Body Mass Index Impact on the Long-Term Outcome after Kidney Transplantation in Japanese Patients
Morita K*, Iwami D, Takada Y, Higuchi H, Sasaki H and Shinohara N
Department of Urology, Hokkaido University Hospital, Sapporo, Japan
- Corresponding Author:
- Ken Morita
Department of Urology
Hokkaido University Hospital
Hokkaido, Japan.
Tel: +81-90-8274-9540
Fax: +81-154-41-2399
E-mail: kenordic@mac.com
Received date: March 30, 2017; Accepted date: April 22, 2017; Published date: April 29, 2017
Citation: Morita K, Iwami D, Takada Y, et al. Body Mass Index Impact on the Long- Term Outcome after Kidney Transplantation in Japanese Patients . Adv kidney Dis Treat. 2017, 1:2.
Abstract
Objective: While high BMI has negative impact on patients with acute or chronic kidney disease, low BMI is related to mal-nutrition and poor survival in patients on dialysis. On the other hand, pretransplant medical policy recommends recipients to improve their overweight status in order to prevent postoperative surgical complications. We investigated how pretransplant BMI influence postoperative course in Japanese end-stage renal disease patients. Patients and methods: We reviewed 219 patients who underwent kidney transplantation between 1986 and 2014 at our institution. Pediatric recipients (age<20) were excluded. We divided the recipients into 4 groups by BMI (under 18.5, 18.5-21.9, 22.0-24.9, over 25.0). Postoperative complications (wound related and infectious adverse events), allograft rejection, and allograft survival were investigated among the BMI groups. Results: Post-transplant infectious disease was more frequent (5 in 27 cases: 18.5%) in over 25.0 group than any of other BMI groups (0 to 2.1%, p=0.006). Ten year allograft survival rate of over 25.0 group was inferior to that of under 18.5 group (p=0.037). Meanwhile, BMI over 25.0 did not impair graft survival compared to other factors (age, preemptive transplantation, ABO blood type incompatibility and mycophenolate mofetile utilization) in Cox proportional hazards analysis. Conclusion: Overweight (BMI>25.0) in Japanese kidney recipients might affect post-transplant infectious disease occurrence; however, it is not a deteriorating factor for long-term allograft survival. Keywords: Chronic kidney disease; Dialysis; Transplantation; BMI
Keywords
Chronic kidney disease; Dialysis; Transplantation; BMI
Introduction
The obesity adversely affects the condition of a patient with AKI and CKD. On the other hand, it is a fact that BMI relates to the survival rate positively in the patients on dialysis, since a drop of the muscle quantity drives malnutrition as the cause of poor patients survival. When such an end-stage renal disease (ESRD) patient is going to receive a renal transplantation, weight loss is instructed in many institutes because of a consideration for complications after the transplant. It has not been well answered whether or not and how much we have to improve obesity before renal transplantation for an altitude obesity patient [1]. In order to prevent complications after transplant, it is necessary to lose weight without reducing quantity of muscle [2]. Since there are some differences in frequency and gravity of obesity by a country and the race, it is difficult to make a constant standard. The difference of patient survival rate between any BMI groups is reported to be negligible compared with dialysis patients who had not been transplanted. Besides post-transplant short-term problems; operation time, wound infection, hospital stay and delayed graft function, high BMI does not affect the long-term patient survival [3]. Pretransplant BMI criteria of our institute had been changed fewer than 25 at 2011, as marginal line of Japanese overweight definition. We reviewed the medical records and estimated the justification of our BMI criteria.
Patients and Methods
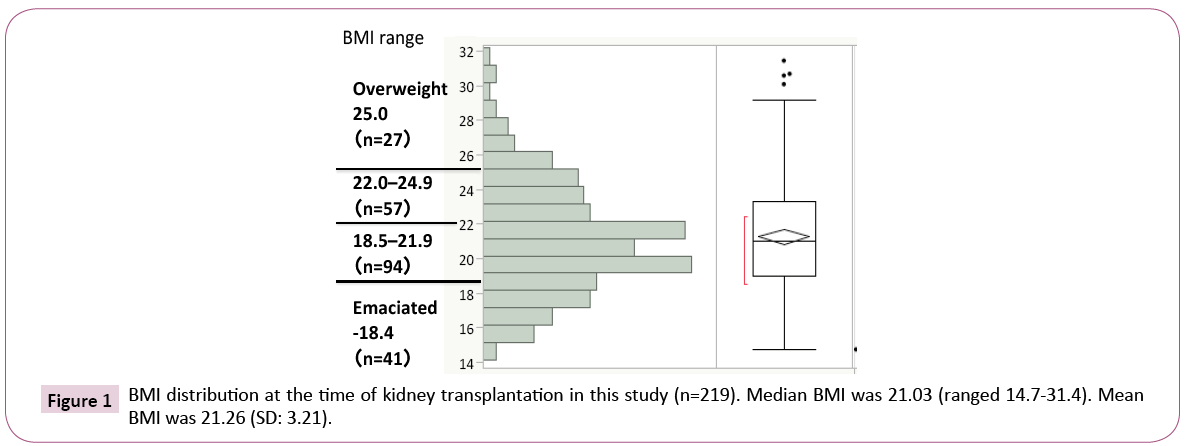
We reviewed medical records of 285 patients who underwent kidney transplantation between 1986 and 2014 at our institution. Pediatric recipients (age at transplantation <20) were excluded. There were residual 219 patients (123 male and 96 female). We divided them into 4 groups by BMI at the transplantation. There were 27 cases of overweight recipients (BMI over 25.0), 57 cases with BMI 22.0-24.9 (high average), 94 cases with BMI 18.5-21.9 (low average), and 41 cases of emaciated (BMI under 18.5). Mean BMI in total recipients was 21.0 (Figure 1). Postoperative comwww.imedpub.com/scholarly/obesity-journals-articles-ppts-list.phpplications (wound related and infectious adverse events), allograft rejection, and allograft survival were investigated among the BMI groups.
This retrospective study was approved by Hokkaido University Hospital Committee of Clinical Research Guideline (#014-0372).
Statistical analyses were performed with JMP Clinical for JMP Academic Suite 32/64-bit (SAS Institute Japan). One-way ANOVA was used to compare normally distributed continuous variables and the Kruskal-Wallis H test was used to evaluate skewed or discrete ordinal variables. The chi-square test was used to compare nominal scale variables. Survival curves were estimated with the Kaplan-Meier method using the log-rank test. In order to evaluate the influences of BMI, the Cox proportional hazards model was employed. Proportional hazards assumption was confirmed by In[-In (survival function)]. Two-tailed P<0.05 was considered statistically significant.
Results
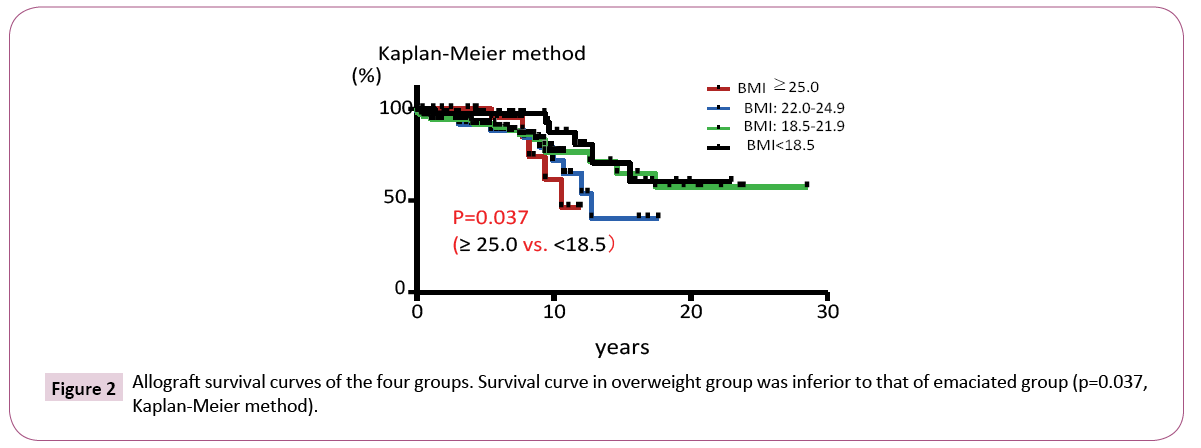
Post-transplant infectious disease (needed hospital stay) was more frequent (5 in 27 cases: 18.5%) in overweight (BMI>25.0) group than any of other BMI groups (0 to 2.1%, p=0.006). Ten years allograft survival of over 25.0 group was inferior to that of emaciated (BMI<18.5) group (45 vs. 88%, p=0.037). There were no significant difference of surgical wound related complications, allograft rejection rate, and the frequency of allograft loss among the BMI groups (Table 1).
| BMI Group (n) |
Wound related | Infection | Acute rejection | Allograft loss | 10 year graft survival |
|---|---|---|---|---|---|
| <18.5 (41) |
2 (4.9%) |
0 (0.0 %) |
7 (17.1%) |
7 (17.1%) |
88% |
| 18.5-21.9 (94) |
4 (4.3%) |
2 (2.1%) |
11 (11.7%) |
16 (17.0%) |
76% |
| 22.0-24.9 (57) |
4 (7.0%) |
1 (1.8%) |
4 (7.0%) |
11 (19.3%) |
65% |
| 25.0< (27) |
3 (11.1%) |
5* (18.5%) |
4 (14.8%) |
5 (18.5%) |
45% ** |
* P=0.006
** P=0.037
Table 1: Adverse effects and survival.
Allograft survival curve in overweight group was inferior to that of emaciated group (p=0.037, Kaplan-Meier method, Figure 2).
Since these four BMI groups presented different baseline components as a patients’ clinical cohort, we examined each differences as Table 2. For baseline factors of the recipient, evaluation period was longer in emaciated group and overweight group, recipient age was younger in emaciated group, male recipient rate was high in higher BMI groups, dialysis period was short in overweight group. For donor, male rate was high in emaciated group; there were some differences in HLA mismatches, DCD rate, ABO incompatibility among the groups. Furthermore, induction rate of some immunosuppressant was different in overweight group (Table 2).
| BMI group |
Emaciated 〜18.4 |
Low ave. 18.5〜21.9 |
High ave. 22.0〜24.9 |
Overweight 25.0〜 |
|
|---|---|---|---|---|---|
| Recipient | FU period (years) | 9.4 0-23 |
6.6 0-28 |
5.2 0-18 |
7.1 0-12 |
| Age (years) |
35 20-67 |
42 21-67 |
45 20-69 |
44 25-63 |
|
| Male(%) | 6 (14.6) | 52 (55.3) | 43 (75.4) | 22 (81.4) | |
| Dialysis (years) | 2.5 0-31.4 |
2.0 0-30 |
2.7 0-22.3 |
1.3 0-13 |
|
| Original disease | Diabetes | 3 (7.3) | 13 (13.8) | 11 19.2) | 4 (14.8) |
| IgAN | 10 (24.4) | 20 (21.3) | 9 (15.8) | 7 (25.9) | |
| polycystic | 1 (2.4) | 7 (7.4) | 7 (12.3) | 2 (7.4) | |
| Donor | Age (years) |
55 21-78 |
55 13-74 |
57 24-75 |
57 39-69 |
| Male(%) | 21 (51.2) | 37 (39.4) | 22 (38.6) | 8 (29.6) | |
| HLA mismatches | 3 0-5 |
3 0-6 |
2 0-6 |
3 0-5 |
|
| Deceased | 9 (22.0) | 22 (23.4) | 9 (15.8) | 3 (11.1) | |
| ABO incompatible | 8 (19.5) | 16 (17.0) | 18 (31.6) | 5 (18.5) | |
| aHLA sensitized | 3 (7.3) | 5 (5.3) | 2 (3.5) | 1 (3.7) | |
| IS | Basiliximab | 35 (85.4) | 82 (87.2) | 50 (87.7) | 22 (81.5) |
| Rituximab | 10 (24.4) | 21 (22.3) | 18 (31.6) | 3 (11.1) | |
| Tacrolimus | 32 (78.0) | 64 (68.1) | 35 (61.4) | 23 (85.2) | |
| MMF | 33 (80.5) | 74 (78.7) | 46 (80.7) | 26 (96.3) |
Table 2: Baseline cohort differences among BMI groups.
In order to adjust these confounding factors in baseline cohort among the groups, Cox proportional hazards analysis was performed. Univariate analysis revealed that recipient age (>60), polycystic kidney disease as an original disease, preemptive transplantation, immunosuppressant (basiliximab, rituximab, tacrolimus, MMF) were related to risk factors (Table 3). We selected 5 exposure factors including BMI as outcome events/total cohort number (39/219) and tested by multivariated alanysis. BMI (>25.0) did not impair long-term graft survival compared to other significant factors (recipient age, preemptive transplantation, ABO blood type incompatibility and mycophenolate mofetile induction) (Table 4).
| HR | 95% CI | P | |
|---|---|---|---|
| Male recipient | 1.03 | [0.76, 1.38] | 0.85 |
| Recipient age>60 * | 2.79 | [1.74, 4.28] | 0.00 |
| BMI ≥ 25 | 0.84 | [0.55, 1.36] | 0.46 |
| Diabetes * | 0.57 | [0.39, 0.88] | 0.01 |
| IgA Nephropathy | 0.84 | [0.60, 1.21] | 0.35 |
| Polycystic kidney dis. * | 0.51 | [0.31, 0.90] | 0.02 |
| Preemptive * | 0.46 | [0.32, 0.68] | 0.00 |
| Deceased | 0.97 | [0.67, 1.44] | 0.87 |
| Donor age>60 | 1.26 | [0.91, 1.72] | 0.16 |
| Male donor | 0.80 | [0.59,1.08] | 0.14 |
| ABO incompatible | 0.97 | [0.67, 1.44] | 0.87 |
| aHLA sensitized | 0.71 | [0.38, 1.50] | 0.34 |
| Basiliximab * | 0.15 | [0.07, 0.30] | 0.00 |
| Rituximab * | 0.28 | [0.19, 0.40] | 0.00 |
| Tacrolimus * | 0.44 | [0.29, 0.67] | 0.00 |
| MMF * | 0.00 | [0.02, 0.02] | 0.00 |
Table 3: Cox proportional hazards analysis (Univariate).
| HR | 95% CI | P | |
|---|---|---|---|
| Recipient age>60 * | 1.81 | [1.12, 2.84] | 0.017 |
| Preemptive * | 0.67 | [0.46, 0.99] | 0.045 |
| ABO incompatible | 1.44 | [0.99, 2.04] | 0.052 |
| MMF * | 0.00 | [0.00, 53.8] | 0.000 |
| BMI ≥ 25 | 1.25 | [0.73, 1.95] | 0.769 |
(Total number: 219/outcome events: 39=5.62)
Table 4: Cox proportional hazards analysis (multivariate).
Discussion
Our data could not clarify the effect of higher BMI for long-term post-transplant allograft survival. It might be due to the fact that there are no recipients with morbidly obese which was seen in other foreign reports [2]. Additionally, such severe obesity may cause short-term events (delayed graft function, wound infection, longer operation time, long hospital stay and new onset diabetes after transplantation), which did not reach any disadvantage for the long-term period [3].
Obesity control guideline in Japan (2006) recommended that overweight case should diet intake restriction (25 kcal/kg/day) along with standard body weight [4]. But well-controlled CKD patients have been restricted in protein intake (0.6 g/kg/day). Calorie restriction in CKD patients may result in mal-nutrition and Nitrate unbalance with simple weight loss for BMI control. Pretransplant high BMI and high muscle volume was reported not to be surgical and immunological risk because of low mortality and graft failure ratio [5]. We have to adjust each recipient’s nutrition status (serum albumin, protein intake) in order to prevent the trap of ‘obesity paradox’ [6].
We must pay much attention for low with high BMI patient as a true high risk recipient (sarcopenia obesity) which is independent risk factor of post-transplant morbidity and mortality [7,8]. For the future, we will test the body cell mass analysis for CVD, fat obesity risk criteria using impedance evaluation other than BMI [9,10]. Our data was small in patient number and there are some limitations existed in our study. Overweight patient population was different from other western countries, our retrospective cohort study could not reveal the significance of BMI in outcome of kidney transplantation and background patient cohort of our data was different among the 4 groups in some clinical patient’s characters.
Conclusion
Overweight (BMI>25.0) in Japanese kidney recipients might affect post-transplant infectious disease occurrence; however, it is not a deteriorating factor for long-term allograft survival.
References
- Kalantar-Zadeh K, von Visger J, Foster III CE (2015) Overcoming the body mass index as a barrier in kidney transplantation. Am J Transplant 15: 2285-2287.
- Matas AJ, Smith JM, Skeans MA, Thompson B, Gustafson SK, et al. (2015) OPTN/SRTR 2013 annual data report: Kidney. Am J Transplant 15: 1-34.
- Bennett WM, McEvoy KM, Henell KR, Pidikiti S, Douzdjian V, et al. (2011) Kidney transplantation in the morbidly obese: Complicated but still better than dialysis. Clin Transplant 25: 401-405.
- Yamakado M (2013) Criteria for obesity diseases, especially for visceral fat obesity and clinical significance of non-apparent visceral obesity. J Japan Soc Ningen Dock 3: 492-499.
- Streja E, Molnar MZ, Kovesdy CP, Bunnapradist S, Jing J, et al.(2011) Associations of pre-transplant weight and muscle mass with mortality in renal transplant recipients. Clin J Am Soc Nephrol 6: 1463-1473.
- Park J, Ahmadi SF, Streja E, Molnar MZ, Flegal KM, et al. (2014) Obesity paradox in end-stage kidney disease patients. Prog Cardiovasc Dis 56: 415-25.
- Dietch ZC, Guidry CA, Davies SW, Sawyer RG (2015) Hypoalbuminemia is disproportionately associated with adverse outcomes in obese elective surgical patients. Surg Obes Relat Dis 11: 912-918.
- Lentine K, Santos RD, Axelrod D, Schnitzler MA, Brennan DC, et al. (2012) Obesity and kidney transplant candidates: How big is too big for transplantation? Am J Nephrol 36: 575-586.
- Krishnan N, Higgins R, Short A, Zehnder D, Pitcher D, et al. (2015) Kidney transplantation significantly improves patient and graft survival irrespective of BMI: A cohort study. Am J Transplant 15: 2378-2386.
- Kalantar-Zadeh K, von Visger J, Foster CE 3rd (2015) Overcoming the body mass index as a barrier in kidney transplantation. Am J Transplant 15: 2285-2287.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences