Comparative Evaluation of Stool Antigen Immunoassay and Blood Antibody Test Methods for the Screening of Helicobacter Pylori Infection in Asymptomatic Adult Population in Delta State, Nigeria
Omosor Kingsley Ifeanyichukwu1, Omosor Omasan Herrienta1, Adejumo Babatunde Ishola Gabriel2*, Ibeh Isaiah Nnana2 and Dimkpa Uchechukwu3
1Shalom Diagnostic Medical Laboratory, Warri, Delta State, Nigeria
2Medical Laboratory, Science Department, University of Benin, Benin City, Nigeria
3Physiology Department, Nnewi Campus, Nnamdi Azikiwe University, Awka, Nigeria
- *Corresponding Author:
- Adejumo Babatunde Ishola Gabriel
Medical Laboratory
Science Department, University of Benin
Benin City, Nigeria
Tel: +2348000000000
E-mail: bigadejumo@yahoo.com
Received Date: 27 February 2018; Accepted Date: 23 March 2018; Published Date: 30 March 2018
Citation: Omosor K.I., Omosor O.H, Adejumo B.I.G., Ibeh I.N., Dimkpa U. (2018) Comparative Evaluation of Stool Antigen Immunoassay and Blood Antibody Test Methods for the Screening of Helicobacter Pylori Infection in Asymptomatic Adult Population in Delta State, Nigeria. J Mol Microbiol. Vol. 2 No. 1: 3.
Copyright: © 2018 Omosor K.I., et al. This is an open-access article distributed under the terms of the creative Commons attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Aim: To compare the H.pylori positivity between stool antigen and blood antibody test methods and to determine the accuracy, sensitivity, specificity of the stool antigen and IgG serology tests as well as sex, age and geographical area variations with the rate of H. pylori positivity. Methods: 408 asymptomatic volunteers (aged 32.55 ± 11.98 years) participated in this study. Stool and serum samples were obtained and assayed quantitatively using the stool antigen Accu-Diag H. pylori Antigen and Accu-Bind antibody ELISA Kits respectively. The stool samples were also assayed qualitatively using the monoclonal fecal H. pylori antigen rapid test kit (Aria H. Pylori Ag Combo Rapid Test. Results: The overall positivity rate of H. pylori stool antigen test (28.2%) was significantly lower (P=0.02) compared to that of the serology test (48.3%). No statistical differences were observed between genders and among age groups and geographical areas in both the stool and serology tests. The positivity in age group of ≥ 60 yrs in the IgG antibody test was significantly (p<0.05) greater compared with age groups 18-39 years and 40-59 years respectively. The stool antigen test had a higher sensitivity (100% vs. 59.8%), specificity (98.7% vs. 57.9%), accuracy (99% vs. 60%) and area under the Receiver Operator Characteristic curve (99.3% vs. 61.4%) compared with the IgG serology test. Conclusion: The present study suggests that H. pylori stool antigen test would be a more appropriate and reliable first-line routine test for diagnosis of H. pylori infection in Delta region of Nigeria. The rate of positivity was not affected by sex and geographical areas, but high prevalence rate of H. pylori infection was observed within the oldest population.
Keywords
Helicobacter Pylori; Stool sample; Enzyme linked immunosorbent assay; Blood antibody test
Introduction
Helicobacter Pylori a Gram-negative bacterium, is recognized as a major cause of chronic gastritis, gastric carcinoma, peptic ulcer disease and lymphoid tissue lymphoma of the gastric mucosa [1,2]. It is estimated that half of the world’s population are carriers of this bacterium [3,4]. The prevalence of H. pylori infection has been reported to be higher in developing countries relative to developed countries [5]. Different modes of transmission have been suggested by scientific literatures and these include, oro-oral, faeco-oral, gastro-oral, gastro-gastric and person-to-person transmissions [3,6]. Some of the risk factors for the transmission of H. pylori include, race, socioeconomic status, residing in rural area, age, poor sanitary conditions, overcrowding, poor diet, poor water supply and lower educational level of mothers [3,4,7-9].
The methods used for the diagnosis of H. pylori infection are classified into two major groups - the invasive and non-invasive tests [10]. The invasive methods are however considered more accurate than the non-invasive and involve culture, endoscopy and biopsy for histology and rapid urease test analysis. The non-invasive methods include serology, urea breath test and stool antigen analysis. Of the three non-invasive methods, urea breath test is reported to be the most accurate method used in determining H. pylori infection [11]. However, despite its accuracy, urea breath test has been found to be unreliable in very young children, cumbersome, expensive and consequently unavailable in certain countries [12,13]. The serologic tests are usually performed to detect specific circulating antibodies against H. pylori. They are commercially available, easy to perform and inexpensive, but reported to be unreliable for the diagnosis of H. pylori since they cannot differentiate between active and asymptomatic colonization and past and current H. pylori infection [14]. The stool antigen test is used to detect traces of H. pylori antigens in the feces. It is a reliable and accurate test for diagnosis of the H. pylori infection and confirmation of its cure after treatment, since it avoids detection of previous H. pylori infection. It is convenient to the patients and can be easily performed even in small laboratories [15,16]. However its accuracy in different clinical situations and outside of controlled studies is a matter of concern [17,18].
There is paucity of studies aimed at determining H. pylori diagnostic tests accuracy among asymptomatic adult population in Nigeria. In the light of the rising incidents of H. pylori infection in Nigeria, there is the need for basic studies on accuracy of cost effective and available non-invasive diagnostic methods. In this study, we compared the H. pylori positivity between the stool antigen test and a blood antibody test method (IgG) in order to determine which method is a more efficient and dependable non-invasive test for detection of H. pylori infection in asymptomatic adult patients population in a Niger-Delta area of Nigeria. In addition, the present study determined the accuracy, sensitivity, specificity, positive and negative likelihood ratios of the stool antigen and IgG serology tests as well as sex, age and geographical area variations with the rate of H. pylori positivity.
Materials and Methods
Participants
Four hundred and eight apparently healthy, asymptomatic volunteers (aged 32.55 ± 11.98 years) were recruited and screened for H. pylori infection. The participants were randomly selected from the three senatorial districts of Delta State - Delta South, Delta Central and Delta North districts after accepting our request asking them to participate in the study. The health history and demographic information of the participants were obtained from a well-structured questionnaire administered to them prior to the study. The exclusion criteria for selection of participants included, history of gastritis, gastric or duedonal ulcers, previous diagnoses or treatment for H. pylori infection, those on medication with proton-pump inhibitors, antibiotic, steroids or non-steroid anti-inflammatory drugs for the past one month. We sought and obtained informed consents of the participants after the purpose of the research was explained to them. The study was approved by the Ethical Committee of the Ministry of Health, Delta State, Nigeria.
Sample collection
Five milliliters of blood was collected and dispensed into a plain container. The non anticoagulated blood was spun at 1500rpm for 10 minutes and the supernatant serum was separated into a separate sterile tubes. The serum was stored at -200°C for up to 2 weeks prior to analysis for H. pylori antibodies (IgG). The quantitative assays of the serum and plasma samples were done using the Accu-Bind ELISA Microwells (system code, 1425-300; Monobind Inc, Lake Forest, CA 92630, USA) for the detection of IgG antibodies to H. pylori in human serum.
Stool samples were obtained from the participants and a small piece of the samples (~5 mm in diameter; ~150 mg) transferred into 1 ml of Sample Treatment Solution and mixed thoroughly in a test tube. This was then quantitatively assayed using the monoclonal H. pylori stool antigen kit (Accu-DiagTM ELISA , Cat #1506-11, USA), which is based on enzyme-linked immunoabsorbent assay (EIA). The stool samples were also assayed qualitatively using the monoclonal fecal H. pylori antigen rapid test kit (Aria H. pylori Ag Combo Rapid Test, Medtek, USA) based on the immunochromatography (ICA) technique. The performance of the quantitative enzyme immunoassay stool test and the IgG antibody serology test were determined with reference to the combined positive results of the EIA and ICA tests. The assay procedures were done according to the manufacturer’s instructions. The analyses of all the samples were carried out at Shalom Medical Services Ltd, Warri – Delta State, Nigeria.
Data analysis
Categorical data were expressed as percentages. Comparison of H. pylori positivity between the stool antigen and blood antibody tests was done using chi-square test (goodness of fit). The sensitivity, specificity, positive and negative likelihood ratios of the quantitative stool antigen and IgG serology tests were determined with reference to the results of the combined positive results of the EIA and ICA tests. The area under a Receiver Operating Characteristic (ROC) curve for each test was determined (with 95% confidence interval) and was compared with each other. The test of statistical significance was set at p<0.05. SPSS/IBM Statistical Software (version 20.0) was used to carry out all statistical analyses.
Results
Table 1 shows the socio-demographic characteristics of the study population. Data indicated that majority (81.6%) of the participants were aged between 18 – 39 years of age and followed by the age group, 40 – 59 years (13%). Those aged ≥ 60 years had the least percentage of the population (5.4%). The mean age of the study population was 32.55 ± 11.98 years (range 18-87 years). Majority (70.6%) of the study population were females, while the males constituted a smaller percentage (29.4%) of the population. The participants were selected from Delta South (34.6%), Delta North (34.1%) and Delta Central (31.4%) districts.
Table 1 Socio-demographic characteristics of the study population.
| Characteristics | Frequency | Percentage |
|---|---|---|
| Age Group | ||
| 18 – 39 yrs | 333 | 81.6 |
| 40 – 59 yrs | 53 | 13 |
| ≥ 60 yrs | 22 | 5.4 |
| Sex | ||
| Males | 120 | 29.4 |
| Females | 288 | 70.6 |
| Location | ||
| Delta Central | 128 | 31.4 |
| Delta North | 139 | 34.1 |
| Delta South | 141 | 34.6 |
The overall prevalence of Helicobacter Pylori in blood and stool of 408 volunteers is shown in Figure 1. The positivity rate of H. pylori EIA stool antigen test [28.2% (n=115)] were significantly lower (P=0.02) compared to that of the serology (IgG antibody) test [48.3% (n=197)]. Among the 408 subjects, 293 (71.8%) tested negative for EIA stool antigen test, while 211 (51.7%) tested negative for serology (antibody) test.
The prevalence of H. pylori according to sex of participants is summarized in Table 2. Data indicated no significant differences (P=0.09) in H. pylori positivity between the EIA stool antigen tests (32.5%) vs. blood (IgG antibody) test (47.5%) in males. In females, the H. pylori positivity in stool test (26.4%) was significantly (p=0.008) lower compared with IgG test (48.6%). Furthermore, higher prevalence rate of the H. pylori was observed in males in the stool antigen tests (32.5%) while in females it constituted 26.4%. In contrast, the H. pylori IgG test indicated higher prevalence rate in the females (48.6%) than the males (47.5%). However, no statistical differences were observed between the genders in both the stool and serology tests.
Table 2 The prevalence rate of H. pylori according to sex of subjects.
| Sex | Number of Subjects | EIA Stool Test | IgG Serology Test | χ2 | P-Value |
|---|---|---|---|---|---|
| N (%) | N (%) | ||||
| Males | 120 | 39 (32.5) | 57 (47.5) | 2.77 | 0.098 |
| Females | 288 | 76 (26.4) | 140(48.6)* | 7.05 | 0.008 |
| Total | 408 | 115 (28.2) | 197 (48.3) |
* Statistical difference between H.pylori positivity between the stool antigen test and blood antibody test; (Abbreviations: EIA = Enzyme-linked immunoabsorbent assay; IgG = Immunoglobulin; χ2 = Chi-square coefficient).
In Table 3 the serology test indicated significantly greater H. pylori positivity compared with the stool antigen test in 18-39 yrs age group (47.7% vs. 27.6%; p=0.02); in 40-59 yrs age group (43.4% vs. 26.4%; p=0.04) and in ≥ 60 yrs groups (68.2% vs. 40.9%); p=0.01). Data further indicated that the highest positive result was found in the age group of ≥ 60 yrs, which indicated 40.9% positivity by stool antigen test, and 68.2% by the serology test. The positivity in age group of ≥ 60 yrs in the IgG antibody test was significantly (χ2=6.60; p<0.05) greater compared with age groups 18-39 years and 40-59 years respectively. In contrast, there was lack of significant differences among age groups in the stool antigen test (χ2=4.18; p=0.12).
Table 3 The prevalence rate of H. pylori in different age groups.
| Age Groups | Number ofSubjects | EIA Stool Test | IgG Serology Test | χ2 | P-Value |
|---|---|---|---|---|---|
| (years) | N (%) | N (%) | |||
| 18 – 39 | 333 | 92 (27.6) | 159 (47.7)* | 5.26 | 0.022 |
| 40 – 59 | 53 | 14 (26.4) | 23 (43.4)* | 4.18 | 0.041 |
| ≥ 60 | 22 | 9 (40.9) | 15 (68.2)* | 6.68 | 0.01 |
| Total | 408 | 115 (28.2) | 197 (48.3) |
* Statistical difference between H.pylori positivity between the stool antigen test and blood antibody test; (Abbreviations: EIA = Enzyme-linked immunoabsorbent assay; IgG = Immunoglobulin; χ2 = Chi-square coefficient)
The prevalence rate of H. pylori according to the residence of participants is summarized in Table 4. H. pylori positivity in blood antibody test was significantly greater compared with the stool antigen test in Delta Central (59.4% vs. 32%; p=0.005), Delta North (44.6% vs. 25.2%; p=0.017), and Delta South (41.8% vs. 27.7%; p=0.043) respectively. Data indicated that the highest prevalence rate for H. pylori was observed in Delta Central as detected by stool test (32%) and blood test (59.4%). However, no statistical differences were observed among the geographical areas in both the stool and serology tests.
Table 4 The prevalence rate of H. pylori according to socio-economic stratified living region.
| Age Groups | Number ofSubjects | EIA Stool Test | IgG Serology Test | χ2 | P-Value |
|---|---|---|---|---|---|
| N (%) | N (%) | ||||
| Delta Central | 128 | 41 (32.0) | 76 (59.4)* | 8.01 | 0.005 |
| Delta North | 139 | 35 (25.2) | 62 (44.6)* | 5.71 | 0.017 |
| Delta South | 141 | 39 (27.7) | 59 (41.8)* | 4.08 | 0.043 |
| Total | 408 | 115 (28.2) | 197 (48.3) |
* Statistical difference between H.pylori positivity between the stool antigen test and blood antibody test; (Abbreviations: EIA = Enzyme-linked immunoabsorbent assay; IgG = Immunoglobulin; χ2 = Chi-square coefficient)
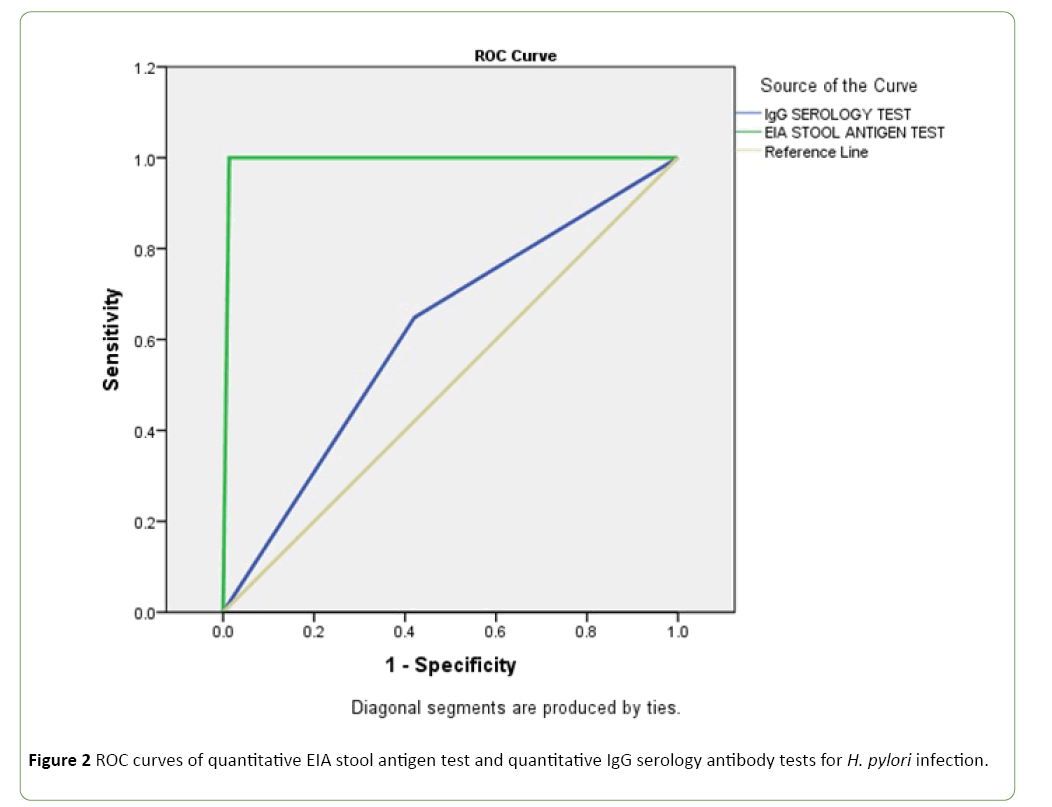
Figure 2 shows the results from ROC curve analyses generated for each test by plotting the true-positive rate (sensitivity) against the false-positive rate (1-specificity). The sensitivity, specificity, positive predictive value, negative predictive value, accuracy and area under ROC curve for each test, based on the predefined criteria, are shown in Table 5.
Table 5 Diagnostic characteristics of quantitative stool antigen test and quantitative IgG serology antibody tests for H.pylori infection.
| Results | H.Pylori Tests | |
|---|---|---|
| Stool Antigen Test | Igg Antibody Test | |
| Sensitivity | 1 | 0.598 |
| Specificity | 0.987 | 0.579 |
| Positive Predictive Value | 0.965 | 0.365 |
| Negative Predictive Value | 1 | 0.815 |
| Accuracy | 0.99 | 0.6 |
| Area under the ROC curve | 0.993 (0.986 – 1.00)* | 0.614 (0.553 – 0.675)* |
*95% confidence interval
Discussion
Helicobacter Pylori is a very common infection in developing countries, therefore a low-cost, rapid diagnostic technique may be useful for the management of H. pylori infection in both children and adults from these developing regions. Nigeria is one of the developing countries with rising incidents of gastritis and duodenal ulcers, as well as increasing prevalence of H. pylori infection hence the need to re-appraise the performances of different cost-effective, easy to use methods in diagnosis of H. pylori infection in the general population.
As expected, the EIA monoclonal stool antigen test was more accurate compared with the IgG serology test. The study showed high sensitivity (100%), high specificity (98.7%) and high accuracy (99%) of the quantitative enzyme-linked stool antigen test (Accu-DiagTM ELISA). However, this result applies only to this particular kit. In addition, the area under the curve of the ROC also indicates that the EIA monoclonal stool test is a more reliable diagnostic test for H. pylori diagnosis compared with the serology test. Previous studies [18-21] using monoclonal stool tests have shown sensitivities of between of 88.5%-98% and specificities of between 93.8%-99% in adults. The monoclonic stool antigen test has also been shown to have an initial diagnostic accuracy comparable with that of urea breath test and higher than both sero- logic and urine antibody tests [22], and may provide a viable alternative to the Urea Breath Test, especially in developing countries. The high accuracy, sensitivity and specificity observed in the present study makes the enzyme-linked stool antigen test suitable for use in clinical practice for primary screening of asymptomatic adult populations in Niger Delta region of Nigeria. The low accuracy, sensitivity and specificity of the serology test also suggest that this method may not be suitable for primary diagnosis of Helicobacter Pylori infection in this region.
In this study, the overall H. pylori positivity rate was higher in the serology test compared to the stool antigen test. The same trend was also observed in tests involving males, all age groups and all selected geographical areas. Previous studies have also reported lower positivity in stool antigen tests compared to the serology tests [23,24]. This may be attributed to the fact that H. pylori stool antigen test is a more accurate indicator of active disease compared to serology test, which may not measure active disease. H. pylori stool antigen test has been shown to be rapid, easy to use and differentiates between active and latent infection; whereas, serology only detects exposure and are not suitable to diagnose active infection or follow-up of eradication because of its low accuracy [25,26].
There were no significant differences between the two sexes with respect to H. pylori positivity in both stool antigen and serology tests. Previous studies [24,27] have also reported lack of gender differences in the rate of H. pylori positivity in both stool antigen and serology tests. In contrast, a study by Alim et al. [28] showed a significantly higher prevalence in female gender in both stool and serology tests. It is noteworthy that a greater number of females [n=288 (70.6%)] participated in this study. This may be a reflection of a greater consciousness of females on issues relating to their health.
The rate of H. pylori positivity showed a trend towards increase in rate of infection with the advancing age. The highest percentage positivity was observed in the age group ≥ 60 years compared with 18-39 years and 40-59 years respectively. The present study is in agreement with previous studies [29,30] which found that the age of H. pylori infection is more likely in patients over 50 years of age than in younger patients. However, another study [27] involving a mass survey of healthy adults, reported lack of age difference in H. pylori positivity.
H. pylori prevalence rates are reported to vary widely between different geographical regions and ethnic groups [31]. The risk of H. pylori prevalence by geographical areas may reflect differences in social and/or hygiene factors [32] and also related to differences in cultural background, social, dietary and environmental factors [33]. In the present study, we categorized geographical areas or residences of participants into three senatorial zones (North, South and Central) of Delta state, Nigeria. Our result indicated that the highest prevalence rate for H. pylori was observed in Delta Central as detected by stool test and blood test. However, when compared, no statistical differences were observed among these geographical areas in both the stool and serology tests. This may suggest that differences in social and cultural backgrounds or dietary and environmental factors among the Delta state people may not play a significant role in the rate of prevalence of H. pylori infection.
Conclusion
Although serologic testing is the most common noninvasive diagnostic method for H. pylori and is relatively inexpensive and convenient, the present findings indicate that the quantitative enzyme-linked stool antigen test (Accu-DiagTM ELISA), would be a more appropriate and reliable first-line routine test for diagnosis of H. pylori infection in large population surveys in Niger Delta region. It also provides a viable alternative to the more expensive and inconvenient 13C-UBT and endoscopy-based tests especially in developing countries. Our data also supports high prevalence rate of H. pylori infection within the oldest population.
References
- Akada JK, Shirai M, Takeuchi H, T suda M, Nakazawa T (2000) Identification of the urease operon in Helicobacter pylori and its controlby mRNA decay in response to pH. Mol Microbiol 36: 1071-1084.
- Akhiani AA, Pappo J, Kabok Z, Schon K,Gao W, et al. (2002) Protection against Helicobacter pylori infection Following immunization is IL-12-dependent and mediated by Th1 cells. J Immunol 169:6977-6984.
- Sethi Monica A, Chaudhuri C, Len Kelly C, Hopman W (2013) Prevalence of Helicobacter pylori in a First Nations population in northwestern Ontario. Can Fam Physician 59:182-1877.
- Hunt RH, Xiao SD, Megraud F, Leon-Barua R, Bazzoli F, Merwe SVD, et al. (2011) Helicobacter pylori in Developing Countries. J Clin Gastroenterol 45:383-388.
- Demiray E, Yılmaz Ö, Şarkış C, Soytürk M, Şimşek Ä° (2006) Comparison of invasive methods and two different stool antigen tests for diagnosis of H pylori infection in patients with gastric bleeding. World J Gastroenterol 12: 4206-4210.
- Brown LM (2000) Helicobacter pylori: epidemiology and routes of transmission. Epidemiol Rev 22:283-297.
- Li YH, Guo H, Zhang PB, Zhao XY, Da SP (2004) Clinical value of Helicobacter pylori stool antigen test, Immuno Card STAT HpSA, for detecting H pylori infection. World J Gastroenterol 10:913-914.
- Miranda ACP, Machado RS, da Silva EMK, Kawakami E (2010) Seroprevalence of Helicobacter pylori infection among children of low socioeconomic level in São Paulo. Sao Paulo Med J 128: 187-191.
- Malaty HM (2007) Epidemiology of Helicobacter pylori infection. Best Pract Res Clin Gastroenterol 21: 205-214.
- Calam J (1996) Clinicians guide to Helicobacter pylori. Chapman & Hall, London.pp:72-78.
- Gisbert JP, Pajares JM (2004) 13C-urea breath test in the diagnosis of Helicobacter pylori infection-a critical review. Aliment Pharmacol Ther 20: 1001-1017.
- Imrie C, Rowland M, Bourke B, Drumm B (2000) Limitations to carbon 13-labeled urea breath testing for Helicobacter pylori in infants. J Pediatr139:734-737.
- Megraud F (2005) Comparison of non-invasive tests to detect Helicobacter pylori infection in children and adolescents: results of a multicenter European study. J Pediatr146:198-203.
- Vaira D, Vakil N (2001) Blood, urine, stool, breath, money, and Helicobacter pylori. Gut 48: 287-289.
- Logan RPH, Walker MM (2001) Epidemiology and diagnosis of Helicobacter pylori infection. BMJ 323: 920-922.
- Malfertheiner P, Megraud F, O'Morain C, Hungin AP, JonesR, et al. (2002) Current concepts in themanagement of Helicobacter pylori infection-the Maastricht2-2000 Consensus Report. Aliment Pharmacol Ther 16:167-180.
- Vaira D, Ricci C, Menegatti M, Gatta L, Berardi S, et al. (2001) Stool test for Helicobacter pylori. Am J Gastroenterol 96: 1935-1938.
- Gisbert JP, Pajares JM (2004) Stool antigen test for the diagnosis of Helicobacter pylori infection: a systematic review. Helicobacter 9: 347-368
- Agha-Amiri K, Peitz U, Mainz D, Kahl S, Leodolter A, et al. (2001) A novel immunoassay based on monoclonal antibodies for the detection of Helicobacter pylori antigens in human stool. J Gastroenterol 39: 555-560.
- Andrews J, Marsden B, Brown D, Wong VS, Wood E, et al. (2003) Comparison of three stool antigen tests for Helicobacter pylori detection. J Clin Pathol 56: 769-771.
- Ashgar SS (2013) Helicobacter pylori diagnosis by stool antigen ELISA and rapid test. J App Med Sci 4: 61-66.
- Malfertheiner P, Megraud F, O’Morain CA, Atherton J, Axon AT, et al. (2012) Management of Helicobacter pylori infection-the Maastricht IV/Florence Consensus Report. Gut 61: 646-64.
- She RC, Wilson AR, Litwin CM (2009) Evaluation of Helicobacter pylori Immunoglobulin G (IgG), IgA, and IgMserologic testing compared to stool antigen testing. Clin Vaccine Immunol 16: 1253-1255.
- Naji AS, Ameri GAA, Alkadasi MN, Hanash S, Ali WAM, et al. (2014) Comparison of stool antigen and blood antibody test methods for detection of Helicobacter pylori infection and the risk factors. Int J Curr Microbiol App Sci 3: 118-127.
- Kazemi S, Tavakkoli H, Habizadeh MR, Emami MH (2011) Diagnostic values of Helicobacter pylori diagnostic tests: stool antigen test, urea breath test, rapid urease test, serology and histology. J Res Med Sci 16: 1097-1104.
- Rashed ME, Yassin MH, AbdelAllah NH, Zidan T (2015) Immunologicaltestscomparisonforthedetectionof helicobacter pylori infection in Egyptian adult patients. Indian J Med Res Pharm Sci 2: 42-48.
- Shimoyama T, Oyama T, Matsuzaka M, Danjo K, Nakaji S, et al. (2009) Comparison of a stool antigen test and serology for the diagnosis of Helicobacter pylori infection in mass survey. Helicobacter 14:87-90.
- Alim A, Ataş M, Güneş T, Özkan S, Dündar N (2010) Comparison of antigen and antibody detection tests used for diagnosing the Helicobacter pylori infection in symptomatic patients. Basic Clin Sci 1:61-70.
- Khan MA, Ghazi HO (2007) Helicobacterpylori infection in asymptomatic subjects in Makkah, Saudi Arabia. J Pak Med Assoc 57:114–117.
- Hanifi MI, Mohamed AM (2013) Helicobacterpylori infection: seroprevalence and predictors among healthy individuals in Al Madinah, Saudi Arabia. J Egypt Public Health Assoc 88: 40-45.
- Goh KL, Chan WK, Shiota S, Yamaoka Y (2011) Epidemiology of Helicobacter pylori Infection and Public Health Implications. Helicobacter 16: 1–9.
- Malaty HM, Graham DY, Wattigney WA, Srinivasan SR, Osato M, et al. (1992) Natural history of Helicobacter pylori infection in childhood: 12-year follow-up cohort study in a biracial community. Clin Infect Dis 28:279-282.
- Dorji D, Dendup T, Malaty HM, Wangchuk K, Yangzom D, et al. (2014) Epidemiology of Helicobacter pylori in Bhutan: the role of environment and Geographic location. Helicobacter 19:69-73.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences