Clinico-Paraclinical Aspects and Prognostic Factors of Extracapillary Glomerulonephritis in Senegal
Mahamat Abderraman G1*, Cisse MM2, Keita N1, Diagne S2, Lemrabot AT2, Faye M2, Fall K2, Faye M2, Keita AI2, Mbengue M2, Bacary BA2, Dieng A2, Mamadou Awa BA2, Elhaj Fary KA2, Niang A2 and Diouf B2
1Department of Nephrology, Renaissance Hospital, France
2Department of Nephrology, Aristide le Dantec Hospital, Dakar, Senegal
- *Corresponding Author:
- Mahamat Abderraman Guillaume
Department of Nephrology
Renaissance Hospital, France
Tel: 00235.66.61.95.95
E-mail: zalba2001@yahoo.fr
Received date: July 10, 2018; Accepted date: November 23, 2018; Published date: November 30, 2018
Citation: Abderraman GM, Cisse MM, Keita N, Diagne S, Lemrabot AT, et al. (2018) Clinico- Paraclinical Aspects and Prognostic Factors of Extracapillary Glomerulonephritis in Senegal. J Nephrol Urol Vol.2 No.1:2
Copyright: © 2018 Abderraman GM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
ECGN (extra-capillary glomerulonephritis) is characterized by a more or less circumferential crescent-shaped cell proliferation surrounding the glomerular flocculus. The prevalence varies between 2 and 10% of all nephrological conditions. With availability of a renal histopathology unit in Senegal since 2009, we conducted this work to study the epidemiological, clinical, paraclinical, therapeutic and evolutionary aspects of ECGN and to determine its factors of poor prognosis.
Patient and method: This was a retrospective and descriptive study carried out in the nephrology department of Aristide le Dantec Hospital in Dakar and in the pathology anatomy laboratory of Grand Yoff General Hospital on a six-year period from January 1, 2010 to December 31, 2015, including all records of patients who had a ECGN diagnosed under an optical microscope, with a crescent percentage greater than or equal to 30%.
Results: Forty-three cases of ECGN out of a total of 750 kidney biopsies were selected, giving a hospital proportion of 5.73%. The mean age of the patients was 32.53 ± 17.91 years with extremes of 4 and 70 years. Predominance was female with a sex ratio of 0.59. The duration of illness at admission was 53.2 days with (15 - 150 days). Edema of the lower limbs was present in 87.3%; hypertension in 53.5% and anuria in 25.6% which was a factor of poor renal prognosis (p=0.027). At the urinary strip, there was proteinuria or hematuria in respectively 44.2% and 32.6%. Extrarenal digestive events were noted in 55.8% of patients, followed by joint and cardiac manifestations at an equal percentage of 25.6%. The mean serum creatinine at admission was 79.4 ± 72.4 mg/l with extremes of 2.83 to 310.3 mg/l. It is correlated with a factor of poor renal prognosis (p= 0.040); the average proteinuria was 3.94 ± 3 g/24 h with (0.56 to 17 g/24 h). In immunology, serum complement was low in 4 patients; native anti DNA antibodies in 4 patients; ANPA positive in 8 patients; GMB (glomerular basement membrane antibodies (Goodpasture syndrom) positive in 1 patient and anti-nuclear antibodies (ANA) in 1 patient. Histologically, the mean number of “sealing bread” was 2.6 with (0- 24), without any statistically significant correlation found with other variables. At diagnosis, Type III of ECGN was noted in 48.9%; type II in 48.8% and type I in 2.3% of cases. The etiologies were vasculitis (48.9%), lupus (30.2%) and post-infectious glomerulonephritis (18.6%). Therapeutically, 97.7% of patients received symptomatic treatment (antihypertensives, diuretics, treatment of extra renal signs…) associated with conventional treatment (methylprednisolone, cyclophosphamide) in 72.1% of cases. Anuria, elevated serum creatinine, and circumferential arrangement of the croissants were the factors of poor prognosis.
Conclusion: This study allowed us to determine the extent of the ECGN in Senegal. We note that in the absence of fast and adequate management of patient evolution is inevitably towards to end renal stage disease.
Keywords
Extracapillary glomerulonephritis; Prognostic factors; CKD; Senegal
Abbreviations
ECGN: Extra Capillary Glomerulonephritis; RPGN: Rapidly Progressive Glomerulonephritis; ANPA: Anti-neutrophil Polynuclear Antibodies; ANA: Anti-nuclear Antibodies; GBM antibodies: Glomerular Basement Membrane Antibodies.
Introduction
Extracapillary glomerulonephritis or ascending glomerulonephritis are a variety of glomerulopathies that are characterized by the presence of more or less circumferential crescent-shaped cell proliferation surrounding the flocculus and associated with a sometimes major inflammatory reaction that may progress to sclerosis [1]. Most commonly, it is a rapidly progressive glomerulonephritis (RPGN) with rapidly progressive renal failure within a few days or weeks with no tendency to spontaneous remission and presence of proteinuria and hematuria. Their diagnosis is histological by the presence of glomerular lesions involved more than 50% of glomeruli on a biopsy with at least a dozen glomeruli [1]. The immunofluorescence (IF) test provides essential elements for the etiological diagnosis and allows to classify them in three groups according to the appearance of the deposits. Prevalence of ECGN varies between 2 and 10% of all nephrological conditions [2]. In Europe, a German study founds an annual incidence of 0.7 / 100000 [3]. In the United States, a study conducted in March 2015 found an annual incidence of 7 cases per million inhabitants [4]. In India, a retrospective study conducted between 2011 and 2014 showed a prevalence of 5.76% [5]. Studies from North Africa found a ECGN incidence of 7.3% of all renal biopsies [6]. In South Africa, a 2009 study reported a prevalence of 11.4% [7]. In Senegal, a study in 2001 found a rate of 2% in a series of 115 renal biopsies [8]. The objective of our study was to study epidemiological, clinical, paraclinical, therapeutic and evolutionary aspects of ECGN and to determine its factors of poor prognosis.
Patients and Method
This was a retrospective and descriptive study conducted in the nephrology department of Aristide le Dantec Hospital in Dakar and the Pathology Anatomy Laboratory at Grand Yoff General Hospital. This study took place over a six-year period from January 1, 2010 to December 31, 2015, including all records of patients who had a ECGN diagnosed under an optical microscope, with a crescent percentage greater than or equal to 30%. We have included all records of patients with extracapillary glomerulonephritis injury. The files were processed using pre-printed cards from kidney biopsy requests and reports; records of hospitalization or consultation of patients. Epidemiological parameters (age, gender), clinical (time to admission, renal and extra-renal signs), biological (protidemia, albuminemia, azotemia, serum creatinine, blood count, antistreptolysin O, blood culture, throat cryoglobulinemia, hepatitis B virus, syphilitic serology, retroviral serology, anti-HCV (hepatitis C virus), native anti DNA antibodies, anti-neutrophil polynuclear antibodies (ANPA), anti-nuclear antibodies (ANA), GMB (glomerular basement membrane) antibodies, proteinuria, urinary sediment, cytobacterioligical urine exam and histological (indications of renal biopsy puncture, type and causes of ECGN).
Therapeutic modalities of each patient were schematically classified into three groups according to the nature of the treatment:
• group 1: Symptomatic treatment only
• group 2: Association symptomatic treatment and conventional treatment
Conventional treatment was 3 bolus of Methylprednisone for 3 days at a dose of 10-15 mg/kg/day, relayed by oral corticosteroid therapy at a dose of 1 mg/kg/day, associated with monthly bolus of cyclophosphamide, dose according to the clearance, for 6 months.
• group 3: Other immunosuppressive (rituximab)
Evolution was either after 6 months of well-conducted treatment:
• favorable: Defined by an estimate of creatinine clearance (MDRD), greater than or equal to 60 ml/min; in complete or partial remission;
• unfavorable in the form of:
• Relapse: Deterioration of the function after a significant improvement
• No response or resistance: No improvement in renal function despite well-conducted treatment
• Occurrence of complications related to the disease or treatment
• Death
According to the evolution, patients were classified into three groups:
• Group A: Patients in remission with the A1 group for patients in complete remission and A2 for patients in partial remission
• Group B: Resistance cases (no answer)
• Group C: For patients who have died
By comparing group A with groups B and C, the parameters (group B or C) with a statistically p<0.05 are considered as factors of poor renal or vital prognosis. Data collected on Excel file have been analyzed in the EPI Info version 3.5.2 software. When p is less than 0.05, it was considered as statistically significant.
Results
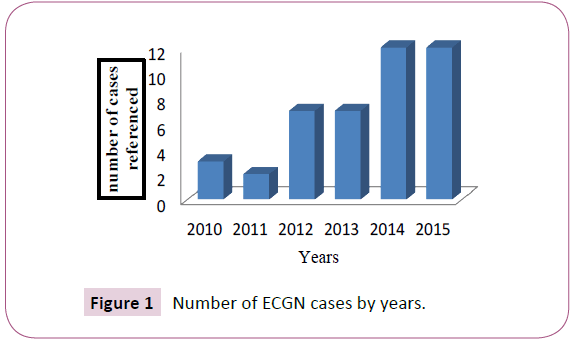
Out of 750 punctures kidney biopsies, 50 biopsies concluded at ECGN. There were 43 files selected for our study (the remaining seven files were excluded because six were not found and one was incomplete). The hospital proportion was 5.73%. There was a progressive increase in the number of cases by years with a maximum of 12 cases in 2014 and 2015 (Figure 1). The mean age was 32.53 years old with (4-70 years). There were 27 women (63%) and 16 men (37%), as a sex-ratio of 0.59. The duration of illness at admission was 53.2 days with (15-150 days). Edema of the lower limbs was present in 87.3%; hypertension in 53.5% of cases; gross hematuria in 23.25% of cases; anuria in 25.6% of cases and oliguria in 11.6% of the cases. Urinary strip showed a proteinuria (44.2%), hematuria (32.6%), and digestive manifestations in 24 patients (55.8%). Polyarthralgia was found in 11 patients (25.6%) and cutaneous signs were detected in 10 patients (23.3%); it was purpura and erythema in vespertilio. Eight patients (18.6%) had cardiac manifestations such as congestive heart failure. There were 4 patients (9.3%) who had pulmonary manifestations including 3 cases of condensation syndrome and 1 case of fluid pleural effusion.
Mean serum creatinine was 79.4 mg/l with (2.83-310.3 mg/l). Blood urea was reported in 34 cases (79.1%). The average was 1.81 g/l with (0.15 to 6.5 g/l). Protidemia was measured in 33 patients (76.7%) with an average of 60.6 mg/l (48.8 to 77 mg/l). Mean albumin levels in 33 patients (76.7%) were 23.8 mg/l with (12.9 - 39 mg/l). The average hemoglobin level was 8.42 g/dl with (4.4- 14 g/dl). The proteinuria of 24 hours in 38 patients (88.4%) was an average of 3.94 g/24 h with (0.56-17 g/24 h). Immunologically, serum complement measurements were performed in 9 patients. The C3 level was low in 2 patients and normal in 7 patients. The C4 level was low in 2 patients, elevated in 2 patients and normal in 5 patients. The ASLOs dosed in 6 patients were normal. The ANA assay (anti-nuclear antibodies) was performed in 3 patients, of which 2 were negative and 1 was positive. The native anti-DNA was reported in 12 patients including 4 positive and 8 negatives. ANPA was measured in 10 patients, 8 positive and 2 negatives. The GBM antibodies were reported in 3 patients including 2 negative and 1 positive case (Goodpasture syndrome). Other immunological and virological parameters were summarized in Table 1.
| Variable | Positiveness | |
|---|---|---|
| n | % | |
| Blood cultures | 1 | 2.3 |
| Anti streptolysin O antibodies | 0 | 0 |
| Anti-nuclear antibodies | 1 | 2.3 |
| Anti DNA antibodies | 4 | 9.3 |
| ANPA | 8 | 18.6 |
| GMB antibodies | 1 | 2.3 |
| Hbs antigen | 1 | 2.3 |
| Hepatitis C virus | 1 | 2.3 |
| HIV | 0 | 0 |
| Syphilis serology | 0 | 0 |
Table 1: Immunological parameters studied.
Indications for renal biopsy were nephrotic syndrome (25.6%) and rapidly progressive glomerulonephritis in 16.3% of cases. The other indications of the renal biopsy are presented in Table 2. Fibrocellular croissants type accounted for 25% of cases. It was an association of croissants of different age.
| Indications | Absolute Frequency (n) | Percentage (%) |
|---|---|---|
| Nephrotic Syndrom | 11 | 25.6 |
| RPGN | 7 | 16.3 |
| Exploration of an impairment of renal function | 7 | 16.3 |
| Proteinuria/lupus | 6 | 14 |
| Glomerular nephropathy syndrome | 5 | 11.6 |
| Atypical acute glomerulonephritis | 2 | 4.6 |
| Persistent acute renal failure | 1 | 2.3 |
| Proteinuria/vasculitis | 1 | 2.3 |
| Not specified | 3 | 7 |
| Total | 43 | 100 |
Table 2: Indications of kidney biopsy puncture.
Fourteen patients (32.6%) were dialysed with the main indication of poorly tolerated uremia. The evolution was marked by: remission in 41.9% of cases and 9.3% of relapse cases. This remission was complete for 16.3% of patients and partial for 25.6%. There were 14% of cases of resistance to treatment and 20.9% of cases of death.
Discussion
In our work, the prevalence of extra-capillary glomerulonephritis (ECGN) was 5.73%. It was similar to the results noted in India [5]. In Morocco, the prevalence is higher [6] probably related to a greater availability of renal biopsy. It remains lower in China and in South Africa [9,10]. In Eastern Europe and North America it varies between 2 and 10% of all nephrological conditions [11]. The age of the patients is relatively young since the main causes of ECGN are pathologies of the young subject namely lupus disease, necrotizing vasculitis and post-infectious acute glomerulonephritis. In addition, 13.95% of our patients are pediatric patients versus 26% in the Gupta series [12]. This greater or lesser incidence in children is mainly related to postinfectious forms, particularly acute glomerulonephritis. These results raise the interest of systematically making the practice of renal biopsy puncture in any child with acute glomerulonephritis whose evolution seems atypical, that is to say, persistence of renal failure for more than 3 days. According to Gupta [12], the female predominance found in all series is linked to the high prevalence of autoimmune diseases in women. This corroborates the results of our study which found the lupus disease as cause in 30.2% of the cases and this one having a feminist tropism demonstrated. Delayed admission may explain the poor clinical outcome of the majority of patients. Average patient admission time was 53.2 ± 36.9 days, related to the use of other therapeutic means such as 46.5% of herbal medicine versus 50 ± 60 days in Morocco the median was 37 days versus 30 in India [5,6].
Comparison with the data of the literature shows that the clinical picture was less severe in our series and the positivity of the immunology is variously appreciated in the literature; this difference in the results is essentially related to the variability of the causes according to the geographical origin and the epidemiology of the countries [5,6,9,13]. Etiologically vasculitis, with a frequency of 48.9%, was the main cause of EGNC in our series as for Andrassy et al. in Germany [3]. Lupus was the second leading cause with 30.2% in our series versus 20.5% in South Africa and 42.6% in Morocco where it is the leading cause of GNEC [6,10]. In our study, anuria, elevated serum creatinine, and the circumferential arrangement of the croissants represented the elements of poor renal prognosis. Arrayhani in his series also retained anuria and creatinine as a factor of poor prognosis [6]. On the other hand, in the Sasatomie series in Japan [14,15], only serum creatinine elevated on admission was considered as a poor prognostic factor (Table 3).
| Elevated Serum creatinine | Oligoanuria | Fibrocellular croissants | ||
|---|---|---|---|---|
| Our Work | + | + | + | |
| Arrayhani [6] | + | + | - | |
| Sasatomie [14] | + | - | - | |
| Rampelli [15] | + | - | + | |
| Choudhury [5] | - | - | + | |
Table 3: Comparison of factors of poor renal prognosis between our study and the literature.
Conclusion
ECGN is a serious kidney disease with a very poor prognosis. This study allowed us to determine its extent in Senegal. We note that in the absence of fast and adequate management of patient evolution is inevitably towards the CKD. Early diagnosis and early management are therefore necessary to increase the chances of recovery from normal renal function and avoid progression to chronicity.
References
- Esnault V, Moreau A, Testa A, Besnier D (2006) Glomerulonephrites extracapillaires. Nephrol Ther 2: 446-60.
- Seitz B, Esnault V (2009) Epidemiologie des maladies renales unite inserm, genetique epidemiologique. EMC: Nephrologie.
- Andrassy K, Kuster S, Waldherr R, Ritz E (1991) Rapidly progressive glomerulonephritis: Analysis of prevalence and clinical course. Nephron 59: 206-212.
- Lohr JW (2015) Rapidly progressive glomerulonephritis: Back ground, pathophysiology epidemiologie. Medscape.
- Choudhury TA, Singh RG, Singh S, Singh TB, Rathore SS, et al. (2014) Clinicopathologic spectrum of crescentic glomerulonephritis: A hospital-based study. Saudi J Kidney Dis Transpl 25: 689-696.
- Arrayhani M, El Amraoui H (2013) GNEC au CHU de Fes: Caracteres epidémiologiques, cliniques, paracliniques therapeutique et evolutive a propos de 68 cas. These de Med, Nephrologie. Fes, CHU de Fes 134.
- Okpechi I, Swanepoel C, Duffield M, Mahala B, Wearne N, et al. (2011) Patterns of renal disease in Cape Town South Africa: A 10 year review of a single-center renal biopsy database. Nephrol Dial transplant 26: 1853-1861.
- Diouf B, Niang A, Ka EF, KéitaY, Dial C, et al. (2001) Analyse de 115 biopsies renales realisees a Dakar. Dakar Med 46: 51-53.
- Tang Z, Wu Y, Wang Q, Zeng C, Yao X, et al. (2003) Clinical spectrum of diffuse cresscenteric glomerulonephritis in chinese patients. Chin Med J 116: 1737-1740.
- Zent R, Van Zyl Smit R, Duffield M, Cassidy MJ (1994) Crescentic glomerulonephritis at goote shuur hospital, South Africa, not a benign disease. Clin Nephrol 42: 22-29.
- Peteersson EE, Saunedlin B, Heigl Z (1995) Incidence and outcome of pauciimmune necrotizing and crescentic glomerulonephritis in adults. Clin Nephrol 43: 141-149.
- Gupta R, Singh L, Sharma A, Bagga A, Dinda AK, et al. (2011) Crescentic glomerulonephritis: A clinical and histomorphological analysis of 46 cases. Indian J Pathol Microbiol 54: 495-500.
- Deepak D, Gulati S, Sharma RK, Prasad N, Jain M, et al. (2008) Clinical spectrum and outcome of crescentic glomerulonephritis in children in developing countries. Pediatr Nephrol 23: 389-394.
- Sasatomi Y, Kiyoshi Y, Takabeyashi S (1999) A clinical and pathological study on the characteristics and factors influencing the prognosis of crescentic glomerulonephritis using a cluster analysis. Pathol Int 49: 781-785.
- Rampelli SK, Rajesh NG, Srinivas BH, Swaminathan RP, Priyamvada PS, et al. (2016) Clinical spectrum and outcomes of crescentic glomerulonephritis: A single center experience. Indian J Nephrol 26: 252-256.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences