Anatomical study of the superior lateral genicular artery : application to composite flaps of the lateral femoral condyle
Ndiaye AI1*, Gaye M1, Wade R1, Ndiaye AB1, Coyette M2, Duisit J2, Lengele B2 and Ndiaye AS3
1Department of Anatomy and Organogenesis Laboratory, Cheikh Anta Diop University, Dakar, Senegal
2Department of Anatomy, Catholic University of Leuven, Brussels, Belgium
3Department of Anatomy, Assane Seck University of Ziguinchor, Dakar, Senegal
- *Corresponding Author:
- Ndiaye AI
Department of Anatomy and Organogenesis Laboratory,
Cheikh Anta Diop University,
Dakar,
Senegal
Tel: 221705023652
E-mail: aynina.ndiaye@ucad.edu.sn
Received date: January 27, 2023, Manuscript No. IPJASR-22-15715; Editor assigned date: January 30, 2023, PreQC No. IPJASR-22-15715 (PQ); Reviewed date: February 14, 2023, QC No. IPJASR-22-15715; Revised date: April 11, 2023, Manuscript No. IPJASR-22-15715 (R); Published date: April 19, 2023, DOI: 10.36648/IPJASR.6.1.006
Citation: Ndiaye AI, Gaye M, Wade R, Ndiaye AB, Coyette M, et al. (2023) Anatomical Study of the Superior Lateral Genicular Artery: Application to Composite Flaps of the Lateral Femoral Condyle. J Anat Sci Res Vol:6 No:1
Abstract
Introduction: The Superior Lateral Genicular Artery (SLGA) is the first collateral branch of the popliteal artery. It vascularises part of the lateral femoral condyle and the surrounding musculocutaneous territory. The possibility of using a composite osteo-fascio-cutaneous flap at the level of the lateral femoral condyle is of definite anatomical interest. The aim of this study was to investigate the descriptive anatomy of the lateral superior knee artery with a view to performing a composite flap of the lateral femoral condyle.
Material and methods: We dissected a series of 52 knees, nine of which were injected.
Results: The mean length of the SLGA was 38.9 mm ± 0.06 mm. It gave short branches to the periosteum of the lateral femoral condyle below and to the popliteal surface of the femur above. The SLGA terminated at the lateral border of the femur and anterior to the lateral intermuscular septum, between the vastus lateralis and the short head of the biceps femoris, on average 39.1 mm (21-58 mm) superiorly and anteriorly to the lateral epicondyle; it gave its terminal branches variably. In addition, in ¾ of the cases, it produced a fasciocutaneous perforator.
Conclusion: The anatomical data show that the composite flap of the lateral femoral condyle centred on the supra-lateral knee artery, whether fascio-cutaneous or osteo-fascio-cutaneous, constitutes an interesting possibility as a free composite flap, provided that a pedicle of approximately 4 cm is sufficient.
Keywords
Superior lateral genicular artery; Anatomy; Dissection; Flap
Introduction
The Superior Lateral Genicular Artery (SLGA) is the first collateral branch of the popliteal artery. It vascularises part of the lateral femoral condyle and the surrounding musculocutaneous territory. The possibility of using an osteo-fascio-cutaneous composite flap at the level of the lateral femoral condyle is of definite anatomical interest [1]. We dissected a series of 52 knees, 9 of which were injected. The objective of this work is to study the descriptive anatomy of the supra-lateral knee artery with a view to making flaps of the lateral-distal part of the thigh.
Materials and Methods
The study was conducted at the anatomy laboratory of the catholic university of Louvain in Brussels. Fifty-two knees from 31 cadaveric subjects were studied. Twenty-one subjects were dissected bilaterally. Twenty-seven knees belonged to fresh bodies and 25 knees to embalmed bodies.
The pure dissection technique was used for 43 knees, while 9 knees were injected and dissected.
For pure dissection, a lateral parasagittal skin incision was made on the posterior aspect of the knee, joining two transverse counter incisions on the distal third of the thigh and the distal quarter of the leg. The skin and subcutaneous cellular tissue on the lateral side were meticulously peeled off flush with the fascia lata, using foam dissecting scissors, sparing the septocutaneous perforators in the distal third of the lateral thigh. The detachment was made up to the lateral part of the patella. The fascia lata was incised longitudinally at the level of the lateral muscle septum [2]. The distal part of the biceps femoris was disinserted and reclined upwards to expose the lateral part of the popliteal fossa and the lateral femoral condyle. The supra-lateral vessels were dissected retrograde from the terminal branches to the original popliteal vessels [3].
Nine knees were dissected after injection of the SLGA.
Measurements of the SLGA were made with a compass, without stretching it while respecting its course.
Results
The SLGA was present in all our cases and originated at the lateral part of the popliteal artery. It had a constant course, running slightly anteriorly and superiorly along the upper border of the lateral femoral condyle to the lateral border of the femur where it divided into terminal branches [4].
The mean length of the SLGA was 38.9 mm ± 0.06 mm.
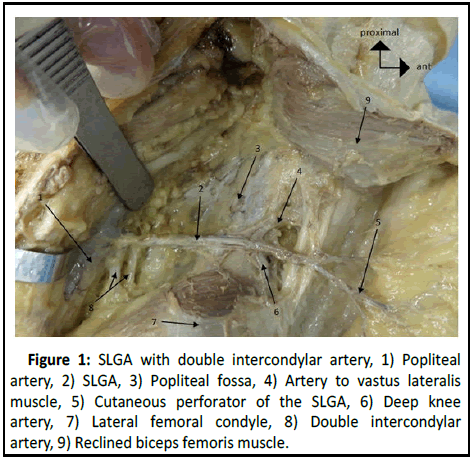
It consistently gave rise to a collateral branch for the intercondylar notch, which originated between 2.5 mm and 8 mm from its origin. In one case, this intercondylar branch was double (Figure 1).
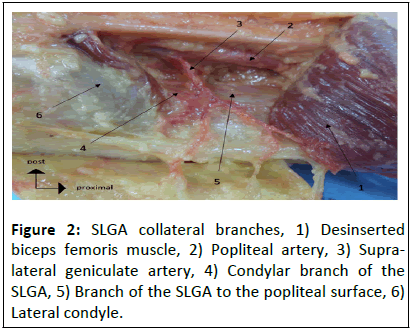
The SLGA gave short branches to the periosteum of the condyle inferiorly and to the popliteal surface superiorly (Figure 2).
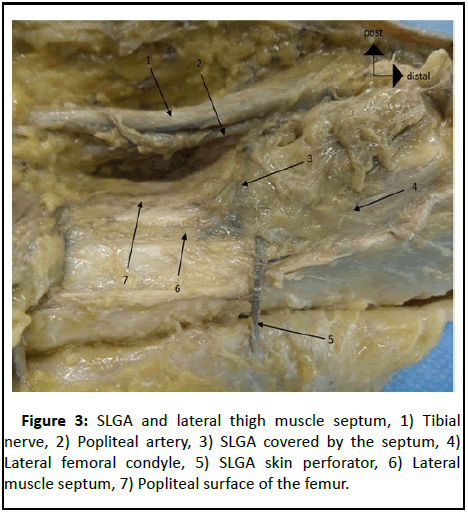
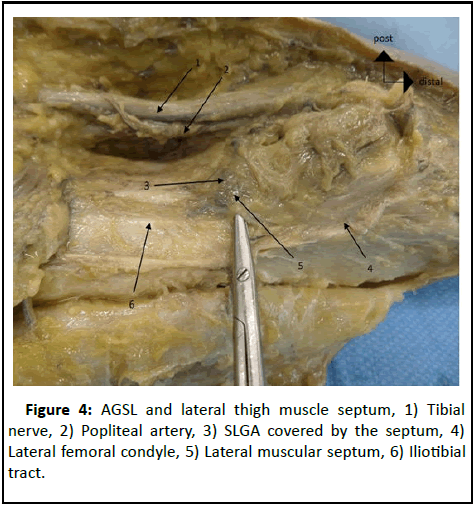
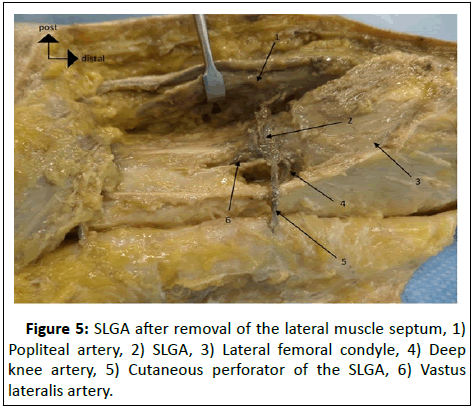
The SLGA terminated at the lateral border of the femur and anterior to the lateral intermuscular septum, between the vastus lateralis and the short head of the biceps femoris, on average 39.1 mm (21-58 mm) superiorly and slightly anterior to the lateral epicondyle (Figures 3-5).
The SLGA gave out its terminal branches in a variable manner. These terminal branches were a fasciocutaneous perforator, a deep branch to the knee joint, a branch to the vastus lateralis muscle and a branch to the biceps femoris muscle.
Of the 52 cases dissected, a fasciocutaneous perforator from the SLGA was present 39 times, i.e. in 75% of cases. In 5 cases, the SLGA produced 2 cutaneous perforations. The fascial-cutaneous perforator crossed the fascia just behind the iliotibial tract and the vastus lateralis muscle [5,6].
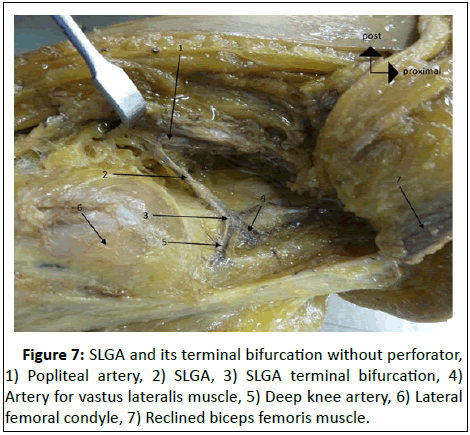
The most common mode of termination of the SLGA was a 3 branch trifurcation (a vastus lateralis branch, a deep knee joint branch and a skin perforator) in 12 cases (Figure 4), followed by a 2 branch bifurcation (a vastus lateralis branch and a deep knee joint branch) in 11 cases (Figures 6-7).
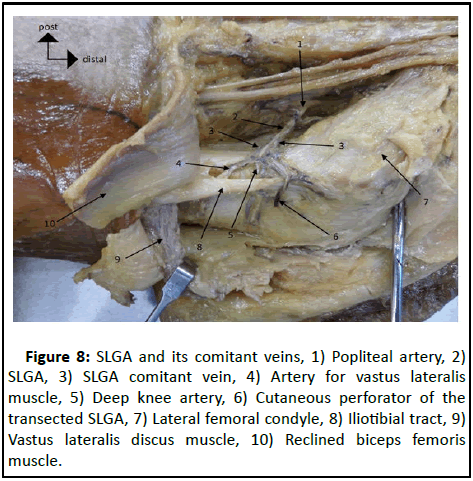
The SLGA was constantly accompanied by 2 satellite veins placed laterally on either side of its wall (Figure 8).
Figure 8: SLGA and its comitant veins, 1) Popliteal artery, 2) SLGA, 3) SLGA comitant vein, 4) Artery for vastus lateralis muscle, 5) Deep knee artery, 6) Cutaneous perforator of the transected SLGA, 7) Lateral femoral condyle, 8) Iliotibial tract, 9) Vastus lateralis discus muscle, 10) Reclined biceps femoris muscle.
The mean external diameter of the cutaneous perforator at its origin was 1.74 mm. In 8 cases, it was small, measuring less than 1 mm in diameter.
Discussion
The SLGA is constantly found in the different studies. In our work, it is always the first collateral branch of the popliteal artery; authors such as Hayashi found its origin in the sural artery in 2 of the 10 cases in his series.
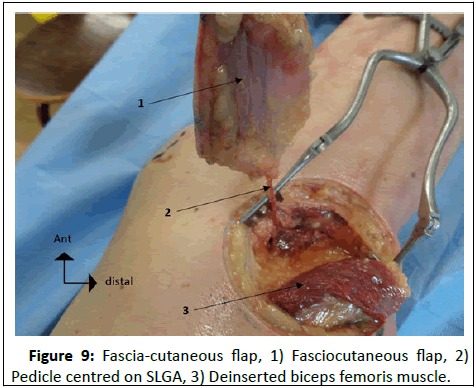
The mean length of the SLGA of 38.9 mm is approximately similar to the 37.86 mm found by Parvizi in his study of 28 knees [7]. Morsy on 23 dissected knees and Wong on 16 fresh knees found an average length of 56 mm and 64 mm respectively from its origin to the iliotibial tract; Gstoettner found the longest pedicle length: 93 mm. In practice, for a flap centred on the ALSG, an average pedicle length of about 4 cm should be considered (Figure 9).
One of the first collateral branches constantly found in our series is that destined for the intercondylar notch; it is poorly documented in the literature, its course and termination correspond to that of the middle artery of the knee, but it differs from it in its origin: In the classic works, the middle artery of the knee arises from the anterior surface of the popliteal artery [8].
During its course, the SLGA gives branches that perforate the periosteum, thus allowing the harvesting of a viable bone component.
The termination zone of the SLGA between the superior aspect of the lateral condyle inferiorly, the intermuscular septum posteriorly and the vastus lateralis muscle anteriorly was described by Hayashi. This zone corresponds to the birth area of the cutaneous perforator arising from the AGSL. The point of emergence was specified in relation to the lateral epicondyle, which is a palpatory landmark accessible on clinical examination; other authors have chosen the femorotibial joint line, which is lower than the epicondyle and more difficult to locate on palpation than the lateral epicondyle of the femur, although this landmark is more reliable using medical imaging [9]. Parvizi found an average distance of 56 mm between the perforator and the joint space, compared with 42 mm between the perforator and the epicondyle in our series and 74 mm between the lateral condyle of the femur and the perforator in Zumiotti.
The mode of termination of the SLGA is more varied than it appears. For Parvizi and Morsy the SLGA terminates in a superficial branch terminating at the superior-lateral part of the patella, with the septocutaneous perforator generally being the collateral of this superficial branch, and a deep articular branch that vascularises the lateral aspect of the femoral condyle with collaterals for the vastus lateralis muscle and the periosteum. We found 23.1% of cases of trifurcation with a cutaneous perforator of the SLGA which constitutes a terminal branch in its own right; similarly, the cutaneous perforator of the SLGA could be collateral of other terminal branches of the SLGA [10].
The SLGA was accompanied by 2 comittant veins also found by Morsy; these 2 vessels can, if necessary, be used for venous drainage of a free flap.
We found the fasciocutaneous perforator of the SLGA in 3 cases out of 4 and with a calibre at its origin greater than 1 mm in almost 85% of cases. With an average diameter of 1.74 mm at its origin, the SLGA cutaneous perforator is sufficiently calibrated for use in microsurgery in the case of a free flap. However, the fact that the cutaneous perforator is absent or small in 2 out of 5 cases justifies at least the performance of a doppler ultrasound before the harvesting of such a flap.
Conclusion
The anatomical data show that the composite flap of the lateral femoral condyle centred on the supra-lateral artery of the knee, whether fascio-cutaneous or osteo-fascio-cutaneous, is an interesting possibility as a free composite flap, provided that a pedicle of approximately 4 cm is sufficient. It has recently been used as is in calcaneal tendon loss and as the medial femoral condyle flap in upper limb pseudarthrosis and other applications are expected.
References
- Hayashi A, Maruyama Y (1990) The lateral genicular artery flap. Ann Plast Surg 24:310-317
[Crossref] [Google Scholar] [PubMed]
- Parvizi D, Vasilyeva A, Wurzer P, Tuca A, Lebo P, et al. (2016) Anatomy of the Vascularized Lateral Femoral Condyle Flap. Plast Reconstr Surg 137:1024e-1032e
[Crossref] [Google Scholar] [PubMed]
- Morsy M, Sur YJ, Akdag O, Eisa A, El-Gammal TA, et al. (2018) Anatomic and high resolution computed tomographic angiography study of the lateral femoral condyle flap: Implications for surgical dissection. J Plast Reconstr Aesthet Surg 71:33-43
[Crossref] [Google Scholar] [PubMed]
- Gstoettner C, Mayer JA, Aman M, Salminger S, Burger H, et al. (2019) Cutaneous angiosome of the chimeric SLGA perforator flap: Anatomical study and clinical considerations. J Plast Reconstr Aesthet Surg 72:1142-1149
[Crossref] [Google Scholar] [PubMed]
- Wong VW, Higgins JP (2016) Distally based iliotibial band flap: Anatomic study with surgical considerations. Reconstr Microsurg 32:551-555
[Crossref] [Google Scholar] [PubMed]
- Hayashi A, Maruyama Y (2001) Lateral intermuscular septum of the thigh and short head of the biceps femoris muscle: An anatomic investigation with new clinical applications. Plast Reconstr Surg 108:1646-1654
[Crossref] [Google Scholar] [PubMed]
- Zumiotti AV, Teng HW, Queipo Briceno NC, Lotierzo PH, Ishida LH, et al. (2005) Lateral flap of the thigh based upon the lateral superior genicular artery: An anatomic and histomorphometric study and clinical applications. Acta Ortop Bras 13:24-27
- Morsy M, Sur YJ, Saint-Cyr M, Moran S (2015) Detailed anatomy of the superior lateral genicular artery for design of a vascularized bone flap from the lateral femoral condyle. Plast Reconstr Surg 136:14-15
- Spokevicius S, Jankauskas A (1995) Anatomy and clinical applications of a composite cutaneo-subcutaneous flap based on the lateral superior genicular vessels. J Reconstr Microsurg 11:15-20
[Crossref] [Google Scholar] [PubMed]
- Wong VW, Burger HK, Iorio ML, Higgins JP (2015) Lateral femoral condyle flap: An alternative source of vascularized bone from the distal femur. J Hand Surg Am 40:1972–1980
[Crossref] [Google Scholar] [PubMed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences