table 5). In flaviviral research, cross-reactions in ELISA kits are so common that we might hypothesize that almost “any” veterinary flaviviral ELISA kit could potentially be used as a screening test for TBEV-exposure, e.g. a WNV kit in horses 21. In the veterinary studies on roe deer, cross-reactions were not ruled out [67], or no comparison was performed [69].
| Sentinel Animals |
Dogs Belgium |
Cattle Belgium |
Wild boar Flanders |
|---|---|---|---|
| Confirmation Panel |
10/10 reactors from TBEV-ELISA (>53/126 VIEU/ml)+5 negatives |
23/23 reactors from TBEV-SNT (1/11-1/30)+10 negatives | 7/10 reactors from TBEV-SNT (1/11-1/243)+3 negatives |
| Confirmation Tests/Results |
TBEV-SNT: 1 pos (1/5) LIV-HIT: 1 pos (1/160) WNV-SNT: All negative |
Rabies-SNT: All neg. WNV-ELISA/-SNT: All negative (1 NI) Mice are protected |
SNT: USUV-WNV-CSFV+ELISA: CSFV/HIT: LIV+IFA:YF-DEN-JE-WN-TBE: Most negative or lower titers+IFA confirmed TBEV-SNT++ +1 strong reaction USUV/WNV |
Table 5: Flaviviral confirmation testing in 3 of the veterinary studies. As compared to TBEV-SNT as gold standard. DSe/DSp: Diagnostic Sensitivity or Specificity; Min: With borderline SNT as true positives; Max: With borderline SNT as true negatives.
Despite being an absolute necessity for robust results, SNT-confirmation testing against other possibly cross-reacting flaviviruses is not always straightforward. The selected SNT for a combination of species and flavivirus is not always readily available in Belgium/Europe (e.g. LIV/USUV) or not validated for the species under study so that quality of the assays could not be guaranteed (e.g. WNV in wild boar). For the confirmation testing we preferably selected genetically related (LIV) and geographically relevant viruses (USUV, WNV, LIV).
However, our sample panels came from non-target species for each respective test, e.g. wild boar, dog and cattle versus birds, horses, or small ruminants. Hence, control sera of the correct species-flavivirus combinations were often not available. Moreover, the SNT is a delicate test and poor quality samples necessitated kaolin sample treatments for the wild boar and cattle sera besides the usual pre-heating and treatment of stable cell cultures with antibiotics.
Occasionally, we had to opt for “second choice” confirmation tests such as ELISA, HIT or IFAT [47]. Nonetheless, despite the potential cross-reactions, in medical diagnosis HIT and IFA are generally known as reasonably sensitive tests [86], that may also be specific in skilled hands through repetition and titer comparisons [87], and that may agree well with SNT [61].
In the wild boar study, we had the opportunity to test the Euroimmun flaviviral IFAT-biochips (www.euroimmun.ch) for medical differential diagnostics (TBEV/WNV/JEV/YFV/DENV1- 4 [61], after recalibration with specific primary/secondary conjugates and with porcine TBEV control samples obtained from the Friedrich Loeffler Institute (FLI). This IFAT confirmed only the three strongly SNT-positive/ELISA-positive wild boar and thus currently seems to be a less sensitive test than TBEV-SNT in wild boar [47].
General Discussion
Experiences with sentinel species surveys
The Belgian medical community so far has delivered almost no evidence for TBEV-presence or TBE-cases in Belgium throughout the last 16 years, despite a considerable amount of positive (but contradicting) serology test results, and despite the correct diagnosis of several imported cases with accredited tests following best laboratory practices. So, unless passive medical surveillance is more enhanced in neurological referral centers through creating awareness in the medical community and with projects, and unless active surveillance is added in occupationally at risk groups (e.g. military, foresters), humans remain bad sentinels at the very tip of the iceberg. Medical data is certainly not sufficient to evaluate whole areas and regions for endemicity and case reporting is considered unreliable and incomplete (only the tip of the iceberg) at the best of times 4 [8,37,38,45,52].
As opposed to this, all five Belgian veterinary studies have been able to suspect (dogs) or indirectly confirm (cattle, wild boar, roe deer) TBE-viral presence in Belgium. However, which is the best species to continue Belgian TBEV sentinel surveillance? The “ideal” Sentinel species for TBEV sentinel surveillance has been described as having an adequately limited home range in comparison to TBE focus size, which is often a few m2 up to 1 km2. It should be available in large numbers; it should be well dispersed in the surveillance area, and should show a long-lasting detectable response after natural infection [88-90]. Additionally and importantly, one may add that TBEV (sero) prevalence should show a good spatial correlation with human TBE incidence/risk, and that sufficiently frequent tick exposure/infestation is clearly advantageous [46].
Considering the results of the Belgian surveys, a number of additional practical and epidemiological surveillance suitability criteria may equally be taken into account to set up effective sentinel surveillance (Table 6). Some of these issues may severely limit certain aspects of the study/surveillance, such as the accuracy and confirmation testing (blood volume/quality, test availability), statistical power, detection limit, precision of freedom/prevalence calculations (sample size) and the potential to proceed to modelling/mapping exercises by obtaining sufficient “case” data: e.g. numbers of tick bites, sentinel TBEVseropositive, TBE cases or TBEV infected ticks [47].
| Suitability Criteria for TBEV Sentinel Surveillance | |
|---|---|
| Clinical Characteristics | •Clinical cases, viraemia and/or lasting antibody response •No flaviviral vaccination or exposure to other flaviviruses than TBEV •Tick exposure, good tick host and lack of preventive actions |
| Correlation with Spatial Human Risk | •Useful proxy for human risk behaviour, mobility and travel •Spatial presence at national (NUTS 1), regional (NUTS 2), or local (NUTS 3/4) level •Suitable home range (km²) and representative-even distribution in the area |
| Epidemiological Parameters | •Knowledge of population size, density and sampling frame •Pre-existing surveillance for other pathogens: passive, active or targeted •Sample size sufficient for the surveillance purpose and design prevalence |
| Practical Parameters | •Organizations/Governments involved and available funding •Serum quality, volume and transport, storage •Available flaviviral diagnostic tests and control samples per spp.-virus combination |
Table 6: Table of suitability criteria for TBEV sentinel surveillance. Compiled from Belgian experiences [47] and literature [46,88-90].
After evaluation of these surveillance suitability criteria for the veterinary sentinels used in Belgium (Appendix B: Veterinary Sentinel Evaluation Tables), it seemed to us that [47]:
1. Dogs are most suited for passive clinical surveillance or local risk-based sero-surveillance at community scale.
2. Cattle are most suited for national randomized serosurveillance at regional/national scale and for studying localized foodborne TBE point outbreaks.
3. Wild boar is most suited for local risk-based targeted serosurveillance at community scale within their range of presence (Wallonia and parts of Flanders: locally representative).
4. Roe deer are suited for both national randomized serosurveillance (range and density is sufficient throughout Belgium UTM squares) as well as for local risk-based targeted sero-surveillance at community scale.
5. None of these hosts are particularly suited for finding the actual virus: for this purpose, rodents and ticks are better study subjects.
6. For mapping and modelling exercises, wild boar, roe deer and cattle seem to be the most promising sentinels to provide enough case data in Belgium. This purpose can potentially be extended to all large tick amplifier mammals.
In the end, we did not identify one single best sentinel species, and concluded that the choice of species depends strongly on the purpose of the survey (e.g. broad screening versus in depth investigations, medical risk, and spatial area description) and on the local epidemiological situation: which hosts are present at which stage of the iceberg? The authors also believe that the local eco-epidemiological situation explains most of the current contradictions in “best sentinel discussions” (e.g. wild boar vs. roe deer) and in the available European risk factor/predictive modelling studies. Many more species have been used on occasion to study TBEV presence or seropositivity (Appendix A: Overview Sentinel Studies) and horses (clinical or active), small ruminants (sheep–goats: National, local or foodborne studies), and other wildlife species such as foxes (e.g. urban settings or Northern Europe) may be better sentinels instead of dogs, cattle and boar/deer under some circumstances.
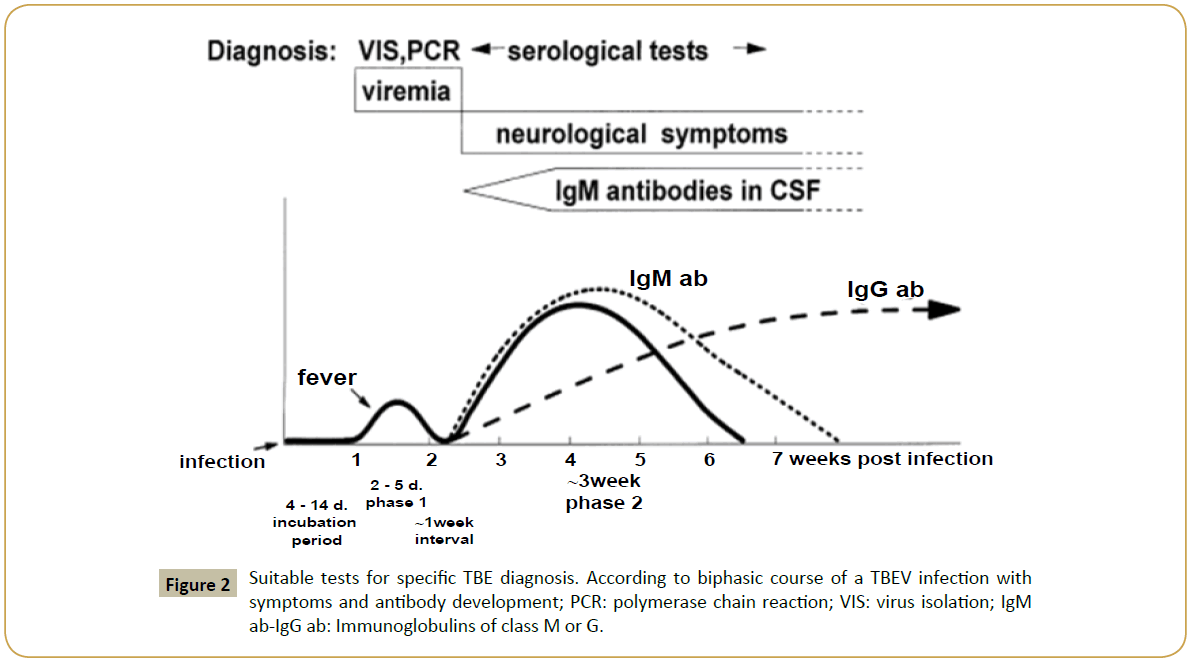
Experiences with diagnostic tests
Despite good international proficiency test results for SNT in the medical setting, it remains an annoying finding that interpretation of IgM/IgG and gold standard SNT serology [65] did so far never provide a conclusive TBE-diagnosis, as it should have based on the data. The contradictions between the IgG-ELISA, HIT and SNT should not even occur more generally [59,76]. Additionally, a final diagnosis should not only be dependent on IgM positivity, as IgM detects only acute infections (Figure 2), i.e., up to 7 weeks or at the most a few months [65] and IgM-seroconversion may not even develop in some patients [59].
Figure 2: Suitable tests for specific TBE diagnosis. According to biphasic course of a TBEV infection with symptoms and antibody development; PCR: polymerase chain reaction; VIS: virus isolation; IgM ab-IgG ab: Immunoglobulins of class M or G.
Paired sera that demonstrate a 4-fold increase in IgG ELISA titers, the use of very specific TBEV-SNT (considered ±100%), and a complete travel, tick-bite, vaccination history should be sufficient to solve these interpretation problems in future medical studies. Additional SNT or IFA testing should rule out other flaviviruses if one is still not convinced.
With the veterinary ELISA accuracy results obtained so far, it seems ill advised to start using any ELISA as a veterinary screening test in a low prevalence area at the fringe of the TBEV geographic distribution, at least not before some further international validation of these tests in multiple species. In general, it is known that measures of accuracy are not fixed indicators of a test performance [66,91] and that test accuracy in the field may be influenced by many factors, including population characteristics, genetic variation in the infectious agent, the sampling, storage and test methodologies and the population prevalence [92,93].
The main reason for this is that Belgium and other low prevalence countries first have to be able to accurately map their endemic risk areas, as opposed to just estimating a true prevalence from an apparent ELISA-prevalence to follow relative trends. For this risk assessment purpose, an unknown proportion of ELISA-false negatives and low sensitivity may constitute a major problem. Clearly, this has never been an issue in the core areas of TBE (V) endemicity where the ELISA-tests were developed, as there the seroprevalence is usually quite high in one or more species and clinical cases are much more common in these areas.
Presently, the IFA and SNT are currently the most accurate veterinary serological tests for the Belgian situation, both for surveillance or diagnostic settings. Even when testing all sera with SNT/IFA tests is not sustainable in veterinary field screening, it should currently be best practice to test all ELISA-positives and -doubtful in SNT/IFA, together with a randomly selected sufficient sample of the ELISA-negatives. In the meantime, research projects should focus on continued (re-) validation and improvement of current ELISA’s e.g. sub-viral particle ELISA [94,95] and should (re-)study matrix and species effects on analytical/diagnostic sensitivity/specificity, sample preparation/storage protocols, etc. The goal would be to obtain a more accurate and better characterized screening tool applicable to low prevalence areas for surveillance, risk assessment and trend watching purposes.
Advice on future Belgian One Health TBE(V) surveillance
Medical surveillance: Belgium has always simply been “assumed” to be TBEV-free, though this was based on very little scientific evidence [53]. In 2016, despite five veterinary sentinel publications between 2010-2016, and despite multiple unexplained/inconclusive seropositive human cases, the medical world still considers TBEV as a non-endemic virus and of little importance to Belgium [96].
However, despite improvements in the diagnosis of viral encephalitis since the use of PCR on CSF to try and detect the more common viruses [83,97,98], the etiology of up to 75% of aseptic/viral encephalitis and meningitis cases remains unknown around the world, even in 2016 [51,82-85].
Moreover, TBEV does not feature in the regular diagnostic panel for locally acquired medical encephalitis unless there are very clear anamnestic indications [83,98,99] and medical surveillance has been very passive and limited. The professional awareness in regards with prevention of travel related TBE cases is only beginning to rise now. For the clinician, it is important to try to establish an etiologic diagnosis in all cases of encephalitis/ meningitis, even if there are no specific effective treatments, since this may be important for the individual prognosis and counseling of patients and family members [100].
The Belgian veterinary sentinel studies [62-64,67,69] the Dutch ones [72,101] and the recent discovery of a new TBE-virus in the Netherlands on tick samples from September 2015 [101,102] as well as the very first Dutch human TBE case [103] should now prompt Belgian scientists and clinicians to reconsider this situation. Clearly, enhanced medical surveillance and increased awareness among medical professionals are now absolute priorities for the Low Countries, necessary to minimize and assess any potential TBE risk to humans from this uncharacterized strain of TBEV and to guide prophylaxis and public health decisions and measures.
Additionally, medical surveillance may lead to explanations for the apparent mismatch between the veterinary findings and the lack of medical cases. Potential hypotheses to be explored may include: suboptimal diagnostic test quality, timing of (paired) sampling, insufficient testing by clinicians, lack of awareness, a large proportion of asymptomatic or clinically mild exposures, and presence of an atypical low-virulent TBEV virus.
TBE should be made notifiable, as in other European member states [8,52,59]. Next to a more enhanced passive component, it should include an active component to increase the detection sensitivity of the overall surveillance system [70,104] and to improve usefulness, value and cost-effectiveness of the data [105]. As suggested for veterinary surveillance, existing medical surveillance schemes and available tick, sera and risk factor datasets should be exploited.
Virological surveillance
Due to a low detection probability and the considerable resources needed to collect sufficient ticks/samples to obtain confident PCR results, scientists are often not activated to conduct such surveillance activities in low prevalence TBE areas [106]. TBEV does not often cause epidemics, though occasionally one may be confronted with a food-borne outbreak with a few dozen cases [107,108]. This flavivirus remains mostly submerged in the bulk of the iceberg. These sylvatic tick-host cycles are within largely unaffected populations of diverse animal species, where TBEV causes only short viremias and a vast majority of asymptomatic infections.
This makes it very difficult to “catch the virus in action” and the international scientific community still rarely succeeds in isolating TBEV-strains from known human/veterinary cases, or from hosts even in known highly endemic areas. Well characterized and fully sequenced TBEV isolates are scarce throughout the entire Eurasian endemic zone [109-111]. Some of the characterized TBEV strains were isolated from ticks or rodents, and rarely from a human case [4,112-115].
However, the TBE RNA-virus is capable of evolution, mutation and recombination when passaged in the lab through different hosts [110,116,117], in the field throughout the Eurasian continent [118,119], and certainly at the biogeographic edges of its distribution, where it is subjected to a number of ecological constraints [120,121]. In Europe, the closely related Louping Ill Virus (LIV), Spanish Sheep Encephalitis Virus (SSEV), Greek Goat Encephalitis (GGEV) virus and Turkish Sheep Encephalitis Virus (TSEV) [122,123] and the in 2015 characterized Spanish Goat Encephalitis Virus (SGEV) virus are present [124].
Very recently (June 2016), a Dutch-Belgian research team successfully detected TBEV-viral RNA from an unknown TBEV strain [101,102]. This was in two ticks collected in Autumn 2015, obtained in a forested area where six roe deer sera from 2010 were found seropositive. The Dutch isolates were found to cluster within the TBEV-species complex, but not within the three established TBEV subtypes (W-S-FE) nor within the LIV-cluster, implying that it concerns a novel TBEV-subtype [101].
So far, the TBE-virus has not been PCR-amplified or isolated yet in Belgium. The study on 13 wild boar tonsils (all negative) was the first published attempt [64]. Secondly, during 2014-2015, the WIV-ISP has executed a field study in rodents in some of the communities where the Belgian TBEV-seropositive cattle were found earlier [63]. Nonetheless, so far the Belgian rodents have been SNT-negative (n=0/173) and PCR-negative (n=0/308). This could be due to a number of factors, such as large rodent turnover, so they remain only seropositive for a short time, low TBEV tick-prevalence and non-viraemic transmission, or just bad luck with the location of the sites, as TBE endemic foci can be quite small. The sentinel, reservoir and tick research should continue at least until a Belgian TBEV-strain is characterized, as this strain may very well be an atypical “Low Countries” strain, as found in the Netherlands.
Bringing it together: One health epidemiology
In a globalized world with increasing numbers of emerging diseases, an interdisciplinary so-called ”one health” approach is indispensable for the prevention and control of vector-borne zoonoses, such as TBE [125]. This approach leads to better preparedness and contingency planning, more effective surveillance and targeted control systems, increased health equity and improved sharing of logistics and costs [126-128].
The presently available veterinary Belgian scientific studies have allowed us to conclude that TBEV is indeed present in Belgium, despite an apparent lack of medical TBE cases and despite previous predictions against emergence. These five humble sentinel studies (often conducted with very limited resources) have at long last made Belgium join the “peloton” of TBE-endemic European countries trying to make sense out of (emerging) TBE(V) eco-epidemiology. The additional (and exciting) Dutch revelations, including the first virus and case detections in 2015- 2016 [101-103,129] make us even more confident that the investigations are moving in the right direction.
The (lack of) medical data leaves us somewhat puzzled for now… However, an immediate increase in medical awareness and sustained virological research are now justified for the Low Countries (e.g. Belgium-Netherlands-Luxemburg). This research will be needed to proceed confidently into the “endemic era” by:
1. Catching and characterizing the Belgian TBEV-strain: is it the “Low Countries” strain of the Netherlands or yet something else?
2. Diagnosing and describing the nature of the first Belgian human TBE cases: have they just been missed by the medics up till now, or are they mostly benign and asymptomatic?
3. Supplying necessary data for the competent governments to perform individual and public health risk assessments: is the risk low-medium-high and is there a difference between the general population and professionally at risk groups?
4. Supply sufficient case data to allow statistical risk prediction modeling [130,131] and spatial mapping: where is TBEV (risk) emerging and what are the driving risk factors in the Low Countries?
Spatial mapping and predictive modeling are risk-based methods that have been used particularly in vector-borne diseases to identify the areas and time periods in which surveillance is more likely to successfully detect emerging health threats at an early stage. Such techniques greatly benefit governments and public health agencies to target resources, research and control measures; have been performed in many other endemic countries or multiple country meta-analysis exercises [132-193].
Conclusion
This comparative review paper described five Belgian veterinary serological studies (ELISA/SNT/IFAT/HIT) in which several surveillance schemes were used (active/passive, risk-/ laboratory-/range-based) in classic TBE sentinel species (dogs, cattle, roe deer, wild boar). Additionally, passive syndromic surveillance in two medical laboratories resulted in inconclusive medical data. Details were given on the scientists’ experiences with available first/second line diagnostic tests and with the different surveillance methods/survey designs.
Each of the veterinary studies clearly demonstrated the presence of TBEV-specific antibodies in Belgian sentinels, sometimes even at high SNT titers, while the medical data remain so far inconclusive, despite positive reactions of some patients in some TBEV-tests. These results have substantiated our suspicion of TBEV-presence in Belgium from 2010 onwards and have allowed sentinel comparisons based on “suitability criteria”. Furthermore, the studies have highlighted the need for further veterinary validation of commercial ELISA-tests in comparison to the gold standard SNT.
We have been able to suggest an integrated future TBEV one health surveillance program for Belgium, combining several components at different levels of the TBEV zoonotic iceberg. This should lead to sufficient data collection for predictive modelling and spatial risk mapping in future studies.
References
- Herpe B, Schuffenecker I, Pillot J, Malvy D, Clouzeau B et al. (2007) Tickborne encephalitis, southwestern France. Emerg Infect Dis 13: 1114-1116.
- Ramelow C, Suss J, Berndt D, Roggendorf M, Schreier E (1993) Detection of tick-borne encephalitis virus RNA in ticks (Ixodes ricinus) by the polymerase chain reaction. J Virol Methods 45: 115-119.
- Mansfield KL, Johnson N, Phipps LP, Stephenson JR, Fooks AR, et al. (2009) Tick-borne encephalitis virus-a review of an emerging zoonosis. J Gen Virol 90: 1781-1794.
- Suss J (2011) Tick-borne encephalitis, epidemiology, risk areas, and virus strains in Europe and Asia-an overview. Ticks Tick Borne Dis 2: 2-15.
- Heinz FX (2008) Etiology, In: Compendium of Tick-borne Encephalitis (TBE, FSME). Monograph, Baxter, ISW-TBE pp: 5-14.
- Labuda M, Randolph SE (1999) Survival strategy of tick-borne encephalitis virus, cellular basis and environmental determinants. Zentralbl Bakteriol 289: 513-524.
- Biernat B, Karbowiak G, Werszko J, Stanczak J (2014) Prevalence of tick-borne encephalitis virus (TBEV) RNA in Dermacentor reticulatus ticks from natural and urban environment, Poland. Exp Appl Acarol 64: 543-552.
- ECDC (2012) Epidemiological situation of tick-borne encephalitis in the European Union and European Free Trade Association countries. European Centre for Disease Prevention and Control, Stockholm pp: 1-54.
- Suss J, Klaus C, Gerstengarbe FW, Werner PC (2008) What makes ticks tick? Climate change, ticks, and tick-borne diseases. J Travel Med 15: 39-45.
- Suss J (2008) Epidemiology, Compendium of Tick-borne encephalitis (TBE, FSME). Monograph pp: 15-20.
- Jaaskelainen AE, Tikkakoski T, Uzcategui NY, Alekseev AN, Vaheri A, et al. (2006) Siberian subtype tickborne encephalitis virus, Finland. Emerg Infect Dis 12: 1568-1571.
- Csango PA, Blakstad E, Kirtz GC, Pedersen JE, Czettel B (2004) Tick-borne encephalitis in southern Norway. Emerg Infect Dis 10: 533-534.
- Skarpaas T, Sundoy A, Bruu AL, Vene S, Pedersen J (2002) Tick-borne encephalitis in Norway. Tidsskr Nor Laegeforen 122: 30-32.
- Skarpaas T, Ljostad U, Sundoy A (2004) First human cases of tickborne encephalitis, Norway. Emerg Infect Dis 10: 2241-2243.
- Skarpaas T, Golovljova I, Vene S, Ljostad U, Sjursen H (2006) Tickborne encephalitis virus, Norway and Denmark. Emerg Infect Dis 12: 1136-1138.
- Skarphedinsson S, Jensen PM, Kristiansen K (2005) Survey of tickborne infections in Denmark, Emerg Infect Dis 11: 1055-1061.
- Gresikova M, Weidnerova K, Nosek J, Rajcani J (1972) Experimental pathogenicity of tick-borne encephalitis virus for dogs. Acta Virol 16: 336-340.
- Janitza-Futterer D (2003) Serological studies on the endemic situation of the infection with the TBE virus in a South-bathing horse and dog population. Dissertation pp: 171.
- Klimes J, Juricova Z, Literak I, Schanilec P, Trachta e Silva, et al. (2001) Prevalence of antibodies to tickborne encephalitis and West Nile flaviviruses and the clinical signs of tickborne encephalitis in dogs in the Czech Republic. E Vet Rec 148: 17-20.
- Leschnik MW, Kirtz GC, Thalhammer JG (2002) Tick-borne encephalitis (TBE) in dogs. Int J Med Microbiol 33: 66-69.
- Rushton JO, Lecollinet S, Hubalek Z, Svobodova P, Lussy H, et al. (2013) Tick-borne encephalitis virus in horses, Austria, 2011. Emerg Infect Dis 19: 635-637.
- Labuda M, Nuttall PA, Kozuch O, Eleckova E, Williams T, et al. (1993) Non-viraemic transmission of tick-borne encephalitis virus: a mechanism for arbovirus survival in nature. Experientia 49: 802-805.
- Rizzoli A, Rosa R, Mantelli B, Pecchioli E, Hauffe H, et al. (2004) Ixodes ricinus, transmitted diseases and reservoirs. Parassitologia 46: 119-122.
- Suss J (2003) Epidemiology and ecology of TBE relevant to the production of effective vaccines. Vaccine 1: S19-S35.
- Bjoersdorff A (2009) Borreliosis and tick-borne encephalitis. Proceedings of the International Conference: Climate change impact on ticks and tick-borne diseases 2002. Brussels, Belgium.
- Beugnet F, Marie JL (2009) Emerging arthropod-borne diseases of companion animals in Europe. Vet Parasitol 163: 298-305.
- Pfeffer M, Dobler G (2013) Chapter 6: Tick-borne encephalitis. Guide to vector borne diseases of pets. Merial, Lyon, France pp: 365-379.
- Dietz O, Huskamp B (2005) Infectious diseases of the central nervous system: Early meningoencephalitis (FSME). Handbuch Pferdepraxis, Georg Thieme Publisher, Germany pp: 677.
- Pfeffer M, Dobler G (2011) Tick-borne encephalitis virus in dogs–is this an issue? Parasit Vectors 4: 59.
- Kirtz G (1999) FSME- Infection in an Austrian dog population. Diss Med Vet Univ Wien 151-160.
- Muller K, Konig M, Thiel HJ (2006) Tick-borne encephalitis (TBE) with special emphasis on infection in horses. Dtsch Tierarztl Wochenschr 113: 147-151.
- Chomel B (2013) Chapter 8: Synthesis and zoonotic aspects. In: Beugnet F (Ed) Guide to vector borne diseases of pets Merial, Lyon, France pp: 399-416.
- Higgins AJ, Snyder JR (2006) Chapter 1: Infectious diseases-Lyme disease (Borreliosis). In: The equine manual, Elsevier Saunders pp: 88-89.
- Leschnik M, Feiler A, Duscher GG, Joachim A (2013) Effect of owner-controlled acaricidal treatment on tick infestation and immune response to tick-borne pathogens in naturally infested dogs from Eastern Austria. Parasit Vectors 6: 1756-3305.
- Rees CA (2010) Chapter 13: Disorders of the skin-Ticks. In: Reed SM, Bayly WM, Sellon DC (eds.) Equine Internal Medicine (3rd edn.), Saunders Elsevier, St Louis, USA pp: 682-729.
- Jongejan F, Uilenberg G (2013) Chapter 2.1 Panorama of vector borne diseases of pets in Europe Guide to vector borne diseases of pets Merial, Lyon, France p: 425.
- Randolph SE, Sumilo D (2007) Tick-borne encephalitis in Europe: dynamics of changing risk. In: Takken W and Knols BGJ (Editors), Emerging pests and vector-borne diseases in Europe, Wageningen Academic Publishers, The Netherlands p: 501.
- Drelich A, Andreassen A, Vainio K, Kruszynski P, Wasik TJ (2014) Prevalence of tick-borne encephalitis virus in a highly urbanized and low risk area in Southern Poland. Ticks Tick Borne Dis 5: 663-667.
- Bormane A, Lucenko I, Duks A, Mavtchoutko V, Ranka R et al. (2004) Vectors of tick-borne diseases and epidemiological situation in Latvia in 1993-2002. Int J Med Microbiol 37: 36-47.
- Brinkley C, Nolskog P, Golovljova I, Lundkvist A, Bergstrom T (2008) Tick-borneencephalitis virus natural foci emerge in western Sweden. Int J Med Microbiol 298: 73-80.
- Makowka A, Gut W, Rogalska J, Michalik J, Wodecka B (2009) Detection of TBEV RNA in ticks as a tool for valuation of endemic area wide and sensitivity of TBE surveillance. Przegl Epidemiol 63: 375-378.
- Suss J, Klaus C, Diller R, Schrader C, Wohanka N et al. (2006) TBE incidence versus virus prevalence and increased prevalence of the TBE virus in Ixodes ricinus removed from humans. Int J Med Microbiol 40: 63-68.
- Takashima I (1998) Epidemiology of tick-borne encephalitis in Japan. Comp Immunol Microbiol Infect Dis 21: 81-90.
- Broker M (2002) Tick-borne encephalitis virus within and outside Japan: a cause for concern. Japaneese J Infect Dis 55: 55-56.
- Suss J (2008) Tick-borne encephalitis in Europe and beyond–the epidemiological situation as of 2007. Euro Surveill 13: 18916.
- Imhoff M, Hagedorn P, Schulze Y, Hellenbrand W, Pfeffer M, et al. (2015) Review: Sentinels of tick-borne encephalitis risk. Ticks Tick Borne Dis 6: 592-600.
- Roelandt S (2016) Questing for tick-borne encephalitis virus in Belgium using veterinary sentinel surveys and risk factor mapping. Doctoral Thesis Merelbeke, Ghent University, Faculty of Veterinary Medicine, Belgium.
- UK Ticks (2015) Tick activity project. University of Liverpool Institute of Infection and Global health, Liverpool, UK.
- Roelandt S, Heyman P, Tavernier P, Roels S (2010) Tick-borne encephalitis in Europe. Review of an emerging zoonosis. Flemish Vet J 79: 23-31.
- Donoso MO, Schadler R, Niedrig M (2008) A survey on cases of tick-borne encephalitis in European countries. Euro Surveill 13: 18848.
- Donoso MO, Vaheri A, Ambrose H, Koopmans M, de Ory F, et al. (2008) Analysis of the surveillance situation for viral encephalitis and meningitis in Europe. Euro Surveill 13: 8017.
- ECDC (2014) Tick-borne encephalitis. European Centre for Disease Prevention and Control. Annual epidemiological report 2014–emerging and vector-borne diseases. ECDC–2014, Stockholm pp: 20-23.
- Haglund M, Settergren B, Heinz FX, Gunther G (2003) Report of the Meningitis Program of the International Scientific Working Group on TBE: Serological screening of patients with viral CNS-infection of unknown etiology in search of undiagnosed TBE cases. Vaccine 1: S66-S72.
- EC (2012) Commission Implementing Decision of 8 August 2012 amending Decision 2002/253/EC laying down case definitions for reporting communicable diseases to the Community network under Decision No 2119/98/EC of the European Parliament and of the Council. J Eur Union 262: 34-35.
- Progen B (2012) Immunozym FSME IgM. Enzyme Immunoassay for the Determination of IgM-Antibodies against the TBE virus in Human Serum, Plasma and Cerebrospinal Fluid (CSF).
- Progen (2014) Immunozym FSME/TBE IgG All Species-ELISA. Data Sheet, Heidelberg, Germany.
- Vene S, Haglund M, Vapalahti O, Lundkvist A (1998) A rapid fluorescent focus inhibition test for detection of neutralizing antibodies to tick-borne encephalitis virus. J Virol Methods 73: 71-75.
- Holzmann H, Kundi M, Stiasny K, Clement J, McKenna P, et al. (1996) Correlation between ELISA, hemagglutination inhibition, and neutralization tests after vaccination against tick-borne encephalitis. J Med Virol 48: 102-107.
- Kollaritsch H, Krasilnikov V, Holzmann H, Karganova G, Barrett A, et al. (2011) WHO Background Document on Vaccines and Vaccination against Tick-borne Encephalitis (TBE).
- WHO (2011) Vaccines against tick-borne encephalitis: WHO position paper, Weekly epidemiological record. Weekly Epidemiological Record 24: 241-256.
- Litzba N, Zelena H, Kreil TR, Niklasson B, Kuhlmann-Rabens I, et al. (2014) Evaluation of different serological diagnostic methods for tick-borne encephalitis virus: enzyme-linked immunosorbent, immunofluorescence, and neutralization assay. Vector Borne Zoonotic Dis 14: 149-159.
- Roelandt S, Heyman P, De Filette M, Vene S, Van der Stede Y, et al. (2011) Tick-borne encephalitis virus seropositive dog detected in Belgium: screening of the canine population as sentinels for public health. Vector Borne Zoonotic Dis 11: 1371-1376.
- Roelandt S, Suin V, Riocreux F, Lamoral S, Van der Heyden S, et al. (2014) Autochthonous tick-borne encephalitis virus-seropositive cattle in belgium: a risk-based targeted serological survey, Vector Borne Zoonotic Dis 14: 640-647.
- Roelandt S, Suin V, Van der Stede Y, Lamoral S, Marche S, et al. (2016) First TBEV serology screening of Flemish wild boar. Infection Ecology Epidemiol 6: 31099.
- Holzmann H (2003) Diagnosis of tick-borne encephalitis. Vaccine 1: S36-S40
- Dohoo I, Martin W, Stryhn H (2009) Chapter 5: Screening and Diagnostic Tests, Veterinary Epidemiologic Research. 2nd Edn, Charlottetown, Prince Edward Island, Canada pp: 91-134.
- Linden A, Wirtgen M, Nahayo A, Heyman P, Niedrig M, et al. (2012) Tickborne encephalitis virus antibodies in wild cervids in Belgium. Vet Rec 170: 108.
- Linden A (2005) Epidemiological surveillance of wildlife diseases in the Walloon Region.
- Tavernier P, Sys SU, De Clerck K, De Leeuw I, Caij AB, et al. (2015) Serologic screening for thirteen infectious agents in roe deer (Capreolus capreolus) in Flanders. Infection Ecol Epidemiol 5: 12.
- Hadorn DC, Stark KD (2008) Evaluation and optimization of surveillance systems for rare and emerging infectious diseases. Vet Res 39: 25.
- Dohoo I, Martin W, Stryhn H (2009) Chapter 2: Sampling, Veterinary Epidemiologic Research. 2nd Edn, Charlottetown, Prince Edward Island, Canada pp: 33-56.
- van der Poel WH, Van der Heide R, Bakker D, De Looff M, De Jong J, et al. Attempt to detect evidence for tick-borne encephalitis virus in ticks and mammalian wildlife in The Netherlands. Vector Borne Zoonotic Dis 5: 58-64.
- Cameron A (1999) Survey Toolbox for Livestock Diseases. A practical manual and software package for active surveillance in developing countries. ACIAR Monograph p: 330.
- Thrusfield M, Ortega C, de Blas I, Noordhuizen JP, Frankena K (2001) WIN EPISCOPE 2.0: improved epidemiological software for veterinary medicine. Vet Rec 148: 567-572.
- Cameron AR, Baldock FC (1998) A new probability formula for surveys to substantiate freedom from disease. Prev Vet Med 34: 1-17.
- Progen BG (2006) Immunozym FSME/TBE IgG All Species-ELISA. User’s Manual. Progen Biotechnik GmbH Heidelberg, Germany.
- Klaus C, Beer M, Saier R, Schubert H, Bischoff S, et al. (2011) Evaluation of serological tests for detecting tick-borne encephalitis virus (TBEV) antibodies in animals. Berl Munch Tierarztl Wochenschr 124: 443-449.
- Reed LJ, Muench H (1938) A simple method of estimating fifty percent endpoints. Am J Hyg 27: 493-497.
- Domingo C, Escadafal C, Rumer L, Mendez JA, Garcia P, et al. (2012) First international external quality assessment study on molecular and serological methods for yellow fever diagnosis. PLoS One 7: 3.
- Donoso Mantke O, Achazi K, Niedrig M (2007) Serological Versus PCR Methods for the Detection of Tick-borne Encephalitis Virus Infections in Humans. Future Virol 2: 565-572.
- Niedrig M, Avsic T, Aberle SW, Ferenczi E, Labuda M, et al. (2007) Quality control assessment for the serological diagnosis of tick borne encephalitis virus infections. J Clin Virol 38: 260-264.
- Glaser CA, Gilliam S, Schnurr D (2003) In search of encephalitis etiologies: diagnostic challenges in the California Encephalitis Project, 1998-2000. Clin Infect Dis 36: 731.
- Jarrin I, Sellier P, Lopes A, Morgand M, Makovec T, et al. (2016) Etiologies and Management of Aseptic Meningitis in Patients Admitted to an Internal Medicine Department. Medicine 95: 2372.
- Frantzidou F, Kamaria F, Dumaidi K, Skoura L, Antoniadis A, et al. (2008) Aseptic meningitis and encephalitis because of herpesviruses and enteroviruses in an immunocompetent adult population. Eur J Neurol 15: 995-997.
- Harrell T, Hammes JS (2012) Meningitis admitted to a military hospital: a retrospective case series. Mil Med 177: 1223-1226.
- Storch GA (2007) Chapter 17: Diagnostic Virology (5th edn.). Fields Virology 1: 592-593.
- Duscher GG, Wetscher M, Baumgartner R, Walder G (2015) Roe deer sera used for TBE surveillance in Austria. Ticks Tick Borne Dis 6: 489-493.
- Dobler G (2010) Zoonotic tick-borne flaviviruses. Vet Microbiol 140: 221-228.
- Gerth HJ, Grimshandl D, Stage B, Doller G, Kunz C (1995) Roe deer as sentinels for endemicity of tick-borne encephalitis virus. Epidemiol Infect 115: 355-365.
- Kunze U (2015) Tick-borne encephalitis as a notifiable disease–Status quo and the way forward. Report of the 17th annual meeting of the International Scientific Working Group on Tick-Borne Encephalitis (ISW-TBE). Ticks Tick Borne Dis 6: 545-548.
- Simundic AM (2008) Measures of diagnostic accuracy: basic definitions. Electronic J IFCC: Int Fed of Clin Chem Lab Med 19: 9.
- Banoo S, Bell D, Bossuyt P, Herring A, Mabey D, et al. Evaluation of diagnostic tests for infectious diseases: general principles. Nat Rev Micro 8: 17-29.
- Leeflang MM, Bossuyt PM, Irwig L (2009) Diagnostic test accuracy may vary with prevalence: implications for evidence-based diagnosis. J Clin Epidemiol 62: 5-12.
- Ikawa-Yoshida A, Yoshii K, Kuwahara K, Obara M, Kariwa H, et al. (2011) Development of an ELISA system for tick-borne encephalitis virus infection in rodents. Microbiol Immunol 55: 100-107.
- Obara M, Yoshii K, Kawata T, Hayasaka D, Goto A, et al. (2006) Development of an enzyme-linked immunosorbent assay for serological diagnosis of tick-borne encephalitis using subviral particles. J Virol Methods 134: 55-60.
- Callens S (2016) Encephalitis clinical approach of uncommon, emerging and traveling causes of encephalitis (UZ Gent-AZ Sint. Lucas). Spring symposium, Seminar: diagnosis and surveillance of infectious diseases.
- Debiasi RL, Tyler KL (2004) Molecular methods for diagnosis of viral encephalitis. Clin Microbiol Rev 17: 903-925.
- Parisi SG, Basso M, Del Vecchio C, Andreis S, Franchin E, et al. (2016) Virological testing of cerebrospinal fluid in children aged less than 14 years with a suspected central nervous system infection: A retrospective study on 304 consecutive children from January 2012 to May 2015. Eur J Paediatr Neurol 16: 30005-30008.
- Solomon T, Hart IJ, Beeching NJ (2007) Viral encephalitis: a clinician’s guide. Pract Neurol 7: 288-305.
- Tunkel AR, Glaser CA, Bloch KC, Sejvar JJ, Marra CM, et al. (2008) The management of encephalitis: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis 47: 303-327.
- Jahfari S, de Vries A, Rijks J, Van Gucht S, Sprong H, et al. (2015) Tick-borne encephalitis virus found in the Netherlands. Euro Surveill.
- RIVM (2016) Signal encephalitis virus found in the Netherlands, National Institute for Public Health and Environment, Ministry of Health, Welfare and Sport.
- RIVM: Patient ill by sign encephalitis virus, National Institute for Public Health and Environment, Ministry of Health, Welfare and Sport.
- Rodriguez-Prieto V, Vicente-Rubiano M, Sanchez-Matamoros A, Rubio-Guerri C, Melero M, et al. (2014) JM: Systematic review of surveillance systems and methods for early detection of exotic, new and re-emerging diseases in animal populations. Epidemiol Infect pp: 1-25.
- Thurmond MC (2003) Conceptual foundations for infectious disease surveillance. J Vet Diagn Invest 15: 501-514.
- Stefanoff P, Pfeffer M, Hellenbrand W, Rogalska J, Ruhe F, et al. (2013) Virus detection in questing ticks is not a sensitive indicator for risk assessment of tick-borne encephalitis in humans. Zoo Pub Health 60: 215-226.
- KICM (2016) Tick-borne encephalitis. Infectology and Travel Medicine, Department (KICM) of the Louis Pasteur University Hospital, Slovakia.
- Markovinovic L, Kosanovic Licina ML, Tesic V, Vojvodic D, Vladusic Lucic I (2015) An outbreak of tick-borne encephalitis associated with raw goat milk and cheese consumption.
- Belikov SI, Kondratov IG, Potapova UV, Leonova GN (2014) The relationship between the structure of the tick-borne encephalitis virus strains and their pathogenic properties. PLoS ONE 9: e94946.
- Bertrand Y, Topel M, Elvang A, Melik W, Johansson M (2012) First dating of a recombination event in mammalian tick-borne flaviviruses. PLoS One 7: e31981
- Formanova P, Cerny J, Bolfikova BC, Valdes JJ, Kozlova I, et al. (2015) Full genome sequences and molecular characterization of tick-borne encephalitis virus strains isolated from human patients. Ticks Tick Borne Dis 6: 38-46.
- Fajs L, Durmisi E, Knap N, Strle F, Avsic-Zupanc T (2012) Phylogeographic characterization of tick-borne encephalitis virus from patients. Rodents and ticks in Slovenia. PLoS ONE 7: e48420.
- Golovljova I, Vene S, Sjolander KB, Vasilenko V, Plyusnin A (2004) Characterization of tick-borne encephalitis virus from Estonia. J Med Virol 74: 580-588.
- Leonova GN, Belikov SI, Kondratov IG, Takashima I (2013) Comprehensive assessment of the genetics and virulence of tick-borne encephalitis virus strains isolated from patients with in apparent and clinical forms of the infection in the Russian Far East. Virology 443: 89-98.
- Wallner G, Mandl CW, Ecker M, Holzmann H, Stiasny K, et al. (1996) Characterization and complete genome sequences of high- and low- virulence variants of tick-borne encephalitis virus. J Gen Virol 77: 1035-1042.
- Romanova L, Gmyl AP, Dzhivanian TI, Bakhmutov DV, Lukashev AN, et al. (2007) Microevolution of tick-borne encephalitis virus in course of host alternation. Virology 362: 75-84.
- Kaluzova M, Eleckova E, Zuffova E, Pastorek J, Kaluz S, et al. (1994) Reverted virulence of attenuated tick-borne encephalitis virus mutant is not accompanied with the changes in deduced viral envelope protein amino acid sequence. Acta Virol 38: 133-140.
- Pogodina VV, Karan LS, Koliasnikova NM, Levina LS, Malenko GV, et al. (2007) Evolution of tick-borne encephalitis and a problem of evolution of its causative agent. Vopr Virusol 52: 16-21.
- Zanotto PM, Gao GF, Gritsun T, Marin MS, Jiang WR, et al. (1995) An arbovirus cline across the northern hemisphere. Virology 210: 152-159.
- Hubalek Z, Pow I, Reid HW, Hussain MH (1995) Antigenic similarity of central European encephalitis and louping-ill viruses. Acta Virol 39: 251-256.
- Carpi G, Bertolotti L, Rosati S, Rizzoli A (2000) Prevalence and genetic variability of tick-borne encephalitis virus in host-seeking Ixodes ricinus in northern Italy. J Gen Virol 90: 2877-2883
- Hubalek Z, Rudolf I (2012) Tick-borne viruses in Europe. Parasitol Res 111: 9-36.
- Hubalek Z, Rudolf I, Nowotny N (2014) Arboviruses pathogenic for domestic and wild animals. Adv Virus Res 89: 201-275.
- Mansfield KL, Balseiro Morales A, Johnson N, Ayllon N, Hofle U, et al. (2015) Identification and characterization of a novel tick-borne flavivirus sub-type in goats (Capra hircus) in Spain. J Gen Virol 20: 000096.
- Braks M, Medlock JM, Hubalek Z, Hjertqvist M, Perrin Y, et al. (2014) Vector-borne disease intelligence: strategies to deal with disease burden and threats. Front Public Health 2: 280.
- Leach M, Scoones I (2013) The social and political lives of zoonotic disease models: narratives, science and policy. Soc Sci Med 88: 10-17.
- Obsomer V, Boucher I, Delmee M (2013) Dutch borders impervious to ticks or Lyme borreliosis underreporting in Belgium. Acta Clin Belg 68: 390.
- Obsomer V, Wirtgen M, Linden A, Claerebout E, Heyman P (2013) Spatial disaggregation of tick occurrence and ecology at a local scale as a preliminary step for spatial surveillance of tick-borne diseases: general framework and health implications in Belgium. Parasit Vectors 6: 190.
- Jahfari S, Coipan EC, Fonville M, van Leeuwen AD, Hengeveld P (2014) Circulation of four Anaplasma phagocytophilum ecotypes in Europe. Parasit Vectors 7: 365.
- Dohoo I, Martin W, Stryhn H (2009) Chapter 18: Modelling count and rate data, Veterinary Epidemiologic Research. 2nd edition, Charlottetown, Prince Edward Island, Canada pp: 462-464.
- Dohoo I, Martin W, Stryhn H (2009) Chapter 16: Logistic Regression, Veterinary Epidemiologic Research. 2nd edition, Charlottetown, Prince Edward Island, Canada pp: 421.
- Lean IJ, Rabiee AR, Duffield TF, Dohoo IR (2009) Invited review: Use of meta-analysis in animal health and reproduction: methods and applications. J Dairy Sci 92: 3545-3565.
- O'Connor AM, Sargeant JM (2014) Meta-analyses including data from observational studies. Prev Vet Med 113: 313-322.
- Sargeant JM, O'Connor AM (2014) Introduction to systematic reviews in animal agriculture and veterinary medicine. Zoon Public Health 1: 3-9.
- Sixl W, Batikova M, Stunzner D, Sekeyova M, Sixl-Voigt B (1973) Haemagglutination-inhibiting antibodies against arboviruses in animal sera, collected in some regions in Austria. Zentralbl Bakteriol Orig 224: 303-308.
- Muller W (1997) TBE in the dog-seroepidemiological studies. Tick-borne Encephalitis and Lyme Borreliosis, Pabst Science Publishers, Lengerich, Germany pp: 204-218.
- Muller W (2002) FSME Seropravalenz beim Hund in Deutschland. 9th InnLab Conference, Munich.
- Reiner B, Grasmuck S, Steffen F, Djuric N, Schindler T (2002) Prevalence of TBE in serum and CSF of dogs with inflammatory and non-inflammatory CNS disease. Int J Med Microbiol 33: 234.
- Wattle O (1992) Tick-borne encephalitis virus infection in dogs. Vet Med Faculty.
- Matile H, Ferrari E, Aeschlimann A, Wyler R (1981) The transmission of tick-borne encephalitis in Switzerland. An attempt at establishing a register of natural reservoirs for a seroepidemiologic examination of forest personnel in the middle of the country. Schweiz Med Wochenschr 111: 1262-1269.
- Takashima I, Morita K, Chiba M, Hayasaka D, Sato T, et al. (1997) A case of tick-borne encephalitis in Japan and isolation of the the virus. J Clin Microbiol 35: 1943-1947.
- Lindhe KE, Meldgaard DS, Jensen PM, Houser GA, Berendt M (2009) Prevalence of tick-borne encephalitis virus antibodies in dogs from Denmark. Acta Vet Scand 51: 56.
- Klaus C, Horugel U, Hoffmann B, Beer M (2013) Tick-borne encephalitis virus (TBEV) infection in horses: clinical and laboratory findings and epidemiological investigations. Vet Microbiol 163: 368-372.
- Vesenjak-Hirjan J, Galinovic-Weisglass M, Brudnjak Z (1976) Infections with tick-borne encephalitis virus in the Pannonian focus Stara Ves 1, Serological studies 1961-1964. Work of the Yugoslav Academy of Arts Science 13: 11-20.
- Vesenjak-Hirjan J, Galinovic-Weisglass M, Brudnjak Z (1972) Infections with tick-borne encephalitis virus in the Pannonian focus Stara Ves 2, Serological studies. Work of the Yugoslav Academy of Arts Science 13: 21-28.
- Luckschander N (1998) TBE infection in the Austrian horse population, dissertation from the Vienna University of Veterinary Medicine.
- Luckschander N, Kolbl S, Enzesberger O, Zipko HT (1999) Tick borne encephalitis (TBE) in an Austrian horse population. Tierarztl Prax Edn Grostiere Farm Animals 127: 235-238.
- Sikutova S, Hornok S, Hubalek Z, Dolezalkova I, Juricova Z, et al. (2009) Serological survey of domestic animals for tick-borne encephalitis and Bhanja viruses in northeastern Hungary. Vet Microbiol 135:267-271.
- Cisak E, Wojcik-Fatla A, Zajac V, Sroka J, Buczek A (2010) Prevalence of tick-borne encephalitis virus (TBEV) in samples of raw milk taken randomly from cows, goats and sheep in eastern Poland. Ann Agric Environ Med 17: 283-286.
- Leutloff R, Nubling M, Neumann-Haefelin D, Rieger M (2006) Cows as indicators for TBE endemic regions: suitability of testing for antibodies in serum and milk. Int J Med Microbiol 296: 87-88.
- Girjabu E, Draganescu N, Iftimovici R (1985) Serological investigations on the presence of antibodies to tick-borne encephalitis virus in domestic animals and birds and in humans. Virologie 36: 161-164.
- Holzmann H, Aberle SW, Stiasny K, Werner P, Mischak A, et al. (2009) Tick-borne encephalitis from eating goat cheese in a mountain region of Austria. Emerg Infect Dis 15: 1671-1673.
- Ernek E, Kozuch O (1970) Zeckenencephalitis virus neutralizing antibodies in cattle as an indicator of viral presence in Central European herds of herds Zbl Bakt parasite 213: 151-160.
- Hubalek Z, Cerny V, Mittermayer T, Kilik J, Halouzka J, et al. (1986) Arbovirological survey in Silica plateau area, Roznava District, Czechoslovakia. J Hyg Epidemiol Microbiol Immunol 30: 87-98.
- Brummer-Korvenkontio M, Saikku P, Korhonen P, Oker-Blom N (1973) Arboviruses in Finnland. I. Isolation of Tick-Borne Encephalitis (TBE) Virus from Arthrophods, Vertebrates, and Patients. Amer J Trop Med Hyg 22: 382-289.
- Cisak E, Wojcik-Fatla A, Sroka J, Zajac V, Bilska-Zajac E, et al. (2012) Prevalence of Tick-Borne Encephalitis Virus Antibodies in Domestic and Game Animals from Eastern Poland. Bulletin of the Veterinary Institute in Pulawy 56: 275-278.
- Rieger MA, Nubling M, Huwer M, Muller W, Hofmann F (1997) Studies on the epidemiology of early summer meningoencephalitis: Do cattle participate in the cycle of virus transmission in the southwestern German endemic area? Immunity Infection 1: 52-57.
- Juceviciene A, Zygutiene M, Leinikki P, Brummer-Korvenkontio H, Salminen M, et al. (2005) Tick-borne encephalitis virus infections in Lithuanian domestic animals and ticks. Scand J Infect Dis 37: 742-746.
- Korenberg EI, Pchelkina AA, Spitsina LN (1984) Consistent patterns in the contact of domestic animals with tick-borne encephalitis virus in the eastern part of the Russian plain. J Hyg Epidemiol Microbiol Immunol 28: 73-84.
- Rieille N, Klaus C, Ambord C, Dupuis G, Peter O, Voordouw MD (2013) Use of goats as indirect indicators for detection of tick-borne encephalitis virus (TBEV) in a new risk area in Switzerland.
- Rizzoli A, Neteler M, Rosa R, Versini W, Cristofolini A, Bregoli M, Buckley A, Gould EA (2007) Early detection of tick-borne encephalitis virus spatial distribution and activity in the province of Trento, Northern Italy. Geospat Health 1: 169-176.
- Klaus C, Hoffmann B, Moog U, Schau U, Beer M, et al. (2010) Can goats be used as sentinels for tick-borne encephalitis (TBE) in nonendemic areas? Experimental studies and epizootiological observations, Berl Munch Tierarztl Wochenschr 123: 441-445.
- Klaus C, Hoffmann B, Beer M, Muller W, Stark B, et al. (2010) Seroprevalence of tick-borne encephalitis (TBE) in naturally exposed monkeys (Macaca sylvanus) and sheep and prevalence of TBE virus in ticks in a TBE endemic area in Germany. Ticks Tick Borne Dis 1: 141-144.
- Klaus C, Beer M, Saier R, Schau U, Moog U, et al. (2012) Goats and sheep as sentinels for tick-borne encephalitis (TBE) virus–epidemiological studies in areas endemic and non-endemic for TBE virus in Germany. Ticks Tick Borne Dis 3: 27-37.
- Klaus C, Ziegler U, Kalthoff D, Hoffmann B, Beer M (2014) Tick-borne encephalitis virus (TBEV)-findings on cross reactivity and longevity of TBEV antibodies in animal sera. BMC Vet Res 10: 78.
- Labuda M, Eleckova E, Lickova M, Sabo A (2002) Tick-borne encephalitis virus foci in Slovakia. Int J Med Microbiol 33: 43-47.
- Vesenjak-Hirjan J, Galinovic-Weisglass M, Brudnjak Z (1976) Infections with tick-borne encephalitis virus in the Mediterranean focus Nadsela (Island of Brac). Work of the Yugoslav Academy of Arts Science 13: 29-36.
- Juricova Z, Hubalek Z (1999) Serological surveys for arboviruses in the game animals of southern Moravia (Czech Republic). Folia Zool 48: 185-189.
- Hubalek Z, Juricova Z, Svobodova S, Halouzka J (1993) A serologic survey for some bacterial and viral zoonoses in game animals in the Czech Republic. J Wildl Dis 29: 604-607.
- Duscher GG, Leschnik M, Fuehrer HP, Joachim A (2014) Wildlife reservoirs for vector-borne canine, feline and zoonotic infections in Austria. Int J Parasitol Parasites Wildl 4: 88-96.
- Radda A, Kunz C, Hofmann H (1968) Demonstration of antibodies in sera of wild animals for the detection of foci of tick-borne encephalitis (TBE) virus in Lower Austria. Central Bl Bacteriol Orig 208: 88-93n
- Kiffner C, Vor T, Hagedorn P, Niedrig M, Ruhe F (2012) Determinants of tick-borne encephalitis virus antibody presence in roe deer (Capreolus capreolus) sera. Med Vet Entomol 26: 18-25.
- Balling A, Plessow U, Beer M, Pfeffer M (2014) Prevalence of antibodies against tick-borne encephalitis virus in wild game from Saxony, Germany. Ticks Tick Borne Dis 5: 805-809.
- Borcic B, Raos B, Kranzelic D, Abu Eldan J, Filipovic V (1990) The role of large wildlife in the maintenance of natural foci of tick-borne meningoencephalitis in northern Croatia. Acta Med Iugosl 44: 399-406.
- Gomez-Martinez C (2014) Role of cervids and wild boar on the presence of tick-borne encephalitis virus in Sweden. Swedish University of Agricultural Sciences pp: 1-17.
- Jemersic L, Dezdek D, Brnic D, Prpic J, Janicki Z, et al. (2014) Detection and genetic characterization of tick-borne encephalitis virus (TBEV) derived from ticks removed from red foxes (Vulpes vulpes) and isolated from spleen samples of red deer (Cervus elaphus) in Croatia. Ticks Tick Borne Dis 5: 7-13.
- Kim SY, Yun SM, Han MG, Lee IY, Lee NY, et al. (2008) Isolation of tick-borne encephalitis viruses from wild rodents, South Korea. Vector Borne Zoonotic Dis 8: 7-13.
- Biernat B, Karbowiak G (2014) Study on the occurrence of tick-borne encephalitis virus RNA in European bison (Bison bonasus) eliminated at Bialowieza Primeval Forest (north-eastern Poland) in 2005-2009. Ann Parasitol 60: 99-102.
- Wurm R, Dobler G, Peters M, Kiessig ST (2000) Serological investigations of red foxes (Vulpes vulpes L.) for determination of the spread of tick-borne encephalitis in Northrhine-Westphalia. J Vet Med B Infect Dis Vet Public Health 47: 503-509.
- Rieger MA, Nubling M, Muller W, Hasselhorn HM, Hofmann F et al. (1999) Foxes as indicators for TBE endemicity–a comparative serological investigation. Extended summary, Central Leaf for Bacteriology 289: 610-618.
- Kozuch O, Labuda M, Lysy J, Weismann P, Krippel E (1990) Longitudinal study of natural foci of Central European encephalitis virus in West Slovakia. Acta Virol 34: 537-544.
- Pinter R, Madai M, Horvath G, Nemeth V, Oldal M, et al. (2014) Molecular Detection and Phylogenetic Analysis of Tick-Borne Encephalitis Virus in Rodents Captured in the Transdanubian Region of Hungary. Vector Borne Zoonotic Dis 14: 621-624.
- Zoldi V, Papp T, Rigo K, Farkas J, Egyed L (2014) A 4-Year Study of a Natural Tick-Borne Encephalitis Virus Focus in Hungary, 2010-2013. Ecohealth 2014.
- Svoboda P, Dobler G, Markotic A, Kurolt IC, Speck S, et al (2014) Survey for Hantaviruses, Tick-Borne Encephalitis Virus, and Rickettsia spp. in Small Rodents in Croatia. Vector Borne Zoonotic Dis 14: 523-530.
- Achazi K, Ruzek D, Donoso-Mantke O, Schlegel M, Ali HS, et al. (2011) Rodents as sentinels for the prevalence of tick-borne encephalitis virus. Vector Borne Zoonotic Dis 11: 641-647.
- Kiebling JR (2005) Investigation on the occurrence of the Early Meningo Encephalitis Virus and Borrelia burgdorferi in selected wild and tick populations of Bavaria. Inaugural Dissertation, Veterinary Faculty of the Ludwig-Maximilians, University of Munich pp: 154.
- Bakhvalova VN, Dobrotvorsky AK, Panov VV, Matveeva VA, Tkachev SE, et al. (2006) Natural tick-borne encephalitis virus infection among wild small mammals in the southeastern part of western Siberia, Russia. Vector Borne Zoonotic Dis 6: 32-41.
- Tonteri E, Jaaskelainen AE, Tikkakoski T, Voutilainen L, Niemimaa J, et al. (2011) Tick-borne encephalitis virus in wild rodents in winter, Finland, 2008-2009. Emerg Infect Dis 17: 72-75.
- Labuda M, Stunzner D, Kozuch O, Sixl W, Kocianova E, et al. (1993) Tick-borne encephalitis virus activity in Styria, Austria. Acta Virol 37: 187-190.
- Knap N, Korva M, Dolinsek V, Sekirnik M, Trilar T, et al. (2012) Patterns of tick-borne encephalitis virus infection in rodents in Slovenia. Vector Borne Zoonotic Dis 12: 236-242.
- Burri C, Korva M, Bastic V, Knap N, Avsic-Zupanc T, et al. (2012) Serological evidence of tick-borne encephalitis virus infection in rodents captured at four sites in Switzerland. J Med Entomol 49: 436-439.
- Mikryukova TP, Moskvitina NS, Kononova YV, Korobitsyn IG, Kartashov MY,et al. (2014) Surveillance of tick-borne encephalitis virus in wild birds and ticks in Tomsk city and its suburbs (Western Siberia). Ticks Tick Borne Dis 5: 145-151.
- Lindh E, Huovilainen A, Ratti O, Ek-Kommonen C, Sironen T, et al. (2008) Orthomyxo-, paramyxo- and flavivirus infections in wild waterfowl in Finland. Virol J 2008 5: 35.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences